Abstract
The present method of C2 laminar screw placement relies on anatomical landmarks for screw placement. Placement of C2 laminar screws using drill template has not been described in the literature. The authors reported on their experience with placement of C2 laminar screws using a novel computer-assisted drill guide template in nine patients undergoing posterior occipito-cervical fusion. CT scan of C2 vertebrae was performed. 3D model of C2 vertebrae was reconstructed by software MIMICS 10.01. The 3D vertebral model was then exported in STL format, and opened in a workstation running software UG imageware12.0 for determining the optimal laminar screw size and orientation. A virtual navigational template was established according to the laminar anatomic trait. The physical vertebrae and navigational template were manufactured using rapid prototyping. The navigational template was sterilized and used intraoperative to assist the placement of laminar screw. Overall, 19 C2 laminar screws were placed and the accuracy of screw placement was confirmed with postoperative X-ray and CT scanning. There were not complications of related screws insertion. Average follow-up was 9 months (range 4–13 months), 77.8% of the patients exhibited improvement in their myelopathic symptoms; in 22.2% the symptoms were unchanged. Postoperative computed tomographic (CT) scanning was available for allowing the evaluation of placement of thirteen C2 laminar screws, all of which were in good position with no spinal canal violation. This study shows a patient-specific template technique that is easy to use, can simplify the surgical act and generates highly accurate C2 laminar screw placement. Advantages of this technology over traditional techniques include planning of the screw trajectory is done completely in the presurgical period as well as the ability to size the screw to the patient’s anatomy.
Keywords: Computer-assisted, C2 laminar screw, Rapid prototyping, Drill template, Surgery
Introduction
Instability of the occipitocervical junction requiring surgical stabilization may be treated with a variety of techniques. The objective is to obtain solid fusion of the involved segments, which is best achieved by minimizing motion between them. Older methods such as the Brooks–Jenkins or modified Gallie wiring techniques, which are simpler procedures [2, 4] have been known for a long time. They are associated with failure rates of fusion up to 25%, primarily in cases with rotational instability. Newer techniques have been described that effectively limit motion along all axes. The addition of transarticular screw fixation, according to Magerl and Seemann, offers a better biomechanical stability [8, 11, 20, 24]. Magerl screw fixation must have a very precise point of insertion of the screw to make the fixation in the lateral mass of atlas. This may result in a significant risk to the vertebral artery [3, 29]. The size of the C2 isthmus can limit the ability to safely place these screws, particularly taking into account the anomalous position of the vertebral artery in relation to the isthmus of C2 in up to 20% of the population [5, 10, 18, 19].
Leonard and Wright [16] and Wright [27, 28] described a new technique of C2 laminar screw for rigid screw fixation of the axis and incorporation into atlantoaxial fixation or subaxial cervical constructs. Subsequent cases have shown good clinical results with this technique. C2 laminar screws are appropriate due to the reduced risk of injury to the vertebral artery and are as biomechanically stable as pedicle screw [7, 14]. The present method of C2 laminar screw placement relies on anatomical landmarks for screw placement. Potentially, serious C2 ventral laminar violations during the insertion of intralaminar screws have been reported [15]. Placement of C2 laminar screws using drill template has not been described in the literature. The aim of this article is to present the clinical results of a novel computer-assisted drill guide template for placement of C2 laminar screws. It is designed to simplify and shorten the surgical act and at the same time to enhance the accuracy of screw positions in the C2 lamina.
Materials and methods
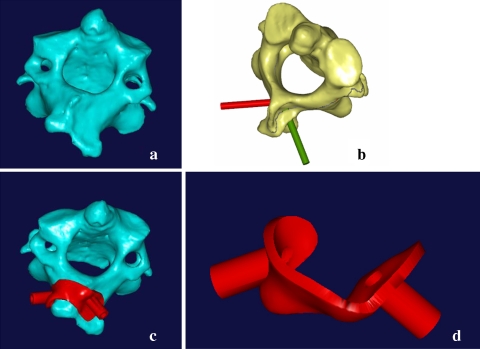
Prior to the operation, a spiral three-dimensional (3D) CT scan (LightSpeed VCT, GE, USA) was performed on cervical spine of each patient with 0.625-mm slice thickness and 0.35-mm in plane resolution. The images were stored in DICOM format, and transferred to a workstation running MIMICS 10.01 software (Materialise company, Belgium) to generate a 3D reconstruction model for the desired C2 vertebrae (Fig. 1a). The 3D vertebral model was then exported in STL format, and opened in a workstation running Reverse Engineering (RE) software UG imageware12.0 (EDS, USA) for determining the optimal screw size and orientation. A screw with a diameter of 4 mm was placed virtually into the 3D spinal model on both sides. The virtual screw’s entry point and the trajectory were placed centered on the lamina without violating the cortex and two screws will not interfere with each other (Fig. 1b).
Fig. 1.
The design of the virtual navigational template. a 3D model of C2 vertebra, b virtual display of the planned laminar screw trajectory, c navigational template fit the vertebral perfectly, d the virtual 3D model of navigational template
The optimal screw size was determined according to the size of lamina as well. Afterwards, a navigational template was constructed with one drill guide on either side. The template surface was created to be the inverse of C2 spinous process and laminar, thus potentially enabling a fit in a lock-and-key fashion similar to a physical casting of the vertebral surface, and specifically avoiding overlap onto adjacent segments (Fig. 1c). The inner diameter of the hollow cylinder was created to accommodate the preplanned trajectory for drilling. Once these had been done, a drill template was constructed with a surface designed to be the inverse of the vertebral surface (Fig. 1d).
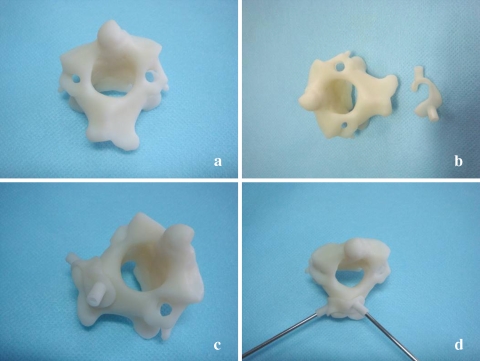
The computer model was then exported in STL format. The biomodel of the C2 vertebra as well as its corresponding navigational template were both produced by acrylate resin (Somos 14120, DSM Desotech Inc, USA) using stereolithography rapid prototyping (RP) technique. The accuracy of the navigational template was before surgery examined by visual inspection. The biomodel and its corresponding template were placed together, and a standard electric power drill was used to drill screw trajectory into the biomodel at the predefined placement, and visual inspection was taken for any violation of C2 laminar (Fig. 2).
Fig. 2.
The accuracy of the navigational template was examined by visual inspection. a RP model of C2 vertebra, b RP model of C2 vertebra and navigational template, c navigational template fit RP model of vertebra perfectly, d insert the K wire by navigational template; the accuracy of the navigational template was examined by visual inspection
From June 2006 to September 2008, nine patients (four males, five females, age 17–53 years) with basilar invagination requiring posterior instrumentation were performed occipitocervical fusion surgery by C2 laminar screw fixation. There were eight cases with occipitalization of the atlas, six cases accompanied by C2–3 vertebral fusion. In three patients, a transoral surgery was initially performed, followed by posterior surgery. The anatomy of C2 pedicle was observed preoperative with X-ray and CT scan, if the pedicle was very narrow, thin, or with vertebral artery riding high, this would be deemed to be an inappropriate indication for pedicle screws, and the laminar screw fixation may be choosed.
Under tracheal intubation and general anesthesia, patients were placed in the prone position with the head and cervical spine maintained in the neutral position using the Mayfield head holder. The spinous process, lamina, and lateral masses of C2 were then exposed as needed. Then, the drill template was placed on the spinous process and lamina of C2. Template and the corresponding spinous process fitted well. The high-speed drill was used along the navigational channel to drill the trajectory of laminar screw. Using a hand drill, the trajectory of laminar screw was carefully drilled to a depth of preoperation plan. A 4.0-mm screw was carefully inserted along the same trajectory. Using the same technique as above, a 4.0-mm screw was placed into the other lamina. After screw placement, all exposed laminar surfaces were decorticated with the high-speed drill. Autologous iliac crest bone grafts were wedged under the rods between the occipital bone and the spinous process and lamina of C2.
Results
Using the virtual 3D model, the optimal entry point for the drill can be choosed, thus, determining the entry point and direction for the C2 laminar screw. The drill template was created to fit the postural surface of C2 spinous process very well. The accuracy of the drill template was before operation examined by drilling K wire trajectory into the vertebra biomodel. Each navigational template fitted its corresponding vertebral biomodel perfectly, and K wire was found to be inserted through the drill hole into the C2 lamina, no violation was found by visual inspection.
Nine patients with basilar invagination underwent occipitocervical fusion surgery. Bilateral cross-laminar screw fixation was preformed in eight patients, unilateral laminar screw fixation and other side of pedicle screw fixation was performed in a patient. Average follow-up was 9 months (range 4–13 months). Preoperative and postoperative functional comparisons were made using the ASIA grading scale for all cases. The myelopathic symptoms improved at least one ASIA grade in seven of the patients (77.8%) and had not change in two patients (22.2%). No patient suffered neurological deterioration as a result of the procedure (Table 1).
Table 1.
Nine patients undergoing posterior occipitocervical fusion with template-guided placement of C2 laminar screws
| Cases | Sex | Ages (years) | Diagnosis | Operative procedure | Follow-up (myelopathic symptoms) | Placement accuracy (postoperative CT) |
|---|---|---|---|---|---|---|
| 1 | F | 42 | BI (OA, C2–3) | C0–2 | Improved | No bony breach |
| 2 | F | 38 | BI (OA) | C0–2 | No change | No bony breach |
| 3 | M | 17 | BI (OA, C2–3) | C0–2a | Improved | No bony breach |
| 4 | F | 29 | BI (OA) | C0–2 | Improved | No bony breach |
| 5 | M | 43 | BI (OA) | C0–2 | Improved | No bony breach |
| 6 | M | 35 | BI (C2–3) | C0–2 | Improved | No bony breach |
| 7 | F | 53 | BI (OA, C2–3) | C0–2 | No change | No bony breach |
| 8 | F | 34 | BI (OA, C2–3) | C0–2 | Improved | No bony breach |
| 9 | M | 27 | BI (OA, C2–3) | C0–2 | Improved | No bony breach |
BI basilar invagination, C0–2 posterior occipital-C2 fixation, OA occipitalization of the atlas, C2–3 C2–3 vertebral fusion
aUnilateral laminar screw fixation and other side of pedicle screw fixation
During the operation, the best-fit for positioning the template can easily be found manually, because no significantly free motion of the template occurs when it was pressed slightly against the C2 spinous process. As such, the navigational template is able to be used as in situ drill guide. The individual navigational template technique had the ability both to customize the placement and size of each screw based on the unique morphology of each patient’s C2 lamina and also to preoperatively prepare the surgical plan. To achieve this, an exact preparation of the bone surface was essential, including thorough removal of the attached muscle and fat tissue without damage to the bony surface.
Seventeen C2 laminar screws were inserted using drill template. No screw inserted complications, such as spinal cord, nerves, vertebral artery injury appeared in this group. The mean operative time between the fixation of the template to the lamina and placement of the screw was 1–2 min. No additional computer assistance was needed during surgery, and fluoroscopy was used only once, after all the C2 laminar screws had been inserted. The method thus reduced radiation exposure for the members of the surgical team.
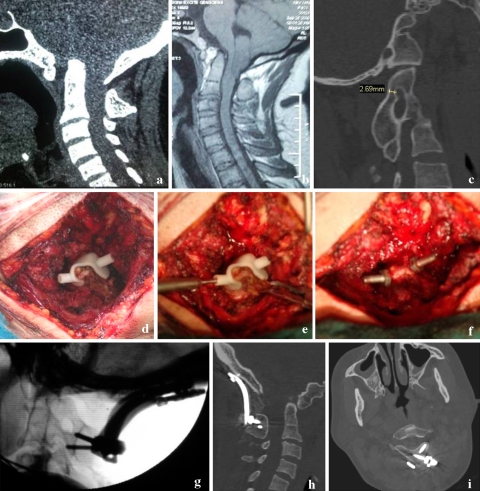
It takes about 16 h to manufacture the RP model, and the price of each RP model of the vertebra and navigational template was about $20. Postoperative CT scans showed that the individual template has a higher precision. No laminar screw misplacement occurred using the individual template (Fig. 3).
Fig. 3.
The navigational template applied in the operation of a 42-year-old women with basilar invagination, occipitalization of the atlas and C2–3 vertebral fusion. a, b Preoperative CT and T1 sagittal MRI displaying ventral brainstem compression, c preoperative CT shows the pedicle of C2 is narrow and cannot accommodate the 3.5-mm pedicle screw, d navigational template fit the spinous process and lamina of C2 perfectly, e the high-speed drill is used along the navigational channel to drill the trajectory of laminar screw, f insert the cervical pedicle screw by navigational template, g, h, i postoperative CT showing accurate placement of C2 laminar screws
Discussion
Traditional methods of intraoperative spinal localization have an important role in spine surgery. However, these methods have shortcomings that have led to the use of computer-assisted instrumentation [9, 12, 13, 25]. Image-guided techniques provide detailed views of hidden spinal anatomy that can be used for surgical planning and navigation. The techniques of C2 laminar screw placement described in the literature rely solely on the anatomical landmarks to guide screw insertion [14, 16, 26–28]. Two-dimensional (2-D) fluoroscopy is of limited benefit in C2 laminar screw placement. Nottmeier and Foy [21] presented a retrospective series of eight patients treated with posterior C1–2 fusion by laminar screws using 3D-fluoroscopy-based image guidance. They concluded that C2 laminar screws can be safely and accurately placed using 3D fluoroscopy-based image guidance. Advantages of this technology over traditional techniques include real-time 3D computerized feedback to the surgeon during placement, as well as the ability to size the screw to the patient’s anatomy using intraoperative computerized planning. However, several caveats should be considered: (1) the learning curve for these techniques is significant, (2) errors may occur if adjacent segments of the spine or the registration frame and optical array shift intraoperatively, (3) the tracking of optical array devices can be obscured by surgeons or tools, (4) the technology is expensive, (5) the techniques can lengthen the time of surgical procedures.
Making patient-specific drill templates with preplanned trajectories is a promising alternative for C2 laminar screw placement. A novel navigational template designed for the use in the placement of C2 laminar screw was introduced in this study, and the clinical application suggested its good applicability and high accuracy. Individual templates can be produced at a reasonable price compared with the cost of intraoperative navigation systems.
In the past decade, drill templates were initially demonstrated in the hip and knee [23], but several studies have described their use in the cervical, thoracic, and lumbar spine [1, 6, 17]. Some authors have designed different individual templates for spinal pedicle screw placement. Berry et al. [1] used a three V-shaped knife design to support the drill template. An advantage of using this design is that excessive soft-tissue dissection from the vertebra is not necessary. Goffin et al. [6] designed a template that featured a number of clamps to interface with the posterior course of the cervical vertebra. More recently, Owen et al. [22] constructed a drill template that was designed to match the posterior surface of the cervical vertebra around the entry point. With its greater contact with the surface area of the vertebra, this template was supposed to provide greater stability.
A preoperative CT scan is obtained to generate the individual templates and for a precise spatial correspondence between the individual bone structure in situ and the intended position of the tool guides. Obviously, the ability to customize the placement of each screw-based on the unique morphology of the C2 vertebra is an appealing concept. Nevertheless, the procedure of generating a medical model can be broken down into the following three major steps: the CT scan for data acquisition, the image segmentation combined with data processing and the building of the model itself. The availability of high-resolution CT scanner and advanced technologies used in the present study provide possibility for high geometric accuracy of the drill template. The Mimics software which is used to segment the CT scan images and perform data processing can provide fast, easy, and powerful 3D image processing and editing. Besides, new rapid prototyping technologies, which build up the object in thin layers, have recently been used instead of milling.
The advantage of the individual template is first, the surgeon can choose the placement and the size of each screw based on the unique morphology of the C2 vertebrae prior to surgery. The results have demonstrated that the lamina may differ individually, hence, preoperative CT evaluation is mandatory for precise planning of the surgical procedure, the diameter of the screw should be appropriate for the individual lamina. Second advantage of the individual template is its uncomplicated applicability and requires no surgeon-derived registration step. The preoperatively prepared drill template was used intraoperatively to assist with surgical navigation and the placement of instrumentation. Third, in contrast to the image-guided technique, individual template technique eliminates the need for complex equipment and time-consuming procedures in the operating room, the techniques reduce the time of surgical procedures. Fourth, the good accuracy has been demonstrated in this study. In addition, the accuracy of the individual template can be examined preoperatively by drilling screw into the biomodel through the cylinder hole. The greatest role of this technology is, perhaps, spinal deformity surgery where radiographic landmarks can be distorted and obscured. Lastly, individual template technique eliminates the need for fluoroscopy, and significantly reduces radiation exposure to the members of the surgical team as a result.
The technique also has potential sources of error. Because the 3D model of each vertebra is constructed manually or automatically, there is a potential for error in the procedure. Furthermore, the RP model could deviate from the computer 3D model, but existing RP technology can control deviation to 0.1 mm. Finally, geometric accuracy alone does not ensure accurate screw placement. In the clinical setting, a template should be able to be used as an in situ drill guide, and any movement between the bones will affect the accuracy.
Because any minor variation in the shape of the vertebra would introduce inaccuracy through poor fit, there could be trouble with soft-tissue on the bone. Thus, it is very important that the surgeon take great care in stripping the soft-tissue off the surface of the bone. Bone preparation must be done more cleanly than in conventional surgeries, and the soft-tissue preparation will take more time. Because more contact with the bone surface enhances the stability of the template, we make the template can contact with the both spinous process and lamina of C2. If attention is paid to these limitations, accurate matching of the template can be achieved, allowing accurate drill trajectories.
Our template design is unique in that it is created based on the posterior surface of the C2 spinal process and therefore can match this surface perfectly. Considering that, the C0–2 complex is highly mobile, so the drill template was designed single level fit. In a clinical situation, however, soft tissues around the spine are a big concern. Fortunately, after preparation of the bone, which involves thorough removal of the attached muscle and fat tissue without damaging the bony surface structure, all our templates can be easily and securely held in place by the surgeons’ free hands.
Conclusion
In summary, this study shows a patient-specific template technique that is easy to use, can simplify the surgical act and generates highly accurate C2 laminar screw placement. Advantages of this technology over traditional techniques include planning of the screw trajectory is done completely in the presurgical period as well as the ability to size the screw to the patient’s anatomy. It gives the surgeon an alternative to the placement of C2 laminar screw.
Acknowledgments
The authors would like to thank Dr. You-hua Cheng for his assistance with the CT data collection.
References
- 1.Berry E, Cuppone M, Porada S, Millner PA, Rao A, Chiverton N, Seedhom BB. Personalised image-based templates for intra-operative guidance. Proc Inst Mech Eng [H] 2005;219:111–118. doi: 10.1243/095441105X9273. [DOI] [PubMed] [Google Scholar]
- 2.Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60:279–284. [PubMed] [Google Scholar]
- 3.Coric D, Branch CL, Jr, Wilson JA, Robinson JC. Arteriovenous fistula as a complication of C1–2 transarticular screw fixation: case report and review of the literature. J Neurosurg. 1996;85:340–343. doi: 10.3171/jns.1996.85.2.0340. [DOI] [PubMed] [Google Scholar]
- 4.Dickman CA, Sonntag VK, Papadopoulos SM, Hadley MN. The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg. 1991;74:190–198. doi: 10.3171/jns.1991.74.2.0190. [DOI] [PubMed] [Google Scholar]
- 5.Ebraheim N, Rollins JR, Jr, Xu R, Jackson WT. Anatomic consideration of C2 pedicle screw placement. Spine. 1996;21:691–695. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 6.Goffin J, Brussel K, Martens K, Vander Sloten J, Audekercke R, Smet MH. Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1–2. Spine. 2001;26:1343–1347. doi: 10.1097/00007632-200106150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Gorek J, Acaroglu E, Berven S, Yousef A, Puttlitz CM. Constructs incorporating intralaminar C2 screws provide rigid stability for atlantoaxial fixation. Spine. 2005;30:1513–1518. doi: 10.1097/01.brs.0000167827.84020.49. [DOI] [PubMed] [Google Scholar]
- 8.Grob D, Jeanneret B, Aebi M, Markwalder TM. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br. 1991;73:972–976. doi: 10.1302/0301-620X.73B6.1955447. [DOI] [PubMed] [Google Scholar]
- 9.Hott JS, Papadopoulos SM, Theodore N, Dickman CA, Sonntag VK. Intraoperative Iso-C C-arm navigation in cervical spinal surgery: review of the first 52 cases. Spine. 2004;29:2856–2860. doi: 10.1097/01.brs.0000147742.20637.49. [DOI] [PubMed] [Google Scholar]
- 10.Igarashi T, Kikuchi S, Sato K, Kayama S, Otani K. Anatomic study of the axis for surgical planning of transarticular screw fixation. Clin Orthop Relat Res. 2003;408:162–166. doi: 10.1097/00003086-200303000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Jeanneret B, Magerl F. Primary posterior fusion C1–2 in odontoid fractures: indications, technique, and results of transarticular screw fixation technique. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K. Cervical pedicle screw insertion: assessment of safety and accuracy with computer-assisted image guidance. J Spinal Disord. 2000;13:218–224. doi: 10.1097/00002517-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Kothe R, Matthias Strauss J, Deuretzbacher G, Hemmi T, Lorenzen M, Wiesner L. Computer navigation of parapedicular screw fixation in the thoracic spine: a cadaver study. Spine. 2001;26:E496–E501. doi: 10.1097/00007632-200111010-00019. [DOI] [PubMed] [Google Scholar]
- 14.Lapsiwala SB, Anderson PA, Oza A, Resnick DK. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery. 2006;58:516–521. doi: 10.1227/01.NEU.0000197222.05299.31. [DOI] [PubMed] [Google Scholar]
- 15.Lehman RA, Jr, Sasso RC, Helgeson MD, Dmitriev AE, Gill NW, Rosner MR, Riew KD. Accuracy of intraoperative plain radiographs to detect violations of intralaminar screws placed into the C2 vertebrae: a reliability study. Spine. 2007;32:3036–3040. doi: 10.1097/BRS.0b013e31815cdab9. [DOI] [PubMed] [Google Scholar]
- 16.Leonard JR, Wright NM. Pediatric atlantoaxial fixation with bilateral, crossing C-2 translaminar screws: technical note. J Neurosurg. 2006;104:59–63. doi: 10.3171/ped.2006.104.1.59. [DOI] [PubMed] [Google Scholar]
- 17.Mac-Thiong JM, Labelle H, Rooze M, Feipel V, Aubin CE. Evaluation of a transpedicular drill guide for pedicle screw placement in the thoracic spine. Eur Spine J. 2003;12:542–547. doi: 10.1007/s00586-003-0549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 19.Mandel IM, Kambach BJ, Petersilge CA, Johnstone B, Yoo JU. Morphologic considerations of C2 isthmus dimensions for the placement of transarticular screws. Spine. 2000;25:1542–1547. doi: 10.1097/00007632-200006150-00014. [DOI] [PubMed] [Google Scholar]
- 20.Marcotte P, Dickman CA, Sonntag VK, Karahalios DG, Drabier J. Posterior atlantoaxial facet screw fixation. J Neurosurg. 1993;79:234–237. doi: 10.3171/jns.1993.79.2.0234. [DOI] [PubMed] [Google Scholar]
- 21.Nottmeier EW, Foy AB. Placement of C2 laminar screws using three-dimensional fluoroscopy-based image guidance. Eur Spine J. 2008;17:610–615. doi: 10.1007/s00586-007-0557-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Owen BD, Christensen GE, Reinhardt JM, Ryken TC. Rapid prototype patient-specific drill template for cervical pedicle screw placement. Comput Aided Surg. 2007;12:303–308. doi: 10.1080/10929080701662826. [DOI] [PubMed] [Google Scholar]
- 23.Radermacher K, Portheine F, Anton M, Zimolong A, Kaspers G, Rau G, Staudte HW. Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop Relat Res. 1998;354:28–38. doi: 10.1097/00003086-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Stillerman CB, Wilson JA. Atlanto-axial stabilization with posterior transarticular screw fixation: technical description and report of 22 cases. Neurosurgery. 1993;32:948–955. doi: 10.1097/00006123-199306000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Villavicencio AT, Burneikiene S, Bulsara KR, Thramann JJ. Utility of computerized isocentric fluoroscopy for minimally invasive spinal surgical techniques. J Spinal Disord Tech. 2005;18:369–375. doi: 10.1097/01.bsd.0000168511.67189.64. [DOI] [PubMed] [Google Scholar]
- 26.Wang MY. C2 crossing laminar screws: cadaveric morphometric analysis. Neurosurgery. 2006;59:84–88. doi: 10.1227/01.NEU.0000219900.24467.32. [DOI] [PubMed] [Google Scholar]
- 27.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004;17:158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Wright NM. Translaminar rigid screw fixation of the axis: technical note. J Neurosurg Spine. 2005;3:409–414. doi: 10.3171/spi.2005.3.5.0409. [DOI] [PubMed] [Google Scholar]
- 29.Wright NM, Lauryssen C. Vertebral artery injury in C1–2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves: American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]