Abstract
The technology used in surgery for spinal deformity has progressed rapidly in recent years. Commonly used fixation techniques may include monofilament wires, sublaminar wires and cables, and pedicle screws. Unfortunately, neurological complications can occur with all of these, compromising the patients’ health and quality of life. Recently, an alternative fixation technique using a metal clamp and polyester belt was developed to replace hooks and sublaminar wiring in scoliosis surgery. The goal of this study was to compare the pull-out strength of this new construct with sublaminar wiring, laminar hooks and pedicle screws. Forty thoracic vertebrae from five fresh frozen human thoracic spines (T5–12) were divided into five groups (8 per group), such that BMD values, pedicle diameter, and vertebral levels were equally distributed. They were then potted in polymethylmethacrylate and anchored with metal screws and polyethylene bands. One of five fixation methods was applied to the right side of the vertebra in each group: Pedicle screw, sublaminar belt with clamp, figure-8 belt with clamp, sublaminar wire, or laminar hook. Pull-out strength was then assessed using a custom jig in a servohydraulic tester. The mean failure load of the pedicle screw group was significantly larger than that of the figure-8 clamp (P = 0.001), sublaminar belt (0.0172), and sublaminar wire groups (P = 0.04) with no significant difference in pull-out strength between the latter three constructs. The most common mode of failure was the fracture of the pedicle. BMD was significantly correlated with failure load only in the figure-8 clamp and pedicle screw constructs. Only the pedicle screw had a statistically significant higher failure load than the sublaminar clamp. The sublaminar method of applying the belt and clamp device was superior to the figure-8 method. The sublaminar belt and clamp construct compared favorably to the traditional methods of sublaminar wires and laminar hooks, and should be considered as an alternative fixation device in the thoracic spine.
Keywords: Thoracic vertebrae, Scoliosis, Orthopedic fixation devices, Biomechanics
Introduction
Surgery for spinal deformity has progressed rapidly since Harrington’s development of nonsegmental instrumentation [12]. Segmental instrumentation using monofilament wires was first introduced by Luque in 1977 and has been used worldwide since [18]. Sublaminar wiring techniques have provided rigid fixation with improved correction [13]. Further developments have included the use of sublaminar cables made of stainless steel [27] or titanium [3]. However, spinal cord injury and neurological complications can occur during the sublaminar wiring procedure [15, 26, 29]. Additionally, delayed neurological complications and progression of spinal deformity have been reported following wire breakage and migration, [1, 7] and the removal of sublaminar wires carries a risk of dural compression [21].
Recently, an alternative fixation technique has been proposed to replace hooks and sublaminar wiring in scoliosis surgery. The device (Universal Clamp®, Abbott Spine, Bordeaux France) consists of a polyester belt and a metal clamp. The belt passes around the lamina and is fixed to a spinal rod by the clamp (Fig. 1). This construct provides increased contact with the bone surface compared to sublaminar wiring, yet maintains a low profile. In contrast to sublaminar wiring, the pliable polyester belt poses little compromise to the canal and can possibly reduce the risk of spinal cord injury. In addition, it allows postoperative imaging of the canal with MRI. In revision surgery, the polyester belt can be removed quickly and easily without damage to the bone. Preliminary clinical outcomes in idiopathic scoliosis are encouraging with average curve reduction of 65% and a low complication rate at 2-year follow-up [14].
Fig. 1.

The device: a polyester belt is passed around the pedicle and a metal clamp secures the belt to the spinal rod
The purpose of this study was to biomechanically assess the pull-out forces and failure mechanisms of two techniques of applying the polyester belt and clamp in the thoracic spine, and to compare them with the commonly used constructs of pedicle screws, laminar hooks, and sublaminar wiring.
Materials and methods
Specimens
The study was approved by our institutional review board. Five fresh frozen human thoracic spines (T5–12) with mean age of 75.8 years (SD 12) were obtained from the Anatomical Bequest Program of our institution. Bone mineral density (BMD) of each vertebra was measured using dual-energy x-ray absorptiometry (Lunar iDXA, GE Lunar, Madison, WI, USA). The spines were then dissected and individual vertebrae isolated. Surrounding soft tissues were removed. The dimensions of the pedicles and vertebral body of each vertebra were measured with a caliper.
Specimen preparation for testing
Each of the 40 individual vertebrae was prepared for potting by inserting two metal screws obliquely into the anterior portion of the vertebral body and placing two polyethylene bands though the spinal canal and around the vertebral body. Each vertebra was then potted in a circular acrylic fixture of 5 cm depth using polymethylmethacrylate (Coltene/Whaledent Inc, Cuyahoga Falls, OH, USA). Specimens were positioned with the posterior elements exposed and the vertebral body in the fixture, anchored by the screws and bands. Each specimen was imaged fluoroscopically and the appropriate vector for inserting a pedicle screw was marked on the outside of the fixture. This vector was also used as the direction of pull in all tests. After potting, specimens were kept moist with saline, wrapped with plastic, and refrigerated.
Groups for surgical procedures
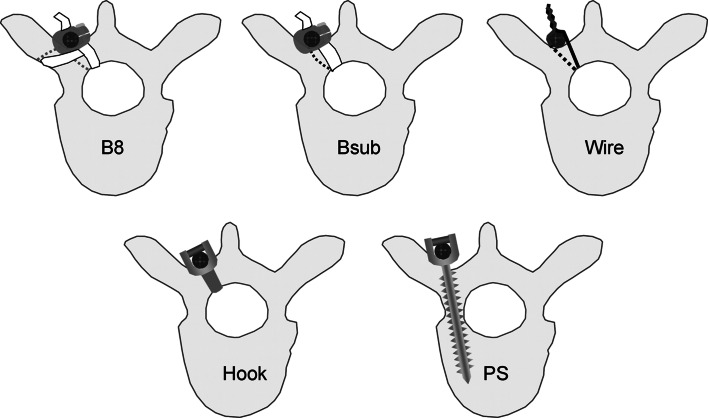
Specimens were sorted according to vertebral level then randomly assigned to one of five groups (8 per group). However, due to the small number of specimens the group mean BMD values demonstrated significant variation after randomization. Therefore, group assignments were adjusted to insure there was no significant difference among the groups in terms of the vertebral levels or BMD. For every specimen, the device being tested was implanted on the right side of the vertebra (Fig. 2) The five groups were as follows:
Figure-8 belt (B8): A polyester belt (1 × 6 mm) was passed around the transverse process and then under the lamina forming a “figure of 8” configuration before passing through the Universal Clamp®. The clamp was attached to a 5.5 mm rod and tightened to 6 Nm using a torque wrench.
Sublaminar belt (Bsub): The polyester belt was passed around the lamina and secured to the rod with the Universal Clamp®. The clamp was attached to a 5.5 mm rod and tightened to 6 Nm using a torque wrench.
Sublaminar wire (Wire): 1.0 m diameter monofilament stainless wire was passed under the lamina and then tightened over a 5.5 mm rod.
Laminar hook (Hook): A laminar hook (Abbott Spine, Bordeaux, France) with 5 mm width and 2 mm depth under the lamina was applied to the superior surface of the lamina, and secured to a 5.5 mm rod.
Pedicle screw (PS): A 5.5 mm polyaxial pedicle screw (Abbott Spine, Bordeaux, France) was inserted as described by Magerl [19]. The screw was then affixed to a 5.5 mm rod and tightened to 6 Nm with a torque wrench.
Fig. 2.
Five groups for surgical procedures. B8 Belt figure-8, Bsub belt sublaminar, Wire sublaminar wire, Hook sublaminar hook, PS pedicle screw
Biomechanical testing
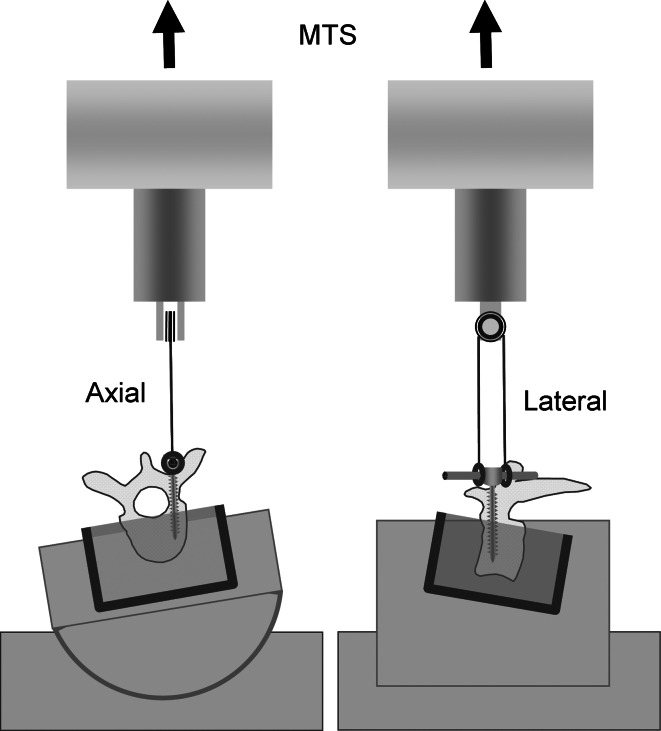
Pull-out tests were performed with an MTS 858 Minibionix II servohydraulic testing machine (MTS, Eden Prairie, MN, USA). Each specimen was placed in an adjustable positioning device such that the vector marked on the outside of the rectangular fixture during fluoroscopy was adjusted to conform to the direction of pull of the MTS actuator. A custom cable and pulley system was used to insure equal tension on each side of the device (pedicle screw, hook, wire, or clamp). The system consisted of two 6.3 mm (1/4 in.) diameter ball joint rod end bearings fixed to a 3.15 mm (1/8 in.) diameter stainless steel braided cable. The cable traveled around a precision bearing pulley attached to the actuator (Fig. 3).
Fig. 3.
Testing set up
To begin a test, the specimen was first aligned and clamped in the device. The crosshead of the cable and pulley system was then lowered and each side of the spine rod placed through the ball joint rod ends. To keep the ball joint rod ends from slipping during distraction collars were fixed to each end of the spine rod. The slack in the cable was then taken up by manually moving the crosshead. Pull-out force was applied at 5 mm per minute until failure, as determined by direct observation of the specimen and the load displacement curve. The mode of failure (screw pull-out, fracture, clamp pull-out, etc.) and the relationship between each device and the adjacent bony surface was carefully observed and recorded. Data (time, force, and displacement) were collected at 100 Hz.
Data analysis
The primary outcome was load at failure. Differences were assessed using one-factor analysis of variance with subsequent Fisher’s PLSD (protected least significant difference) post hoc tests. The relationship between failure load and BMD and between failure load and vertebral geometrical dimensions were analyzed with Pearson’s correlation coefficients. Analyses were executed with the StatView statistical package (SAS Institute Inc., Cary, NC, USA). P values ≤ 0.05 were considered statistically significant.
Results
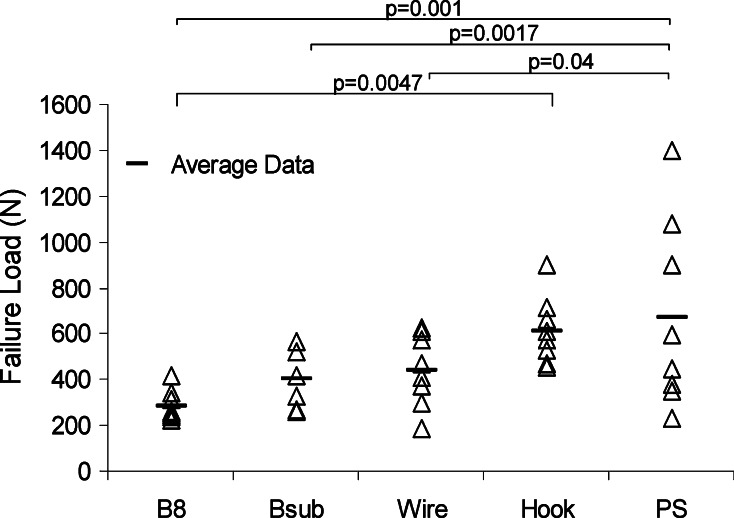
The means and standard deviations (SD) for BMD, pedicle diameter and vertebral body diameter are shown in Table 1. There were no significant differences among the groups in terms of these parameters. The mean (SD) failure loads (Newtons) were 286 ± 65 (B8), 401 ± 120 (Bsub), 441 ± 157 (Wire), 613 ± 147 (Hook), and 672 ± 412 (PS) (Fig. 4). Post hoc comparisons demonstrated that the mean failure load of the pedicle screw group was significantly higher than the figure-8 belt (P = 0.001), sublaminar clamp (0.0172), and sublaminar wire (P = 0.04). The failure load of the Hook construct was also significantly higher than the figure-8 belt group (P = 0.0047). There were no significant differences among the failure loads for the figure-8 belt, sublaminar belt, and sublaminar wire constructs (Fig. 4).
Table 1.
Mean and standard deviation of the vertebral parameters of the five groups
| Parameter | Figure-8 belt | Sublaminar belt | Sublaminar wire | Laminar hook | Pedicle screw | P value (ANOVA) |
|---|---|---|---|---|---|---|
| Vertebral levels |
7.5 ± 2.6 (4, 5, 6, 7, 7, 9, 11, 11) |
7.9 ± 2.5 (5, 6, 6, 7, 8, 8, 11, 12) |
8.1 ± 2.8 (4, 6, 7, 8, 9, 9, 10, 11) |
7.6 ± 2.7 (4, 5, 7, 8, 8, 10, 11, 12) |
8.1 ± 2.5 (4, 5, 6, 7, 8, 9, 10, 12) |
0.983 |
| BMD (g/cm2) | 0.82 ± 0.26 | 0.82 ± 0.28 | 0.80 ± 0.16 | 0.77 ± 0.17 | 0.80 ± 0.28 | 0.964 |
| Pedicle width (mm) | 6.3 ± 1.8 | 6.6 ± 2.1 | 6.1 ± 1.6 | 6.1 ± 2.8 | 6.4 ± 1.6 | 0.979 |
| Pedicle height (mm) | 12.7 ± 2.4 | 12.9 ± 2.3 | 13.4 ± 2.0 | 13.3 ± 2.3 | 12.4 ± 2.2 | 0.856 |
| Body height (mm) | 23.0 ± 2.8 | 24.4 ± 3.4 | 23.5 ± 2.0 | 22.8 ± 2.8 | 22.6 ± 3.1 | 0.665 |
| Body width (mm) | 35.5 ± 5.6 | 38.2 ± 7.2 | 37.4 ± 7.2 | 36.7 ± 7.2 | 34.2 ± 6.1 | 0.724 |
| Body AP depth (mm) | 31.5 ± 3.7 | 33.3 ± 4.2 | 33.8 ± 4.5 | 32.2 ± 3.8 | 32.1 ± 5.4 | 0.793 |
Fig. 4.
Failure loads of 5 configurations. B8 = Belt figure 8, Bsub = Belt sublaminar, Wire = Sublaminar wire, Hook = Sublaminar hook, PS = Pedicle Screw
Modes of failure for each group are listed in Table 2. Seven of eight specimens in both the sublaminar belt and sublaminar wire groups failed by fracture of the pedicle base as did four in the figure-8 belt group. The hook construct failed by cutting out of the lamina in five and fracture of the pedicle in three. Four of eight pedicle screw specimens failed by screw pull out at the interface between the bony matrix and the screw threads without gross disruption of bony structure and four failed by fracture of the pedicle base. Correlations between failure loads and BMD and between failure loads and bony dimensions are shown in Table 3. There was a significant correlation between BMD and failure load only in the B8 and PS constructs. In general, the larger the anatomical vertebral dimensions, the higher the failure load.
Table 2.
Mode of failure
| Figure-8 belt | Sublaminar belt | Sublaminar wire | Laminar hook | Pedicle screw | |
|---|---|---|---|---|---|
| Pedicle base fracture | 4 | 7 | 7 | 3 | 4 |
| Transverse process fracture | 2 | 0 | 0 | 0 | 0 |
| Lamina fracture | 0 | 0 | 1 | 5 | 0 |
| Clamp slip | 2 | 1 | NA | NA | NA |
| Screw pull-out | NA | NA | NA | NA | 4 |
Table 3.
Correlations of failure load with vertebral parameters
| Figure-8 belt | Sublaminar belt | Sublaminar wire | Laminar hook | Pedicle screw | |
|---|---|---|---|---|---|
| BMD | 0.883** | 0.644 | 0.452 | 0.084 | 0.957** |
| Pedicle width | 0.730* | 0.863** | 0.186 | 0.505 | 0.648 |
| Pedicle height | 0.854** | 0.831* | 0.226 | 0.500 | 0.566 |
| Body height | 0.743* | 0.835** | 0.636 | 0.282 | 0.667 |
| Body width | 0.743* | 0.825* | 0.068 | 0.300 | 0.617 |
| Body A-P depth | 0.350 | 0.644 | 0.133 | 0.217 | 0.770* |
Pearson’s correlation coefficient (r)
* P < 0.05, ** P < 0.01
Discussion
This study compared the pull-out strength and mode of failure of a new belt and clamp system with the traditional thoracic spine fixation techniques of pedicle screws, sublaminar wiring, and laminar hooks. The only traditional construct found to have a statistically significant higher failure load than the sublaminar belt was the pedicle screw. This may be due to the difference in the device-bone interface. The sublaminar method of applying the belt and clamp device appeared to be superior to the figure-8 method, because the transverse processes were not always strong enough to prevent fracture. The sublaminar belt construct compared favorably to the sublaminar wiring and laminar hook methods.
The mode of failure of the belt and clamp constructs was different than the traditional constructs. The figure-8 belt failed primarily by fracture of the pedicle base or transverse process. Including the transverse process in the belt configuration did not enhance its stability. Application of the belt in a figure-8 pattern increased the contact surface area of the belt but introduces a new mode of failure and does not appear to be a viable construct as applied in this study. The sublaminar belt construct failed primarily by pedicle base fracture similar to sublaminar wiring. Although the clamp slipped in 3 of 16 trials, design modifications of the clamp may reduce slippage.
There was high correlation between failure load and BMD in the pedicle screw construct, suggesting the obvious; pedicle screws are more likely to pull out of osteoporotic bone. The factors that correlated most with pull-out load of the sublaminar belt were related to the size of the pedicle and vertebral body. There was only moderate correlation of pull out load with BMD (r = 0.644).
The belt and clamp system is novel and may provide advantages in thoracic fixation compared to the traditional methods we used for comparison. The sublaminar belt method distributes the stress over a larger area of bone than sublaminar wires or hooks, thereby reducing the risk of failure at the device-bone interface. The mode of failure of the sublaminar belt and sublaminar wire constructs were similar, but none of the anatomical factors we considered significantly correlated with sublaminar wire failure load, suggesting that the belt may provide more predictable fixation in osteoporotic bone. The belt is less likely than wires to cause neural damage if displaced and should prove easier to remove from the central spinal canal.
Posterior instrumentation using pedicle screws has been widely used over the past two decades in the treatment of spinal deformities, degenerative disorders, and spinal injuries [5]. Segmental pedicle screws can effectively correct triplanar thoracic deformities [11, 28]. Pedicle screws are more resistant to axial and tangential loading than laminar hooks [8]. Triangulation of pedicle screws produces higher resistance to pull-out than single pedicle screws, and provides more secure vertebral manipulation [9]. However, safety concerns have been raised in regard to pedicle screws [2]. Loosening and failure of the screws have been reported in cases with inadequate fixation conditions, such as osteoporosis. This can result in non-union, sagittal collapse of the construct, or painful kyphosis [4, 22]. Surgical revision of failed pedicle screw constructs is challenging. Strategies include increasing the diameter and/or length of the screws or, in cases of severe bone loss, filling the void with polymethylmethacrylate or calcium phosphate cement [20, 24]. Other concerning issues in pedicle screw fixation are increased risk of pedicle fracture with concurrent neural injury, and anterior body penetration with vascular or visceral injuries [17]. Different screw designs have been studied, and conical screws have been found superior to cylindrical ones because of the speed of insertion and greater pull-out strength [23]. Expansive pedicle screws have also been proposed as a solution to problematic applications and were found to have greater pull-out force than USS, Tenor and CDH screws (6.5 × 40 mm) suggesting that they might perform better when bone integrity is compromised such as in osteoporosis or in revision surgery [16].
Supplemental offset laminar hooks have been used to share the bending moment applied to pedicle screws. However, the failure load of pedicle screws does not appear to increase if a hook is used at the same level [10]. Although offset hooks may enhance the pedicle screw construct when placed at the adjacent level, extending the fusion an additional level might also be considered.
Gayet et al. [6] investigated the traction resistance and mode of failure of posterior thoracic implants in single human motion segments. Pedicular-laminar traction resulted in fracture at the base of the pedicles. When pedicle screws were used a medial fissure was found at the base of the pedicle. Hooks imposed additional stresses on the vertebrae and had lower maximum failure strength than screws. However, hook fixation is often preferred to pedicle screws in elderly or osteoporotic patients. Yet, laminar hooks present additional risks; cauda equina compression due to hooks has been reported as a cause of late neurological complication in scoliosis surgery [25].
Although many different anchors have been developed most clinical failures still occur at the bone-instrumentation interface. A successful anchor design must attach firmly to the bone to provide sufficient fixation during fusion maturation. This is especially true in cases of osteoporosis. The Belt and clamp fixation technique tested in this study appears to be a promising alternative to laminar hooks and sublaminar wires in many scoliosis surgeries. It increases the contact surface of the device with the bone and maintains a low profile. Preliminary clinical outcomes are encouraging with low complication rates and high rates of fusion at 2 years follow-up [14]. In contrast to sublaminar wiring, the use of the polyester belt can possibly reduce the risk of long-term complications and spinal cord injury. In addition, the polyester material allows postoperative investigation of the canal with MRI. In the case of revision procedures, the polyester belt can be removed and new instrumentation applied as the likelihood of the belt damaging the bone is not great.
Acknowledgment
The biomechanical testing described in this study was funded by a contract with Abbott Spine Cite’ Mondiale, France.
Footnotes
All work performed at Mayo Clinic Rochester.
References
- 1.Bernard TN, Jr, Johnston CE, 2nd, Roberts JM, Burke SW. Late complications due to wire breakage in segmental spinal instrumentation. Report of two cases. J Bone Joint Surg Am. 1983;65:1339–1345. [PubMed] [Google Scholar]
- 2.Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke K. Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine. 1998;23:1566–1571. doi: 10.1097/00007632-199807150-00012. [DOI] [PubMed] [Google Scholar]
- 3.Doran SE, Papadopoulos SM, Miller LD. Internal fixation of the spine using a braided titanium cable: clinical results and postoperative magnetic resonance imaging. Neurosurgery. 1996;38:493–496. doi: 10.1097/00006123-199603000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Faraj AA, Webb JK. Early complications of spinal pedicle screw. Eur Spine J. 1997;6:324–326. doi: 10.1007/BF01142678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaines RW., Jr The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82-A:1458–1476. doi: 10.2106/00004623-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Gayet LE, Pries P, Hamcha H, Clarac JP, Texereau J. Biomechanical study and digital modeling of traction resistance in posterior thoracic implants. Spine. 2002;27:707–714. doi: 10.1097/00007632-200204010-00007. [DOI] [PubMed] [Google Scholar]
- 7.Goll SR, Balderston RA, Stambough JL, Booth RE, Jr, Cohn JC, Pickens GT. Depth of intraspinal wire penetration during passage of sublaminar wires. Spine. 1988;13:503–509. doi: 10.1097/00007632-198805000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Hackenberg L, Link T, Liljenqvist U. Axial and tangential fixation strength of pedicle screws versus hooks in the thoracic spine in relation to bone mineral density. Spine. 2002;27:937–942. doi: 10.1097/00007632-200205010-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hadjipavlou AG, Nicodemus CL, al-Hamdan FA, Simmons JW, Pope MH. Correlation of bone equivalent mineral density to pull-out resistance of triangulated pedicle screw construct. J Spinal Disord. 1997;10:12–19. doi: 10.1097/00002517-199702000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine. 1994;19:2415–2420. doi: 10.1097/00007632-199411000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 12.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44-A:591–610. [PubMed] [Google Scholar]
- 13.Herndon WA, Sullivan JA, Yngve DA, Gross RH, Dreher G. Segmental spinal instrumentation with sublaminar wires. A critical appraisal. J Bone Joint Surg Am. 1987;69:851–859. [PubMed] [Google Scholar]
- 14.Ilharreborde B, Mazda K. The universal clamp: a new method of thoracic fixation in the treatment of adolescent idiopathic scoliosis. Eur Musculoskeletal Rev. 2007;2:66–68. [Google Scholar]
- 15.Johnston CE, 2nd, Happel LT, Jr, Norris R, Burke SW, King AG, Roberts JM. Delayed paraplegia complicating sublaminar segmental spinal instrumentation. J Bone Joint Surg Am. 1986;68:556–563. [PubMed] [Google Scholar]
- 16.Lei W, Wu Z. Biomechanical evaluation of an expansive pedicle screw in calf vertebrae. Eur Spine J. 2006;15:321–326. doi: 10.1007/s00586-004-0867-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res. 1982;19:2–198. [PubMed] [Google Scholar]
- 19.Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;12:5–141. [PubMed] [Google Scholar]
- 20.Moore DC, Maitra RS, Farjo LA, Graziano GP, Goldstein SA. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine. 1997;22:1696–1705. doi: 10.1097/00007632-199708010-00003. [DOI] [PubMed] [Google Scholar]
- 21.Nicastro JF, Hartjen CA, Traina J, Lancaster JM. Intraspinal pathways taken by sublaminar wires during removal. An experimental study. J Bone Joint Surg Am. 1986;68:1206–1209. [PubMed] [Google Scholar]
- 22.Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H. Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine. 1993;18:2240–2245. doi: 10.1097/00007632-199311000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Ono A, Brown MD, Latta LL, Milne EL, Holmes DC. Triangulated pedicle screw construct technique and pull-out strength of conical and cylindrical screws. J Spinal Disord. 2001;14:323–329. doi: 10.1097/00002517-200108000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Reulen HJ, Pfaundler S, Ebeling U. The lateral microsurgical approach to the “extracanalicular” lumbar disc herniation. I: A technical note. Acta Neurochir (Wien) 1987;84:64–67. doi: 10.1007/BF01456353. [DOI] [PubMed] [Google Scholar]
- 25.Rittmeister M, Leyendecker K, Kurth A, Schmitt E. Cauda equina compression due to a laminar hook: a late complication of posterior instrumentation in scoliosis surgery. Eur Spine J. 1999;8:417–420. doi: 10.1007/s005860050197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schrader WC, Bethem D, Scerbin V. The chronic local effects of sublaminar wires. An animal model. Spine. 1988;13:499–502. doi: 10.1097/00007632-198805000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Songer MN, Spencer DL, Meyer PR, Jr, Jayaraman G. The use of sublaminar cables to replace Luque wires. Spine. 1991;16:S418–S421. doi: 10.1097/00007632-199108001-00022. [DOI] [PubMed] [Google Scholar]
- 28.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199520120-00012. [DOI] [PubMed] [Google Scholar]
- 29.Wilber RG, Thompson GH, Shaffer JW, Brown RH, Nash CL., Jr Postoperative neurological deficits in segmental spinal instrumentation. A study using spinal cord monitoring. J Bone Joint Surg Am. 1984;66:1178–1187. [PubMed] [Google Scholar]