Abstract
The objective of our study is to report a rare complication of halo pin insertion associated with an epileptic seizure and brain abscess, and to discuss the diagnostic and therapeutic approach to its management. The treatment of unstable cervical spine injuries with a halo vest is an established procedure. Complications of pin penetration such as brain abscess and seizure are rare, and need to be urgently treated. Intracranial abscess and seizure associated with the use of the halo device is an unusual complication, and only a few cases have been reported in the literature. A 21-year-old male had a halo vest placed for the management of an odontoid type II fracture, which he sustained from a motor vehicle accident. Ten weeks after halo ring placement he complained of headaches which relieved by analgesics. After 2 weeks he was admitted at the emergency unit in an unconscious condition after a generalized tonic-clonic seizure. The halo pins were displaced during the seizure and were removed at his admission. No drainage was noted from the pin sites, and a Philadelphia cervical collar was applied. A brain CT and MRI revealed intracranial penetration of both posterior pins and a brain abscess in the right parietal lobe. Computed tomography of the cervical spine revealed stable fusion of the odontoid fracture. Cultures from the pin sites were negative; however, intravenous wide spectrum antibiotic treatment was administered to the patient immediately for 4 weeks followed by oral antibiotics for additional 2 weeks. Anti-epileptic medication was also started at his admission. The patient was discharged from the hospital in 6 weeks without symptoms, continuing anti-epileptic medication. On the follow-up visits he had fully recovered without any neurologic sequelae. In conclusion, complications of halo pin penetration are rare which need immediate intervention. Any neurologic or infectious, local or generalized, symptom need to be investigated urgently with available imaging techniques and treated promptly. Pin over-tightening may cause bone penetration and possible deep cranial infection with serious complications.
Keywords: Odontoid fractures, Halo pin penetration, Brain abscess, Seizure
Introduction
Odontoid fractures account for approximately 20% of all cervical fractures and most of them are classified as type II fractures according to Anderson and D’Alonzo classification [1, 2, 4, 15]. The decision for operative or nonoperative treatment is still controversial [11, 12].
The treatment of unstable cervical spine injuries with a halo vest is an established procedure. The halo vest is commonly used for conservative treatment of an unstable cervical spine secondary to fractures, infections, neoplasms, inflammatory arthritis, and deformities [10, 17, 20].
Despite the advantages, application of a halo ring may result in complications such as pin loosening, pin site infection, pressure sores, dysphagia, and loss of reduction [5, 6]. Intracranial abscess and seizure associated with the use of the halo device is an unusual complication, and only a few cases have been reported in the literature [3, 6, 7, 9, 10, 13, 16, 18, 19, 22]. We present a case of a 21-year-old man with a brain abscess associated with epileptic seizure, after intracranial penetration of both posterior halo pins and a review of the literature.
Case report
A 21-year-old man sustained an isolated odontoid fracture after a motorbike accident, with no neurological deficits. He was admitted at the orthopedic department and treated with a halo vest, which was placed in situ to stabilize the cervical spine. The patient was discharged from the hospital 4 days after the application of the halo. The halo pins were tightened and checked 24 h after the insertion and at 2-week intervals. In 2 weeks of halo placement patient noted loosening of both posterior halo pins, which were retightened with a usual wrench. No signs of local infection at the pin sites were identified during the follow-up visits. The patient’s family was educated about the pin site care.
After 10 weeks and in between the follow-up visits he started suffering from periodic headaches which were relieved by analgesics. The patient was not seen by a doctor at this time and personally decided to start with analgesics. After 2 weeks and just 3 days before the arranged appointment for halo removal, the patient had a generalized tonic-clonic seizure, with tongue bite according to the statement of a general practitioner and was admitted at the emergency unit of our hospital in an unconscious condition. The halo pins were displaced during the seizure and were removed at his admission, no drainage was noted from the pin sites, and a Philadelphia cervical collar was applied.
The patient gained consciousness half an hour later, after receiving intravenous 20 mg diazepam, 500 mg epanutin, and 4 mg midazolam.
The neurological examination revealed a slight confusion with normal speech and orientation in time and place. Mobility, sensitivity, and cerebellum tests were normal and Babinsky reflex negative.
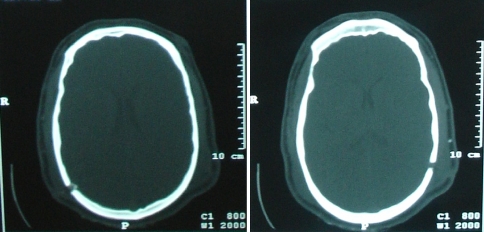
Immediate computed tomography (CT) of the brain showed intracranial penetration of both posterior halo pins at the parietal bones with a gap of the inner table. The right penetration site was associated with a brain abscess and surrounding cerebral edema (Figs. 1, 2). Cervical spine CT revealed a stable fusion of the dens fracture. Magnetic resonance imaging of the brain demonstrated a ring lesion enhanced with gadolinium and surrounding cerebral edema at the parietal lobe, diagnosed as brain abscess (Fig. 3).
Fig. 1.
CT scan of the brain showing intracranial penetration of both posterior halo pins at the parietal bones, with a gap of the inner table
Fig. 2.

The right penetration site was associated with a brain abscess and surrounding cerebral edema
Fig. 3.
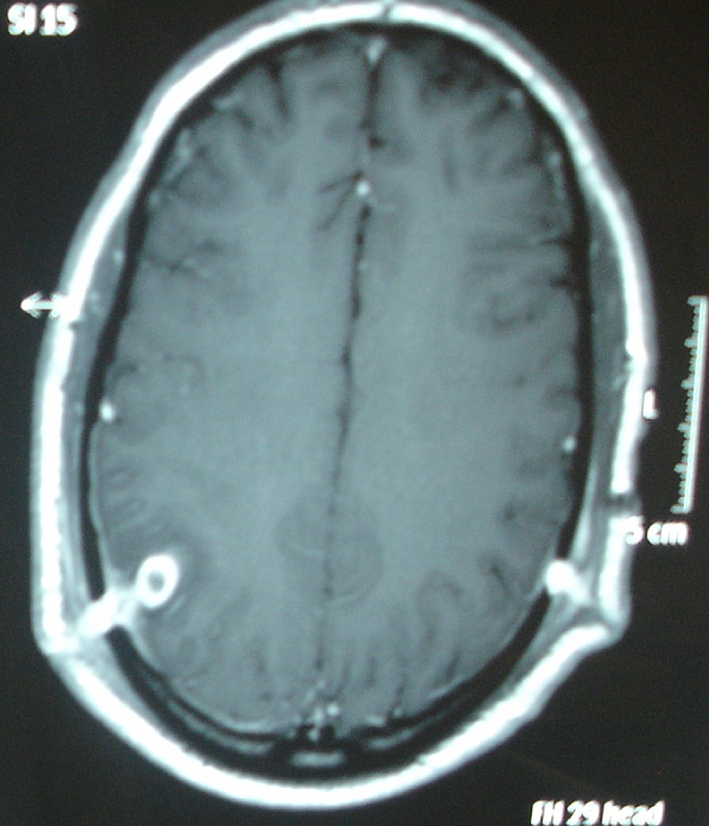
MRI of the brain demonstrated a ring lesion with surrounding cerebral edema at the parietal lobe, diagnosed as brain abscess
The patient was non-febrile, and the cultures from the pin sites were negative; however, intravenous wide spectrum antibiotic treatment consisted of vancomycin and ceftriaxone was administered immediately to the patient for 4 weeks followed by oral antibiotics for additional 2 weeks. The patient was also given epanutin and midazolam as anti-epileptic medication.
Ten days after his admittance to the hospital a bone scan revealed edema and inflammation of soft tissues around the penetration, with mild bone participation. After 3 weeks a second MRI of the brain was performed and demonstrated improvement with alleviation of the size of the abscess and the surrounding edema (Fig. 4).
Fig. 4.
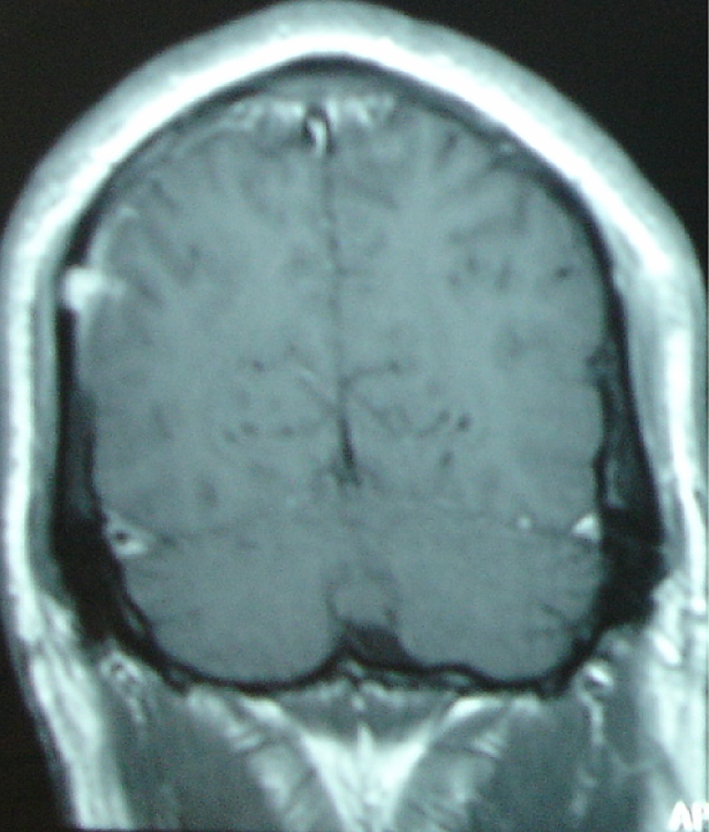
MRI of the brain after three weeks of intravenous antibiotic therapy, demonstrated improvement, with alleviation of the size of the abscess and the surrounding edema
The patient was discharged from the hospital in 6 weeks without symptoms, continuing anti-epileptic medication for a period of 10 months. The patient was followed up monthly for a year and had fully recovered without any neurologic sequelae.
Discussion
Complications of halo fixation device use are reported in detail by Garfin et al. In this comprehensive review of 179 patients they reported pin loosening in 36%, pin-site infection in 20%, pin discomfort in 18%, cosmetically disfiguring scars in 9%, nerve injuries in 2% and dural penetration in 1% of patients. In the same study 25% of 180 pins inserted were loose at least once and one-third of the loosed pins were associated with infection [5].
In a similar report of Glaser et al. [6], 14 of 245 patients with a halo device had pin related complications.
Intracranial pin penetration is a rare complication after halo pin insertion. It is usually associated with falls, over tightening of the pins, prolonged halo use, poor patient compliance, and improper pin placement [8].
Rizzolo et al. [17] reported the effect of torque application to the halo pins and the risk of skull penetration, concluding that halo pins must be inserted with a torque of 6 in./lb to minimize the risk of pin penetration and to allow retightening if required. In a similar study, Vertullo et al. [21] concluded that pin retightening at 24 h and at 1 week after halo application is a safe procedure minimizing pin-site complications.
Intracranial abscess is a serious and rare complication that needs urgent investigation and treatment. A few cases have been reported in the literature [3, 7, 9, 10, 13, 18, 19, 22]. It may result after penetration of the inner table of the skull and is usually manifested with local or generalized signs of infection, headache, seizure, psychosis, disorientation, lethargy, and aphasia [3, 7, 10, 14, 18, 19]. In a review of the literature Saeed et al. [19] reported 17 cases of halo-associated brain abscess, including their own case.
Epileptic seizures are usually associated with brain abscess; however, intracranial penetration has also been reported to cause epileptic seizure with no infection [10, 18]. Nottmeier et al. [14] reported a delayed onset of epileptic seizure due to scar tissue formation as a complication of halo orthosis.
We report the case of a patient with bilateral posterior pin penetration and brain abscess at the right parietal lobe developed 3 months after halo brace application, who had no signs of pin track infection or systemic symptoms before the seizure.
We believe that in our case a few factors have affected the outcome. Application of the halo brace in situ, in the patient’s room, inappropriate skin sterilization and finally over tightening of the screws, without the use of a special torque wrench, 2 weeks after the halo vest application are considered responsible for pin penetration and infection.
Conclusion
Complications of halo pin penetration are rare and need immediate intervention. Any neurologic or infectious, local or generalized, symptom need to be investigated urgently with available imaging techniques and treated promptly. Pin over-tightening may cause bone penetration and possible deep cranial infection with serious complications. The use of a special torque wrench is mandatory avoiding over-tightening and pin penetration.
Application technique with routine pin retightening at 24 h and 1 week after halo application is a safe method that minimizes the risk of halo pin penetration. Any patient with severe headaches, eye pain, neurological changes, systemic signs of infection, or seizure should be evaluated for brain abscess.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Aderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 2.Clark C, White A. Fractures of the dens: a multicenter study. J Bone Joint Surg Am. 1985;67:1340–1348. [PubMed] [Google Scholar]
- 3.Dennis GC, Clifton GL. Brain abscess as a complication of halo fixation. Neurosurgery. 1982;10:760–761. doi: 10.1097/00006123-198206010-00017. [DOI] [PubMed] [Google Scholar]
- 4.Frangen T, Zilkens C, Muhr G. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to Halo-Vest immobilization. J Trauma. 2007;63:83–89. doi: 10.1097/TA.0b013e318060d2b9. [DOI] [PubMed] [Google Scholar]
- 5.Garfin S, Botte M, Waters R. Complications in the use of halofixation device. J Bone Joint Surg Am. 1986;65:320–325. [PubMed] [Google Scholar]
- 6.Glaser J, Whitehill R, Stamp W. Complications associated with the halo vest. A review of 265 cases. J Neurosurg. 1986;65:762–769. doi: 10.3171/jns.1986.65.6.0762. [DOI] [PubMed] [Google Scholar]
- 7.Goodman ML, Nelson PB. Brain abscess complicating the use of a halo orthosis. Neurosurgery. 1987;20:27–30. doi: 10.1097/00006123-198701000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hashimoto Y, Doita M, Hasuda K, et al. Intracerebral pneumonocephalus and hemiparesis as a complication of a halo vest in a patient with multiple myeloma. J Neurosurg. 2004;100:367–371. doi: 10.3171/jns.2004.100.3.0367. [DOI] [PubMed] [Google Scholar]
- 9.Humbyrd DE, Latimer FR, Lonstein JE, et al. Brain abscess as a complication of halo traction. Spine. 1981;6:365–368. doi: 10.1097/00007632-198107000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Kingma R, Peters JM, Coene LNGEM. Intracranial penetration of a halo pin causing an epileptic seizure. J Bone Joint Surg Br. 2006;88:1654–1655. doi: 10.1302/0301-620X.88B12.17562. [DOI] [PubMed] [Google Scholar]
- 11.Koivikko M, Kiuru M, Koskinen S, et al. Factors associated with non-union in conservatively-treated type-II fractures of the odontoid process. J Bone Joint Surg Br. 2004;86:1146–1151. doi: 10.1302/0301-620X.86B8.14839. [DOI] [PubMed] [Google Scholar]
- 12.Komadina R, Brilej D, Kosanovic M, et al. Halo jacket in adontoid fractures type II and III. Arch Orthop Trauma Surg. 2003;123:64–67. doi: 10.1007/s00402-003-0473-4. [DOI] [PubMed] [Google Scholar]
- 13.Muller EJ, Wick M, Muhr G. Subdural absess as a complication of halo fixator. Unfallchirurg. 1998;101:655–657. doi: 10.1007/s001130050319. [DOI] [PubMed] [Google Scholar]
- 14.Nottmeier EW, Bondurany CP. Delayed onset of generalized tonic-clonic seizures as a complication of halo orthosis. Case report. J Neurosurg. 2000;92:233–235. doi: 10.3171/spi.2000.92.2.0233. [DOI] [PubMed] [Google Scholar]
- 15.Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36:54–64. doi: 10.1016/j.injury.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Platzer P, Thaihammer G, Sarahrudi K, et al. Nonoperative management of odontoid fractures using a halothoracic vest. Neurosurg. 2007;61:522–530. doi: 10.1227/01.NEU.0000290898.15567.21. [DOI] [PubMed] [Google Scholar]
- 17.Rizzolo SJ, Piazza MR, Cotler JM, et al. The effect of torque pressure on halo pin complication rates: a randomized prospective study. Spine. 1993;18:2163–2166. doi: 10.1097/00007632-199311000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Rosenblum D, Ehrlich V. Brain abscess and psychosis as a complication of a halo orthosis. Arch Phys Med Rehabil. 1995;76:865–867. doi: 10.1016/S0003-9993(95)80553-2. [DOI] [PubMed] [Google Scholar]
- 19.Saeed MU, Dacuycuy MAC, Kennedy DJ. Halo pin insertion associated brain abscess: case report and review of literature. Spine. 2007;32:271–274. doi: 10.1097/01.brs.0000259976.46403.8a. [DOI] [PubMed] [Google Scholar]
- 20.Strohm PC, Muller Ch A, Kostler W, et al. Halo-fixator vest—indications and complications. Zentralbl Chir. 2007;132:54–59. doi: 10.1055/s-2006-960479. [DOI] [PubMed] [Google Scholar]
- 21.Vertullo C, Duke P, Askin G, et al. Pin-site complications of the halo thoracic brace with routine pin re-tightening. Spine. 1997;22:2514–2516. doi: 10.1097/00007632-199711010-00010. [DOI] [PubMed] [Google Scholar]
- 22.Victor DI, Bresnan MJ, Keller RB. Brain abscess complicating the use of halo traction. J Bone Joint Surg Am. 1973;55:635–639. [PubMed] [Google Scholar]