Abstract
Abstract
Cervical pedicle screw is thought to be the most stable instrumentation for reconstructive surgery of the cervical spine. However, because of the unresolved and inherent risk of neurovascular injuries due to screw perforation, it remains not widespread nowadays despite the excellent biomechanical property. Fifty-two consecutive cases having undergone spinal reconstruction using cervical pedicle screw were investigated. There were 24 females and 28 males. The mean follow-up period was 53 months. Those patients were stratified into three groups according to the period of screw insertion. A total of 280 screws were inserted. Ninety-two screws in 19 cases, 100 screws in 18 cases and 88 screws in 15 cases were inserted in the earlier, the middle and the later periods, respectively. Clinical results including complications were recorded in all cases. Screw perforations were evaluated in both plain X-ray and CT. Screw perforations occurred in 11 (12.0%), 7 (7.0%) and 1 (1.1%) screws in each period. There were no complications, such as infection, neurological deterioration and neurovascular injury directly related to screw insertion. The learning curve showed a significant improvement especially in the later period. However, the perforation rates in both the earlier and middle periods must not be underestimated. Surgeons with less experience must insert cervical pedicle screws with the assistance of a senior surgeon to avoid lethal complications.
Keywords: Cervical spine, Pedicle screw, Accuracy, Screw perforation, Learning curve
Introduction
Because of the biomechanical stability, the in vitro investigations of cervical pedicle screw (CPS) insertion have been conducted by many researchers [11, 15, 16, 23–25, 32, 35, 36] Nowadays, the number of reports concerning clinical application of CPS except for Abumi is gradually increasing even though there is the unresolved and inherent risk of neurovascular complications [12, 20, 30, 37, 40, 41]. It is very helpful for cervical spine surgeons who would try to start cervical spine fusion with CPS to appreciate the exact results including its accuracy and complications.
Abumi et al. first reported the clinical application of CPS [1, 2]. They showed much experience and excellent results of cervical spine reconstruction using CPS [3–6, 8, 17]. They advocated the screw insertion angle from 25° to 45° in the axial plane. In addition, they also mentioned that the lateral location of the insertion point of CPS should have been almost at a bisecting point of the width of each facet. However, several in vitro studies showed that, according to the exact pedicle axis, the appropriate insertion of CPS should have been done both from a more lateral point and in a steeper angle in the axial plane [17, 18, 38]. Abumi et al. also reported complications of CPS [7]. Especially, the pedicle perforation rate was 6.2% (45 out of 667 screws) and neurovascular complications occurred in two screws. As well as Abumi et al. many authors showed that most of pedicle perforations occurred to the lateral direction, which might cause injuries of the vertebral artery. It is very important to lessen the screw perforation rate and complications to apply this procedure safely and effectively. Therefore, the methods to insert CPS should be improved and become more sophisticated.
Some authors reported the improved accuracy and insertion angle of CPS using navigation systems [24, 30, 37]. It is likely to be the best method to avoid the lethal perforation of CPS at the present time. So far, it seems unrealistic for every cervical spine surgeon to benefit from the navigation system. Most surgeons will have to perform CPS insertion under the guidance of fluoroscopy. Therefore, the learning curve of CPS insertion using fluoroscopy should be sternly investigated.
The objectives of this study are to report the learning curve of CPS insertion and to evaluate whether this innovative technique could be utilized by all cervical spine surgeons without any special instructions.
Methods
Patient demographics
Fifty-two patients who underwent posterior cervical spine fusion with CPS systems in our hospital from May 1998 were analyzed in the current study. There were 24 females and 28 males. The mean age was 62.6 years, ranging from 21 to 87 years. The mean follow-up period was 53 months, ranging from 6 to 113 months. The pathologies consisted of cervical spondylotic myelopathy with either severe instability and kyphosis or athetoid cerebral palsy in 12, failed cervical spine surgery including adjacent diseases, non-union and postlaminectomy stenosis in 11, fracture and/or dislocation in 9, cervical radiculopathy including cervical unilateral amyotrophy in 6, metastatic spine tumor in 6, rheumatoid arthritis in 6, pyogenic spondylitis in 2, atlantoaxial subluxation and retrodental pseudotumor in 1 each.
Complications
Because the aim of the current study is to analyze the accuracy of CPS insertion radiologically, we have omitted clinical evaluation from this paper except for complications in relation to CPS insertion.
Instrumentations
The Ti-mini-VSP system (Depuy Spine, Inc., Raynham, MA, USA), the Axon system (Synthes Spine, West Chester, PA) and the Universal Spine System (Synthes Spine, West Chester, PA) were used in 35, 15 and 2 cases, respectively.
The methods of pedicle screw insertion
All screws were inserted by the first author (H.Y.) without assistances and/or instructions of experienced surgeons. H.Y. started this technique after watching several cases of posterior cervical spine reconstructions using CPS with lateral fluoroscopy performed by several other experienced surgeons.
The methods of CPS insertion were divided into three:
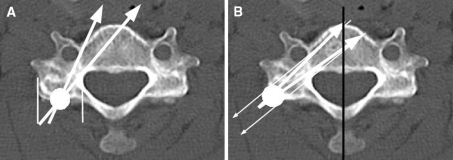
The first method in the earlier period (Period E): This is according to that described by Abumi and Kaneda [2]. An insertion hole is made on the posterior surface of the lateral mass by a high-speed burr under the guidance of lateral fluoroscopy at the bisecting point of the width of each facet joint. A screw hole is excavated by the original pedicle probe of the Ti-mini VSP system. The angle of screw insertion in the axial plane is aimed from 25° to 45° (Fig. 1a). This method was applied to 92 screws in 18 cases.
The second method in the middle period (Period M): an insertion hole is also made by a high-speed burr on the surface of the lateral mass where the pedicle axis is supposed to pass through. Using the same pedicle probe as the earlier period, a screw hole is excavated at the angle of 45° or more (Fig. 1b). This was applied to 100 screws in 19 cases.
The third method in the later period (Period L): the methods to create an insertion hole and the aiming angle of the screw hole are similar to those of Period M. The original pedicle probe of Ti-mini-VSP in both Periods E and M was relatively elastic. Therefore, it was sometimes bent very easily when pushing the probe to penetrate the pedicle or when the paravertebral muscles interfered with the correct trajectory of the pedicle probe, so that it occasionally led us to the misplacement of screws. From this point of view and due to the concept of a thoracic pedicle probe provided by Kim et al. [22], we have developed a new pedicle probe which is very stiff and is not bent at all with a keener and more curved tip. This makes it very easy to penetrate the sclerotic pedicle and to prevent breaching of the lateral pedicle wall. Eighty-eight screws in 15 cases were inserted through this procedure.
Fig. 1.
The method of screw insertion in each period. a The method of Period E. According to the original method provided by Abumi et al. an insertion hole is made on the posterior surface of the lateral mass by a high-speed burr under the guidance of lateral fluoroscopy at the bisecting point of the width of each facet joint. Then, a screw hole is excavated by a pedicle probe at the axial angle from 25° to 45°. Thin white lines represent the width of a facet joint. A white circle is the bisecting point of the width of a facet joint. White arrows are acceptable screw trajectories. b The method of Period M: an insertion point is made on the surface of the lateral mass where the pedicle axis passes through. A screw hole is excavated at the angle of 45° or more. Thin white arrows show the pedicle axis, which is defined as a perpendicular line to a line on the shortest distance between the transverse foramen and the lateral recess. A white circle is an inserting point just on the surface where the pedicle axis passes through. Thick white arrows are aiming screw trajectories. A black line represents perpendicular line to the posterior surface of the vertebral body, which is a base line of measurement of both anatomical pedicle angles (APA) and screw trajectory angles (STA)
In all periods, the longitudinal placement of the insertion holes and the longitudinal direction of the screw holes were confirmed with lateral fluoroscopy. Navigation systems were not used in the current study.
Screw placement
A total of 280 CPS were inserted. In this study, C1 lateral mass screws and thoracic pedicle screws that were inserted for patients having undergone either posterior atlantoaxial fusion or posterior cervicothoracic fusion were excluded from the current evaluation. The numbers of CPS were 16 in C2, 30 in C3, 48 in C4, 62 in C5, 74 in C6, 50 in C7, respectively.
Radiological investigations
Radiological investigations were implemented using plain X-ray films and computed tomography (CT). Both upward and downward pedicle perforation were checked by oblique X-ray films. The medial and lateral perforations of CPS were evaluated by CT. The perforation of a pedicle screw was classified into three ways: (1) complete perforation (CP) was defined as deviation of the screws from the pedicles by more than half of the screw diameter (Fig. 4); (2) partial perforation (PP) was defined as deviation from the pedicle of less than half of the screw diameter; and (3) when the screw did not violate the pedicle cortex and they were classified as having no perforation. Both the anatomical pedicle angle (APA) and the screw trajectory angle (STA) in the axial plane were also measured by CT in each patient (Fig. 1b). APA was defined as an angle between a perpendicular line to a line on the shortest distance between the transverse foramen and the lateral recess, which is a pedicle axis, and a perpendicular line to the posterior surface of the vertebral body. STA was also defined as an angle between an inserted screw and a perpendicular line to the posterior surface of the vertebral body. All measures of radiological evaluation were compared in those three groups, i.e. from Periods E to L. The accuracy of screw insertion and the learning curve were analyzed intensively.
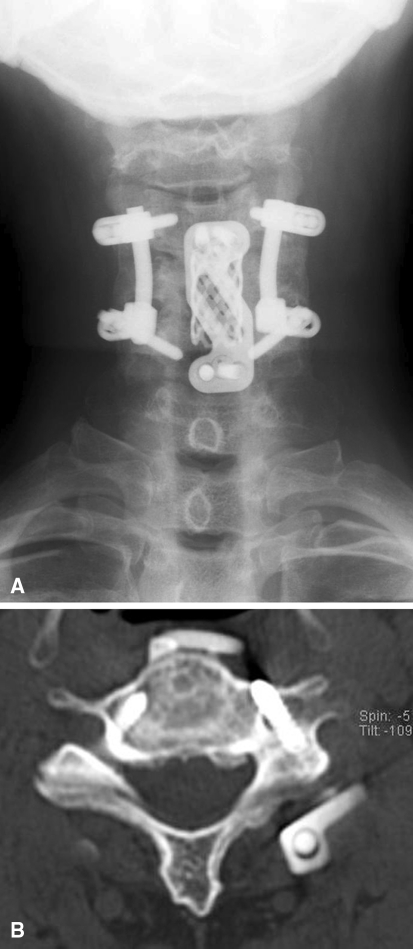
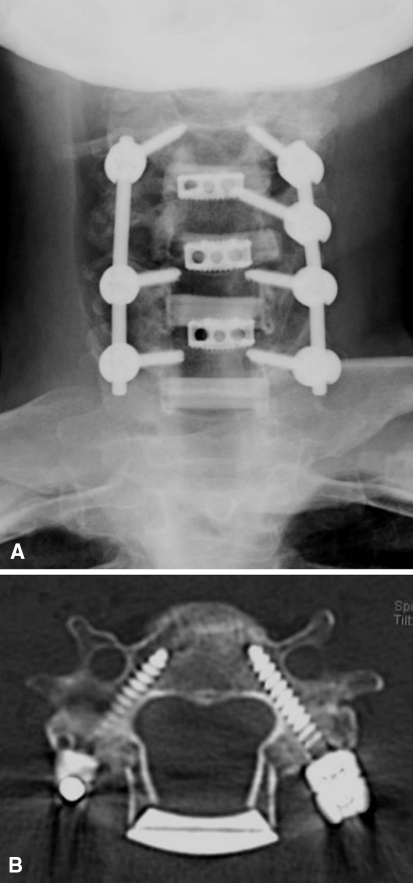
Fig. 4.
A representative case of Period E. A 52-year-old man with failed C4–C6 anterior fusion for cervical spondylotic radiculopathy. a Anteroposterior X-ray film after surgery. b Postoperative CT at C6. Right and left APA of C4 were 50° and 52°, respectively. The corresponding STA were 40° and 28°, respectively. Left C4 screw was recognized as “complete perforation”. Although the patient showed neither neurological complications nor vertebral artery insufficiency, screw removal was not undertaken. After 8 years of surgery, he is doing well with some posterior neck pain and slight radicular pain in the left arm
Statistical analysis
Chi-square test with Haberman’s residual analysis, analysis of variance, multiple comparison using Fisher’s PLSD and Spearman rank correlation were used for statistical analyses. In each analysis, P values <0.05 were considered as statistically significant.
Results
Complications
There were no complications such as neurovascular injuries relating to CPS insertion. During the follow-up, three patients died of diseases such as acute myocardial infarction, lung cancer and an accident not relating to cervical spine problems.
Radiological assessments
Screw perforations and the learning curve
There were no screws showing either upward or downward pedicle perforation in oblique X-ray films.
In the axial plane, a total of 19 screws (6.8%) were considered as showing pedicle perforations. Five screws were recognized as CP and the others were PP. All screws that showed CP were lateral perforations. Five out of 14 screws that showed PP were medial perforations.
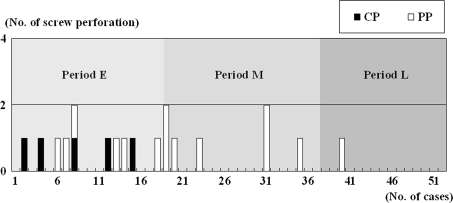
Figure 2 shows screw perforations in all patients in each period. All CP occurred in Period E. There is a statistically significant improvement of the learning curve of screw placement in Spearman rank correlation. (ρ = −0.674, P < 0.001) The demographics of patients in each period were showed in Table 1. There were no significant difference among three periods in terms of age, gender and etiologies.
Fig. 2.
An occurrence of screw perforations in 52 cases. The case numbers are completely in order. The cases were divided into three categories according to the methods of screw insertion, i.e. Period E (the earlier period), Period M (the middle period) and Period L (the later period). CP and PP mean complete screw perforation and partial perforation, respectively. All CP occurred in Period E. There is a definite tendency that both CP and PP became less as we encountered more cases. Spearman’s rank correlation shows a significant negative correlation between case number and occurrence of screw perforations (ρ = −0.674, P < 0.001)
Table 1.
Patients demographics in each period of CPS Insertion
| Period E | Period M | Period L | ||
|---|---|---|---|---|
| Age (years) | 60.3 ± 17.0 | 63.7 ± 17.9 | 64.9 ± 11.6 | NSa |
| Gender (n) | ||||
| Female | 8 | 8 | 8 | NSb |
| Male | 10 | 11 | 7 | |
| Entities (n) | ||||
| Degenerative | 10 | 13 | 9 | NSb |
| Tumor | 3 | 2 | 2 | |
| Inflammation | 4 | 2 | 0 | |
| Trauma | 1 | 2 | 4 | |
The values of ages were means and standard deviations
Degenerative is including cervical spondylotic myelopathy, cervical spondylotic radiculopathy, cervical myelopathy with athetoid palsy, retrodental pseudotumor and cervical spondylotic amyotrophy
Tumor means metastatic spine tumors
Inflammation consists of rheumatoid arthritis and pyogenic spondylitis
Trauma contains fracture-dislocation of the cervical spine and atlantoaxial dislocation due to odontoid fracture
CPS cervical pedicle screw
aNS not significant in ANOVA
bNS not significant in χ2 test
Table 2 summarized the results of screw perforations. Screw perforations in Periods E, M and L were 11 (12.0%), 7 (7.0%) and 1 (1.1%), respectively. CP significantly occurred in Period E in Haberman’s residual analysis (P < 0.01). PP was not significant in χ2 analysis. The sum of CP and PP was significantly frequent in Period E and rare in Period L in Haberman’s residual analysis (P < 0.05).
Table 2.
Numbers of CPS with complete perforation and partial perforation in each period
| Period E (92 screws) | Period M (100 screws) | Period L (88 screws) | χ2 test | |
|---|---|---|---|---|
| PP (n) | 6 | 7 | 1 | NS |
| CP (n) | 5* | 0a | 0a | P < 0.01 |
| CP + PP (n) | 11# (12.0%) | 7a (7.0%) | 1# (1.1%) | P < 0.05 |
CPS cervical pedicle screw, PP partial perforation, CP complete perforation, NS not significant in χ2 test
aNot significant in Haberman’s residual analysis
* P < 0.01 in Haberman’s residual analysis
#P < 0.05 in Herberman’s residual analysis
To eliminate the difference of the difficulty of screw insertions among those periods, we investigated the numbers of pedicles with degenerative sclerosis that were difficult to insert the pedicle probe. Among them, we divided those which were possible to excavate by pedicle probes from the others which required to be drilled by Kirschner wires [3]. The difficulty of pedicle screw insertion because of degenerative sclerosis of the pedicles was evaluated by operation records (Table 3) There were no significant differences in terms of the above-mentioned factors among three periods in χ2 test.
Table 3.
Numbers of CPS which were difficult to probe and/or drilled by K-wires in each period
| Period E (92 screws) | Period M (100 screws) | Period L (88 screws) | χ2 test | |
|---|---|---|---|---|
| Difficult pedicle probing (n) | 15 | 11 | 7 | NS |
| Drilled by K-wires (n) | 9 | 5 | 4 | NS |
CPS cervical pedicle screw, NS not significant in χ2 test
As shown in Table 4, screw perforations occurred two in C3, eight in C4, seven in C5, two in C6, whereas there were no perforations in C2 and C7. Haberman’s residual analysis revealed that perforations were more frequent in C4, but less in C7 with statistical significance.
Table 4.
Numbers of screw perforation in each vertebra
| C2 | C3 | C4 | C5 | C6 | C7 | χ2 test | |
|---|---|---|---|---|---|---|---|
| No. of CPS | 16 | 30 | 48 | 62 | 74 | 50 | P < 0.01 |
| No. of screw perforation | 0 (0%) | 2 (6.7%) | 8 (14.6%) | 7 (12.9%) | 2 (2.7%) | 0 (0%) | |
| NS | NS | P < 0.01 | NS | NS | P < 0.05 |
CPS cervical pedicle screw, NS not significant in χ2 test
NS not significant in Haberman’s residual analysis
Radiological assessments
Screw insertion angles in the axial plane
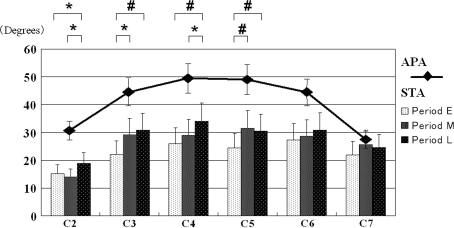
The mean APA and STA of all cases in the axial plane were shown in Table 5. The mean APA was generally greater than the mean STA with statistical significance.
Table 5.
The anatomical pedicle angles and the screw trajectory angles in all vertebrae
| Mean (°) | Range (°) | |
|---|---|---|
| C2 | ||
| APA | 29.8 | 27–33 |
| STA | 16.9 | 12–22 |
| C3 | ||
| APA | 41.8 | 34–56 |
| STA | 27.4 | 15–45 |
| C4 | ||
| APA | 46.0 | 33–58 |
| STA | 28.9 | 16–45 |
| C5 | ||
| APA | 45.6 | 39–64 |
| STA | 28.7 | 14–44 |
| C6 | ||
| APA | 41.7 | 30–54 |
| STA | 28.9 | 9–41 |
| C7 | ||
| APA | 27.0 | 21–34 |
| STA | 24.3 | 15–49 |
APA anatomical pedicle angle, STA screw trajectory angle
The differences of the average STA in each period were also shown in Fig. 3. In Fig. 3, the mean APA in each vertebra was superimposed by a bar graph. Except for C6 and C7, the mean STA in the later periods were steeper than those in the earlier periods with statistical significance. Although there was no statistical significance, the mean STA in C6 and C7 tended to be steeper in the later periods. As the periods advanced, STA became closer to APA.
Fig. 3.
Anatomical pedicle angles (APA) and screw trajectory angles (STA) of each vertebra in each period. The mean STA of each vertebra in each period were represented by a bar graph. The mean APA in each vertebra was superimposed by a line graph. Note a tendency to show larger STA in the later period than those of earlier period. The symbols # and * are P values <0.01 and those <0.05 in Fischer’s PLSD, respectively
Figures 4 and 5 show representative cases in Periods E and L, respectively. There are obvious differences of screw insertion angles between them.
Fig. 5.
A representative case of Period L. A 48-year-old woman suffering from athetoid cervical myelopathy who underwent C3–C6 circumferential fusion with Axon system and SynCage-C was shown. a Anteroposterior X-ray film after surgery. b Postoperative CT at C6. Right and left APA of C6 were 54° and 51°, respectively. The corresponding STA were 36° and 35°, respectively. Note all the screws were obviously inserted in steeper angles than those of a case in Fig. 4
Discussion
There are many papers considering the characteristics and efficacies of CPS in the in vitro study. They have analyzed the screw perforation rates [9, 19, 21, 27, 28, 33, 34], anatomical morphologies of the cervical pedicle and feasible screw trajectories [10, 13, 17, 18, 24, 29], biomechanical stability of CPS compared with lateral mass screw [11, 15, 16, 35], and other miscellaneous factors. [23, 25, 26, 32, 36] Contrarily, nowadays, we have a small number of clinical case studies using CPS [12, 20, 30, 37, 40, 41]. It is simply depending on the anatomical feature of the cervical pedicles, which are surrounded between the transverse foramens containing the vertebral arteries and the neural canal of the spinal cord. Therefore, lateral and medial perforations of CPS possibly lead us to the injury of the vertebral arteries and the spinal cord, respectively. Owing to the inherent risk of neurovascular injuries, clinical trials of CPS have not been widespread throughout the world yet.
However, some clinical trials of CPS have been gradually increasing for sure and were reporting excellent results. Because of the biomechanical stability, there are many advantages to select CPS for posterior reconstruction of the cervical spine, that is, the outstanding ability to reduce and maintain the rigid deformities of the cervical spine [5], high rate of bony fusion [39, 40, 41], early mobilization of patients and satisfactory maintenance of spinal alignment without excessive external fixation after surgeries [4, 31] and miscellaneous others. In terms of screw perforation, Abumi et al. [7] reported that the rate was 6.7% (45 out of 669 screws). Yoshimoto et al. [40] and Yukawa et al. [41] reported the entire rates were 11.1% (15 out of 134 screws) and 14.3% (59 out of 417 screws), respectively. Kast et al. described the pedicle perforation rate was up to 30% (28 out of 94 screws) including eight screws with the critical breaching [20]. Neo et al. showed 29% of screw perforation (25 out of 86 screws) [30]. Abumi et al. inserted CPS under the assistance of lateral fluoroscopy, and Yukawa et al. under oblique fluoroscopy (Table 6).
Table 6.
Review of the literature especially focusing on screw perforation rates
| Author | No. of CPS | No. of screw perforation | Percentage (%) | Methods of insertion |
|---|---|---|---|---|
| Abumi | 667 | 45 | 6.7 | Fluoroscopy (lateral) |
| Kotani | 78 | 1 | 1.1 | Navigation |
| Yoshimoto | 134 | 15 | 11.1 | Fluoroscopy (lateral) |
| Richter | 93 | 8 | 8.3 | Fluoroscopy (lateral) |
| 167 | 5 | 3.0 | Navigation | |
| Neo | 86 | 25 | 29.1 | Fluoroscopy (lateral) |
| Kast | 94 | 28 | 29.8 | Fluoroscopy (lateral) |
| Yukawa | 417 | 59 | 14.3 | Fluoroscopy (oblique) |
| Ito | 27 | 6 | 27.3 | Fluoroscopy (lateral) |
| 25 | 0 | 0 | Navigation |
CPS cervical pedicle screw
Richter et al. [37] mentioned that the rates of screw perforations were 8.6% (8 out of 93 screws) under the assistance of lateral fluoroscopy and 3.0% (5 out of 167 screws) with a navigation system. Kotani et al. [24] reported 1.1% (1 out of 78 screws) of perforation with their custom-made navigation system. Ito et al. [14] stated that, in RA patients, no screws were perforated the pedicle under the guidance of a navigation system but 22% (6 out of 27 screws) under conventional fluoroscopy (Table 6). Although reports of Richter et al. showed excellent perforation rates with navigation systems, those of them and the other authors who had inserted CPS under the guidance of fluoroscopy did not show any perforation rates. CPS insertion using a fluoroscopy is obviously less accurate than that of with a navigation system.
The authors showed the learning curve of CPS insertion in the current study. According to the review of the literature, there are no papers analyzing the learning curve of CPS insertion. The screw perforation rates in Periods E, M and L were 12.0, 7.0 and 1.1%, respectively, even though the difficulty of pedicle probing and the demographics of patients were not significantly different in each period. Obviously, time related and hands on experience of the authors to insert CPS could be a factor for the improved accuracy. However, the authors believe that changes to the methods of insertion CPS should have also been important for an improved screw perforation rate. As showed in Fig. 3, APA was much larger than STA. In addition, considering the fact that most of screw perforations were for the lateral side, to put insertion points more lateral and to make insertion angles larger, as explained in “Material and methods”, were natural for us who intended to improve the accuracy of screw insertion as mentioned previously by Neo et al. [30]. As shown in Fig. 4, STA in each vertebra was obviously improved as the periods advanced.
A custom-made pedicle probe was also likely to be effective to improve the accuracy. The stiff property of the new probe makes it relatively easy to aim the correct trajectory of the screw holes, whereas the original pedicle probe did not because of its elastic property. However, the benefit to utilize the new pedicle probe was not proven in the current study because the authors did not compare it with the original one at the same period.
Table 4 showed the rate of pedicle perforation in each vertebra. Pedicle perforations were significantly more frequent in C4, but less in C7. However, except for two, those were relatively frequent in C5 and less in C2 with marginal significance. This coincides with the result reported by Karaikovic et al. [19]. From the anatomical point of view, the pedicles of C4 and C5 are sometimes very stiff and sclerotic. Therefore, surgeons should take care when inserting CPS into both C4 and C5 whose APA are relatively larger than the other.
The screw perforation rate of Period L, i.e. 1.1%, is just as satisfactory as those reported by Richter et al. with navigation systems. Therefore, the authors want to emphasis that thorough trainings and experiences of cervical spine surgeons will make CPS insertion with fluoroscopy just as safe as those with a navigation system. However, the authors must not underestimate the perforation rates in Periods E and M. Indeed, there were no complications of spinal reconstruction using CPS, but, that may have been merely good fortune because the authors cannot help stating that the screw perforation rates in Periods E and M were drastically high.
If the screw perforation causes nerve root irritation, the screw should be removed as soon as possible. If it is possible for the screw misplacement to cause vertebral artery involvement, the surgeons should decide whether the screw must be removed. Either MR angiography or conventional angiography is useful to investigate the flow of the corresponding vertebral artery. Because, fortunately, the authors have not experienced the cases with either nerve root irritation or vertebral artery insufficiency, no cases underwent screw removal in this series. However, especially concerning the arterial involvement, the perforated screw might cause the late onset of cerebral and/or cerebellar infarction due to the chronic intimal injury of the vertebral artery. Therefore, the screw at risk might be removed as soon as possible.
If we accurately insert CPS, the authors assure that it will become a very powerful and useful tool for surgeons who want to reconstruct the cervical spine efficiently. To lessen the screw perforation rates in early periods, less-experienced surgeons must be assisted by experienced cervical spine surgeons, and should avoid the dangers of lethal and/or severe complications. When trying to begin cervical spine reconstruction using CPS, the authors highly recommend, from the view point of the learning curve, that they should do so a while under the supervision of experienced cervical spine surgeons until they learn exquisite techniques to insert CPS safely.
Conclusions
The learning curve of CPS insertion using lateral fluoroscopy was retrospectively analyzed in 52 consecutive cases. The screw perforation rates in the earlier, the middle and the later period were 12.0, 7.0 and 1.1%, respectively. The screw perforation rate of the later period was quite similar to those with navigation systems in the literature. However, surgeons must not underestimate the perforation rates of both the earlier and the middle periods in the current study. Less-experienced cervical spine surgeons should try this procedure with the assistance of experienced surgeons.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript. The devices used in the current study, i.e. the CPS system and the Axon system, have not been approved by the Food and Drug Administration in the United States.
Footnotes
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22:1853–1863. doi: 10.1097/00007632-199708150-00010. [DOI] [PubMed] [Google Scholar]
- 3.Abumi K, Kaneda K, Shono Y, Fujiya M. One-stage posterior decompression and reconstruction of the cervical spine by using pedicle screw fixation systems. J Neurosurg. 1999;90(Suppl 1):19–26. doi: 10.3171/spi.1999.90.1.0019. [DOI] [PubMed] [Google Scholar]
- 4.Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine. 1999;24:1425–1434. doi: 10.1097/00007632-199907150-00007. [DOI] [PubMed] [Google Scholar]
- 5.Abumi K, Shono Y, Taneichi H, Ito M, Kaneda K. Correction of cervical kyphosis using pedicle screw fixation systems. Spine. 1999;24:2389–2396. doi: 10.1097/00007632-199911150-00017. [DOI] [PubMed] [Google Scholar]
- 6.Abumi K, Shono Y, Kotani Y, Kaneda K. Indirect posterior reduction and fusion of the traumatic herniated disc by using a cervical pedicle screw system. J Neurosurg. 2000;92(Suppl 1):30–37. doi: 10.3171/spi.2000.92.1.0030. [DOI] [PubMed] [Google Scholar]
- 7.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Abumi K, Ito M, Kaneda K. Surgical treatment of cervical destructive spondyloarthropathy (DSA) Spine. 2000;25:2899–2905. doi: 10.1097/00007632-200011150-00011. [DOI] [PubMed] [Google Scholar]
- 9.Cha SH, Kim C, Choi BK, Kim HJ, Baek SY. C-arm assessment of cervical pedicle screw: screw coaxial fluoroscopy and oblique view. Spine. 2007;32:1721–1727. doi: 10.1097/BRS.0b013e3180b9f29b. [DOI] [PubMed] [Google Scholar]
- 10.Chazono M, Soshi S, Inoue T, Kida Y, Ushiku C. Anatomical considerations for cervical pedicle screw insertion: the use of multiplanar computerized tomography reconstruction measurements. J Neurosurg Spine. 2007;4:472–477. doi: 10.3171/spi.2006.4.6.472. [DOI] [PubMed] [Google Scholar]
- 11.Dickerman RD, Reynolds AS, Stevens Q, Zigler J. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2007;7:384. doi: 10.1016/j.spinee.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Djurasovic M, Dimar JR, 2nd, Glassman SD, Edmonds HL, Carreon LY. A prospective analysis of intraoperative electromyographic monitoring of posterior cervical screw fixation. J Spinal Disord Tech. 2005;18:515–518. doi: 10.1097/01.bsd.0000173315.06025.c6. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim NA, Xu R, Knight T, Yeasting RA. Morphometric evaluation of lower cervical pedicle and its projection. Spine. 1997;22:1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 14.Ito H, Neo M, Yoshida M, Fujibayashi S, Yoshitomi H, Nakamura T. Efficacy of computer-assisted pedicle screw insertion for cervical instability in RA patients. Rheumatol Int. 2007;27:567–574. doi: 10.1007/s00296-006-0256-7. [DOI] [PubMed] [Google Scholar]
- 15.Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667–672. doi: 10.1016/j.spinee.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws: anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 17.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine. 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 18.Karaikovic EE, Kunakornsawat S, Daubs MD, Madsen TW, Gaines RW., Jr Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord. 2000;13:63–72. doi: 10.1097/00002517-200002000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Karaikovic EE, Yingsakmongkol W, Gaines RW., Jr Accuracy of cervical pedicle screw placement using the funnel technique. Spine. 2001;26:2456–2462. doi: 10.1097/00007632-200111150-00012. [DOI] [PubMed] [Google Scholar]
- 20.Kast E, Mohr K, Richter HP, Börm W. Complications of transpedicular screw fixation in the cervical spine. Eur Spine J. 2006;15:327–334. doi: 10.1007/s00586-004-0861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim HS, Heller JG, Hudgins PA, Fountain JA. The accuracy of computed tomography in assessing cervical pedicle screw placement. Spine. 2003;28:2441–2446. doi: 10.1097/01.BRS.0000090830.94641.AE. [DOI] [PubMed] [Google Scholar]
- 22.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 23.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems: an assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 24.Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99(Suppl 3):257–263. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 25.Kothe R, Rüther W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29:1869–1875. doi: 10.1097/01.brs.0000137287.67388.0b. [DOI] [PubMed] [Google Scholar]
- 26.Kowalski JM, Ludwig SC, Hutton WC, Heller JG. Cervical spine pedicle screws: a biomechanical comparison of two insertion techniques. Spine. 2000;25:2865–2867. doi: 10.1097/00007632-200011150-00005. [DOI] [PubMed] [Google Scholar]
- 27.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine. 2000;25:1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 28.Ludwig SC, Kowalski JM, Edwards CC, 2nd, Heller JG. Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine. 2000;25:2675–2781. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 29.Miller RM, Ebraheim NA, Xu R, Yeasting RA. Anatomic consideration of transpedicular screw placement in the cervical spine: an analysis of two approaches. Spine. 1996;21:2317–2322. doi: 10.1097/00007632-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 30.Neo M, Sakamoto T, Fujibayashi S, Nakamura T. The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine. 2005;30:2800–2805. doi: 10.1097/01.brs.0000192297.07709.5d. [DOI] [PubMed] [Google Scholar]
- 31.Oda I, Abumi K, Ito M, Kotani Y, Oya T, Hasegawa K, et al. Palliative spinal reconstruction using cervical pedicle screws for metastatic lesions of the spine: a retrospective analysis of 32 cases. Spine. 2006;31:1439–1444. doi: 10.1097/01.brs.0000219952.40906.1f. [DOI] [PubMed] [Google Scholar]
- 32.Papagelopoulos PJ, Currier BL, Neale PG, Hokari Y, Berglund LJ, Larson DR, et al. Biomechanical evaluation of posterior screw fixation in cadaveric cervical spines. Clin Orthop Relat Res. 2003;411:13–24. doi: 10.1097/01.blo.0000068359.47147.bd. [DOI] [PubMed] [Google Scholar]
- 33.Reinhold M, Magerl F, Rieger M, Blauth M. Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J. 2007;16:47–56. doi: 10.1007/s00586-006-0104-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reinhold M, Bach C, Audigé L, Bale R, Attal R, Blauth M, et al. Comparison of two novel fluoroscopy-based stereotactic methods for cervical pedicle screw placement and review of the literature. Eur Spine J. 2008;22:564–575. doi: 10.1007/s00586-008-0584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rhee JM, Kraiwattanapong C, Hutton WC. A comparison of pedicle and lateral mass screw construct stiffness at the cervicothoracic junction: a biomechanical study. Spine. 2005;30:E636–E640. doi: 10.1097/01.brs.0000184750.80067.a1. [DOI] [PubMed] [Google Scholar]
- 36.Richter M, Cakir B, Schmidt R. Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine. 2005;30:2280–2287. doi: 10.1097/01.brs.0000182275.31425.cd. [DOI] [PubMed] [Google Scholar]
- 37.Richter M, Wilke HJ, Kluger P, Neller S, Claes L, Puhl W. Biomechanical evaluation of a new modular rod-screw implant system for posterior instrumentation of the occipito-cervical spine: in-vitro comparison with two established implant systems. Eur Spine J. 2000;9:417–425. doi: 10.1007/s005860000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Su P, Ma R, Li C, Liu S, Huang D. Pedicle screw fixation of the cervical spine: guidance by computed tomography. Clin Orthop Relat Res. 2007;462:99–104. doi: 10.1097/BLO.0b013e3180ebe4e5. [DOI] [PubMed] [Google Scholar]
- 39.Sudo H, Ito M, Abumi K, Kotani Y, Takeuchi T, Yasui K, et al. Long-term follow up of surgical outcomes in patients with cervical disorders undergoing hemodialysis. J Neurosurg Spine. 2006;5:313–319. doi: 10.3171/spi.2006.5.4.313. [DOI] [PubMed] [Google Scholar]
- 40.Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Spinal reconstruction using a cervical pedicle screw system. Clin Orthop Relat Res. 2005;431:111–119. doi: 10.1097/01.blo.0000150321.81088.ab. [DOI] [PubMed] [Google Scholar]
- 41.Yukawa Y, Kato F, Yoshihara H, Yanase M, Ito K. Cervical pedicle screw fixation in 100 cases of unstable cervical injuries: pedicle axis views obtained using fluoroscopy. J Neurosurg Spine. 2006;5:488–493. doi: 10.3171/spi.2006.5.6.488. [DOI] [PubMed] [Google Scholar]