Abstract
The purpose of this study was to examine factors affecting the severity of neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture (OVF). Reports of insufficient union following OVF have recently increased. Patients with this lesion have various degrees of neurological deficits and back pain. However, the factors contributing to the severity of these are still unknown. A total of 45 patients with insufficient union following OVF were included in this study. Insufficient union was diagnosed based on the findings of vertebral cleft on plain radiography or CT, as well as fluid collection indicating high-intensity change on T2-weighted MRI. Multivariate logistic regression analysis was performed to determine the factors contributing to the severity of neurological deficits and back pain in the patients. Age, sex, level of fracture, duration after onset of symptoms, degree of local kyphosis, degree of angular instability, ratio of occupation by bony fragments, presence or absence of protrusion of flavum, and presence or absence of ossification of the anterior longitudinal ligament (OALL) in the adjacent level were used as explanatory variables, while severity of neurological deficits and back pain were response variables. On multivariate analysis, factors significantly affecting the severity of neurological deficits were angular instability of more than 15° [adjusted odds ratio (OR), 9.24 (95% confidence interval, CI 1.49–57.2); P < 0.05] and ratio of occupation by bony fragments in the spinal canal of more than 42% [adjusted OR 9.23 (95%CI 1.15–74.1); P < 0.05]. The factor significantly affecting the severity of back pain was angular instability of more than 15° [adjusted OR 14.9 (95%CI 2.11–105); P < 0.01]. On the other hand, presence of OALL in the adjacent level reduced degree of back pain [adjusted OR 0.14 (95%CI 0.03–0.76); P < 0.05]. In this study, pronounced angular instability and marked posterior protrusion of bony fragments in the canal were factors affecting neurological deficits. In addition, marked angular instability was a factor affecting back pain. These findings are useful in determining treatment options for patients with insufficient union following OVF.
Keywords: Osteoporotic vertebral fracture, Risk factor, Insufficient bone union, Neurological deficit, Back pain
Introduction
Fracture associated with osteoporosis has become a major problem because the population of elderly individuals has been increasing [4]. Modalities efficacious in preventing as well as treating osteoporosis-associated fractures are thus desired in the coming decade [7]. Among such fractures, vertebral fractures are the most common type with significant morbidity [24].
The osteoporotic vertebral fracture (OVF) has severe impact on activities of daily living and quality of life in elderly patients and is the beginning of a long-lasting deterioration of the patient’s health [28]. Some patients present with intractable back pain for prolonged periods of time, while others suffer from neurological deficits within a few months’ time after fracture. In such cases, insufficient union is often noted on plain radiography and/or MRI [18, 22]. Recently, reports of insufficient union have been increasing [13, 15, 19, 26, 29].
Patients with insufficient union following OVF have been treated with various methods conservatively and surgically. Surgical procedures include resection of fractured vertebral bodies and grafting of autologous bone with implants through the anterior approach are one option, while closed-wedge osteotomy through the posterior approach has been another [9, 20, 25, 27]. However, considering the age and comorbidities of affected patients, each of these procedures is rather invasive. Vertebroplasty is less invasive and has been reported to yield successful clinical results for painful OVF, but not to yield satisfactory results for patients with neurological deficits [2, 8, 14, 23].
Thus, the treatment options for insufficient union following OVF have not been clearly established. To elucidate useful treatment options for this lesion, it is necessary to evaluate the factors contributing to neurological deficits and/or intractable back pain associated with this type of fracture. The purpose of this study was to elucidate the factors affecting the severity of neurological deficits and intractable back pain in patients with insufficient bone union following OVF.
Material and methods
Patient population
A total of 45 patients treated for insufficient union following OVF were retrospectively reviewed. Insufficient union was diagnosed based on intravertebral vacuum cleft on plain radiography or CT, as well as fluid collection on T2-weighted MRI within the vertebral body. All patients had continued to complain of symptoms for longer than 2 months (range 2–36 months, mean 6.9 months).
There were 10 men and 35 women whose mean age at the time of diagnosis was 74 years (range 56–87 years). The fracture levels were T9 in 1 patient, T11 in 3, T12 in 22, L1 in 11, L2 in 6, L4 in 1, and L5 in 1. In these patients, bone mineral density was measured in the lumbar spine or femoral neck, and the diagnosis of osteoporosis was confirmed. Other metabolic bone diseases and malignancies such as myeloma and metastatic cancer were excluded. The precipitating events leading to the fracture were fall in 22 patients (48.8%), lift of a heavy object in 5 (11.1%), and no recollection of trauma in 18 (40%). The comorbidities were diabetes in 12 patients (26.7%) and rheumatoid arthritis in four (8.9%) take steroids. For neurological findings, 10 patients had a hyperreflexia and 19 a hyporeflexia in their legs. Twenty-five patients had a sensory deficit. Eleven patients had a sphincter dysfunction.
Eight patients were managed with posterior decompression and fusion surgery, 23 vertebroplasty, and 14 conservative therapies such as a corset or analgesics.
Radiological assessment
Local kyphosis was calculated as the Cobb angle between the cranial endplate of the vertebra just cranial to the fracture and the caudal endplate of the vertebra just caudal to the fractured vertebra on lateral plain X-ray films (Fig. 1). Angular instability was calculated as change in vertebral wedge angle on lateral dynamic radiography. Ratio of occupation by bony fragments of the spinal canal was calculated as the ratio in percentage of sagittal diameter of bony fragments to sagittal diameter of the spinal canal on mid-sagittal MR images.
Fig. 1.
Radiological assessment. a Local kyphosis was calculated as Cobb angle between the upper endplate of the vertebra just cranial to the fractured vertebra and the inferior endplate of the vertebra just caudal to the fractured vertebra on lateral plain X-ray films. b, c Angular instability was calculated as change in Cobb angle on lateral dynamic radiography (b extension, c flexion). d Ratio of occupation by bony fragments of the spinal canal was calculated as ratio in percentage of bony fragment diameter to adjacent normal canal diameter on mid-sagittal MR images
Statistical analysis
As response variables, severities of neurological deficits and of back pain were each graded using three levels. For neurological deficits, “none” was defined as no neurological deficit, “mild” as Manual Muscle Test (MMT) score of grade 4, and “severe” as MMT score of grade 3 or less. For back pain, “none or mild” was defined as VAS score less than 30, “moderate” as VAS score from 30 to 70, and “severe” as VAS score above 70.
Explanatory variables included age, sex, level of fracture, duration of symptoms after onset, angle of local kyphosis, degree of angular instability, ratio of occupation by bony fragments of the spinal canal, presence or absence of protrusion of flavum in the spinal canal, and presence or absence of ossification of the anterior longitudinal ligament (OALL) in the adjacent level. Continuous variables (angle of local kyphosis, degree of angular instability, and ratio of occupation by bony fragments of the spinal canal) were categorized by approximate tertile, except for age, and duration of fracture. Levels of fracture were divided into three categories. The first category was the level cranial to T12, that of the spinal cord. The second category was the level of L1, that of the conus medullaris. The third category was L2 and caudal to L2, the levels of the cauda equina. Other characteristics were treated as dichotomous variables (male/female for sex, present/absent for protrusion of flavum, or adjacent OALL).
To express the associations between severe neurological deficits or severe back pain and explanatory variables, odds ratio (ORs) and their 95% confidence intervals (CIs) were computed using the proportional odds model in logistic regression. We calculated P values for the scores to test the proportional odds assumption in order to confirm that use of the proportional odds model would be appropriate for these models.
All analyses were performed using Statistical Analysis System Version 9.1 (SAS Institute, Inc., Cary, NC, USA). Findings of P < 0.05 were considered significant.
Results
Patient demographic variables are shown in Table 1. Overall, 46.7% of patients exhibited mild or severe neurological deficits, with findings of less than grade 4 on MMT, and 84.4% had moderate or severe back pain, with a VAS score of more than 30.
Table 1.
Patient demographics
| Characteristics | No. of subjects | Mean or percent |
|---|---|---|
| Mean age (years) | 74.0 | |
| Mean duration of fracture (months) | 6.9 | |
| Sex | ||
| Male | 10 | 22.2% |
| Female | 35 | 77.8% |
| Level of injury | ||
| L2 or below | 8 | 17.8% |
| L1 | 11 | 24.4% |
| T12 or above | 26 | 57.8% |
| Mean local kyphosis (°) | 24.8 | |
| Mean angular instability (°) | 11.4 | |
| Mean ratio of occupation by bony fragments (%) | 38.1 | |
| Protrusion of flavum | ||
| Absent | 36 | 80% |
| Present | 9 | 20% |
| Adjacent OALL | ||
| Absent | 31 | 71.1% |
| Present | 13 | 28.9% |
| Neurological deficits | ||
| None | 24 | 53.3% |
| Mild | 10 | 22.2% |
| Severe | 11 | 24.5% |
| Back pain | ||
| None or mild | 7 | 15.6% |
| Moderate | 16 | 35.6% |
| Severe | 22 | 48.8% |
Neurological deficits
Table 2 shows the associations between explanatory variables and severity of neurological deficits. Univariate analysis showed that pronounced angular instability within the affected vertebral body of more than 15° significantly increased the OR of neurological deficits [crude OR, 10.0 (95%CI 2.12–47.7); P < 0.01]. Marked spinal canal encroachment by protruding bony fragments was also a factor significantly contributing to neurological deficits. ORs were 6.74 (95%CI 1.11–40.9, P < 0.05) for moderate protrusion from 33 to 41% and 11.9 [(95%CI 2.11–68.0); P < 0.01] for severe protrusion of more than 42%. No other explanatory variables examined significantly contributed to neurological deficits on univariate analysis.
Table 2.
Univariate and multivariate ORs for severity of neurological deficits
| Characteristics | Neurological deficits | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|
| None | Mild | Severe | OR (95%CI) | P value | OR (95%CI) | P value | |
| n | n | n | |||||
| Age (year) per 1 year | 0.96 (0.89–1.04) | 0.341 | 0.91 (0.82–1.02) | 0.106 | |||
| Sex | |||||||
| Male | 5 | 4 | 1 | 1 | 1 | ||
| Female | 19 | 6 | 10 | 1.20 (0.31–4.66) | 0.794 | 0.66 (0.12–3.69) | 0.634 |
| Level of injury | |||||||
| L2 or below | 4 | 4 | 0 | 1 | 1 | ||
| L1 | 6 | 2 | 3 | 2.09 (0.37–11.8) | 0.406 | 3.31 (0.31–35.6) | 0.323 |
| T12 or above | 14 | 4 | 8 | 2.06 (0.47–9.05) | 0.341 | 4.87 (0.66–35.9) | 0.120 |
| Duration of fracture (month) per 1 month | 0.96 (0.85–1.08) | 0.532 | 0.99 (0.84–1.18) | 0.932 | |||
| Local kyphosis (°) | |||||||
| −21 | 5 | 6 | 2 | 1 | 1 | ||
| 22–28 | 10 | 3 | 2 | 0.45 (0.10–1.94) | 0.281 | 0.31 (0.04–2.44) | 0.263 |
| 29+ | 9 | 1 | 7 | 1.14 (0.29–4.37) | 0.855 | 0.62 (0.08–4.97) | 0.653 |
| Angular instability(°) | |||||||
| −7 | 12 | 1 | 2 | 1 | 1 | ||
| 8–14 | 7 | 5 | 1 | 2.59 (0.51–13.2) | 0.252 | 2.20 (0.25–19.6) | 0.479 |
| 15+ | 5 | 4 | 8 | 10.0 (2.12–47.7) | 0.004 | 9.24 (1.49–57.2) | 0.017 |
| Ratio of occupation by bony fragments (%) | |||||||
| −32 | 12 | 1 | 1 | 1 | 1 | ||
| 33–41 | 5 | 6 | 2 | 6.74 (1.11–40.9) | 0.038 | 2.35 (0.29–18.9) | 0.421 |
| 42+ | 7 | 3 | 8 | 11.9 (2.11–68.0) | 0.005 | 9.23 (1.15–74.1) | 0.037 |
| Protrusion of flavum | |||||||
| Absent | 21 | 7 | 8 | 1 | 1 | ||
| Present | 3 | 3 | 3 | 2.27 (0.58–8.94) | 0.241 | 0.56 (0.08–4.06) | 0.569 |
| Adjacent OALL | |||||||
| Absent | 17 | 8 | 7 | 1 | 1 | ||
| Present | 7 | 2 | 4 | 1.15 (0.34–3.89) | 0.828 | 1.79 (0.35–9.26) | 0.483 |
OR odds ratio, CI confidence interval
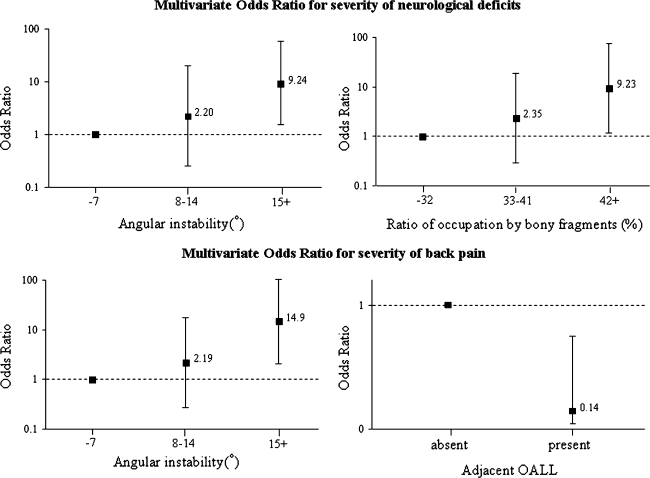
Multivariate analysis showed that pronounced angular instability in the upper tertile, of more than 15°, and high ratio of occupation by bony fragments, in the upper tertile of more than 42%, were factors significantly contributing to the degree of neurological deficit [adjusted OR 9.24 (95%CI 1.49–57.2); P < 0.05 and adjusted OR 9.23 (95%CI 1.15–74.1); P < 0.05, respectively]. No other variables examined were significant factors on multivariate analysis (Fig. 2).
Fig. 2.
Multivariate odds ratios for severity of neurological deficits and back pain. The y axis is on a log scale. The I bars denote 95% confidence intervals
Intractable back pain
Table 3 shows the associations between explanatory variables and severity of back pain in patients with insufficient union following OVF. Univariate analysis revealed that moderate angular instability ranging from 8° to 14° had an OR of 4.45 [(95%CI 1.01–19.6); P < 0.05)] while marked angular instability of more than 15° had an OR of 9.83 [(95%CI 2.19–44.1); P < 0.01). No other variables examined were significant factors on univariate analysis.
Table 3.
Univariate and multivariate ORs for severity of back pain
| Characteristics | Back pain | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|
| None or mild | Moderate | Severe | OR (95%CI) | P value | OR (95%CI) | P value | |
| n | n | n | |||||
| Age (year) per 1 year | 0.98 (0.91–1.06) | 0.658 | 1.05 (0.94–1.18) | 0.406 | |||
| Sex | |||||||
| Male | 2 | 4 | 4 | 1 | 1 | ||
| Female | 5 | 12 | 18 | 1.56 (0.42–5.84) | 0.509 | 2.15 (0.43–10.6) | 0.348 |
| Level of injury | |||||||
| L2 or below | 0 | 2 | 6 | 1 | 1 | ||
| L1 | 1 | 7 | 3 | 0.24 (0.04–1.48) | 0.125 | 0.15 (0.01–213) | 0.160 |
| T12 or above | 6 | 7 | 13 | 0.30 (0.06–1.44) | 0.133 | 0.20 (0.02–1.96) | 0.165 |
| Duration of fracture (month) per 1 month | 0.96 (0.87–1.07) | 0.459 | 0.97 (0.83–1.14) | 0.715 | |||
| Local kyphosis (°) | |||||||
| −21 | 1 | 3 | 9 | 1 | 1 | ||
| 22–28 | 3 | 5 | 7 | 0.36 (0.08–1.63) | 0.186 | 0.72 (0.10–5.35) | 0.751 |
| 29+ | 3 | 8 | 6 | 0.28 (0.06–1.20) | 0.086 | 0.37 (0.04–3.36) | 0.377 |
| Angular instability(°) | |||||||
| −7 | 6 | 5 | 4 | 1 | 1 | ||
| 8–14 | 0 | 7 | 6 | 4.45 (1.01–19.6) | 0.048 | 2.19 (0.28–17.2) | 0.456 |
| 15+ | 1 | 4 | 12 | 9.83 (2.19–44.1) | 0.003 | 14.9 (2.11–105) | 0.007 |
| Ratio of occupation by bony fragments (%) | |||||||
| −32 | 3 | 5 | 6 | 1 | 1 | ||
| 33–41 | 1 | 3 | 9 | 3.19 (0.69–14.7) | 0.137 | 4.72 (0.65–34.2) | 0.124 |
| 42+ | 3 | 8 | 7 | 0.99 (0.27–3.63) | 0.983 | 0.47 (0.07–3.29) | 0.445 |
| Protrusion of flavum | |||||||
| Absent | 5 | 13 | 18 | 1 | 1 | ||
| Present | 2 | 3 | 4 | 0.72 (0.18–2.84) | 0.958 | 4.04 (0.47–34.6) | 0.202 |
| Adjacent OALL | |||||||
| Absent | 3 | 11 | 18 | 1 | 1 | ||
| Present | 4 | 5 | 4 | 0.30 (0.09–1.05) | 0.059 | 0.14 (0.03–0.76) | 0.023 |
OR odds ratio, CI confidence interval
Multivariate analysis showed that pronounced angular instability of more than 15° was a factor significantly contributing to intractable pain [adjusted OR 14.9 (95%CI 2.11–105); P < 0.01]. On the other hand, the existence of OALL in the level adjacent to the fracture was a factor reducing the degree of back pain [adjusted OR 0.14 (95%CI 0.03–0.76); P < 0.05]. No other variables examined were significant factors on multivariate analysis.
Discussion
The pain associated with OVF usually improves if there is no severe residual deformity. Ettinger et al. reported that vertebral deformities cause marked back pain if vertebral height ratios fall four standard deviations below the normal mean [6]. However, pseudoarthrosis following OVF has recently come to be considered a poor prognostic factor for prolonged and intractable pain [10, 14, 16]. On the other hand, Hashidate et al. reported that in 66.7% of patients back pain decreased naturally despite the presence of vertebral instability in cases of vertebral pseudoarthrosis [11]. Thus, not all patients with non-union exhibited prolonged and intractable back pain. As noted above, the factors causing prolonged and intractable back pain in the case of insufficient bone union following OVF are still unknown. Toyone et al. reported a significant correlation between back pain and changes in wedging rate from supine to standing positions for OVF of recent onset [31]. In the present study, marked angular instability of the affected vertebral body significantly contributed to severity of back pain.
The presence of an intravertebral cleft had been reported to be a risk factor for progressive vertebral collapse inducing neurological deficits [15, 17]. A few previous studies investigated the relationship between neurological deficits and radiological findings. Hashimoto et al. reported that ratios of occupation by bone fragments in the spinal canal of more than 35% at epiconus level, more than 45% at conus medullaris level, and more than 55% at cauda equina level were factors significantly associated with neurological impairment in traumatic burst fracture [12]. Trafton et al. reported that burst fracture at T12 or L1 with canal encroachment of more than 50% of mid-sagittal canal diameter was a significant risk factor for neurological impairment [32]. These reports were both on acute traumatic vertebral fracture. Nguyen et al. reported a series of ten patients with osteoporotic vertebral burst fracture, which led to varying degrees of neurologic compromise. In their cases, mean canal compromise was 41% [21]. No reports were found in our review of the literature on the relationship between neurological deficits and intravertebral instability. Baba et al. reported 27 patients who suffered osteoporotic vertebral collapse with late neurological complications. They considered the pathology in this lesion to involve abnormal hypermobility at the fractured spinal level with gradual retropulsion of fractured fragments into the spinal canal, resulting in late paralysis [1].
In the present study, it was found that intravertebral instability contributes to the degree of neurological deficits in cases of insufficient union following OVF. Stabilization of the lesion site without decompression is, thus, a treatment option for this condition. Some studies have reported that treatment with immobilization without decompression, such as conservative management using a plaster body cast, vertebroplasty, or posterior in situ stabilization, could result in neurological improvement with progression of bone union [3, 5, 30]. These findings suggest that spinal instability is related to the pathogenesis of neurological deficits.
In this study, the factors significantly contributing to neurological deficits were angular instability of more than 15° and ratio of occupation by bony fragments of the spinal canal of more than 42%. The factors contributing to severity of back pain were angular instability of more than 15° and absence of OALL in the adjacent segment. As noted above, intravertebral angular instability was a factor common to neurological deficits and back pain. Stabilization of the fractured vertebra thus appears to be the most important treatment option for insufficient fracture following OVF. In patients with bony encroachment of higher percentage, decompression is needed to obtain satisfactory surgical results.
Conclusions
In conclusion, we investigated the factors contributing to the severity of symptoms in patients with insufficient union following OVF. Factors significantly contributing to the severity of neurological deficits were angular instability of more than 15° within the affected vertebral body and ratio of occupation by bony fragments in the spinal canal of more than 42%. Factors significantly contributing to the severity of back pain were angular instability of more than 15° and absence of adjacent OALL. Angular instability was thus a factor common to both neurological deficits and prolonged back pain.
References
- 1.Baba H, Maezawa Y, Kamitani K, Furusawa N, Imura S, Tomita K. Osteoporotic vertebral collapse with late neurological complications. Paraplegia. 1995;33:281–289. doi: 10.1038/sc.1995.64. [DOI] [PubMed] [Google Scholar]
- 2.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000;25:923–928. doi: 10.1097/00007632-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 3.Braakman R, Fontijne WP, Zeegers R, Steenbeek JR, Tanghe HL. Neurological deficit in injuries of the thoracic and lumbar spine. A consecutive series of 70 patients. Acta Neurochir (Wien) 1991;111:11–17. doi: 10.1007/BF01402507. [DOI] [PubMed] [Google Scholar]
- 4.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 5.Klerk LW, Fontijne WP, Stijnen T, Braakman R, Tanghe HL, Linge B. Spontaneous remodeling of the spinal canal after conservative management of thoracolumbar burst fractures. Spine. 1998;23:1057–1060. doi: 10.1097/00007632-199805010-00018. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK. Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1992;7:449–456. doi: 10.1002/jbmr.5650070413. [DOI] [PubMed] [Google Scholar]
- 7.Fujiwara S. Epidemiology of osteoporosis in Japan. J Bone Miner Metab. 2005;23(Suppl):81–83. doi: 10.1007/BF03026329. [DOI] [PubMed] [Google Scholar]
- 8.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26:1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 9.Gertzbein SD, Harris MB. Wedge osteotomy for the correction of post-traumatic kyphosis. A new technique and a report of three cases. Spine. 1992;17:374–379. doi: 10.1097/00007632-199203000-00025. [DOI] [PubMed] [Google Scholar]
- 10.Hasegawa K, Homma T, Uchiyama S, Takahashi H. Vertebral pseudarthrosis in the osteoporotic spine. Spine. 1998;23:2201–2206. doi: 10.1097/00007632-199810150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Hashidate H, Kamimura M, Nakagawa H, Takahara K, Uchiyama S. Pseudoarthrosis of vertebral fracture:radiographic and characteristic clinical fractures and natural history. J Orthop Sci. 2006;11:28–33. doi: 10.1007/s00776-005-0967-8. [DOI] [PubMed] [Google Scholar]
- 12.Hashimoto T, Kaneda K, Abumi K. Relationship between traumatic spinal canal stenosis and neurologic deficits in thoracolumbar burst fractures. Spine. 1988;13:1268–1272. doi: 10.1097/00007632-198811000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Heggeness MH. Spine fracture with neurological deficit in osteoporosis. Osteoporos Int. 1993;3:215–221. doi: 10.1007/BF01623679. [DOI] [PubMed] [Google Scholar]
- 14.Hoshino M, Nakamura H, Konishi S, Nagayama R, Terai H, Tsujio T, Namikawa T, Kato M, Takaoka K. Endoscopic vertebroplasty for the treatment of chronic vertebral compression fracture. Technical note. J Neurosurg Spine. 2006;5:461–467. doi: 10.3171/spi.2006.5.5.461. [DOI] [PubMed] [Google Scholar]
- 15.Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2:101–106. doi: 10.1016/S1529-9430(01)00165-6. [DOI] [PubMed] [Google Scholar]
- 16.Jang JS, Kim DY, Lee SH. Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine. 2003;28:1588–1592. doi: 10.1097/00007632-200307150-00021. [DOI] [PubMed] [Google Scholar]
- 17.Kaneda K, Asano S, Hashimoto T, Satoh S, Fujiya M. The treatment of osteoporotic posttraumatic vertebral collapse using the Kaneda device and bioactive ceramic vertebral prosthesis. Spine. 1992;17:S295–S303. doi: 10.1097/00007632-199208001-00015. [DOI] [PubMed] [Google Scholar]
- 18.Kim DY, Lee SH, Jang JS, Chung SK, Lee HY. Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg. 2004;100:24–31. doi: 10.3171/jns.2004.100.1.0024. [DOI] [PubMed] [Google Scholar]
- 19.Lafforgue P, Chagnaud C, Daumen-Legre V, Daver L, Kasbarian M, Acquaviva PC. The intravertebral vacuum phenomenon (“vertebral osteonecrosis”). Migration of intradiscal gas in a fractured vertebral body? Spine. 1997;22:1885–1891. doi: 10.1097/00007632-199708150-00015. [DOI] [PubMed] [Google Scholar]
- 20.Mochida J, Toh E, Chiba M, Nishimura K. Treatment of osteoporotic late collapse of a vertebral body of thoracic and lumbar spine. J Spinal Disord. 2001;14:393–398. doi: 10.1097/00002517-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen HV, Ludwig S, Gelb D. Osteoporotic vertebral burst fractures with neurologic compromise. J Spinal Disord Tech. 2003;16:10–19. doi: 10.1097/00024720-200302000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Peh WC, Gelbart MS, Gilula LA, Peck DD. Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol. 2003;180:1411–1417. doi: 10.2214/ajr.180.5.1801411. [DOI] [PubMed] [Google Scholar]
- 23.Phillips FM. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine. 2003;28:S45–S53. doi: 10.1097/00007632-200308011-00009. [DOI] [PubMed] [Google Scholar]
- 24.Ross PD, Fujiwara S, Huang C, Davis JW, Epstein RS, Wasnich RD, Kodama K, Melton LJ., III Vertebral fracture prevalence in women in Hiroshima compared to Caucasians or Japanese in the US. Int J Epidemiol. 1995;24:1171–1177. doi: 10.1093/ije/24.6.1171. [DOI] [PubMed] [Google Scholar]
- 25.Saita K, Hoshino Y, Kikkawa I, Nakamura H. Posterior spinal shortening for paraplegia after vertebral collapse caused by osteoporosis. Spine. 2000;25:2832–2835. doi: 10.1097/00007632-200011010-00018. [DOI] [PubMed] [Google Scholar]
- 26.Sarli M, Perez Manghi FC, Gallo R, Zanchetta JR. The vacuum cleft sign: an uncommon radiological sign. Osteoporos Int. 2005;16:1210–1214. doi: 10.1007/s00198-005-1833-4. [DOI] [PubMed] [Google Scholar]
- 27.Suk SI, Kim JH, Lee SM, Chung ER, Lee JH. Anterior–posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine. 2003;28:2170–2175. doi: 10.1097/01.BRS.0000090889.45158.5A. [DOI] [PubMed] [Google Scholar]
- 28.Suzuki N, Ogikubo O, Hansson T. The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months. Eur Spine J. 2008;17:1380–1390. doi: 10.1007/s00586-008-0753-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Theodorou DJ. The intravertebral vacuum cleft sign. Radiology. 2001;221:787–788. doi: 10.1148/radiol.2213991129. [DOI] [PubMed] [Google Scholar]
- 30.Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. The treatment of acute thoracolumbar burst fractures with transpedicular intracorporeal hydroxyapatite grafting following indirect reduction and pedicle screw fixation: a prospective study. Spine. 2006;31:E208–E214. doi: 10.1097/01.brs.0000208161.74286.ad. [DOI] [PubMed] [Google Scholar]
- 31.Toyone T, Tanaka T, Wada Y, Kamikawa K, Ito M, Kimura K, Yamasita T, Matsushita S, Shiboi R, Kato D, Kaneyama R, Otsuka M. Changes in vertebral wedging rate between supine and standing position and its association with back pain: a prospective study in patients with osteoporotic vertebral compression fractures. Spine. 2006;31:2963–2966. doi: 10.1097/01.brs.0000247802.91724.7e. [DOI] [PubMed] [Google Scholar]
- 32.Trafton PG, Boyd CA., Jr Computed tomography of thoracic and lumbar spine injuries. J Trauma. 1984;24:506–515. doi: 10.1097/00005373-198406000-00008. [DOI] [PubMed] [Google Scholar]