Abstract
Hydatid disease is a parasitic tapeworm infection that usually involves liver and lungs. Primary skeletal muscle hydatid cyst without liver and lung involvement is rare. En bloc resection without inducing rupture and spreading the daughter cyst is recommended treatment strategy and accepted to be curative for intramuscular hydatid cyst. We report a case of primary hydatid cyst of the erector spinae muscle which was treated successfully with ultrasonography guided puncture, aspiration, injection of 95% ethanol and re-aspiration (PAIR) technique.
Keywords: Hydatid cyst, Skeletal muscle, Percutaneous treatment
Introduction
Hydatid disease is a parasitic tapeworm infection that usually involves liver and lungs. Primary skeletal muscle hydatid cyst without liver and lung involvement is rare even in endemic districts [1]. Currently, first treatment choice of muscular hydatid cyst is the combination of en bloc resection and albendazole chemotherapy [2]. On the other hand, puncture, aspiration, injection of scolicidal agent and re-aspiration (PAIR) is a non-operative technique which is now widely used for the treatment of liver hydatid cyst [13]. We report a case of primary hydatid cyst seated in erector spinae muscle which was treated successfully with PAIR technique.
Case report
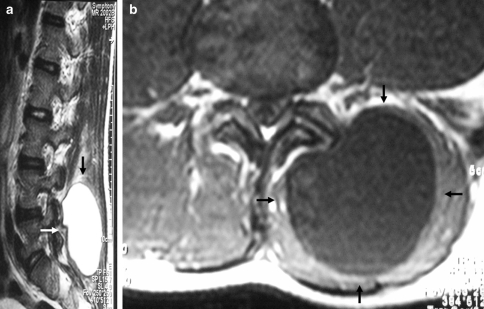
A 22-year-old man was admitted to our outpatient clinic with pain and a palpable mass in the left flank. The mass was present for 5 months and slowly increased in size. Routine physical examination was not significant and his past medical history was unremarkable except for the flank mass. All routine laboratory tests and direct radiographs were normal. Ultrasonographic examination revealed with maximal diameters of 5 × 5 cm thick walled hyperechogenic cyst situated in paraspinal muscle (Fig. 1a). MRI demonstrated a uni-ocular encapsulated cystic lesion with regular contours in the erector spinae muscle. The signal intensity of the cystic area was low on T1 sequences and uniformly high on T2 sequences, which is consistent with fluid. Both T1 and T2 sequences revealed that the lesion had a rim of low signal intensity. There was no evidence of bone destruction or mass effect on adjacent bone (Fig. 2).
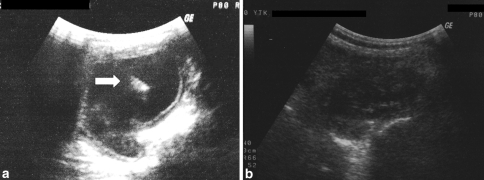
Fig. 1.
a Ultrasonographic appearance of the cyst at initial admission. Arrow shows the detached germinative membrane within the cyst indicating Type II hydatid cyst according to Gharbi classification. b Twenty-six months after the PAIR treatment, cyst showed decrease in dimensions, solidification of the content and thickening of the cyst wall
Fig. 2.
MRI of the hydatid cyst. a T1 axial sequence and b T2 sagittal sequence. Arrows show the cyst
Based on all these clinical and radiological data, the mass was suspected as hematoma, abcess or hydatid cyst. The echinococcal haemagglutination test (IHA) was negative and further imaging studies ruled out coexistent hydatid disease in other organs. En bloc resection of the cyst was planned but the patient refused the surgical operation.
The cyst was drained percutaneously with ultrasonographic guidance and then irrigated with 95% ethanol solution through a fine needle and reaspirated under local cutaneous anesthesia and sterile conditions. Albendazole (10 mg/kg/day) was administered 48 h before percutaneous drainage and for 3 months after the procedure to prevent the implantation of spilled scolices. During the procedure, fully equipped anesthesiology team was present in case of anaphylactic shock. Definitive diagnosis was confirmed by demonstrating protoscoleces and hydatid membranes in the liquid obtained by percutaneous aspiration of the cyst. At the final follow-up 26 months after the aspiration, patient was free of symptoms and ultrasonography revealed solidification of the cyst content, and thickening and irregularity of the cyst wall, all of which were considered as signs of cure (Fig. 1b).
Discussion
Primary hydatid disease of the skeletal muscle without liver and lung involvement is rare. Furthermore, paraspinal muscles are much more rarely affected [3, 12, 14]. The parasite has to cross pulmonary and hepatic filters to reach the muscles. High lactic acid level in muscle is regarded to be unsuitable for the parasite survival and muscular contractions prevent fixation of larva to the tissue [4, 6]. Sener et al. proposed an alternative mechanism explaining how the parasite gained access to the paraspinal muscles. According to his speculation, the parasite penetrated the intestinal muscle and directly entered into the inferior vena cava system through small venous connections between this system and portal circulation. Various conditions in daily life associated with Valsalva maneuver caused such an atypical passage of the parasite to the inferior caval system toward the retroperitoneum and spinal–paraspinal structures via lumbar epidural venous plexuses [12]. This alternative mechanism may be valid for the isolated paraspinal involvement as in our case. However, it does not explain the various reported lower and upper extremity isolated muscle involvements. Most probably, some parasite leak to the systemic circulation without being held by liver or lung.
Isolated muscular involvement in the absence of liver or lung hydatid disease is usually a diagnostic challenge both for the orthopedic surgeon and the radiologist. Serologic tests are valuable when they are positive but in half of the primary intramuscular hydatidosis case serology is false negative because the capsule isolates the parasite from the host’s immune system [8, 10]. Therefore, complete reliance on serology for definitive diagnosis is not recommended. Ultrasonography should be the first preferred imaging modality for the detection of muscular hydatid cyst as being a non-invasive method. It is also helpful in guiding the physician during aspiration and following up the course of disease. However, the extent of lesion, clear identification of involved structures and surgical planning may best be performed with magnetic resonance imaging [5].
Complete cure of the osseous involvement is a therapeutic challenge. The disease generally is not curable, and recurrence is likely. Surgery is the treatment of choice in osseous echinococcosis, although it can only eliminate the macroscopic cysts and local recurrence is reported half of the patients. However, en bloc resection without inducing rupture and spreading the daughter cyst is recommended treatment strategy and accepted to be curative for intramuscular hydatid disease [2, 4]. Puncture-aspiration-injection-reaspiration (PAIR) refers to an ultrasound guided technique consisting of puncture and evacuation of the contents of the hydatid cyst; injection of scolecidal agents such as 95% ethanol; and reaspiration of the contents of the cyst. This technique was first developed by Mueller et al. as an alternative treatment method against surgical excision of the liver hydatid cysts [7]. Although, puncture of a hydatid cyst has long been discouraged because of potential complications, such as anaphylactic shock or risk of iatrogenic spreading, there is an expanding literature suggesting that PAIR is effective for treatment of primary uncomplicated hepatic cysts [13]. However, this technique has been used for solid organ hydatid cysts. To our knowledge, there is only one study in which a modification of PAIR (percutaneous drainage without re-aspiration) has been used for the treatment of muscular hydatid cyst in the literature [9]. Herein, we report the first case of muscular hydatid cyst treated with PAIR technique combined with albendazole. In the presented case, patient did not accept the surgical excision. Thereafter, we performed percutaneous drainage, 95% ethanol injection and re-aspiration. Albendazole was given as an adjunctive therapy for the suspect of dissemination that might have been caused by needle aspiration [11]. Fortunately, neither procedure related complication nor recurrence was occured and the patient was free of symptoms at the 26 month follow-up.
Conclusion
Primary hydatid cyst of the erector spinae muscle without liver and lung involvement is extremely rare. In spite of the rarity, hydatid cyst should be included in the differential diagnosis of any cystic lesion of the soft tissue in endemic districts. The PAIR technique can be used as an alternative method of treatment in muscular hydatid cyst when en bloc resection could not be performed.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Ammari FF, Khasawneh Z, Salem MK, Mesmar M, Omari H, Masa’deh R. Hydatid disease of the musculoskeletal system. Surgery. 1998;124(5):934–937. [PubMed] [Google Scholar]
- 2.Arazi M, Erikoglu M, Odev K, Memik R, Ozdemir M. Primary echinococcus infestation of the bone and muscles. Clin Orthop Relat Res. 2005;432:234–241. doi: 10.1097/01.blo.0000149816.86222.2d. [DOI] [PubMed] [Google Scholar]
- 3.Atalay F, Orug T, Arda K, Tosun O, Atalay F. An unusual case of hydatid disease located in the erector spinae muscle. JBR-BTR. 2003;86(6):329–331. [PubMed] [Google Scholar]
- 4.Garcia-Alvarez F, Torcal J, Salinas JC, Navarro A, Garcia-Alvarez I, Navarro-Zorraquino M, et al. Musculoskeletal hydatid disease: a report of 13 cases. Acta Orthop Scand. 2002;73(2):227–231. doi: 10.1080/000164702753671858. [DOI] [PubMed] [Google Scholar]
- 5.Memis A, Arkun R, Bilgen I, Ustun EE. Primary soft tissue hydatid disease: report of two cases with MRI characteristics. Eur Radiol. 1999;9:1101–1103. doi: 10.1007/s003300050798. [DOI] [PubMed] [Google Scholar]
- 6.Merkle EM, Schulte M, Vogel J, Tomczak R, Rieber A, Kern P, et al. Musculoskeletal involvement in cystic echinococcosis: report of eight cases and review of the literature. AJR Am J Roentgenol. 1997;168:1531–1534. doi: 10.2214/ajr.168.6.9168719. [DOI] [PubMed] [Google Scholar]
- 7.Mueller PR, Dawson SL, Ferrucci JT, Jr, Nardi GL. Hepatic echinococcal cyst: successful percutaneous drainage. Radiology. 1985;155(3):627–628. doi: 10.1148/radiology.155.3.3890001. [DOI] [PubMed] [Google Scholar]
- 8.Nasrieh MA, Abdel-Hafez SK. Echinococcus granulosus in Jordan: assessment of various antigenic preparations for use in the serodiagnosis of surgically confirmed cases using enzyme immuno assays and the indirect haemagglutination test. Diagn Microbiol Infect Dis. 2004;48:117–123. doi: 10.1016/j.diagmicrobio.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 9.Ormeci N, Idilman R, Akyar S, Palabiyikoglu M, Coban S, Erdem H, et al. Hydatid cysts in muscle: a modified percutaneous treatment approach. Int J Infect Dis. 2007;1(3):204–208. doi: 10.1016/j.ijid.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Prousalidis J, Tzardinoglou K, Sgouradis L, Katsohis C, Aletras H. Uncommon sites of hydatid disease. World J Surg. 1998;22(1):17–22. doi: 10.1007/s002689900343. [DOI] [PubMed] [Google Scholar]
- 11.Rodop O, Arpacıoglu MO, Akmaz I, Kiral A. Primary hydatidosis of the peripheral muscles: treatment by surgery and chemoterapy. Eur J Plast Surg. 2001;24:261–263. [Google Scholar]
- 12.Sener RN, Calli C, Kitis O, Yalman O. Multiple, primary spinal-paraspinal hydatid cysts. Eur Radiol. 2001;11(11):2314–2316. doi: 10.1007/s003300000771. [DOI] [PubMed] [Google Scholar]
- 13.Smego RA, Jr, Bhatti S, Khaliq AA, Beg MA. Percutaneous aspiration-injection-reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis 15. 2003;37(8):1073–1083. doi: 10.1086/378275. [DOI] [PubMed] [Google Scholar]
- 14.Tekkok IH, Benli K. Primary spinal extradural hydatid disease: report of a case with magnetic resonance characteristics and pathological correlation. Neurosurgery. 1993;33(2):320–323. [PubMed] [Google Scholar]