Abstract
We present the case of a 62-year-old gentleman who presented with an epidural abscess and vertebral osteomyelitis secondary to a spontaneous rupture of the oesophagus. The causative organisms were Candida and Lactobacillus. This has not been recorded previously in the literature. Cases of vertebral osteomyelitis and epidural abscess secondary to oesophageal rupture are rare, and diagnosis is often delayed.
Keywords: Epidural abscess, Vertebral osteomyelitis, Oesophageal rupture
Case report
A 62-year-old gentleman with a known history of type 2 diabetes mellitus, diabetic retinopathy and hypertension was admitted to hospital in the United States with pneumonia. He was diagnosed with Chlamydia pneumonia, which improved with antibiotics. Two weeks following admission he developed neck pain, associated with weakness and pins and needles in both upper limbs, and difficulty walking. He subsequently had an episode of severe choking followed by a cardiac arrest. He was resuscitated, including intubation, and was later successfully extubated, but was noted to have a weak voice afterwards. Investigations at that time included c-spine X-rays and an MRI, which revealed a large prevertebral collection, and evidence of an epidural abscess with discitis. This was assumed to be secondary to a Staphylococcus aureus infection, and was treated with a combination of vancomycin and cefotaxime. His neurology improved with antibiotics, and a barium swallow was later performed which revealed an oesophageal defect and associated residual pocket of barium in the anterior midline of his neck.
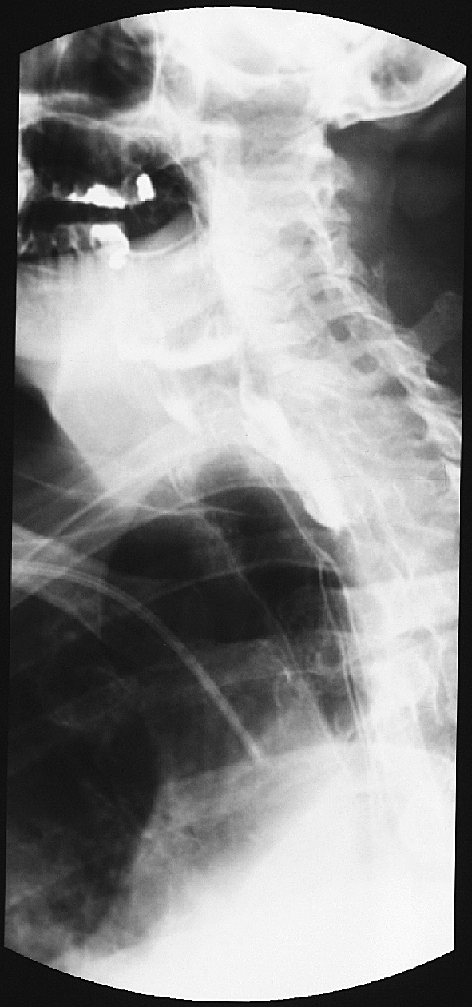
He was repatriated to Britain several weeks later, and admitted to the Queen’s Medical Centre, Nottingham. He was GCS 15, with power 4+/5 in his C7 myotomes bilaterally, but otherwise power 5/5 throughout, with normal sensation. His voice was noted to be hoarse. His initial investigations revealed a WCC of 14.7 (neutrophils 11.72) and CRP 13. A Speech and Language Therapy assessment was performed, which noted dysphagia and hoarseness, with coughing and aspiration on thick and thin fluids, and variable laryngeal elevation. He was subsequently prevented from taking fluid or food orally, and an ENT opinion was recommended. An MRI scan (Fig. 1) revealed C6/7 discitis with an anterior epidural collection causing compression and a prevertebral collection (predominantly right-sided). A barium swallow revealed a residual pocket of contrast in the lower neck (Fig. 2). He underwent a CT-guided aspiration, which revealed gram positive cocci and gram negative bacilli, and he was continued on vancomycin and cefotaxime, with metronidazole added, pending further microbiological results.
Fig. 1.
MRI on admission showing C6/7 discitis with an anterior epidural collection causing compression and a prevertebral collection (predominantly right-sided)
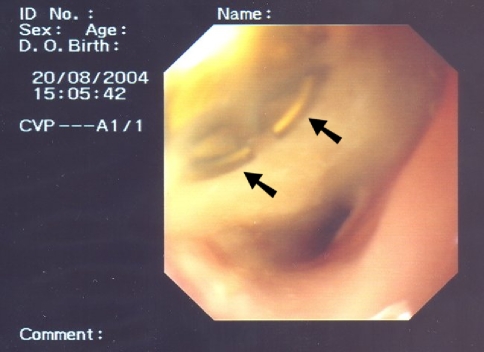
Fig. 2.
Barium swallow following admission, revealing a residual pocket of contrast in the lower neck
On the morning following the procedure, the patient was found unresponsive, GCS 3, which improved to 12 and then 15 with airway management. He was taken to theatre the same day, and underwent a C6/7 partial vertebrectomy and drainage of his cervical epidural abscess via an anterior approach. He was found to have a right-sided abscess around his carotid artery and extending deep. Pus was drained from the C6/7 disc space, and he had a partial C6 and complete C7 vertebrectomy, with an iliac crest graft inserted and secured with two screws. He was taken to ITU post-operatively, but returned to the ward the following day.
Microbiology results revealed Candida from the CT-guided aspiration, and Candida and Lactobacillus from the pus and bone samples taken in theatre. Histology revealed Candida osteomyelitis. These results suggested an oesophageal leak as the route of infection, and an oesophagogastroduodenoscopy (OGD) was advised. Treatment was based on case reports due to the rare nature of the pathology, and the patient was commenced on ambizone (4 weeks), fluconazole po (5 months) and doxycycline (6 weeks). An ENT review was requested, which revealed a paretic right vocal cord, with no more than a flicker of movement. The left vocal cord was compensating. There was no evidence of upper aerodigestive tract Candida on examination. Video fluoroscopy was performed, which confirmed the abnormal collection of contrast on the right side of the pharynx, suggestive of a leak into the abscess cavity. An oesophagogastroduodenoscopy (OGD) was then performed, which visualised the two screws inserted during his previous operation (Fig. 3). He was therefore returned to theatre the same day, and had the screws removed. At this stage, he had an NG-tube placed, which was later replaced by a PEG tube.
Fig. 3.
Oesophagogastroduodenoscopy (OGD) visualising one of the two screws inserted during his previous operation
He had a complicated hospital course, but was transferred to a rehabilitation hospital approximately 3 months after this admission. He was discharged home from the rehabilitation hospital a month later (4 months after his repatriation to Britain), and at this stage he remained on fluconazole and doxycycline antibiotics.
Follow-up CT scans a month after his surgery revealed bone destruction of C5/6/7/T1, with no incorporation of the bone graft at this time (Fig. 4a, b). An MRI scan 3 months after this showed extensive destruction of the anterior bodies of C5–T1, spanned by the bone graft, and the presence of air in the retropharyngeal soft-tissues extending to the operative defect and vertebral bodies (Fig. 5). There were extensive inflammatory changes surrounding the vertebral bodies and perivertebral space, and a defect in the posterior pharyngeal wall, but no evidence of an epidural mass or abscess noted. He had his PEG removed 14 months after his admission to Queen’s Medical Centre, Nottingham. C-spine X-rays and an MRI 1 year after presentation showed a stable neck with no evidence of osteomyelitis. At his last review 17 months after presentation, he was independently mobile, eating normally, with no residual neurological deficit. His fluconazole had just been stopped, and he was still taking doxycycline, although this was subsequently stopped as his inflammatory markers were normal at the time of his 17-month review.
Fig. 4.
a, b Follow-up CT scans a month after his surgery revealing bone destruction of C5/6/7/T1, with no incorporation of the bone graft at this time
Fig. 5.

MRI scan 4 months after surgery showing extensive destruction of the anterior bodies of C5–T1, spanned by the bone graft, and the presence of air in the retropharyngeal soft-tissues extending to the operative defect and vertebral bodies
Literature review and discussion
There have been several cases in the literature on both vertebral osteomyelitis and epidural abscesses, some with combined pathologies. With regards to oesophageal perforation as the underlying cause, all recorded cases have been secondary to trauma. There are currently no cases of spontaneous oesophageal perforation leading to Candida and Lactobacillus infection in the literature.
Mattingly et al. [6] reported the case of a 54-year-old male with insulin-dependent diabetes mellitus, who presented with C6 and C7 osteomyelitis after oesophagoscopy for progressive dysphagia, who sustained an oesophageal perforation during the procedure. Cullen et al. [3] presented two cases of cervical osteomyelitis secondary to tracheo-oesophageal puncture, a technique used for establishing a tracheo-oesophageal fistula in laryngectomy patients. Barr et al. [2] described cervical osteomyelitis in a 61-year-old lady with portal hypertension and chronic liver disease, who underwent oesophagogastroduodenoscopy (OGD) for upper-GI haemorrhage. Frot-Martin et al. [4] described cervical osteomyelitis and epidural and prevertebral collections in a 56-year-old man who had sustained a severe injury requiring a period ventilated in ITU with an NG-tube in situ, and had developed a fistula from an oesophageal diverticulum to the prevertebral space at C4.
Vertebral osteomyelitis occurs in the cervical spine in between 3–11% of cases [1]. The mean age of occurrence is 57–60 years, with 66–87% of cases occurring in males, with medical co-morbidities (including diabetes) in 43–64% of the cases. The most common causes are haematogenous spread, or direct spread, such as from surgery, oesophageal perforation, or a contiguous focus. Delayed diagnosis is common, and delayed treatment increases the risk of neurological deterioration. Epidural abscesses co-exist with vertebral osteomyelitis in 44% of cases, with the most common site of spread being haematogenous (26%), in which the primary location of the abscess is the posterior aspect of the spinal canal, and direct spread of infection into the epidural space, in which case the primary site of the abscess is anterior. Co-morbidities are also often present [5].
The organisms most commonly responsible for vertebral osteomyelitis are Staphylococcus aureus (25–64%) and Streptococcus pyogenes (8–12%), with negative culture results in 31–42% of cases. Candida has also been recorded as a causative organism, along with Haemophilus influenzae, Salmonella and Nocardia [1]. In epidural abscess, Staphylococcus aureus is again the most common causative organism (57–73%), with other gram positive cocci (10%), gram negative organisms (18%), anaerobes (2%) and Mycobacterium tuberculosis (25%) also recorded. Disseminated fungal infections are rare, and usually occur in immunocompromised patients [5].
Conclusions
We present the case of a 62-year old gentleman who presented with vertebral osteomyelitis and epidural abscess secondary to a spontaneous ruptured oesophagus, with Candida and Lactobacillus as the causative organisms, which has not been recorded previously in the literature. Cases of vertebral osteomyelitis and epidural abscess secondary to oesophageal rupture are rare, and diagnosis is often delayed. Surgery to drain the abscess and debride osteomyelitis is required, both to confirm the underlying organism and to initiate correct antibiotic therapy, and to treat any neurological compression. If oesophageal perforation is suspected, then an oesophagogastroduodenoscopy (OGD) is essential to confirm the diagnosis.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Barnes B, Alexander JT, Branch CL., Jr Cervical osteomyelitis: a brief review. Neurosurg Focus. 2004;17:E11. doi: 10.3171/foc.2004.17.6.11. [DOI] [PubMed] [Google Scholar]
- 2.Barr RJ, Hannon DG, Adair IV, McCoy GF. Cervical osteomyelitis after rigid oesophagoscopy: brief report. J Bone Joint Surg. 1988;70-B:147–148. doi: 10.1302/0301-620X.70B1.3339050. [DOI] [PubMed] [Google Scholar]
- 3.Cullen JR, Primrose WJ, Vaughn CW. Osteomyelitis as a complication of a tracheo-oesophageal puncture. J Laryngol Otol. 1993;107:242–244. doi: 10.1017/s0022215100122753. [DOI] [PubMed] [Google Scholar]
- 4.Frot-Martin B, Carlier RY, Morand-Blot V, et al. Zenker’s diverticulum associated with multilevel cervical osteomyelitis. Spine. 2001;26(9):E193–E197. doi: 10.1097/00007632-200105010-00020. [DOI] [PubMed] [Google Scholar]
- 5.Mackenzie AR, Laing RBS, Smith CC, et al. Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry. 1998;65:209–212. doi: 10.1136/jnnp.65.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mattingly WT, Dillon ML, Todd EP. Cervical osteomyelitis after esophageal perforation. South Med J. 1992;75:626–627. doi: 10.1097/00007611-198205000-00036. [DOI] [PubMed] [Google Scholar]