Abstract
Knowledge on the outcome of C2-fractures is founded on heterogenous samples with cross-sectional outcome assessment focusing on union rates, complications and technical concerns related to surgical treatment. Reproducible clinical and functional outcome assessments are scant. Validated generic and disease specific outcome measures were rarely applied. Therefore, the aim of the current study is to investigate the radiographic, functional and clinical outcome of a patient sample with C2-fractures. Out of a consecutive series of 121 patients with C2 fractures, 44 met strict inclusion criteria and 35 patients with C2-fractures treated either nonsurgically or surgically with motion-preserving techniques were surveyed. Outcome analysis included validated measures (SF-36, NPDI, CSOQ), and a functional CT-scanning protocol for the evaluation of C1–2 rotation and alignment. Mean follow-up was 64 months and mean age of patients was 52 years. Classification of C2-fractures at injury was performed using a detailed morphological description: 24 patients had odontoid fractures type II or III, 18 patients had fracture patterns involving the vertebral body and 11 included a dislocated or a burst lateral mass fracture. Thirty-one percent of patients were treated with a halo, 34% with a Philadelphia collar and 34% had anterior odontoid screw fixation. At follow-up mean atlantoaxial rotation in left and right head position was 20.2° and 20.6°, respectively. According to the classification system of posttreatment C2-alignment established by our group in part I of the C2-fracture study project, mean malunion score was 2.8 points. In 49% of patients the fractures healed in anatomical shape or with mild malalignment. In 51% fractures healed with moderate or severe malalignment. Self-rated outcome was excellent or good in 65% of patients and moderate or poor in 35%. The raw data of varying nuances allow for comparison in future benchmark studies and metaanalysis. Detailed investigation of C2-fracture morphology, posttreatment C2-alignment and atlantoaxial rotation allowed a unique outcome analysis that focused on the identification of risk factors for poor outcome and the interdependencies of outcome variables that should be addressed in studies on C2-fractures. We recognized that reduced rotation of C1–2 per se was not a concern for the patients. However, patients with worse clinical outcomes had reduced total neck rotation and rotation C1–2. In turn, C2-fractures, especially fractures affecting the lateral mass that healed with atlantoaxial deformity and malunion, had higher incidence of atlantoaxial degeneration and osteoarthritis. Patients with increased severity of C2-malunion and new onset atlantoaxial arthritis had worse clinical outcomes and significantly reduced rotation C1–2. The current study offers detailed insight into the radiographical, functional and clinical outcome of C2-fractures. It significantly adds to the understanding of C2-fractures.
Electronic supplementary material
The online version of this article (doi:10.1007/s00586-009-0901-4) contains supplementary material, which is available to authorized users.
Keywords: Cervical spine, Atlantoaxial motion, C2-fracture, Clinical outcome, Functional outcome
Introduction
The ideal treatment of odontoid and other C2-fractures remains controversial. The lack of a comprehensive treatment-oriented classification of C2-fractures, that guides when to operate and when to select conservative treatment, reflects the fact that there exists no ideal solution for the clinical problem, yet [56]. In contrast, there is a large body of literature concerning techniques, indications and union rates in C2-fractures [72], but data regarding the most important outcome measure, the functional and clinical outcome, are scant [24, 68]. Currently, in addition to nonsurgical treatment including semirigid collars or the Halo-thoracic-vest (HTV), contemporary surgical techniques for the treatment of C2-fractures include anterior odontoid screw fixation (AOSF) [2, 62], posterior and anterior transarticular screw fixation C1–2 [51], C1-lateral mass and C2-Isthmus/lamina fixation [32] and plated anterior discectomy and fusion for the unstable Hangman’s fracture (Hmfx) [46, 83]. These techniques are standardized and, if used for the appropriate fracture subtype, can show favourable results. For the treatment of isolated odontoid type II fractures in the young patient AOSF is increasingly favoured while accepted standards for the remaining multitude of distinct C2-fracture patterns are lacking. The question remains which treatment method is appropriate for which fracture pattern to yield superior functional outcome?
In addition to the interest in outcomes concerning pain and well-being, the treatment of C2-fractures is also to be discussed with regard to the impact on the resulting posttreatment function and atlantoaxial motion. Any C2-fracture affects at least theoretically the ability of the C1–2 complex to take the major part in total neck rotation. Using functional CT-scans in 14 patients, Jeanneret [39] showed that the range of motion (ROM) for the rotation C1–2 (RotC1–2) was significantly reduced even after anatomical reduction of odontoid fractures with AOSF. Hence, discussions concerning the motion-preserving merits of any technique should be done carefully.
Therefore, the authors intended to add objective outcome data in the C2-fracture research evaluating clinical and functional long-term results after non-surgical or surgical treatment of C2-fractures on a homogenous sample of neurologically intact patients. For a detailed insight into functional outcome, validated generic and disease specific outcome measures and the use of functional CT-scanning for the assessment of the ROTC1–2 were indicated. In this context, the malunion rates were also assessed. Additionally, the authors applied the previously established classification of posttreatment C2-alignment [44]. The scoring system enables correlative analysis of posttreatment C2-alignment, ROTC1–2 and clinical outcome measures.
This study was undertaken to: (1) assess the interdependencies between posttreatment C2-alignment and the range of ROTC1–2, (2) assess the impact of fracture pattern, C2-alignment and ROTC1–2 on the clinical outcome in terms of validated measures, (3) identify risk factors for poor outcome. With the use of objective outcome measures applied on a homogenous group of patients with C2-fractures, the current study is unique in the cervical spine trauma literature.
Materials and methods
Patient sample
We reviewed all charts of patients treated for cervical spine injuries at the authors’ institution between 1997 and 2007. Patients’ demographics including injury type description were recorded. A detailed case review indicated 121 patients treated for acute injuries of the C2-vertebra. For the purpose of reconstructing a strongly homogenous sample patients had to fullfill the following criteria: (a) C2-fracture with or without stable atlas fracture treated surgically or nonsurgically, (b) age between 18 and 80 years at injury, (c) full set of injury cervical spine antero-posterior (ap) or transoral and lateral radiographs, (d) interval between injury and treatment ≤10 days, (d) understanding of author’s language, (e) minimum 6-months follow-up, (f) absence of spinal cord injury (ASIA A-D). Cases were excluded if they met the following criteria: (a) significant shoulder-girdle injury neccessitating surgery, (b) peripheral nerve injuries, (c) prohibitive medical comorbidity and endstage diseases, (d) drug or alcohol withdrawl, (e) a subaxial cervical spine injury, (f) polytrauma, (g) congenital cervical deformity, (h) injuries from neoplastic disease, infections or lesions associated with AS or DISH, (i) psychiatric illness necessitating medical treatment, (j) documented osteoporosis, (k) postoperative tracheostoma, (l) grade II or III skull–brain trauma, (m) prior medical treatment for degenerative cervical disease or trauma, (n) worker’s compensation claims, (o) fusion of C1–2.
Clinical outcome
Patients were assessed by written interview prior to follow-up and results were blinded to the authors during clinical survey. Outcome measure included the 36-item short-form health survey (SF-36) version 2, the long-term cervical spine outcome questionnaire (CSOQ) [4] and the neck pain disability index (NPDI) [77]. The questionnaires have been validated for issues related to cervical disorders [4, 23, 75] and the methods for scoring as well as the interpretation of results were illustrated in detail in previous articles [23, 38, 44, 50, 75, 77].
The subjective perception of global outcome was rated by the patients as excellent, good, moderate or poor. The participants’ satisfaction was also expressed according to distinct answers ticked within the CSOQ (No. 40–42).
The incidence of dysphagia was evaluated with the grading system of Bazaz [3]. None, mild, moderate or severe was graded by distinct combinations of difficulties with liquid and solid nutrition. Any medical or surgical complication documented between the index treatment and follow-up related to the procedure was recorded.
Radiographic analysis
Plain injury ap and lateral radiographs were available in all cases. Injury CT-scans were available in 32 patients (86%). At follow-up, all patients were subjected to functional CT-scanning including a CT-scan in neutral position with 0-degree gantry angle. The cervical spine CT-scans were performed on a 4-row helical CT scanner (Somatom Volume Zoom, Siemens) using a 14–18 cm field of interest (FOI) with 4 × 1 mm collimation and overlapping axial slice thickness of 1 mm. Sagittal and coronal reconstructions were performed using standard spine algorithms and files were stored digitally (PACS Magic View VC 42, Siemens). Digital CT measurements (0.1 mm increments) were performed on the reconstructed CT-scans in a commercially available software program (Escape Medical Viewer V3).
Classification of fractures
Radiographs and CT-scans were reviewed for fracture classification. Global radiographical assessment of fracture types was performed with differentiation into main categories, such as odontoid or Hmfx, using a descriptive taxonomy (see Table 1 in Electronic supplementary material). For the purpose of future data pooling as well as due to the lack of a single comprehensive classification including all kinds of C2-fracture patterns [47] detailed stratification of C2- and concommittant C1-injuries was done using a numerical system as templated in Electronic supplementary material Table 2. Through combinations, the numerical classification addresses all kinds of C2 and C1–2 fracture patterns. It allows for nominal statistical analysis and correlative assessment of both radiological and clinical outcome. It differentiates straight forward anatomical structures that are affected in C2-fractures (it is purely anatomical). It does not rely on fracture mechanism or morphometric measurements of displacement, but embodies the hierarchy of damage within the C2-vertebra and in particular articulating surfaces. Interpretation of the inherent stability of the various fractures is not different to accepted definitions [56] e.g., qualifiers of instability like discoligamentous injury C2–3, axial osseo-ligamentous distraction of C2, rupture of transverse ligament of C1, burst fracture of C2 or displaced odontoid fracture.
Assessment of lateral atlantoaxial joint degeneration
On injury-ap radiographs or CT-scans degenerative changes at the lateral C1–2 joints were assessed. Grading of degeneration of the lateral atlantoaxial joints (AAJ) was performed in two types of atlantoaxial osteoarthritis (AAOA) as previously elaborated [44]. Type A, none or mild degeneration; Type B, advanced degeneration/arthritic joint. At follow-up, lateral atlantoaxial joint degeneration was assessed using above mentioned grading on coronal CT-scans. In addition, the left and right atlantoaxial joint hights (lAAJH and rAAJH) were measured on injury CT-scans, if available, and on all follow-up CT-scans at the center of the lateral C1–2 joints as described [44]. For the purpose of comparative studies, AAJ degeneration was assessed using the classification of Lakshmanan [54] too.
Assessment of fusion and posttreatment C2-alignment
At final follow-up, reconstructed sagittal and coronal CT-scans in neutral head position were assessed for osseus union by three of the authors. Fusion was present if bridging trabeculae were confirmed at least on one of the cortices in both the sagittal and lateral plane by all observers.
With the same CT-reconstructions, assessment of C2-alignment was performed using the classification for posttraumatic C2-alignment (CPA-C2) [44]. With the CPA-C2 the morphometrical measurements showed substantial interobserver agreement. Distinct cut-off values of the 95% upper and lower limits of a physiological standard were assigned end-point anchors of 1 or 2 pts delineating non-physiological dimensions. The final grading of the C2-aligment into normal, mild, moderate and severe malalignment based on the summed points [44].
Functional computerized tomography
Apart clinical examination by the author all patients were subjected to functional computerized tomography. The assessment of ROTC1–2 was performed using functional CT-scans in supine position. A reduced radiation exposure with low energy beam was selected with settings of 120 kv and 80 mA sufficient to delineate bony landmarks, joint configurations and fusion.
Because subaxial flexion or extension influences the rotational capacity at the C1–2 joints and total neck rotation, meticulous care was given to level the patients’ cervical spine in neutral sagittal alignment. The subject’s body was kept in the same supine position for all head rotation sequences. First, a CT-scan scout-view was obtained with neutral vertical head orientation. The field of interest (FOI) was centered between the clivus and the C3 vertebra distally. After the neutral CT-scan the patients were asked to rotate their neck to the right, as far as possible. CT-scans were completed following adjustments of the FOI for axial slice reconstructions in the plane of the approximately 20° inclined atlas vertebra. Finally, the procedure was repeated for the assessment of left-sided rotation. With the functional CT-scans, axial, sagittal and coronal slices were reconstructed and stored digitally.
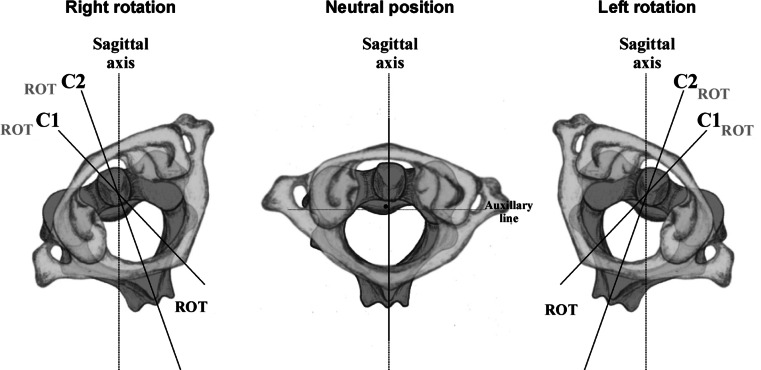
To investigate the ROTC1–2, adjacent motion at the C0–C1 joints (ROTC0–1), total neck rotation (ROTC0) and subaxial rotation (ROTC2) computer measurements on the axial slices were as follows (Fig. 1): in each head position the occipital midline indicated maximum head rotation (ROTC0) delineating the ability of the total cervical spine to rotate to either side. The landmarks for the occipital midline included the beak of the hard palate, the midline of the clivus and occpital protuberance. Next, the mid-sagittal line of C1, that is a line connecting the anterior atlas tubercle with the middle of the posterior atlas arch, was drawn. Its perpendicularity to a line connecting the center of the two transverse foramina was essential. The mid-sagittal line of C1 was calculated to the vertical axis delineating maximum atlas rotation to either side (ROTC1). Similarly, rotation of C2 was assessed drawing a mid-sagittal line of C2, that is a line perpendicular to the posterior cortical wall of the C2-vertebral body at its most caudad level. If the C2-vertebral body was affected by fracture trace up to the mid-sagittal plane, then the mid-sagittal axis of C2 was the line joining the slight midline anterior prominence on the C2-body and the cleft of the bifid spine or the perpendicular of the intertransversarium line. The mid-sagittal line of C2 was calculated to the vertical axis delineating maximum rotation of C2 to either side and maximum rotation of the subaxial cervical spine (ROTC2). Finally, left and right ROTC1–2 were calculated and expressed as the separation angle between C1 and C2, i.e., subtracting the C2 angle by the C1 angle. Similarly, the atlantooccipital rotation (ROTC0–1) was calculated subtracting the C1 by the C0 angulation. In addition, angulation C1–2 was calculated as percentage rotation C1–2 of the total neck rotation, expressed as %ROTC1–2. ROTC0 resembles total neck rotation to either side and the results were controlled for age and gender and also expressed as percentage restricted total neck rotation (%restricted neck rotation) compared to data of normals published by Castro [9].
Fig. 1.
On axial CT-scans, the angles C1° and C2° are those subtended by the respective sagittal axes of C1 and C2 against the sagittal axis at 0°. The separation angle between C1 and C2, C1–C2°, was therefore the algebraic difference between C1° and C2°. The mid-sagittal plane of C1 is defined by a line connecting the anterior and posterior atlas tubercle which is about the bisector of the line connecting both transverse foramina at their most posterior margins (auxillary line). Total rotation of the head and cervical spine are resembled by the Occ-angle in left and right rotation (not shown)
With functional CT-scanning, the left and right ROTC1–2 were classified into four types: Type 1 (no restriction), ≥30°; Type 2 (mild), 20 to <30°; Type 3 (substantial), 10 to <20°; Type 4 (severe), 0 to <10°. The worst type of restriction of ROTC1–2 (left or right) was used for statistical analysis. We determined a cut-off rendering physiological and pathological ROTC1–2 as any measure <30°, that is a deviation of approximately ±2SD from normalcy.
For the purpose of assessing changes of the instantenous center of rotation (ICR) of the C1–2 joints the authors applied a technique similar to White and Panjabi [81] on each subject (For technique and results see Electronic supplementary material).
Statistical analysis
Statistical analysis included parametric methods (independent and dependent two-sided Student t tests, Pearson’s correlation coefficient) and nonparametric tests (Kruskal–Wallis ANOVA, Mann–Whitney U test, Spearman’s correlations coefficient). Analyses of cross-tabulation tables were done using Pearson Chi-square test and Fisher’s Exact test. A P value less than 5% indicated statistical significance. All analyses were done using Statistica 6.1 (StatSoft, Tulsa, OK). Statistical analysis was performed by one of the authors (WH). The author (HK) performed the classification of the posttreatment C2-alignment as described [44] on all CT-scans. As there are currently no data on the reliability of measurements using CT-scans, the author performed the assessment of the C2-alignment with all indicated measurements on plain radiographs and on CT-scans in six patients having a healed C2-fracture. Reliability was expressed using the intraclass correlation coefficient (ICC). Interpretation of ICC was done as described [44].
Results
Patient sample and demographics
Fourty-four (36.4%) of 121 patients identified met all eligibility criteria. Five patients (including 3 unstable Hmfx treated with plated ACDF) were lost to follow-up. Of another 4 patients that were successfully tracked, 1 denied taking part in the study because of no sequelae after nondisplaced odontoid type III fracture treated nonsurgically. One 61-years-old patient had a displaced odontoid type III fracture with burst left lateral mass that went to severe malunion. She joined the follow-up but could not be included into the study because of mental retardation. She displayed restricted axial rotation in flexed position (10°–0°–5°), complained of pain during head rotation, had a cock-robin head posture and suffered from left-sided suboccipital neuralgia. Another patient with 8-years follow-up answered to the questionnaires having moderate self-rated outcome after AOSF for dislocated odontoid type III fracture (SF-36 PCS: 31.6, MCS 31.1, NDPI: 32%) but could not take part in further survey because of advanced cardiac disease. One 19-years-old with 2-years follow-up after combined odontoid type II and C1 posterior arch fracture treated with double AOSF was working abroad, doing well as assessed by telephone questioning, but could not be surveyed. Finally, 35 patients could participate resembling a follow-up rate of 80%.
Mean age at injury was 46.9 ± 21.7 years (range 17–78 years) and 52 ± 20.7 years (range 18–80 years) at follow-up. There were 12 female and 23 male patients. Follow-up was 65.4 ± 7 months on average (range 7–142 months) and mean hospital stay was 12.2 ± 9.8 days (range 1–40 days). Eleven patients (31.4%) were smokers. Except for mild skull traumas, 12 patients (34.3%) had co-morbidities and concommittant peripheral skeletal injuries (Table 3 in Electronic supplementary material). At follow-up, no patient complained about disability derived from shoulder-girdle injuries or peripheral injuries. Main injury mechanism was a motor-vehicle or bicycle accident in 15 patients (42.9%), a skiing casual in 4 (11.4%) and a fall from height in 15 (42.9%). One suffered a direct blow (2.9%). Eighteen patients (51.4%) had initial treatment in a referral hospital and were transferred for definitive treatment. Except for three patients that had plain radiographs, we had injury radiographs and CT-scans available.
Treatment
Twenty-three patients (65.7%) were subjected to nonsurgical treatment: 11 patients (31.4%) had HTV treatment and 12 (34.3%) had a Philadelphia collar. Twelve patients (34.3%) had anterior surgical treatment using AOSF and 1 patient had secondary anterior buttress-plating at C2 for redislocation of her odontoid type III fracture. Mean time to index surgery was 2.5 days (range 0–10 days). Patients’ characteristics are summarized in Table 1 in Electronic supplementary material.
Radiographic results
Fracture pattern
Twenty-three patients (65.7%) had 2-part-fractures, 11 (31.4%) had 3-part-fractures and 1 (2.9%) had a 4-part-fracture. There were 24 fractures (68.6%) involving the odontoid that could be classified into 12 (50%) type II fractures (including IIa) and 12 (50%) type III fractures according to the Anderson classification. Eighteen patients (51.4%) had a fracture pattern involving the vertebral body. Seven patients (20%), out of a total of 8 with an atypical Hmfx, had a vertebral body fracture separating the posterior axis wall [45, 46]. In 11 patients (31.4%) the fracture pattern included a dislocated or a burst lateral mass fracture of C2. At all, 19 patients (54.3%) had an intraarticular fracture pattern resembling an involvement of the lateral mass and its articular surface inside or outside the weight-bearing zone, displaced or non-displaced.
Out of 35 patients, 7 (20%) had a concomittant C1 fracture. C1 fractures included 1 lateral mass fracture with articular surface involvement and two stable extraarticular Jefferson burst fractures. Follow-up CT-scans showed that 31 fractures (88.6%) of C2 (and all fractures of C1) went on to union, in 4 cases (11.4%) a nonunion developed. Nonunion was mobile in 2 (50%) patients, showing a tight fibrous-stable nonunion in the remaining 2 (50%). Stability was established on flexion-extension films at follow-up. Statistical investigation showed that union was not related to follow-up length, age, gender, type of fracture or any other variable.
Atlantoaxial joints
At injury 7 patients had a left-sided AAJ configuration of Type B and 5 of these had also a right-sided Type B. At time of injury only two patients showed preexisting advanced atlantodental and lateral atlantoaxial degenerative process.
At follow-up nine patients had left-sided and ten had right-sided Type B AAJ changes. Seven patients (20%) had a new onset AAOA of Type B.
According to the classification of Lakshamanan [54] AAOA was a mean of 1.1 ± 1.0 points (range 0–3) left and 1.0 ± 1.0 points (range 0–3) right at follow-up. Injury AAJH was assessable in 16 patients (45.7%). LAAJH was a mean of 2.9 ± 0.7 mm (range 1.6–4 mm) and rAAJH was 3.1 ± 0.8 mm (range 1.6–4.5 mm). At follow-up lAAJH was a mean of 2.9 ± 0.8 mm (range 1–4.4 mm) and rAAJH was 3.1 ± 0.7 mm (range 1.5–4.3 mm). Unlike in normals [44] left- and right-sided AAJH at follow-up did not correlate with patients’ age (P = 0.05, P = 1.0). There was a significant difference regarding the incidence of left- and right-sided AAOA of Type A and of Type B between time of injury and follow-up (P = 0.0001 and P = 0.0008, two-tailed test). LAAJH and rAAJH were significantly reduced (P = 0.0007, P < 0.0001) in patients that had AAOA of Type B (left Ø2.0 mm, right Ø2.2 mm) compared to patients that had AAOA of Type A (left Ø3.1 mm, right Ø3.4 mm).
Functional outcome
The results of the functional CT-scans are illustrated in Table 1 and compared to data derived from normals. An illustrative case is given in Fig. 2. The interdependencies of the cervical rotation angles are ranked in Table 2. Patients displayed an increased total neck rotation (ROTC0) in the presence of increased subaxial rotational capacity (ROTC2). As expected, total neck rotation was further increased if the C1–2 joints (ROTC1–2) could substantially contribute to overall neck rotation. Likewise, with increasing ROTC1–2, the %ROTC1–2 of total neck rotation increased significantly too. On the contrary, ROTC1–2 did not correlate with subaxial rotation (%ROTC1–2 had strong inverse correlation with the subaxial rotation (ROTC2) because of the definition of %ROTC1–2). In case of decreased atlantoaxial rotation the subaxial spine tended towards compensational rotation not reaching significance: In patients with no subaxial degenerative changes we observed a trend of the subaxial spine to compensate for a lack of ROTC1–2 but a reduced ROTC1–2 could not be fully compensated by subaxial or atlantooccipital rotational efforts.
Table 1.
Physiological and pathological ranges of CT- and MRI-based atlantoaxial, subaxial and total neck rotation (in degrees)
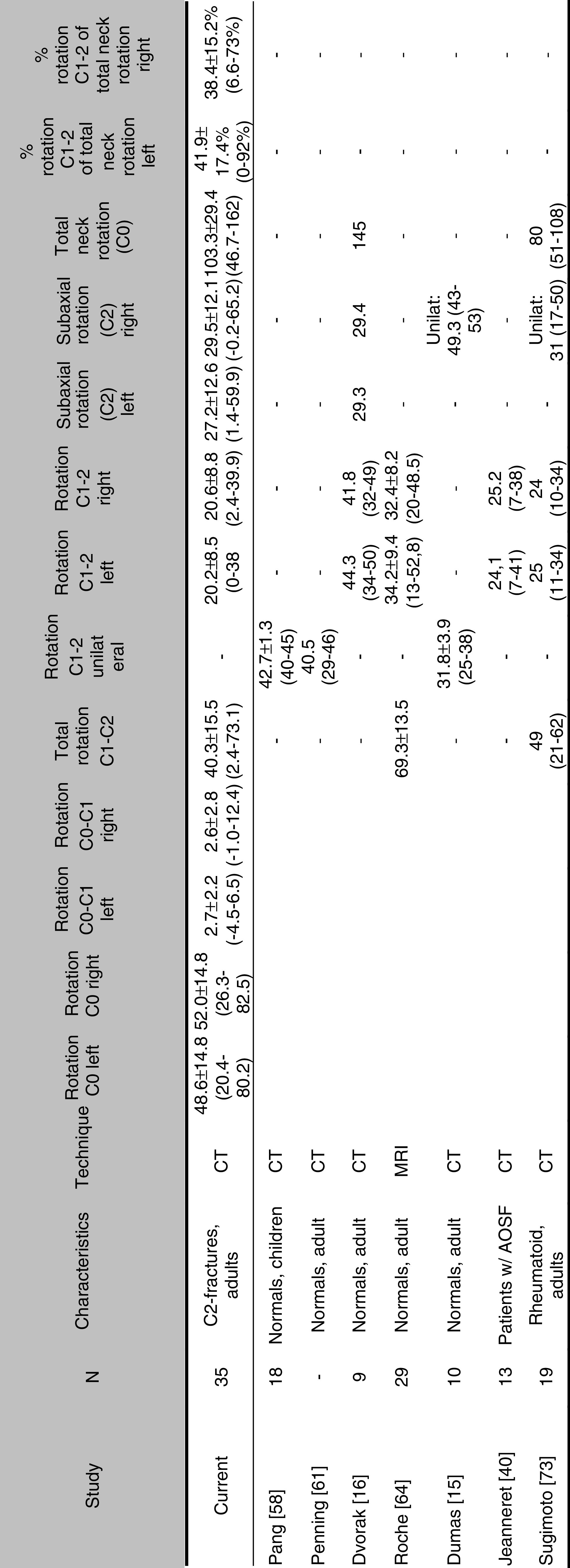
Current results and comparison with literature
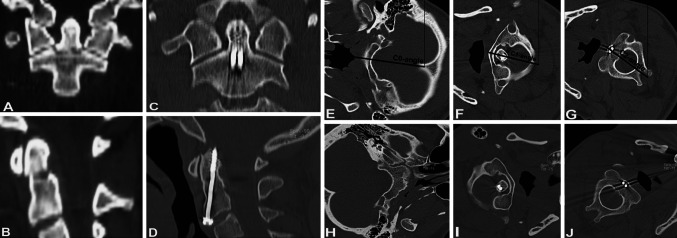
Fig. 2.
Patient with non-displaced odontoid type III fracture. Injury CT-scans depict transverse fracture course both in coronar and sagittal plane and treatment was with double AOSF. Eight years follow-up revealed solid union. Dynamic CT-scan in right head rotation showed C0-angle of 82.5°, C1-angle of 78.8° and C2-angle of 51.4° resembling an atlantoaxial separation angle of 27.4°. Accordingly, C1–2 rotation accounted for 33.2% of total head rotation. Patient had no malalignment and excellent self-rated clinical outcome. The atlantoaxial joints were unremarkable and congruent
Table 2.
Results of statistical correlations for cervical rotation
| Variables | Spearman R | P |
|---|---|---|
| Left-sided rotation | ||
| C0 and C1 | 0.99 | <0.0001 |
| C0 and C2 | 0.82 | <0.0001 |
| C0 and C1–2 (%) | NS | |
| C0 and C1–2 | 0.61 | 0.0001 |
| C1 and C2 | 0.82 | <0.0001 |
| C1 and C1–2 | 0.63 | <0.0001 |
| C2 and C1–2 | NS | NS |
| C2 and C1–2 (%) | −0.68 | <0.0001 |
| C1–2 and C1–2 (%) | 0.58 | 0.0004 |
| Right-sided rotation | ||
| C0 and C1 | 0.98 | <0.0001 |
| C0 and C2 | 0.76 | <0.0001 |
| C0 and C1–2% | 0.65 | 0.00004 |
| C0 and C1–2 | 0.60 | 0.0002 |
| C1 and C2 | 0.80 | <0.0001 |
| C1 and C1–2 | 0.57 | 0.0004 |
| C2 and C1–2 | NS | NS |
| C2 and C1–2 (%) | −0.69 | <0.0001 |
| C1–2 and C1–2 (%) | 0.65 | <0.0001 |
| Left/right rotation | ||
| C1–2 L and C1–2 R | 0.65 | <0.0001 |
| C0 L and C0 R | 0.84 | <0.0001 |
| C1 L and C1 R | 0.89 | <0.0001 |
| C2 R and C2 L | 0.79 | <0.0001 |
| C1–2 (%) L and C1–2 (%) R | 0.61 | 0.0001 |
| Total rotation C1–2 and total neck rotation | 0.63 | <0.0001 |
| Total rotation C1–2 and C1–2 (%) rotation | 0.58 | <0.0001 |
| Total rotation C1–2 and % restriction in comparison to total neck rotation in normals (Castro) | 0.57 | 0.001 |
Our analysis showed a significant difference between left and right ROTC0 (P = 0.01), ROTC1 (P = 0.002) and ROTC2 (P = 0.007) with the higher rotational ability to the right for all measurements. But the differences were small (3°–4°) and there was no significant difference between left and right %ROTC1–2 or between left- and right-sided ROTC1–2. A unilaterally restricted ROTC1–2 was not compensated for by a substantially increased contralateral rotation. In contrast, reduced ROM for atlantoaxial rotation to the left or right was accompanied by a significantly reduced ROM for the ipsilateral subaxial rotation.
Out of 35 patients 4 (11.4%) were identified having ROTC1–2 according to Type 1, 6 patients (17.1%) Type 2, 20 patients (57.1%) Type 3 and 5 patients (14.3%) Type 4. Thus, more than 70% had substantial (<20°) or severe (<10°) restriction of ROTC1–2 at least to one side. The different types of rotational restriction and the definition of total neck rotation with a cut-off of 30° had no impact on the clinical outcome measures.
We calculated the rotation against age and encountered a significant inverse correlation (Table 3). It was strong for total neck rotation (ROTC0) and subaxial rotation (ROTC2) but weak for ROTC1–2.
Table 3.
Results of statistical analysis concerning interdependencies of age and cervical rotation
| Variables | Spearman R | P |
|---|---|---|
| Age and rot C0 left | −0.76 | <0.0001 |
| Age and rot C1 left | −0.77 | <0.0001 |
| Age and rot C2 left | −0.57 | <0.0001 |
| Age and rot C1–2 left | −0.52 | 0.001 |
| Age and rot C0 right | −0.76 | <0.0001 |
| Age and rot C1 right | −0.75 | <0.0001 |
| Age and rot C2 right | −0.51 | <0.0001 |
| Age and rot C1–2 right | −0.49 | 0.003 |
Calculated separately for isolated odontoid fractures we observed a total ROTC1–2 of 36° on average and a mean total neck rotation of 96°.
Posttreatment C2-alignment
The first author performed all measurements. The analysis of intraobserver reliability demonstrated good to excellent agreement between radiographic and CT-based measurements with intraclass coefficients of >0.6 for all measurements applied. There were no measurements performed that were classified as ‘pathological’ but otherwise were within normalcy on CT-scans, et vice versa.
According to the author’s classification and grading of morphometrical alignment [44] after treatment of C2-fractures, mean malunion score was 2.8 ± 2.5 points (range 0–11points). According to the classification [44], in 5 patients (14.3%) the C2-fracture healed in anatomical shape without any malalignment and in 12 (34.3%) with mild malalignment. Twelve fractures (34.3%) healed with moderate and 6 (17.1%) with severe malalignment. At all, the C1–2 complex showed moderate or severe malalignment in 18 fractures (51.4%). Statistical analysis revealed a significantly reduced ROTC1–2 in patients with the higher malunion score (P = 0.01) and in those classified with a ‘moderate’ or ‘severe malalignment’ (P = 0.01). Accordingly, patients with higher malunion score had a higher grade of rotational restriction (Types 1–4, P = 0.02). In addition, it striked that patients with higher malunion scores (ANOVA) and moderate/severe malalignment showed a significantly reduced clinical outcome in terms of SF-36 MCS (P = 0.02 and P = 0.001), NPDI (P < 0.0001 and P < 0.00001), CSOQ-neck pain severity composite score (P < 0.005 and P < 0.0001), CSOQ-functional disability score (p < .0002 and P < 0.00001), CSOQ-psychological distress score (P = 0.04 and P = 0.03), physical symptoms score (P = 0.004 and P = 0.0002) and CSOQ-health care utilization score (P = 0.036 and P = 0.036).
Clinical outcome
Means, SD, and ranges of outcome measures are illustrated in Tables 4 and 5. Data are presented in comparison to results of other studies.
Table 4.
Clinical outcome following treatment of C2-fractures
| Study | FU (mo) | n | NPDI (%) | CSOQ | SF-36 | NASSa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Composite neck pain severity score | Composite shoulder/arm pain severity score | Functional disability score | Psychological distress score | Physical symptoms score | Healthcare utilization score | Physical component summary score | Mental component summary score | |||||
| Current, C2-fractures | 65 | 34 | 20.4 ± 20.4 (0−73.3) | 23.7 ± 21.3 (0−76.6) | 17.2 ± 21.6 (0–73.7) | 14.6 ± 16.5 (0–57.2) | 29.7 ± 23.7 (0–83.3) | 32.4 ± 28.8 (0–85.7) | 15.7 ± 21.6 (0–60) | 47.0 ± 11.5 (21.3–60.2) | 46.0 ± 12.89 15.9–62.3 | – |
| Koller [50], ACDFP C3–T1 | 62 | 26 | 12.4 ± 12.7 (0–40) | 15.6 ± 14.0 (0–40) | 15.0 ± 13.5 (0–33.3) | 8.1 ± 12.2 (0–28.6) | 19.0 ± 17.8 (0–50) | 26.6 ± 21.5 (0–66.7) | 9.2 ± 15.2 (0–40) | 47.0 ± 9.8 (18.2–59.3) | 52.2 ± 12.4 (14.6–75.3) | – |
| Dvorak [18] Jefferson burst fractures | 75 | 34 | – | – | – | – | – | – | – | 43.3 ± 13.4 | 49.1 ± 14.2 | 76.7 ± 21.5 |
| Kwon [53] ACDFP C3–T1 | 12 | 20 | – | – | – | – | – | – | – | 46.8 ± 3.1 | 52.3 ± 2.2 | 85.8 ± 8 |
| Kwon [43, 53, 68] posterior instrumented fusion | 12 | 22 | – | – | – | – | – | – | – | 46.9 ± 2.0 | 49.3 ± 2.3 | 81.7 ± 3.5 |
| Dvorak [17, 47] surgically treated facet fractures w or w/o dislocation | 28 | 72 | – | – | – | – | – | – | – | 49.5 ± 9.9 | – | 85 ± 18.5 |
| Dvorak [17] non-surgically treated facet fractures w/o dislocation | 35 | 18 | – | – | – | – | – | – | – | 47.8 ± 11.3 | – | 84.3 ± 15.8 |
| Normative values [17] | – | – | – | – | – | – | – | – | – | 50.5 ± 9.0 | 51.7 ± 9.1 | 89.1 ± 15.5 |
Comparison with results of literature concerning traumatic injuries C1 to T1 in neurological intact patients
aAmerican Academy of Orthopedic Surgeons/North American Spine Society outcome instrument
Table 5.
Results of the SF-36-v2 (transformed scores) in patients with C2-fractures and comparison with results of strictly homogenous groups of patients with subaxial cervical spine instabilities and thoracolumbar burst fractures
| SF-36 subscales | C2-fractures, current study (n = 35) | Nonsurgical treatment for burst fractures T11-L4 (n = 21) [50] | ACDFP for subaxial injuries (n = 26) [50] |
|---|---|---|---|
| Physical functioning | 76.5 | 74.5 | 77.3 |
| Social functioning | 81.6 | 87.5 | 88.5 |
| Role physical | 63.2 | 67.9 | 72.4 |
| Role-emotionial | 67.4 | 79.8 | 85.3 |
| Mental health | 70.5 | 71.9 | 77.1 |
| Vitality | 58.1 | 61.0 | 63.2 |
| Bodily pain | 62.4 | 67.9 | 72.3 |
| General health | 69.6 | 67.9 | 67.9 |
The outcome measures and questionnaires utilized showed good consistency when assessing differences in clinical outcome. Assessment of clinical outcomes with the validated measures (SF-36, NPDI, CSFQ) and their correlation with the patient’s self-rated clinical outcome (‘excellent’ to ‘poor’) showed strong consistency (Kruskal–Wallis testing: P = 0.03 to P = 0.003). There were significant differences within the validated measures if calculated for the 4 groups of global outcome: ‘excellent’, ‘good’, ‘moderate’ and ‘poor’ (Table 4 in Electronic supplementary material). There was also a significant correlation between the validated outcome measures and inbetween the various scoring items of the queries (Table 5 in Electronic supplementary material).
Self-rated outcome was judged excellent by 15 patients (44.1%), good by 7 (20.6%), moderate by 10 (28.6%) and poor by 2 patients (5.9%). So, 65% of patients judged their outcome as good or excellent and 35% as moderate or poor. With the worse self-rated outcome patients displayed a significantly reduced total ROTC1–2 rotation (P = 0.02) and total neck rotation (P = 0.05). Likewise, reduced total ROTC1–2 showed slight correlation with decreased outcome measures yielding significance for the SF-36 PCS (R = 0.36, P = 0.04), the NPDI (R = −0.34, P = 0.05) and the CSOQ-shoulder pain severity composite score (R = −0.44, P = 0.01). Patients with reduced total neck rotation had decreased outcomes yielding stronger significance for the SF-36 PCS (R = 0.53, P = 0.002), the NPDI (R = −0.37, P = 0.04) and the CSOQ-shoulder pain severity composite score (R = −0.45, P = 0.01). When calculating the age and gender matched percentage restriction of total neck rotation [9] against the clinical outcome measures, correlations existed for the SF-36 PCS (R = 0.54, P = 0.001), the NPDI (R = −0.38, P = 0.03), the CSOQ-shoulder pain severity composite score (R = −0.45, P = 0.007), the CSOQ-neck pain severity composite score (R = −0.39, P = 0.02) and the CSOQ-functional disability score (R = −0.35, P = 0.04). Summarizing, reduced clinical outcome was more reflected by a decreased total neck rotation rather than a reduced C1–2 rotation.
As it was with the ability to rotate the neck, statistical analysis revealed a decreased clinical outcome for elderly patients in terms of the NPDI (R = 0.41, P = 0.02) and the SF-36 PCS (R = −0.56, P = 0.001). Older patients had higher health care utilization demands in terms of the CSOQ (R = 0.36, P = 0.04). Elderly patients had a significantly shorter follow-up period (R = −0.45, P = 0.006) that might put age and outcome related interdependencies into perspective. It is of note that patients with worse outcomes had reduced total neck rotation, however, the %ROTC1–2 did not correlate with the clinical outcome reflecting that a reduced absolute rotational ability affecting the whole cervical spine was a factor of aging, motion induced pain and a low functional outcome.
Significant gender-related differences existed in terms of the NPDI (P = 0.03), the CSOQ-psychiological distress score (P = 0.005) and the physical symptoms score (P = 0.01). These results have to be interpreted with the awareness of gender distribution with varying fracture patterns and ages. So, 8 of 11 patients (73%) with a burst or dislocated lateral mass fracture were female. Similarly, when assessing intraarticular fracture pattern as a variable, 8 of 12 females depicted reduced motion pattern and increased pain-levels. Neither the presence of a nonunion nor combined C1–2 fractures, nor any complication or whether surgery was performed or not had impact on clinical outcome or cervical rotation (Table 3).
Notably, the number of main fragments identified (2-part, 3-part, 4-part-fractures of C2) had significant impact on the %ROTC1–2 (P = 0.03) but not on the clinical outcome measures. If the smallest denominator was assumed to be an intraarticular fracture pattern involving the C2-superior articulating facets then patients had significantly reduced total ROTC1–2 (P = 0.03) and in particular reduced %ROTC1–2 (P = 0.006). Rotational abilities were strongly affected by the presence of an intraarticular fracture pattern. Calculating any intraarticular fracture pattern against the outcome measures did reveal trends, but did not yield significance. In this context it is of note that only 11 patients were identified to have had a dislocated fracture or burst pattern involving the articular pillar and lateral mass. If calculating rotation and clinical outcome against the presence of a burst or dislocated lateral mass fracture in eight patients at all, the statistical analysis still revealed a trend for reduced %ROTC1–2, but it striked that this group of patients had significantly reduced outcomes in terms of the SF-36 MCS (P = 0.006), the NDPI (P = 0.04), the CSOQ-functional disability score (P = 0.01) and the CSOQ-physical symptoms score (P = 0.01). SF-36 PCS scores did not reach statistical significance but a strong trend existed (SF-36 PCS Ø35.7 ± 9.0 vs. Ø43.0 ± 10.2). Differences of 2.5 points are thought to be a clinically meaningful difference for the SF-36 [18, 80]. Patients that had the vertebral body affected (51%) had reduced total ROTC1–2 (P = 0.02), but %ROTC1–2 and total neck rotation were not significantly reduced. However, these patients had worst scores with the CSOQ-functional disability score (P = 0.007) and the SF-36 MCS (P = 0.05). This group of patients included most of the dislocated burst lateral mass fractures, patients with intraarticular fractures and the group with highest malunion scores.
Clinical survey
Eleven patients (31.4%) had at least one lateral AAJ of Type B and 6 of these 11 (54.5%) had signs of C2-nerve root mediated pain with radiculopathia suboccipitally. At all, 20 patients (57.1%) reported on pain when approaching the mid-range or extremes of axial head rotation in neutral or sagittally flexed head position or reported on tenderness and localized pain at the C2-spinous process during daily activities. According to distinct questions within the CSOQ 20% of patients reported that they would need additional treatment for their neck condition in the future. Sixty-one percent of patients judged they would be extremly or moderately satisfied if their neck condition would be the same as at follow-up, while 20% judged they would be moderate or extremely dissatisfied if the neck condition would remain the same (20% ticked ‘neither satisfied nor dissatisfied’). Twenty-three percent reported that the actual result was somewhat or much worse as expected, 49% reported it was somewhat or much better than expected, and 28% as expected.
AAOA
Concerning AAOA, the presence of Type B changes at follow-up had significant impact on the rotational ability and outcome measures. Type B patients displayed significantly decreased total ROTC1–2 (P = 0.006) and %ROTC1–2 (P = 0.04) but not significantly reduced total neck rotation. Clinical outcomes were worse than in patients with Type A changes in terms of the SF-36 PCS (P = 0.01), the SF-36 MCS (P = 0.01), the NPDI (P = 0.002), the CSOQ-psychological distress score (P = 0.0005), the CSOQ-physical symptoms score (P = 0.01) and health care utilization score (P = 0.02). The same interdependencies existed even more in patients that had newly developed Type B changes with a significantly decreased total ROTC1–2 (P = 0.01) and %ROTC1–2 (P = 0.02) as well as reduced outcome measures in terms of SF-36 MCS (P = 0.0009), NPDI (P = 0.003), the CSOQ-neck pain severity composite score (P = 0.04), CSOQ-functional disability score (P = 0.02), CSOQ-psychologic distress score (P = 0.0009), CSOQ-physical symptoms score (P = 0.04) and CSOQ-health care utilization score (P = 0.006). Patients that had preexisting AAOA of Type B, that had just progressed, had significantly reduced left and right AAJH (P = 0.04 and P = 0.03) as compared to Type A patients, but clinical outcome measures were not different (Table 4).
Fracture of the C2 articular pillar
In 8 of 11 patients (72.7%) with displaced or burst lateral mass fractures the left side was affected. At follow-up, these patients had significantly reduced left-sided AAJH (P = 0.02). With increasing malunion score, ROTC1–2 was significantly reduced, the most on the left side (P = 0.0005). When calculating for the intraarticular fracture pattern that affected the left side in 11 of 19 patients (58%) it also striked that left-sided %ROTC1–2 (P = 0.005) and left-sided ROTC1–2 (P = 0.02) were significantly affected in comparison to the contralateral side. The findings of left-sided preponderance were incidental, but substantiated that the intraarticular and particularly burst fracture patterns show their main adverse effects on the development of ipsilateral AAOA, reduced total ROTC1–2 and %ROTC1–2 and C2-malunion scores. The latter had the largest impact on clinical outcome measures.
Work status
Fourteen patients (40%) were already retired at time of injury unrelated to disorders of the neck. Of 21 patients occupied at time of injury 15 achieved a level of W1 (42.9%) according to Denis’ Work Scale, 1 had W2 (2.9%), 2 had W3 (5.8%) and 3 patients (85.7%) were not able to resume previous full-time employment or were unable to work because of neck related impairment. Eighteen patients (85.7%) went back to a full-time employment with a mean time out of work of 17.0 ± 6.8 weeks (range 3–24 weeks) after injury.
Complications
With the dysphagia grading system of Bazaz [3] the mean score was 1.4 ± 0.7 (range 0–3) for liquids and 1.7 ± 1.0 (range 1–4) for solid nutrition. Buzz-scores were not significantly affected by anterior surgery.
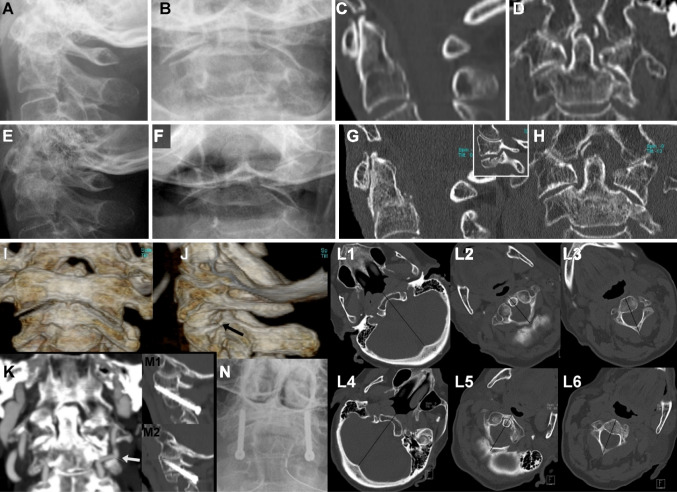
In summary, 7 out of 35 patients (20%) sustained a complication: 1 (2.9%) with odontoid type II fracture had delayed-union in the HTV but eventually fused after 6 months. Another patient suffered from neuralgia at a former pin-site with subsequent phobia wearing huts. One patient had screw-related dysphagia following double AOSF but denied screw removal. Another had hard-to-treat C2-referred pain lasting for 8 months after nonsurgical treatment of an odontoid type III fracture with split-impression fracture of the lateral mass. Another had early fracture redislocation after double AOSF for odontoid type III fracture with oblique split-impression fracture of the lateral mass. The fracture healed uneventful. One female patient with 10 years follow-up had HTV treatment for a displaced odontoid type III fracture with en bloc fracture-separation of the comminuted lateral mass. Symptomatic nonunion with severe malalignment developed and the patient was subjected to anterior retropharyngeal release with reduction and C2-buttress-plating 6 months after the index treatment. Implant removal was performed 1.5 years after index therapy. After 3 years the patient showed up reporting a progression of myelopathic signs during a 4-weeks period which was found to be related to anterior subluxation of C1 on C2. The patient denied a second trauma. Intraoperatively, there was no significant sagittal motion C1–C2. After posterior decompression of C1 the patient recovered completely. Finally, during survey of our patients a 76-year old was subjected to C1–2 Magerl fixation for painful C1–2 joint destruction (Fig. 3). The patient achieved immediate pain resolution after immobilization of the C1–2 joints.
Fig. 3.
Seventy-five-years-old patient had suffered a low-height fall. Injury radiographs (a, b) and CT-scans (c, d) displayed an anteriorly displaced odontoid type III fracture with comminuted (impression/depression) fracture of the left lateral mass. Patient was treated with Philadelphia collar. At 6-months follow-up, radiographs (e, f) and CT-scans revealed malunion of C2 with anterior displacement of the odontoid/vertebral body fragment, relative stenosis C1–2, deformed left atlantoaxial joint. Rotation C1–2 was painful and restricted due to bony deformation of the articular surface (j). Left-sided rotation was 9.1° and right-sided was 13.8°. Patient had motion induced pain and vertigo which was recognized to be a sequelae of dynamic vertebral artery stenosis (k). Patient underwent posterior fixation C1–2 (M1 + 2, N) and she immediatedly gained complete pain resolution
Discussion
The current study is a unique approach to the outcome investigation of C2-fractures, and it is the largest reporting of functional CT-scanning in patients with cervical trauma. The author identified several articles [47, 49, 68] reporting on miscellaneous C2-fractures included into cross-sectional outcome analysis or using nonvalidated instruments; most studies are reluctant to further delineate distinct fracture morphology and outcome variables in heterogenous samples [5, 25–27, 29, 62, 68]. Therefore, we intended to seek objective outcome data through assessment of validated outcome measures, functional outcome using dynamic CT-scanning, a detailed classification of fracture pattern and an analysis of posttreatment C2-alignment using a classification system based on valid measurements [44]. The efforts are indicated as there is no consensus on the ideal treatment for all subtypes of C2-fractures [2, 29, 43, 46, 62].
Our study yielded for a homogenous sample. We assessed different fractures (odontoid, vertebral body, Hmfx,…), but unlike prior studies with difficulties addressing all fracture patterns, the authors’ characterization of C2-fractures at injury and at follow-up implicates the focus on identical morphological characteristics within the C2-fracture subtypes. Consequently, beside general outcome analysis of C2-fractures, we sought to analyse the influence of distinct morphological subtypes (intraarticular fracture pattern, number of main fragments, burst component,…) on the remaining rotation C1–2 and the clinical outcome. We wanted to identify risk factors for poor outcome and thereby identified the severity of malunion. We aimed out being able to identify at an early stage of treatment those fractures prone to symptomatic malunion and poor outcome, thus resulting in an adaption of treatment protocols (nonsurgical vs. surgical, nonfusion vs. fusion procedure).
Malunion of C2
Rarely, the type of anatomical alignment and associated outcome after various motion-preserving treatments is reported [1, 10–12, 21, 26, 34, 41, 42, 46, 47, 57, 63, 71, 74, 78]. A meaningful number of subtypes of C2-fractures exists where complete reduction, normal C1–2 rotation and a physiological anatomy is difficult to restore [1, 10, 11, 34, 42, 43, 71, 82]. Likewise, a non-anatomical posttreatment C2-alignment, resembling a malunion, can cause significant symptoms even indicating fusion C1–2 [13, 26, 30, 42, 47, 51, 52, 67, 70, 71, 78, 79] as it had to be done in one of our cases (Fig. 3), two others being scheduled (Fig. 4). Malunion in C2-fractures can produce significant sequelae and we sought to stratify those C2-fracture subtypes prone to malunion after motion-preserving therapy: In the literature, the approximate rate of malunion in odontoid fractures was reported to be 12–22% [57, 63]. Using the classification we established in part I of the project [44] we identified 49% of patients having either no or only mild malalignment but 51% having moderate or severe malalignment of C2 or the C1–2 complex. Patients with advanced malalignment had significantly reduced ROTC1–2 and, even more important, the presence of advanced malunions had a strongly significant adverse impact on all clinical outcome measures. This study offers evidence for the correlation between a distorted posttreatment C2-alignment, including distortion of the physiologic C1–2 relationships, and worse clinical outcomes, both involving restricted ROTC1–2. Our findings substantiate previous studies that noted reduced outcomes in patients with distorted C1–2 joint configurations [19, 26]. Dvorak [18] reported on 34 Jefferson fractures and demonstrated that patients with residual lateral displacement of the lateral mass of C1 ≥ 7 mm were more likely to report worse functional status in terms of the SF-36. In another study [17] on 90 isolated subaxial facet injuries, the group of 18 patients treated nonoperatively contained the most benign fracture patterns but had significantly worse clinical outcomes (NASS, SF-36 subscales). Dvorak hypothesized that the worse outcome even after non-displaced, non-surgically treated facet fractures is due to the development of secondary degenerative changes with malalignment at the injury level. Similarly, we observed that malunion as a result of distorted C2-lateral mass, altered C2-articular surfaces, widening of the vertebral body or increased odontoid tilt caused a remarkable drop in outcome measures and ROTC1–2. We demonstrated that maintaining anatomic C2-alignment has a decisive role for clinical outcomes (Table 5).
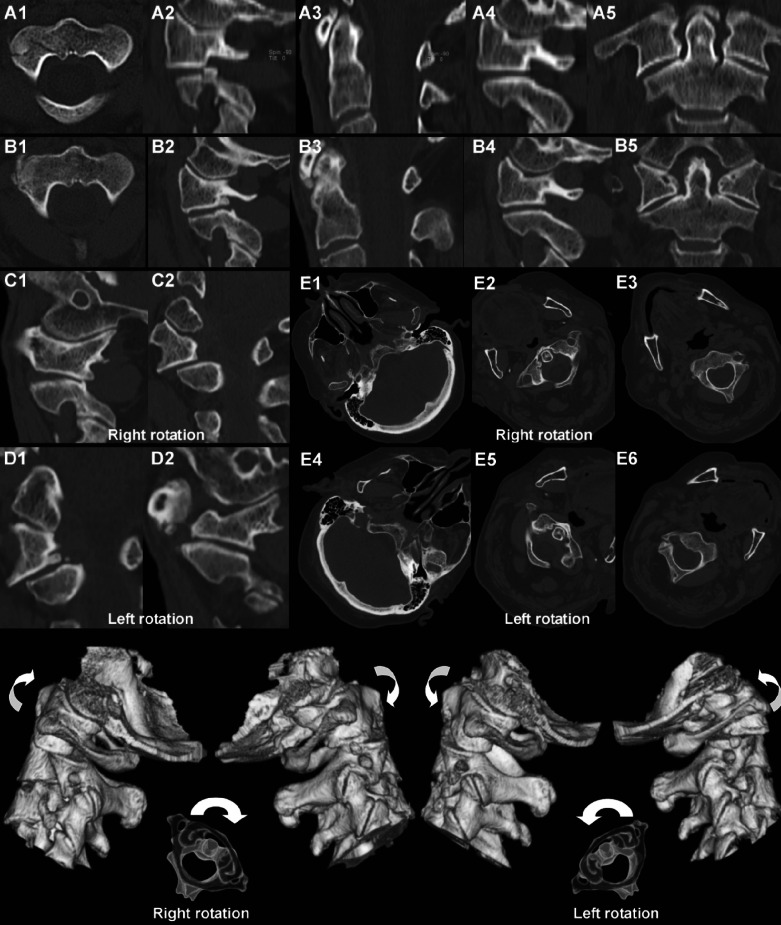
Fig. 4.
Sixty-seven-years-old patient had suffered a motor-vehicle accident. Injury CT-scans (A1–A5) revealed 3-part fracture of C2, intraarticular odontoid type III fracture and separated split-fracture of the right lateral mass. Patient was treated with Philadelphia collar. Five-year follow-up showed the patient having serious suboccipital C2-referred pain right. CT-scans in neutral position (B1–B5) show AAOA of the left C1–2 joint and vertebral widening with relative stenosis C1–2. C1 and C2 show right rotation to the right at both joints in sagittal CT-reconstruction. D1 and D2 show rotation to the left in both joints. E1–E3 and E4–E6 demonstrate the axials of the functional CT-scans in right and left neck rotation. As the lower 3D-reconstructions demonstrate, right-sided rotation C1–2 was restricted with degenerative changes restricting a full range of axial rotation C1–2. The patient was in pain and was offered C1–2 fusion but rejected surgeries
Functional outcome and atlantoaxial rotation
After motion-preserving C1-ring osteosynthesis in five Jefferson fractures, Ruf [65] reported a mean left and right ROTC1–2 of 20.6° and 18.6° using dynamic MRI-scans. The patient with worst C1–2 incongruency had the worst functional and clinical outcome which was attributed to the distorted C1-2 articular surface pattern. Jeanneret [39] measured left and right ROTC1–2 25° and 24° after AOSF using functional CT-scans. Likely due to sample size and fracture analysis, the study did not find any correlation between residual ROTC1–2 and fracture pattern, quality of reduction or osteosynthesis. We investigated the ROTC1–2 after treatment of C2-fractures. In our sample with 35 patients, only 30% had normal ROTC1–2 or mild restriction, but 70% had substantial (<20°) or severe (<10°) restriction of ROTC1–2 at least unilateral. Likewise, in Jeanneret’s sample only 38% had normal motion C1–2 and Verheggen [10] noted that only 61% of patients revealed standard rotation after AOSF. We explored the rotational interdependencies (Table 2) and observed that in case of decreased C1–2 rotation, the subaxial spine yielded for compensation, but did not reach significance and is suggested to be an effect of pain-mediated (due to malunions) overall restriction of rotation and coincident a factor of aging. Concerning age, some elderly patients showed advanced subaxial spondylosis and normally the C1–2 rotation increases compensatorically with aging [9]. Calculating the ability for neck rotation against age we observed a significant inverse correlation, pronounced for total neck rotation (ROTC0) and subaxial rotation (ROTC2). Although we expected an increased %ROTC1–2 in the elderly, the correlations were weakest for the %ROTC1–2 and ROTC1–2 rendering other factors decisive for reduced ROTC1–2 also in the elderly patients.
Concerning compensational mechanisms we observed that unilaterally restricted ROTC1–2 was not compensated for by a substantially increased contralateral rotation. In addition, reduced ROTC1–2 to one side was accompanied by a significantly reduced ipsilateral subaxial rotation.
We did not observe a significantly increased C0–1 rotation in case of reduced ROTC1–2 as it was in children with pathological stickiness C1–2 [58, 60]. We had a mean ROTC0–C1 of 2.6° and 2.7° to the right and left suggesting a normal coupling between C0 and C1 [58]. Only a few patients exhibited increased motion above 2SD but never achieved ranges of 30° as in the forementioned study. Overall, we demonstrated a significant reduction of ROTC1–2 in the C2-fractures with decreasing order in odontoid, vertebral body and atypical Hmfx, and fractures affecting the articular pillar of C2.
Like Jeanneret, we investigated the reasons for reduced ROTC1–2. While reduction of total neck rotation after the C2-fractures is assumed to be a function of pain-related restriction of overall motion [42], aging and degenerative processes, we showed the reduction of ROTC1–2 and %ROTC1–2 to be significantly associated with the degree of anatomical distortion and the severity of malunion, outperforming the statistically analysed influence of pain in terms of the outcome vehicles. Our patients had no other cervical injuries and the source of pain could be focused at C1–2. Statistically a pain-related reduction of ROTC1–2 and an associated reduction of total neck rotation existed, but the severity of malunion had the highest effect on the rotational ability of C1–2. There was a slight correlation between total ROTC1–2 and clinical outcome measures, but no correlation existed for the %ROTC1–2 and the clinical outcome. It seemed that the restriction of rotation was perceived by the patients to be an acceptable ‘price’ to pay causing less disability if they did not perceive motion induced pain. Likewise, Grob [31] reported the residual neck rotation in 35 fusions of C1–2 for AAOA with a mean of 58°. Notably, rotation was not different between the patients reporting a ‘good’ or a ‘poor’ outcome. Our current findings substantiate that loss of ROTC1–2 and total neck rotation do not cause worse outcomes.
Where has the rotation gone?
In normals the C1–2 joints are responsible for up to 60% of total neck rotation equaling 30°–45° [16, 25, 58, 64, 73]. Even though the osseus contour of the lateral C1–2 joints looks concave on radiographs, the padding of joint cartilage converts the articulating surfaces to biconvex discs [58] with the cartilage cover averaging 1.5–2 mm [48, 51]. The spaces anterior and posterior where the articular surfaces diverge are filled by intra-articular meniscoids [48]. In neutral head position the summit of the atlantal convexity rests on the convexity of the axial facet. As C1 rotates, one atlantal facet slides down the posterior slope of its axial facet, and the contralateral atlantal facet slides down the anterior slope of its facet (Fig. 4) [8]. Because of the convex shape of the articular surfaces each facet of C1 and C2 moves downwards and forwards/backwards at the same time during rotation [15, 69]. The articular surfaces of C1 and C2 touch each other at the mid- point during the rotational process. The understanding of this process is crucial for recognizing the C1–2 joints as a source of pain. Pang [58] established the blue print of normal rotation C1–2 by analysing CT-based motion curves containing three distinct phases [58, 59]: a single motion phase (C1° = 0°–23°) when only C1 turns; a double motion phase (C1° = 24°–65°) when both C1 and C2 are turning in the same direction because of ligamentous yoking; and a unison motion phase (C1° = 65°–90°) when both C1 and C2 turn as a fixed couple. The authors showed that neck rotation was initiated at the C1–2 joints and rotation of C1 occured before C2 rotated [64]. Therefore, any rotation of the head is conferred to the C1–2 facets and in the current sample with an overall reduced total ROTC1–2 of 40° the articulating surfaces of C1 and C2 must, at some point, have encountered a restraint. As Jeanneret [39], Pang [58], Ruf [65], Kim [42] and others pointed out, soft or bony interlock can have its source in malunited vertebral bodies, odontoid or lateral mass fractures, intraarticular scarring and pieces of cartilage wedged into the joint spaces, or can be a sequelae of capsular and periarticular ligamentous scarring like arthrofibrosis. We demonstrated that an altered joint anatomy of C1–2 caused reduced ROTC1–2 and %ROTC1–2, sometimes deformation being striking and the restraint of axial rotation obvious (Fig. 3j). Concerning the loss of rotation, our findings echo previous observations describing significantly reduced rotation C1–2 after prolonged immobilization, e.g., with temporary Magerl fixation [7, 71], after ligamentous and capsular injuries to the C1–2 joints [60] and after intraarticular or malunited fractures of C2 [52, 57]. In addition to articular surface deformities, distortion of the rotational axis of C1 and C2 in terms of deviated instantaneous center of rotation (ICRC1–2), e.g. as a sequelae of a widened C2-vertebral body, deformed lateral mass or tilted odontoid is thought to contribute to reduced ROTC1–2 [37]. We investigated the ICRC1–2 and observed a trend towards an anterior shift of the ICRC1–2 (Electronic supplementary material). Currently there is no definition of normal ICRC1–2 or grading of any deviation of the ICRC1–2, so observations warrant further research.
Jeanneret noted three patients with restricted ROTC1–2 and explained the decreased motion with intraarticular comminution of the C1–2 joints that was supposed to produce painful posttraumatic AAOA [39]. AAOA can disrupt the smooth, gliding joint motions [60] and a clinical hallmark of AAOA is known to be the significantly reduced ROTC1–2 [20, 31, 35, 66]. Accordingly, our patients with AAOA (preexisting and new onset Type B joints) had significantly decreased total ROTC1–2 and %ROTC1–2. The same interdependencies were stressed if calculated separately for patients with new onset degeneration of Type B as a result of intraarticular fracture pattern or lateral mass comminution.
Clinical outcome
The patient’s subjective perception of the treatment-related outcome has increasingly become the focus in spinal care. The current study is one of the first to assess clinical outcomes of fractures at C1–2 using validated outcome measures [18] applied on a sample, homogenous for the neurologically intact, with exclusion of many confounding patient based variables through hard selection process. Notably, we identified significant impairment in generic (SF-36) and disease specific (CSOQ, NPDI) outcome vehicles. The use of validated measures allowed an objective comparison of C2-fractures morphologically classified with other spinal injuries: Tables 4 and 5 illustrate that our outcome was better than reported with, e.g., Jefferson burst fractures, except for the SF-36 MCS. On the other hand in comparison to, e.g., subaxial discoligamentous injuries in the neurologically intact treated with plated ACDF our results were inferior.
For our purpose of identifying prognostic factors we investigated whether pain and disability in patients with reduced outcomes depended on (1) a restricted ability for axial rotation, (2) distortion of C1–2 anatomy and severity of malunion, or (3) intraarticular damage with subsequent degeneration and development of AAOA. The statistical analysis revealed that clinical outcome was in the majority influenced by the severity of malunion. Malunion was a frequent sequelae of intraarticular and particularly burst lateral mass fractures with subsequent evolvement of AAOA over time. At all, 65% of patients judged their outcome as good or excellent. But 35% judged their outcome as moderate or poor and 20% assumed that they would need additional treatment for their neck condition in the future. In contrast, in literature the results of various treatment modalities for C2-fractures, particularly for odontoid fractures, were frequently recognized as ‘good’ if not ‘excellent’ [25, 62, 72]. In the past, detailed data have been sparse commonly not exceeding cross-sectional assessments and despite the prevailing opinion that overall outcome was favourable, long-term analysis identified persisting symptoms of pain and stiffness in a meaningful number of patients [1, 11, 57, 76]. Platzer [62] reported on 110 patients subjected to AOSF. Outcome was 1.4 points on a ‘Smiley-Webster’ scale, judged ‘good to excellent outcome’. Astonishingly, only 14% were reported complaining about limitations in daily living, occasional or chronic pain symptoms and decrease of cervical motion. Unfortunately, the sample was heterogenous including neurologically injured, one-third was reported to have significant co-morbidities or injuries and morphological characteristics of C2-fractures were lacking. In contrast, after AOSF subjective-rated pain can be found in 10–40% [1, 11, 57, 76]. Müller [57] reported on 27 odontoid fractures subjected to AOSF. Fourty-one percent of patients demanded pain medication and 29% noted motion related pain, only 18% were completely satisfied with their outcome and 22% of fractures went on to malunion. Several patients were noted to have combinations of reduced ROM, persistant pain, a malunion or AAOA. Müller [49] stressed the importance of anatomical alignment in C2-fractures and the findings of the current study give evidence that with an increasing number of C2-fragments, deformation of the C2 vertebral body and particularly fractures of the C2 lateral mass clinical outcome drops: Fractures involving the C2 articular pillar can be isolated articular or lateral mass fractures or extensions of vertebral body fractures [5, 26] and were found to be prone to a high rate of non-anatomical union [21] frequently indicating secondary fusion of C1–2 [30, 67, 70]. Up to 50% of Hmfx involve the articular facets of C2 and in the largest sample regarding anterior fusion C2–3 for the treatment of unstable Hmfx, Koller [46] observed a decreased functional and clinical outcome with a subset of patients having reduced rotation C1–2 and motion induced C2-referred pain. Similar to our study, several of these patients showed incongruency and deformity of the C1–2 joints and a positive correlative relationship between the severity of malunion C1–2 and reduced clincial outcomes. Likewise, Fujimura et al. [26] reported on 31 C2-vertebral body fractures subjected to nonsurgical treatment including 3 burst and 17 sagittal fractures of the lateral mass. In 15 of 17 sagittal fractures malunion C1–2 was recognized at follow-up, 8 of the 17 fractures (47%) went to AAOA reporting moderate or severe nuchal pain. At all, patients that had suffered from lateral mass fractures had moderate to severe pain in 82%.
Since Jeanneret’s series, several reports substantiate that C2-fractures affecting the upper facets of C2 can show symptomatic C1–2 incongruency at follow-up [26, 40, 42, 52] and our study adds objective data delineating a significantly decreased outcome in terms of validated measures with increasing C2-malunion. Accordingly, from the current results the authors support primary fusion C1–2 in C2-fractures with comminuted or displaced C1–2 joints showing a high risk of malunion and poor outcomes.
Literature [20, 26, 31, 35, 39, 40, 52, 66] and our current results demonstrate that the C1-2 facet joints can be a meaningful source of pain. Thirty-one percent of our patients had at least one lateral C1–2 joint displaying advanced AAOA, more than half had signs of C2-nerve root conferred radiculopathy and motion induced suboccipital pain. The pain was not caused by nerve root or C2-ganglion compression, as there was no abnormal interlaminar space at C1–2 [6] in any patient. Facet joint pain is likely to be transmitted by unencapsulated receptors and free nerve endings in the joint capsule and synovial lining [35]. With aging or posttraumatic changes, degeneration with capsular laxity and synovitis can occur and finally AAOA can arise with a mechanical nature of pain [35, 36]. As in our sample, pain derived from the C1–2 facet joints is frequently described in nonneuropathic terms such as ‘pressurelike’, ‘deep boring’, ‘dull’, and ‘heavy’ [20, 35] and located almost exclusively at the ipsilateral retromastoid and occipital region [14, 20, 22, 28, 31, 35, 66]. As in the current study the main manifestations of C1–2 degeneration and AAOA are pain with significantly restricted ROM [22, 31], elicited or exacerbated by ipsilateral neck rotation [20, 22, 28, 35, 66]. Our current findings are in line with previous authors’ symptoms predominating on the side of the more significant lateral mass arthropathy, some patients even reporting crepitation [22, 45]. The pain in AAOA is secondary to an irritative phenomenon in the joint itself. When motion is eliminated in the joint, the irritation within ceases and pain generation is halted [22]. Therefore, immobilization and definite posterior fusion C1–2 relieves pain in patients with sequelae of AAOA [22, 28, 31, 35, 55] like in one of our cases with intractable pain resulting from a C2-vertebral body fracture with a burst pattern at the lateral mass (Fig. 3, 4). Several authors noticed AAOA to be a distracting source of pain [20, 31, 35, 36] and one of the sequelae following C1–2 fractures [26, 33, 39]. In part I of our project we elaborated the incidence of AAOA with 5% in normals with a mean age of 50 years [84]. Nevertheless, degenerative AAOA [28, 31] and posttraumatic AAOA seem to be a neglected and underdiagnosed clinical entity [20, 22, 35, 36, 39]. Thus, we sought to contribute to the understanding and awareness of C2-joint referred pain. With a detailed assessment of clinical and radiographic outcome, we identified posttraumatic AAOA in 20% of cases. We observed a strong correlation between the presence of posttraumatic AAOA and worse clinical outcome. Hence, beside its influence on ROTC1–2, the restoration of C1–2 anatomy is another important factor to be considered in C2-fracture treatment to avoid C2-malunion and accelerated atlantoaxial degeneration.
Conclusions
With growing awareness and the more liberal use of CT-scans using 3D-reconstructions, distinct fracture subtypes that frequently come along with odontoid, Hmfx or vertebral body fractures (e.g. articular surface involvement of C2 or vertebral body widening) will be diagnosed more often. The current study entailed a new approach to the outcome investigation of C2-fractures emphasizing the morphological stratification of distinct fracture subtypes. Using a functional CT-scanning protocol to assess rotation C1–2, validated outcome vehicles and applying a validated classification for the posttreatment alignment of C2 and the C1–2 complex, we demonstrated that malunion in C2-fractures had strong association with development of AAOA and a significant impact on clinical outcomes, atlantoaxial and total neck rotation.
Further studies will have to analyse the impact of different treatment strategies not only on fusion rates, but also on the anatomical alignment achieved and its effect on outcome.
Electronic supplementary material
Below is the link to the electronic supplementary material.
The analysis of the instantaneous center of rotation (ICR) of C1-C2 following C2-fractures. (DOC 648 kb)
Supplementary Tables 2, 3 and 10 (DOC 134 kb)
References
- 1.Aebi M, Etter C, Coscia M, et al. Fractures of the odontoid process: treatment with anterior screw fixation. Spine. 1989;14:1066–1070. doi: 10.1097/00007632-198910000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Apfelbaum RI, Lonser RR, Veres R, Casez A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg (Spine 2) 2000;93:227–236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]
- 3.Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine. 2002;27:2453–2458. doi: 10.1097/00007632-200211150-00007. [DOI] [PubMed] [Google Scholar]
- 4.BenDebba M, Heller J, Ducker TB, Eisinger JM. Cervical spine outcomes questionnaire. Its development and psychometric properties. Spine. 2002;27:2116–2124. doi: 10.1097/00007632-200210010-00007. [DOI] [PubMed] [Google Scholar]
- 5.Benzel EC, Hart BL, Ball PA, Baldwin NG, Orrison WW, Espinosa M. Fractures of the C2-vertebral body. J Neurosurg. 1994;81:206–212. doi: 10.3171/jns.1994.81.2.0206. [DOI] [PubMed] [Google Scholar]
- 6.Bilge O. An anatomic and morphometric study of C2 nerve root ganglion and its corresponding foramen. Spine. 2004;29:495–499. doi: 10.1097/01.BRS.0000113872.18219.7B. [DOI] [PubMed] [Google Scholar]
- 7.Blauth M, Richter M, Lange U. Transarticular screw fixation C1/C2 in traumatic atlantoaxial instabilities. Comparison between percutaneous and open procedures. Orthopade. 1999;28:651–661. doi: 10.1007/PL00003654. [DOI] [PubMed] [Google Scholar]
- 8.Bogduk N, Mercer S. Biomechanics of the cervical spine. I: normal kinematics. Clin Biomech (Bristol, Avon) 2000;15:633–648. doi: 10.1016/S0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]
- 9.Castro WH, Sautmann A, Schilgen M, Sautmann M. Noninvasive three-dimensional analysis of cervical spine motion in normal subjects in relation to age and sex. An experimental examination. Spine. 2000;25:443–449. doi: 10.1097/00007632-200002150-00009. [DOI] [PubMed] [Google Scholar]
- 10.Chang K, Liu Y, Cheng P. One Herbert double-threaded compression screw fixation of displaced type II odontoid fractures. J Spinal Disord. 1994;71:62–69. doi: 10.1097/00002517-199407010-00009. [DOI] [PubMed] [Google Scholar]
- 11.Chiba K, Fujimura Y, Toyama Y, Takahata T, Nakanishi T, Hirabayashi K. Anterior screw fixation for odontoid fracture: clinical results in 45 cases. Eur Spine J. 1993;2:76–81. doi: 10.1007/BF00302707. [DOI] [PubMed] [Google Scholar]
- 12.Clark CR, White AA. Fractures of the dens: A multicenter study. J Bone Joint Surg. 1985;67-A:1340–1348. [PubMed] [Google Scholar]
- 13.Dai LY, Yuan W, Ni N, Liu HK, Jia LS, Zhao DL, Xu YK. Surgical treatment of non-united fractures of the odontoid process, with special reference to occipitocervical fusion for unreducible atlantoaxial subluxation or instability. Eur Spine J. 2000;9:118–122. doi: 10.1007/s005860050221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dreyfuss P, Michaelsen M, Fletcher D. Atlanto-occipital and lateral atlanto-axial joint pain patterns. Spine. 1994;19:1125–1131. doi: 10.1097/00007632-199405001-00005. [DOI] [PubMed] [Google Scholar]
- 15.Dumas JL, Thoreux P, Attali P, Goldlust D, Chevrel JP. Three-dimensional CT analysis of atlantoaxial rotation: results in the normal subject. Surg Radiol Anat. 1994;16:199–204. doi: 10.1007/BF01627595. [DOI] [PubMed] [Google Scholar]
- 16.Dvorak J, Penning L, Hayek J, Panjabi MM, Grob D, Zehnder R. Functional diagnostics of the cervical spine using computer tomography. Neurorad. 1988;30:132–137. doi: 10.1007/BF00395614. [DOI] [PubMed] [Google Scholar]
- 17.Dvorak MF, Fisher CG, Aarabi B, Harris MB, Hurbert J, Rampersaud R, Vaccaro A, Harrop JS, Nockerls RP, Madrazo IN, Schwartz D, Kwon BK, Zhao Y, Fehlings MG. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine. 2007;32:3007–3031. doi: 10.1097/BRS.0b013e31815cd439. [DOI] [PubMed] [Google Scholar]
- 18.Dvorak MF, Johnson MG, Boyd M, Johnson G, Kwon BK, Fisher CG. Long-term health-related quality of life outcomes following Jefferson-type burst fractures of the atlas. J Neurosurg Spine. 2005;2:411–417. doi: 10.3171/spi.2005.2.4.0411. [DOI] [PubMed] [Google Scholar]
- 19.Dvorak MF Johnston M, Pitzen T (2002) The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion/distraction injuries. Presented at Canadian Spine Society 2nd Annual Meeting. Vernon, British Columbia, Canada [DOI] [PubMed]
- 20.Ehni G, Benner N. Occipital neuralgia and the C1–2 arthrosis syndrome. J Neurosurg. 1984;61:961–965. doi: 10.3171/jns.1984.61.5.0961. [DOI] [PubMed] [Google Scholar]
- 21.Ferrer S. Letter to the editor. Spine. 2001;26:158–159. [Google Scholar]
- 22.Finn M, Fassett DR, Apfelbaum RI. Surgical treatment of nonrheumatoid atlantoaxial degenerative arthtiris producing pain and myelopathy. Spine. 2007;32:3067–3073. doi: 10.1097/BRS.0b013e31815d004c. [DOI] [PubMed] [Google Scholar]
- 23.Fisher CG, Dvorak MFS, Leith J, Wing PC. Comparison of outcomes for unstable lower cervical flexion teardrop fractures managed with halo thoracic vest versus anterior corpectomy and plating. Spine. 2002;27:160–166. doi: 10.1097/00007632-200201150-00008. [DOI] [PubMed] [Google Scholar]
- 24.Fisher CG, Noonan VK, Dvorak MF. Changing face of spine trauma care in North America. Spine. 2006;31(Suppl):S2–S8. doi: 10.1097/01.brs.0000217948.02567.3a. [DOI] [PubMed] [Google Scholar]
- 25.Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG, Nikolakakos LG, Boev AN, Choudhri H, Smisson HF, Robinson JS., Jr Results of long-term follow-up in patients undergoing anterior odontoid screw fixation for type II and rostral type III odontoid fractures. Spine. 2005;30:661–669. doi: 10.1097/01.brs.0000155415.89974.d3. [DOI] [PubMed] [Google Scholar]
- 26.Fujimura Y, Nishi Y, Koyabashi K. Classification and treatment of axis body fractures. J Orthop Trauma. 1996;10:536–540. doi: 10.1097/00005131-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 27.German JW, Hart BL, Benzel EC. Nonoperative management of verticla C2 body fractures. Neurosurg. 2005;56:516–520. doi: 10.1227/01.NEU.0000153908.53579.E4. [DOI] [PubMed] [Google Scholar]
- 28.Ghanayem AJ, Leventhal M, Bohlman HH. Osteoarthrosis of the atlantoaxial joints. Long-term follow-up after treatment with arthrodesis. J Bone Joint Surg. 1996;78-A:1300–1307. doi: 10.2106/00004623-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, Albert TJ, Fehlings MG, Vaccaro AR. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5:123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Greene KA, Dickmann CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures: analysis of management and outcome in 340 consequitive cases. Spine. 1997;22:1843–1852. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 31.Grob D, Bremerich FH, Dvorak J, Mannion AF. Transarticular screw fixation for osteoarthritis of the atlantoaxial segment. Eur Spine J. 2006;15:283–291. doi: 10.1007/s00586-005-0963-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gunnarsson T, Massicotte EM, Govender PV, Rampersaud YR, Fehlings MG. The use of C1 lateral mass screws in complex cervical spine surgery: indications, techniques, and outcome in a prospective consecutive series of 25 cases. J Spinal Disord Tech. 2007;20:308–316. doi: 10.1097/01.bsd.0000211291.21766.4d. [DOI] [PubMed] [Google Scholar]
- 33.Hähnle U, Wiesniewski TF, Craig JB. Shear fracture through the body of the axis vertebra. Spine. 1999;24:2278–2281. doi: 10.1097/00007632-199911010-00018. [DOI] [PubMed] [Google Scholar]
- 34.Heller JG, Levz MJ, Barrow DL. Odontoid fracture malunion with fixed atlantoaxial subluxation. Spine. 1993;18:311–314. doi: 10.1097/00007632-199302000-00024. [DOI] [PubMed] [Google Scholar]
- 35.Holly LT, Batzdorf U, Foley KT. Treatment of severe retromastoid pain secondary to C1–2 arthrosis by using cervical fusion. J Neurosurg (Spine 2) 2000;92:162–168. doi: 10.3171/spi.2000.92.2.0162. [DOI] [PubMed] [Google Scholar]
- 36.Hollz LT, Batzdorf U, Foley KT. Treatment of severe retromastoid pain secondary to C1–2 arthrosis by using cervical fusion. J Neurosurg (Spine 2) 2000;92:162–168. doi: 10.3171/spi.2000.92.2.0162. [DOI] [PubMed] [Google Scholar]
- 37.Ishii K, Chiba K, Maruiwa H, Nakamura M, Matsumotot M, Toyama Y. Pathognomic radiological signs for predicting prognosis in patients with chronic atlantoaxial rotatory fixation. J Neurosurg Spine. 2006;5:385–391. doi: 10.3171/spi.2006.5.5.385. [DOI] [PubMed] [Google Scholar]
- 38.Javid D, Hedlund R, Vavruch L, Leszniewski W. Is the efficacy of the cloward procedure overestimated? Technique of evaluation affects the outcome. Eur Spine J. 2001;10:222–227. doi: 10.1007/s005860100261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jeanneret B, Vernet O, Frei S, Magerl F. Atlantoaxial mobility after screw fixation of the odontoid: a computer tomographic study. J Spinal Disord Tech. 1991;4:203–211. doi: 10.1097/00002517-199106000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Jeanneret B, Magerl M. Klinische Analyse der Spätresultate nach Hangman-Frakturen. Z Orthop. 1985;123:721. [Google Scholar]
- 41.Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidence based analysis of odontoid fracture management. Neurosurg Focus. 2000;8(6):1–6. doi: 10.3171/foc.2000.8.6.2. [DOI] [PubMed] [Google Scholar]
- 42.Kim YS, Lee YK, Moon SJ, Kim SH. Post-traumatic atlantoaxial rotatory fixation in an adult: a case report. Spine. 2007;32:E682–E687. doi: 10.1097/BRS.0b013e318158cf55. [DOI] [PubMed] [Google Scholar]
- 43.Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with nonunion in conservatively treated type-II fractures of the odontoid process. J Bone Joint Surg. 2004;86-B:1146–1151. doi: 10.1302/0301-620X.86B8.14839. [DOI] [PubMed] [Google Scholar]
- 44.Koller H, Acosta F, Tauber M, Komarek E, Fox M, Moursy M, Hitzl W (2009) C2-fractures: part I. Quantitative morphology of the C2 vertebra is a prerequisite for the radiographic assessment of posttraumatic C2-alignment and the investigation of clinical outcomes. Eur Spine J. doi:10.1007/s00586-009-0900-5 [DOI] [PMC free article] [PubMed]
- 45.Koller H, Assuncao A, Kammermeier V, Holz U. Simulateous anterior arthrodesis C2–3 and anterior odontoid screw fixation for stabilization of a 4-part fracture of the axis—a technical description. J Spinal Disord Tech. 2006;19:362–367. doi: 10.1097/01.bsd.0000204502.99471.9a. [DOI] [PubMed] [Google Scholar]
- 46.Koller H, Daniaux H, Gruber H, Blauth M, Kathrein A. The unstable traumatic spondylolisthesis C2–3. Akt Traumatol. 2006;35:183–202. doi: 10.1055/s-2005-865960. [DOI] [Google Scholar]
- 47.Koller H, Kammermeier V, Assuncao A, Holz U. Spinal stenosis C1–2 following redo surgery for failed odontoid screw fixation—scrutinizing the odontoid fracture classification. Internet J Spine Surg. 2007;3:1–11. [Google Scholar]
- 48.Koller H, Kathrein A. Letter to the editor concerning: a systematic review of the management of hangman’s fractures by Xin-Feng Li et al. (2006) Eur Spine J 15:257–269. Eur Spine J. 2006;15:257–269. doi: 10.1007/s00586-005-0918-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Koller H, Tauber M, Kathrein A. Letter to the editor. Spine. 2007;32:1571–1572. doi: 10.1097/BRS.0b013e318068660c. [DOI] [PubMed] [Google Scholar]
- 50.Koller H, Reynolds J, Zenner J, Forstner R, Hempfing A, Maislinger I, Kolb K, Tauber M, Resch H, Hitzl W (2009) Mid- to long-term outcome of instrumented anterior cervical fusion for subaxial injuries. Eur Spine J. doi:10.1007/s00586-008-0879-3 [DOI] [PMC free article] [PubMed]
- 51.Koller H, Kammermeier V, Ulbricht D, Assuncao A, Karolus S, van den Berg B, Holz U. Anterior retropharyngeal fixation C1–2 for stabilization of atlantoaxial instabilities: study of feasibility, technical descriotion and preliminary results. Eur Spine J. 2006;15:1326–1338. doi: 10.1007/s00586-006-0103-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Korres DS, Papagelopoulos PJ, Mavrogenis AF, Sapkas GS, Patsinevelos A, Kyriazopoulos P, Evangelopoulos D. Multiple fractures of the axis. Orthopedics. 2004;27:1096–1099. doi: 10.3928/0147-7447-20041001-21. [DOI] [PubMed] [Google Scholar]
- 53.Kwon BK, Fisher CG, Boyd MC, Cobb J, Jebson VN, Wing P, Dvorak MF. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1–12. doi: 10.3171/SPI-07/07/001. [DOI] [PubMed] [Google Scholar]
- 54.Lakshmanan P, Jones A, Howes J, Lyons K. CT evalutation of the pattern of odontoid fractures in the elderly-relationship to upper cervical spine osteoarthrosis. Eur Spine J. 2005;14:78–83. doi: 10.1007/s00586-004-0743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu G, Buchowski JM, Shen H, Yeom JS, Riew D. The feasibility of microscope-assisted ‘free-hand’ C1 lateral mass screw insertion without fluoroscopy. Spine. 2008;33:1042–1049. doi: 10.1097/BRS.0b013e31816d72b5. [DOI] [PubMed] [Google Scholar]
- 56.Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine. 2006;31:S53–S60. doi: 10.1097/01.brs.0000217941.55817.52. [DOI] [PubMed] [Google Scholar]
- 57.Müller EJ, Wick M, Russe OJ, Palta M, Muhr G. Anterior screw fixation for odontoid fractures (in german) Unfallch. 2000;103:38–43. doi: 10.1007/s001130050006. [DOI] [PubMed] [Google Scholar]
- 58.Pang D, Li Veetai. Atlantoaxial rotatory fixation: part 1—biomechanics of normal rotation at the atlantoaxial joint in children. Neurosurg. 2004;55:614–625. doi: 10.1227/01.NEU.0000134386.31806.A6. [DOI] [PubMed] [Google Scholar]
- 59.Pang D, Veetai Li. Atlantoaxial rotatory fixation: part 2—new diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging. Neurosurg. 2005;57:941–953. doi: 10.1227/01.NEU.0000181309.13211.3A. [DOI] [PubMed] [Google Scholar]
- 60.Pang D, Veetai Li. Atlantoaxial rotatory fixation: part 3—a prospective study of the clinical manifestation, diagnosis, management, and outcome of children with atlantoaxial rotatory fixation. Neurosurg. 2005;57:954–972. doi: 10.1227/01.NEU.0000180052.81699.81. [DOI] [PubMed] [Google Scholar]
- 61.Penning L, Wilmink JT. Rotation of the cervical spine. A CT study in normal subjects. Spine. 1987;12:732–738. doi: 10.1097/00007632-198710000-00003. [DOI] [PubMed] [Google Scholar]
- 62.Platzer P, Thalhammer G, Ostermann R, Wieland T, Vecsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32:1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 63.Platzer P, Thalhammer G, Sarahrudi K, Kovar F, Vekszler G, Vécsei V, Gaebler C. Nonoperative management of odontoid fractures using a halo-thoracic vest. Neurosurg. 2007;61:529–530. doi: 10.1227/01.NEU.0000290898.15567.21. [DOI] [PubMed] [Google Scholar]
- 64.Roche CJ, King SJ, Dangerfield PH, Carty HM. The atlanto-axial joint: physiological range mof rotation on MRI and CT. Clin Radiol. 2002;57:103–108. doi: 10.1053/crad.2001.0703. [DOI] [PubMed] [Google Scholar]
- 65.Ruf M, Melcher R, Harms J. Transoral reduction and osteosynthesis C1 as a function-preserving option in the treatment of unstable Jefferson fractures. Spine. 2003;29:823–827. doi: 10.1097/01.BRS.0000116984.42466.7E. [DOI] [PubMed] [Google Scholar]
- 66.Schaeren S, Jeanneret B. Atlantoaxial osteoarthritis: case series and review of literature. Eur Spine J. 2005;14:501–506. doi: 10.1007/s00586-004-0856-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Seelig M, Roth R, Worsdorfer O, Keerl R. Transoral correction osteotomy in transdental fracture dislocation that healed in the wrong position. Unfallch. 2000;103:791–794. doi: 10.1007/s001130050619. [DOI] [PubMed] [Google Scholar]
- 68.Seybold EA, Bayley JC. Functional outcome of surgically and conservativly managed dens fractures. Spine. 1998;23:1837–1846. doi: 10.1097/00007632-199809010-00006. [DOI] [PubMed] [Google Scholar]
- 69.Sgambati E, Capaccioli L, Biagiotti R, Giurovich E, Montigiani L, Brizzi E. Anatomical-radiological and morphometric analysis of the lateral atlantoaxial joint. Ital J Anat Embryol. 1998;103:117–123. [PubMed] [Google Scholar]
- 70.Signoret F, Feron JM, Bonfait H, Patel A. Fractured odontoid with fractured superior articular process of the axus. J Bone Joint Surg. 1986;68-B:182–184. doi: 10.1302/0301-620X.68B2.3957998. [DOI] [PubMed] [Google Scholar]
- 71.Stulik J, Vyskocil T, Sebesta P, Kryl J (2006) Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J (Epub) [DOI] [PMC free article] [PubMed]
- 72.Subach BR, Morone MA, Haid RW, McLaughlin MR, Rodts GR, Comey CH. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurg. 1999;45:812–820. doi: 10.1097/00006123-199910000-00015. [DOI] [PubMed] [Google Scholar]
- 73.Sugimoto Y, Tanaka M, Nakanishi K, Misawa H, Takigawa T, Ozaki T. Assessing the range of cervical rotation in patients with rheumatoid arthritis after atlantoaxial screw fixation using axial CT. Spine. 2007;32:2318–2321. doi: 10.1097/BRS.0b013e3181557222. [DOI] [PubMed] [Google Scholar]
- 74.Tuite GF, Papadopoulos SM, Sonntag VK. Caspar plate fixation for treatment of complex hangman’s fracture. Neurosurg. 1992;30:3761–3764. doi: 10.1097/00006123-199205000-00019. [DOI] [PubMed] [Google Scholar]
- 75.Venon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–419. [PubMed] [Google Scholar]
- 76.Verheggen R, Jansen J. Fractures of the odontoid process: analysis of the functional results after surgery. Eur Spine J. 1994;3:146–150. doi: 10.1007/BF02190576. [DOI] [PubMed] [Google Scholar]
- 77.Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–419. [PubMed] [Google Scholar]
- 78.Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation. Spine. 2007;32:643–646. doi: 10.1097/01.brs.0000257539.75693.cc. [DOI] [PubMed] [Google Scholar]
- 79.Wang C, Zan M, Yhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine. 2006;31:E30–E313. doi: 10.1097/01.brs.0000217686.80327.e4. [DOI] [PubMed] [Google Scholar]
- 80.Ware JE., Jr SF-36 health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 81.White AA, Panjabi MM. Kinematics of the spine. In: White AA, Panjabi MM, editors. Clinical biomechanics of the spine. Philadelphia: JB Lippincott; 1978. pp. 87–125. [Google Scholar]
- 82.Whitesides TE, McDonald AP. Lateral retroparyngeal approach to the upper cervical spine. Orthop Clin North Am. 1978;9:1115–1127. [PubMed] [Google Scholar]
- 83.Ying Z, Wen Y, Xinwei W, Yong T, Hongyu L, Zhu H, Qinggang Z, Weihong Z, Yonggeng C. Anterior cervical discectomy and fusion for unstable traumatic spondylolisthesiss of the axis. Spine. 2008;33:255–258. doi: 10.1097/BRS.0b013e31816233d0. [DOI] [PubMed] [Google Scholar]
- 84.Zapletal J, de Valois JC. Radiographic prevalance of advanced lateral C1–C2 osteoarthritis. Spine. 1997;22:2511–2513. doi: 10.1097/00007632-199711010-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The analysis of the instantaneous center of rotation (ICR) of C1-C2 following C2-fractures. (DOC 648 kb)
Supplementary Tables 2, 3 and 10 (DOC 134 kb)