Abstract
Discal cyst is a very rare lesion that can cause refractory low back pain and radiating leg pain. Although there are some reports to remove this lesion, there has been no report of discal cyst removed by percutaneous endoscopic transforaminal approach. Two young patients manifested left gluteal and leg pain due to a discal cyst at L5–S1 level and L4–5 level, respectively. Percutaneous endoscopic transforaminal approach was performed to remove the discal cyst, achieving complete decompression of the nerve root. The symptom was relieved and the patient was discharged the next day. Percutaneous endoscopic transforaminal approach could be a good alternative option in selected cases for the treatment of lumbar discal cyst.
Keywords: Lumbar, Discal cyst, Percutaneous, Endoscopic transforaminal approach
Introduction
Discal cysts arise from spinal discs [1, 2, 10, 12]. As the cyst grows, particularly when it arises due to degenerative disc changes, it could cause radiculopathy, such as lumbar disc herniation. The authors report rare cases of discal cysts that originated from the posterior margin of the lumbar disc, and discuss their clinical, radiological, and surgical findings.
Case report
Surgical technique
These procedures were performed with the patients under local anesthesia in the prone position on a radiolucent table under the guidance of C-arm fluoroscopy. The midline as well as the extent of the iliac crest was marked with a marking pen. The skin entry point was usually about 10–12 cm from the midline for the L4–L5 and L5–S1 levels. After the entry point was numbed with local anesthetics, an 18-gauge spinal needle was introduced under fluoroscopic image guidance. The target of the spinal needle was the medial pedicular line on the anteroposterior image and the posterior vertebral line on the lateral image. After the insertion of a spinal needle into the disc, an intraoperative discogram was performed with a 2-ml mixture of radio opaque dye (Telebrix, Guerbet, France), indigo carmine (Carmine, Korea United Pharmaceutical, Seoul, South Korea), and normal saline in the ratio of 2:1:2. The dye leaks through the tear in the annulus in the epidural space, and indigo carmine stains the degenerated acidic nucleus blue, helping to identify the herniated fragment. The next steps were as follows; (1) A guide wire was inserted through the spinal needle, (2) the spinal needle was removed, (3) a small skin incision was made at the skin entry site, (4) a tapered, cannulated obturator was inserted along the guide wire. (5) After touching the annulus, an obturator was inserted into the disc after the annulotomy was performed. Finally, (6) a bevel-shaped, oval working cannula was inserted into the disc along the obturator and then the obturator was removed. The appropriate position of the working cannula to remove a discal cyst is shown in (Fig. 1).
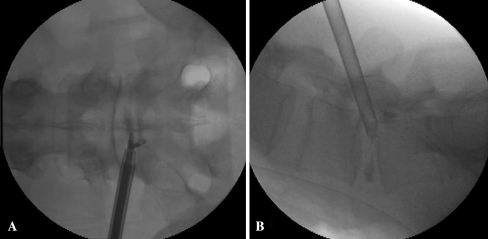
Fig. 1.
a Fluoroscopic images showing the position of the tip of working cannula in anteroposterior view. See the endoscopic forceps grasping the discal cyst in downward direction. b Fluoroscopic images showing the position of the tip of working cannula anchored in the subannulus in the lateral view, and the slight downward inclination of the needle trajectory on lateral view
Through this cannula, manual partial discectomy is performed in the subannular region to secure adequate space to handle the working cannula under fluoroscopic guidance. An endoscope with a working channel and two irrigation channels is introduced. At this time, the blue-stained annular surface and part of the disc material could be observed under endoscopic visualization. To gain access to the discal cyst, widening the sidewalls of the annular fissure is performed using a radiofrequency electrode (Ellman International, Hewlett, NY, USA), and a side-firing Holmium: Yttrium–Aluminum–Garnet laser (Trimedyne Inc., Irvine, CA, USA). After clearing the endoscopic visualization, the authors could remove the extruded disc fragments and discal cyst.
After that, we could identify the decompressed thecal sac and nerve root. One day after the operation, the patient was ambulatory and without pain. The traversing nerve root was successfully decompressed and the result was confirmed by postoperative magnetic resonance imagings (MRIs). Pathological studies showed a collagenous fibrous wall with no synovial lining cell or inflammatory cell infiltration corresponding to the discal cyst.
Case 1
A 28-year-old male presented with complaints of radicular pain and numbness in the left gluteal region and the posterior aspects of thigh and leg. Physical examination demonstrated a positive straight leg raising sign at 20° on the left side. There was an objective weakness of the plantar flexion graded as 4. The ankle reflex had decreased on the left side. The patient had no fasciculation, muscle atrophy, or upper motor neuron signs. MRI showed an intraspinal extradural space-occupying lesion just caudal to the L5–S1 disc space on the left side. The round lesion was isointense on a T1-weighted image and hyperintense on a T2-weighted sequence, suggesting a cystic lesion (Figs. 2, 3). The patient’s symptoms did not improve after conservative treatments, including medication and physiotherapy for 3 weeks. We performed a transforaminal percutaneous endoscopic approach. The thecal sac and S1 nerve root were successfully decompressed in endoscopic view (Fig. 4) and the result was confirmed on postoperative MRIs (Fig. 5).
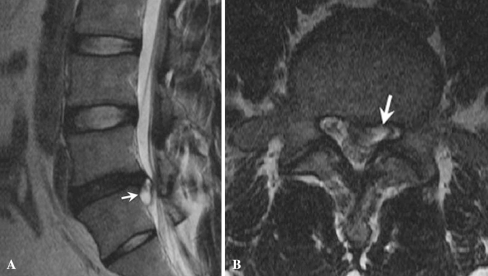
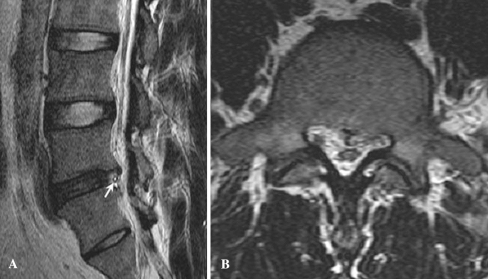
Fig. 2.
a Preoperative sagittal T2-weighted MRI showing a cystic lesion with a high signal intensity (white arrows) at L5–S1 disc level. b Preoperative axial T2-weighted MRIs showing a cystic lesion with high signal intensity (white arrows) compressing the S1 nerve root
Fig. 3.
a Preoperative sagittal T1-weighted MRI showing a cystic lesion with an iso signal intensity (white arrows) at L5–S1 disc level. b Preoperative axial T1-weighted MRIs showing a cystic lesion with iso signal intensity (white arrows) compressing S1 nerve root
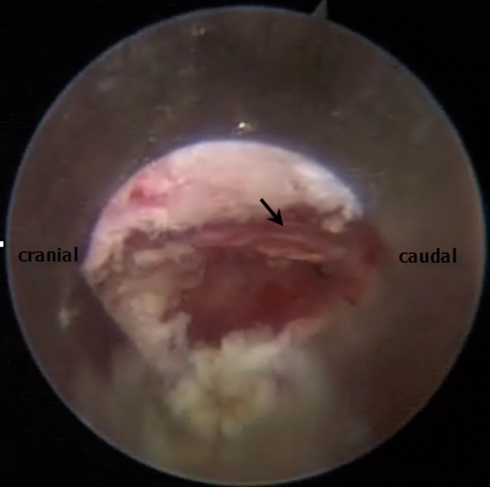
Fig. 4.
Endoscopic view showing superior facet at 12 O’clock, decompressed thecal sac and traversing S1 root (black arrow)
Fig. 5.
a Sagittal T2-weighted MRI obtained postoperatively, showing no residual cystic mass. See the tip of drain in subannular space (white arrow). b Axial T2-weighted MRI obtained postoperatively, showing decompressed S1 root
Case 2
A 27-year-old male presented with complaints of radicular pain in the left gluteal region and posterolateral aspects of his thigh and leg. Physical examination demonstrated a positive straight leg raising sign on the left side. There was an objective weakness of the tibialis anterior and extensor hallucis longus graded as 4/5. An MRI of the lumbar spine revealed the discal cyst that compressed the L5 root (Fig. 6). A computed tomography (CT) scan showed disc bulging without calcification. We performed a transforaminal percutaneous endoscopic approach. Histopathological examination identified the cyst wall that revealed fibrous connective tissue without lining cells in each case.
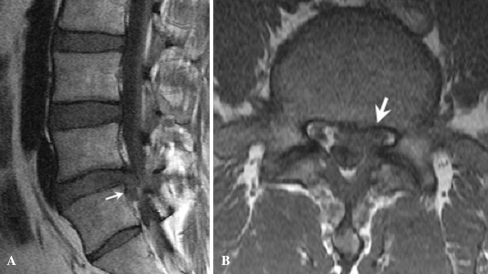
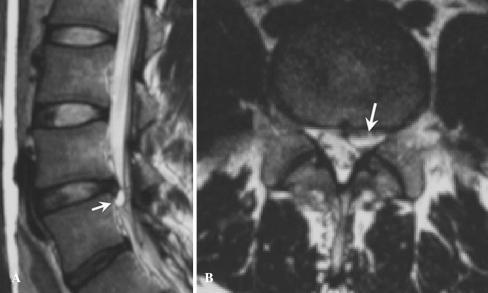
Fig. 6.
a Preoperative sagittal T2-weighted MRI showing a cystic lesion with a high signal intensity (white arrows) at L4–L5 disc level. b Preoperative axial T2-weighted MRIs showing a cystic lesion with high signal intensity (white arrows) compressing the L5 nerve root
Discussion
There are many kinds of cystic lesions within the spinal canal, including synovial cysts, arachnoid cysts, perineural cysts, cysts of the ligament flavum, ganglion cysts, and discal cysts [4, 5, 7, 9, 11, 13, 15, 16]. In contrast to other cysts, which usually develop in the connective tissue around the peripheral joint and tendon, a discal cyst is not common and has rarely been reported in the literature [1–3, 6, 8, 10, 12, 14]. The symptoms of a discal cyst vary. In our series, symptoms and signs were indistinguishable from a lumbar disc herniation, causing sciatica and nerve root tension because the cyst was located ventro-medially to the nerve root, compressing the root dorso-laterally. Because the differential diagnosis between discal cysts and other intraspinal cysts is based on the presence of lining cells surrounding the connective tissue, Nabeta et al. emphasized any strict distinction between the two in the clinical diagnosis is not need [12]. Another literature by Chiba et al. reported the importance of discography by which communication between the cyst and the corresponding disc was detected in their most cases [1].
In the literature [1, 14], some authors have summarized the characteristics of discal cysts; (1) All the cysts are located posterolateral to the vertebral body and just caudally located to the disc space, (2) the discs adjacent to the cysts also show degenerative bulging. There is associated disc degeneration, disc bulging, and disc protrusion in all cases, (3) a connection between the cyst and the corresponding intervertebral discs on discograms with severe radiating pain in the affected leg at the time of injection, and (4) in most cases, the direction of the cysts coincides with the direction of disc bulging.
It is supposed that disc degeneration may play an important role in the formation of the discal cyst, even though disc degeneration is not always the precursor of a cyst [1]. These findings were all compatible with our cases.
Various methods for removal of discal cysts have been performed. To date, surgical treatments including surgical excision, and percutaneous CT-guided punctures with steroid injections [8] have been reported and clinical outcomes of these treatments have been considered to be favorable. Chou et al. [2] first described spontaneous regression of a discal cyst after epidural injections and selective nerve blocks. However, nearly all reported discal cysts have been treated surgically or with some direct intervention, such as CT-guided aspirations and steroid injections. Recently, Ishii et al. [6] reported on a patient with a discal cyst who was treated using the METRx™ (Medtronic Sofamor Danek, Inc., Memphis, TN, USA) microendoscopic discectomy system and Min et al. [11] attempted to remove a synovial cyst of the facet joint in the lumbar spine by a percutaneous endoscopic transforaminal approach. They noted that excellent pain relief was achieved in patients using this procedure.
To our knowledge, however, no study has previously reported an endoscopic transforaminal approach for the treatment of a discal cyst. Since the discal cyst manifested symptoms and signs resembling those of lumbar disc herniation and its location was very similar to lumbar disc herniation, we considered a minimally invasive percutaneous endoscopic procedure for the treatment of the discal cyst. The success rate of percutaneous endoscopic procedures for lumbar disc herniation was also comparable to that of open surgery with the aid of specialized instruments. The procedure was successfully performed, and the unilateral radiculopathy subsided immediately after the procedure. The traversing nerve root was successfully decompressed and the result was confirmed by postoperative MRIs.
Conclusion
In this report, we performed a minimally invasive procedure using the percutaneous endoscopic transforaminal approach for a discal cyst in the lumbar spine with a successful outcome. Therefore, we suggest that discal cysts could be removed by a percutaneous endoscopic transforaminal approach in properly selected cases.
Acknowledgment
This study was sponsored by a fund from the Wooridul Spine Foundation.
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Nishizawa T. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: discal cyst. Spine. 2001;26(19):2112–2118. doi: 10.1097/00007632-200110010-00014. [DOI] [PubMed] [Google Scholar]
- 2.Chou D, Smith JS, Chin CT. Spontaneous regression of a discal cyst. Case report. J Neurosurg Spine. 2007;6:81–84. doi: 10.3171/spi.2007.6.1.81. [DOI] [PubMed] [Google Scholar]
- 3.Coscia MF, Broshears JR. Lumbar spine intracanalicular discal cysts: two case reports. J Spinal Disord Tech. 2002;15(5):431–435. doi: 10.1097/00024720-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: prevalence on magnetic resonance imaging. Spine. 2004;29:874–878. doi: 10.1097/00007632-200404150-00010. [DOI] [PubMed] [Google Scholar]
- 5.Hsu KY, Zucherman JF, Shea WJ, et al. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine. 1995;20:80–89. doi: 10.1097/00007632-199501000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Ishii K, Matsumoto M, Watanabe K, Nakamura M, Chiba K, Toyama Y. Endoscopic resection of cystic lesions in the lumbar spinal canal: a report of two cases. Minim Invasive Neurosurg. 2005;48:240–243. doi: 10.1055/s-2005-870927. [DOI] [PubMed] [Google Scholar]
- 7.Khan AM, Synnot K, Cammisa FP, Girardi FP. Lumbar synovial cysts of the spine: an evaluation of surgical outcome. J Spinal Disord Tech. 2005;18:127–131. doi: 10.1097/01.bsd.0000156830.68431.70. [DOI] [PubMed] [Google Scholar]
- 8.Koga H, Yone K, Yamamoto T, Komiya S. Percutaneous CT-guided puncture and steroid injection for the treatment of lumbar discal cyst: a case report. Spine. 2003;28:E212–E216. doi: 10.1097/00007632-200306010-00028. [DOI] [PubMed] [Google Scholar]
- 9.Langdown AJ, Grundy JR, Birch NC. The clinical relevance of Tarlov cysts. J Spinal Disord Tech. 2005;18:29–33. doi: 10.1097/01.bsd.0000133495.78245.71. [DOI] [PubMed] [Google Scholar]
- 10.Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC, Kahng SK, Roh SW, Rhim SC. Discal cyst of the lumbar spine: MR imaging features. Clin Imaging. 2006;30:326–330. doi: 10.1016/j.clinimag.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 11.Min JH, Chung BJ, Lee SH. Endoscopically managed synovial cyst of the lumbar spine. Korean J Spine. 2006;3:242–245. [Google Scholar]
- 12.Nabeta M, Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Discal cysts of the lumbar spine. Report of five cases. J Neurosurg Spine. 2007;6:85–89. doi: 10.3171/spi.2007.6.1.17. [DOI] [PubMed] [Google Scholar]
- 13.Ogawa Y, Kumano K, Hirabayashi S, Aota Y. A ganglion cyst in the lumbar spinal canal. A case report. Spine. 1992;17:1429–1431. doi: 10.1097/00007632-199211000-00030. [DOI] [PubMed] [Google Scholar]
- 14.Roh SW, Rhim SC, Lee HK, Kang SK. Spinal ganglion cyst of lumbar posterior longitudinal ligament. J Korean Neurosurg Soc. 2000;29:543–549. [Google Scholar]
- 15.Sato K, Nagata K, Sugita Y. Spinal extradural meningeal cyst: correct radiological and histopathological diagnosis. Neurosurg Focus. 2002;13:ecp 1. doi: 10.3171/foc.2002.13.4.8. [DOI] [PubMed] [Google Scholar]
- 16.Wildi LM, Kurrer MO, Benini A, Weishaupt D, Michel BA, Brühlmann P. Pseudocystic degeneration of the lumbar ligamentum flavum: a little known entity. J Spinal Disord Tech. 2004;17:395–400. doi: 10.1097/01.bsd.0000109837.59382.0e. [DOI] [PubMed] [Google Scholar]