Abstract
The general population has a pessimistic view of low back pain (LBP), and evidence-based information has been used to positively influence LBP beliefs in previously reported mass media studies. However, there is a lack of randomized trials investigating whether LBP beliefs can be modified in primary prevention settings. This cluster randomized clinical trial investigated the effect of an evidence-based psychosocial educational program (PSEP) on LBP beliefs for soldiers completing military training. A military setting was selected for this clinical trial, because LBP is a common cause of soldier disability. Companies of soldiers (n = 3,792) were recruited, and cluster randomized to receive a PSEP or no education (control group, CG). The PSEP consisted of an interactive seminar, and soldiers were issued the Back Book for reference material. The primary outcome measure was the back beliefs questionnaire (BBQ), which assesses inevitable consequences of and ability to cope with LBP. The BBQ was administered before randomization and 12 weeks later. A linear mixed model was fitted for the BBQ at the 12-week follow-up, and a generalized linear mixed model was fitted for the dichotomous outcomes on BBQ change of greater than two points. Sensitivity analyses were performed to account for drop out. BBQ scores (potential range: 9–45) improved significantly from baseline of 25.6 ± 5.7 (mean ± SD) to 26.9 ± 6.2 for those receiving the PSEP, while there was a significant decline from 26.1 ± 5.7 to 25.6 ± 6.0 for those in the CG. The adjusted mean BBQ score at follow-up for those receiving the PSEP was 1.49 points higher than those in the CG (P < 0.0001). The adjusted odds ratio of BBQ improvement of greater than two points for those receiving the PSEP was 1.51 (95% CI = 1.22–1.86) times that of those in the CG. BBQ improvement was also mildly associated with race and college education. Sensitivity analyses suggested minimal influence of drop out. In conclusion, soldiers that received the PSEP had an improvement in their beliefs related to the inevitable consequences of and ability to cope with LBP. This is the first randomized trial to show positive influence on LBP beliefs in a primary prevention setting, and these findings have potentially important public health implications for prevention of LBP.
Keywords: Primary prevention, Patient education, Biopsychosocial, Public health
Introduction
Low back pain (LBP) is a common chronic musculoskeletal disorder [19, 32] that causes significant disability [2, 31, 33, 40]. Specifically, LBP has been associated with the inability to obtain or maintain employment [31] and lost productivity while still employed [33]. Cost-effective interventions for LBP are a research priority given its adverse impact on society [10]. Providing evidence-based education is one example of a cost-effective intervention for LBP.
Educational approaches based solely on anatomical explanations of LBP are known to be inadequate given the contemporary understanding of a biopsychosocial conceptualization of LBP [17, 26, 37]. Currently, it is recommended that patient education for LBP de-emphasizes the anatomical cause of the pain, encourages the patient to focus on resuming activity, teaches the patient to view LBP as a common condition, and reinforces the importance of maintaining positive attitude and coping styles [36, 38].
This change in education approach has had a positive influence on management of existing LBP. For example, advice to stay active and resume normal activities was more effective than usual medical care for LBP in separate randomized trials [14, 15, 18]. Psychosocial education that encourages positive coping was associated with decreased work absence in a quasi-experimental study [34]. The Back Book [27] is a pamphlet that delivers standard, evidenced-based information consistent with a biopsychosocial model, and has been used in randomized clinical trials demonstrating reduced disability and fear-avoidance beliefs in general practice [8] and physical therapy settings [12]. A quasi-experimental study also indicated that general practice patients given the Back Book reported higher patient satisfaction ratings and lower rates of persistent LBP [10].
Although these secondary prevention findings are important, less evidence is available to inform decision-making regarding whether psychosocial education can be effective in primary prevention of LBP. In an effective primary prevention model, evidence-based information would alter unwarranted beliefs about the consequences and management of LBP, as well as reduce the fear and threat of experiencing LBP. Understanding whether favorably altering beliefs about LBP before LBP develops has become a critical research priority given the huge cost burden of LBP on society [3, 20] and the pessimistic views held by the general population about the consequences of LBP [13].
Several population-based studies have investigated the primary prevention effects of psychosocial information on LBP delivered by media campaigns [6, 7, 39, 43]. Collectively these studies demonstrated a positive shift in LBP beliefs [6, 7, 39, 43], with persistent effects noted 3 years later by Buchbinder et al. [5]. Although these results are encouraging, these population-based studies utilized quasi experimental [7, 43] and “pragmatic observational” [39] methodologies; no randomized trials have been reported to date. Therefore, the purpose of this paper is to report the effect of an evidence-based PSEP on LBP beliefs for soldiers completing military training and participating in an ongoing cluster randomized clinical trial. This particular setting was selected for this study, because disability from LBP is commonly experienced in the military [16, 29] and favorable shifts in LBP beliefs before LBP is experienced could potentially alter this trend.
Materials and methods
Overview
The institutional review boards at the Brooke Army Medical Center (Fort Sam Houston, TX, USA) and the University of Florida (Gainesville, FL, USA) granted approval for this project. Consecutive soldiers entering the combat medic advanced individual training (AIT) at Fort Sam Houston, TX were considered for participation in this study. This study reported a planned analysis of a proximal outcome of the prevention of low back pain in the military (POLM) clinical trial (NCT00373009) [11] which has been registered at http://clinicaltrials.gov.
The goals of this study were to twofold. First, we wanted to determine the efficacy of an implemented PSEP for improving LBP beliefs. Second, we wanted to investigate the potential of responder subgroups to the PSEP. Our a priori hypothesis was that soldiers receiving the education program would have an improvement in LBP beliefs, in comparison to those that not receiving the education program. We also investigated whether demographic or psychological factors were predictive of improvement in LBP beliefs to identify responder subgroups.
Subjects
Research staff at Fort Sam Houston, Texas introduced the study to individual companies of soldiers. Soldiers were screened for eligibility, and informed consent was obtained, as appropriate. For 12 consecutive months soldiers were screened for eligibility according to the following inclusion/exclusion criteria.
Inclusion criteria
age 18 (or emancipated minor that is 17-year-old) to 35-year-old,
participating in combat medic military occupational specialty (MOS) training,
English speaking and reading.
Exclusion criteria
prior history of LBP (operationally defined as LBP that limited work or physical activity, lasted longer than 48 h, and caused the subject to seek healthcare) or previous medical history for any surgery for LBP,
currently seeking medical care for LBP,
history of degenerative joint disease, arthritis, spine trauma or vertebral fractures, and/or spondylolisthesis,
currently unable to participate in physical fitness training due to injury in foot, ankle, knee, hip, neck, shoulder, elbow, wrist, or hand injury,
history of fracture (stress or traumatic) in proximal femur and/or pelvis,
currently pregnant,
previous failure of AIT.
Randomization
Military training environments requires living in close quarters with other members of the unit making individual randomization an unfeasible option for this trial due to concerns related to disruption of normal training schedule and treatment contamination. Therefore, a cluster randomization strategy was utilized for assigning companies to receive or not receive the PSEP. This meant that for a given company, every soldier who consented to the study received the same study condition. Cluster randomization is viable methodological choice that has been effectively used in other large samples of primary prevention [23, 24, 42]. The randomization schedule was prepared by computer and was determined before recruitment began. The randomization schedule was balanced to ensure equal allocation to each condition after 18 companies were recruited.
Intervention
Companies of soldiers were randomized to receive or not receive the PSEP. It was not possible to mask soldiers in this study, because of the nature of the educational program. The interventions are described below.
Psychosocial educational program (PSEP)
The PSEP involved an educational session within the first 14 days of entering AIT. The session consisted of an interactive seminar designed by the POLM investigative team and was implemented by study personnel. The overall goal of the 45-min session was to emphasize current scientific evidence on LBP. The seminar covered topics related to the favorable natural history of LBP, lack of definitive anatomical causes of LBP, the importance of returning to normal activity, and decreasing fear-avoidance beliefs and pain catastrophizing when experiencing LBP. After the seminar, soldiers were involved in a question and answer session and issued The Back Book [27]. The Back Book was used as the educational supplement, because of our prior experience with it in a physical therapy clinical trial [12] and its prior association with positive shifts in patient LBP beliefs [8, 10].
Control group (CG)
The CG received no formal instruction on LBP. An anatomy-based education program was not appropriate for a comparison, because prior studies have demonstrated no favorable change in LBP beliefs [8, 12, 34]. Furthermore, use of a CG (as opposed to an alternate form of education) is consistent with the methodology from the previously reported population-based studies [6, 7, 39, 43].
Measurement
Study-related measures were collected by research personnel unaware of randomization assignment before AIT and 12 weeks later, when AIT was completed. All measures were scored in a masked manner by computer algorithm.
Primary outcome measure
The back beliefs questionnaire (BBQ) was the primary outcome variable for this study. The BBQ is a previously validated self-report questionnaire used to quantify beliefs about the likely consequences of having LBP [35]. The BBQ has 14 items with response options ranging from 1 (agree) to 5 (disagree), and only the nine inevitability items are included for scoring (potential range: 9–45). Higher BBQ scores are indicative of better LBP beliefs and indicate the potential of a better ability to cope with LBP [6, 7]. In addition to having sound psychometric properties, the BBQ has been used as an outcome measure in other studies investigating educational and mass media interventions [5–7, 34]. Use in this trial is appropriate for our hypotheses and will also allow for cross-study comparisons.
Other measures
Commonly implemented and previously validated self-report questionnaires were used to compare baseline attributes for the intervention groups and to determine baseline influence on LBP belief outcomes. The medical outcomes survey 12-item short-form health survey (SF-12) was used as a self-report of health status for physical and mental function. The physical and mental component summary scales (PCS and MCS) were reported individually in this study because they are valid estimates of physical and mental health [41]. The state-trait anxiety questionnaire (STAI) [30] and Beck depression inventory (BDI) [9, 28, 44] were used to measure negative affect from generalized anxiety and generalized depression, respectively. Nine items from the fear of pain questionnaire (FPQ-III) were used to measure fear about specific situations that normally produce pain [1, 21, 25].
Sample size estimation
In a previous study from Buchbinder et al. [5.], it was estimated that a sample size of 550 provided 80% power to detect a shift in BBQ of 0.5 (at 0.05 significance). Our primary sample size estimation was based on determining the effect of education and exercise programs on the occurrence and severity of LBP episodes [11]. Such a sample size (16 companies, approximately 3,200 soldiers) provided adequate statistical power for the planned proximal outcome analysis of LBP beliefs, as well as the consideration of responder subgroups from various demographic and psychological factors.
Data analysis
Demographic and baseline levels of variables were compared between the two randomly assigned groups using t test for comparison of means and chi-square tests for comparison of proportions. It was determined a priori that variables significantly different between the two groups would be considered in the final analyses, in addition to previously specified covariates of sex, age, and race.
First, we analyzed the 12-week follow-up completers only, as a liberal estimate of treatment effect. A linear mixed model was fitted for the BBQ at the 12-week follow-up in continuous scale, and a generalized linear mixed model was fitted for the dichotomous outcomes on BBQ change of more than two points. Two points was selected as a criterion of meaningful change in the BBQ, because it corresponded with previously reported thresholds in the literature such as 2-year population changes in BBQ scores that were associated with improvements in worker’s compensation claims [7]. There was no sample-specific cut-off scores available for this part of the analysis, as the BBQ has not been previously studied in military samples.
A sensitivity analysis regarding missing data was conducted with the following 3-step process: (1) the dropout rates were compared across the education programs to assess systematic differences; (2) demographic and baseline levels of variables were examined for their relationship to dropout. Those variables related to dropout status were used to impute missing values for use in the intention to treat analysis of all soldiers; (3) comparison of the completers versus imputation analyses would provide an additional estimate of the effect of dropouts on hypothesis tests. All statistical analyses were performed using the SAS software, version 9 (SAS Institute Inc, 1996).
Results
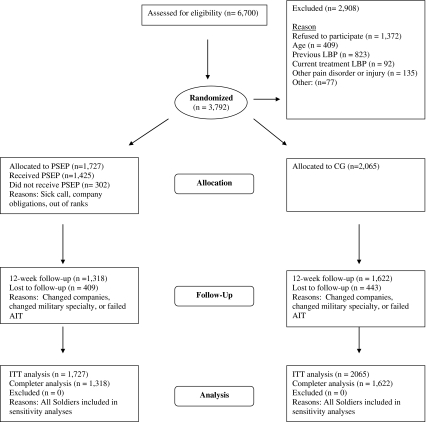
Refer to Fig. 1 for a flow chart describing the number of patients considered for this trial, eventually enrolled into the trial, and completed follow-up assessment, as per CONSORT guidelines [22]. Descriptive statistics for the sample (n = 3,792) are summarized in Table 1. There were small post randomization differences noted for the PSEP and CG, such that soldiers assigned to PSEP had worse BBQ scores, were older, more likely to have college level or more education, and more likely to have enlisted in the army for 1–3 years (P < 0.01). These variables were included as covariates in the subsequent analyses.
Fig. 1.
Summary of recruitment, enrollment, follow-up, and analysis for psychosocial education trial. LBP low back pain, PSEP psychosocial education program, CG control group, AIT advanced individual training, ITT intention to treat analysis
Table 1.
Sociodemographic and psychological characteristics of the military sample
| Factors | Intake (n = 3,792) | Missed 12-week follow-up (n = 852) | ||||
|---|---|---|---|---|---|---|
| Total | CG (n = 2,065) | PSEP (n = 1,727) | Total | CG (n = 443) | PSEP (n = 409) | |
| BBQ total [mean (SD)] | 25.9 (5.7) | 26.1 (5.7) | 25.6 (5.7)* | 25.4 (5.6) | 25.7 (5.5) | 25.2 (5.7) |
| PCS total [mean (SD)] | 53.5 (5.1) | 53.5 (5.2) | 53.4 (5.1) | 52.8 (5.6) | 52.9 (5.4) | 52.6 (5.8) |
| MCS total [mean (SD)] | 49.1 (8.6) | 49.2 (8.6) | 49.0 (8.7) | 47.7 (9.8) | 48.3 (9.5) | 47.0 (10.1) |
| FPQ total [mean (SD)] | 18.1 (5.8) | 17.9 (5.9) | 18.3 (5.7) | 18.1 (6.1) | 17.7 (6.3) | 18.5 (5.9) |
| BDI total [mean (SD)] | 6.4 (6.6) | 6.4 (6.7) | 6.3 (6.5) | 7.9 (8.0) | 7.8 (8.0) | 7.9 (8.0) |
| STAI total [mean (SD)] | 36.0 (9.2) | 35.9 (9.3) | 36.0 (9.0) | 37.7 (9.8) | 37.6 (10.0) | 37.8 (9.7) |
| Age [mean (SD)] | 22.0 (4.4) | 21.6 (4.2) | 22.4 (4.6)* | 21.9 (4.4) | 21.6 (4.1) | 22.2 (4.7) |
| Race [n (%)] | ||||||
| Other | 1,049 (27.7) | 581 (28.1) | 468 (27.1) | 288 (33.8) | 173 (39.1) | 115 (28.1)* |
| White or Caucasian | 2,743 (72.3) | 1,484 (71.9) | 1,259 (72.9) | 564 (66.2) | 270 (61.0) | 294 (71.9) |
| Gender [n (%)] | ||||||
| Female | 1,103 (29.1) | 625 (30.3) | 478 (27.7) | 252 (29.6) | 144 (32.5) | 108 (26.4) |
| Male | 2,689 (70.9) | 1,440 (69.7) | 1,249 (72.3) | 600 (70.4) | 299 (67.5) | 301 (73.6) |
| Education [n (%)] | ||||||
| College or more | 2,028 (53.5) | 1,073 (52.0) | 955 (55.3) | 391 (45.9) | 195 (44.0) | 196 (47.9) |
| High school or less | 1,764 (46.5) | 992 (48.0) | 772 (44.7) | 461 (54.1) | 248(56.0) | 213 (52.1) |
| Income [n (%)] | ||||||
| $35,000 or more | 665 (17.6) | 322 (15.6) | 343 (19.9)* | 143 (16.8) | 63 (14.3) | 80 (19.7) |
| Less than $35,000 | 3,118 (82.4) | 1,738 (84.4) | 1,380 (80.1) | 706 (83.2) | 379 (85.8) | 327 (80.3) |
| Time in army [n (%)] | ||||||
| 1–3 years | 322 (8.5) | 153 (7.4) | 169 (9.8)* | 54 (6.3) | 25 (5.6) | 29 (7.1) |
| <1 year | 3,199 (84.4) | 1,794 (87.0) | 1,405 (81.4) | 733 (86.0) | 386 (87.1) | 347 (84.8) |
| >3 years | 269 (7.1) | 116 (5.6) | 153 (8.9) | 65 (7.6) | 32 (7.2) | 33 (8.1) |
BBQ back beliefs questionnaire, PSEP psychosocial education program, FPQ-III fear of pain questionnaire, BDI Beck depression inventory, STAI state trait anxiety index, PCS physical component summary, MCS mental component summary
* P < 0.01 in t tests for comparison of means and chi-square tests for comparison of proportions between the two randomly assigned groups
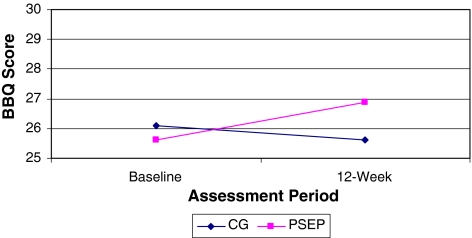
The BBQ score improved significantly (P < 0.0001) from baseline of 25.6 ± 5.7 (mean ± SD) to 26.9 ± 6.2 at the 12-week follow-up for those receiving the PSEP, while there was a significant decline (P < 0.0001) from 26.1 ± 5.7 to 25.6 ± 6.0 for those in the CG (Fig. 2). The effect sizes of BBQ change were 0.18 and −0.10, for the PSEP and CG groups, respectively. These differences favoring the PSEP for BBQ scores were statistically significant at the 12-week follow-up (P < 0.0001). Table 2 presents the results of linear mixed modeling of the BBQ at the 12-week follow-up and the results of generalized linear mixed models for the dichotomous outcomes of BBQ improvement (greater than two points). The adjusted mean improvement for those receiving the PSEP was 1.49 points higher than those in the 4CG (P < 0.0001). The adjusted odds ratio of BBQ improvement for those receiving the PSEP was 1.51 (95% CI = 1.22–1.86) compared to those in the CG.
Fig. 2.
Psychosocial education results in improvement in low back pain beliefs. BBQ back beliefs questionnaire, CG control group, PSEP psychosocial education program. Statistically significant differences were present at the 12-week assessment (P < 0.0001)
Table 2.
Summary of analyses results for low back pain beliefs
| Effects | BBQ total at follow-up (continuous) | BBQ improvement (categorical) | |||||
|---|---|---|---|---|---|---|---|
| Estimate | SE | P value | Odds ratios | 95% CI | P value | ||
| Intercept | 15.66 | 2.35 | <0.0001 | ||||
| BBQ total at intake | 0.41 | 0.02 | <0.0001 | ||||
| PSEP | 1.49 | 0.22 | <0.0001 | 1.51 | 1.22 | 1.86 | 0.0001 |
| Age | 0.06 | 0.02 | 0.0090 | 1.01 | 0.99 | 1.03 | 0.1939 |
| Gender: female | 0.84 | 0.24 | 0.0004 | 0.90 | 0.76 | 1.07 | 0.2217 |
| Race: others | −0.23 | 0.24 | 0.3271 | 0.82 | 0.68 | 0.96 | 0.0128 |
| Education: college or more | 0.45 | 0.22 | 0.0401 | 1.23 | 1.05 | 1.44 | 0.0106 |
| Income: $35,000 or more | −0.13 | 0.28 | 0.6374 | 1.00 | 0.82 | 1.22 | 0.9722 |
| Time in army: 1–3 years | 0.51 | 0.54 | 0.3432 | 1.11 | 0.76 | 1.62 | 0.5814 |
| Time in army: <1 year | −0.03 | 0.42 | 0.9516 | 0.95 | 0.71 | 1.27 | 0.7344 |
| FPQ-III total at intake | −0.04 | 0.02 | 0.0205 | 1.00 | 0.99 | 1.02 | 0.5859 |
| BDI total at intake | −0.10 | 0.02 | <0.0001 | 0.99 | 0.97 | 1.01 | 0.1905 |
| STAI total at intake | −0.01 | 0.02 | 0.7679 | 1.01 | 0.99 | 1.02 | 0.3146 |
| PCS total at intake | 0.00 | 0.02 | 0.8621 | 1.00 | 0.98 | 1.02 | 0.9922 |
| MCS total at intake | −0.02 | 0.02 | 0.1889 | 1.00 | 0.99 | 1.01 | 0.9270 |
Continuous outcome was calculated by raw change score and categorical outcome was defined as yes/no depending whether BBQ score increased more than two points from time of intake to follow-up. Statistically significant predictors are indicated in bold font (P < 0.05)
BBQ back beliefs questionnaire, PSEP psychosocial education program, FPQ-III fear of pain questionnaire, BDI Beck depression inventory, STAI state trait anxiety index, PCS physical component summary, MCS mental component summary
BBQ score at intake, older age, female, race other than white, college education or higher are significantly associated with higher BBQ score at the follow-up. When psychological factors were investigated, only fear of pain and depression were statistically associated with BBQ follow-up score. These psychological associations were small in magnitude, as every unit increase in FPQ and BDI was associated with a 0.04 and 0.10 point lower follow-up BBQ score, respectively. The analyses investigating subgroup responder characteristics indicated potential demographic influences on BBQ scores (Table 2). BBQ improvement for soldiers of race other than white had an odds ratio of 0.82 (95% CI: 0.69–0.98). College education or higher was also related to BBQ improvement, with an odds ratio of 1.23 (95% CI: 1.05–1.44). In contrast, none of the psychological variables were associated with BBQ improvement of greater than two.
There were no major changes in results when the sensitivity analyses were performed, suggesting minimal influence of study drop out. The CG had a higher drop out rate than the PSEP group (25.7 vs. 19.8%). The drop outs from the two groups had the same intake characteristics, except that proportion of soldiers of race other than white in the CG was higher than that of the PSEP group. There were significant differences (P < 0.05) from the soldiers, who completed the follow-up (n = 2,940) at 12 weeks compared to those soldiers that dropped out (n = 852) in baseline BBQ, PCS, MCS, BDI, STAI, race, education level, and time enlisted in army. These variables were used to predict the BBQ at follow-up for those dropped out using a linear mixed model fitted based on complete data. Sensitivity analyses were then performed by running two separate models. The first model was an intention to treat analysis with all soldiers (n = 3,792) using the imputed outcome for those not completing follow-up. The second model was an analysis of the imputed outcome for only those soldiers (n = 852) not completing follow-up. In the intention to treat analysis, the adjusted mean BBQ scores at follow-up for those receiving the PSEP was 1.44 points higher than those in the CG (P < 0.0001), with an odds ratio for BBQ improvement of 1.75 (95% CI: 1.44–2.13). In the imputation outcome analysis the adjusted mean BBQ scores for those receiving the PSEP was 1.31 points higher than those in the CG (P < 0.0001), with an odds ratio for BBQ improvement of 2.10 (95% CI: 1.52–2.92).
Discussion
The general population has a pessimistic view on the consequences of LBP, and it has been hypothesized that such beliefs contribute to the development of disability from LBP [13]. Information that positively alters beliefs about LBP to better reflect current evidence has potential treatment implications in a variety of settings [7, 8, 10, 12, 39, 43]. Consecutive companies of soldiers were recruited for the current study, excluding those with a previous history of LBP or with a current musculoskeletal pain condition. Our findings suggested that for this cohort, the PSEP resulted in a small improvement in LBP beliefs and potential ability to cope with LBP. Our study included a CG that suggests the natural history of LBP beliefs is to slightly worsen in this particular environment. Although only a small effect size was associated with BBQ improvement, the current study adds to the existing literature as it is the first randomized trial to demonstrate positive influence on LBP beliefs in a primary prevention setting.
These results are consistent with earlier findings on improving LBP beliefs from population-based studies that used quasi-experimental or observational designs in Australia [5–7], Scotland [39], and Norway [43]. Although the evidence-based educational messages regarding LBP were likely similar across all studies, the current study incorporated one time, group instruction as compared to information delivered by radio, television, or print advertisements. The current study had the shortest follow-up time (12 weeks), while previously reported studies had follow-up times up to 3 years. Despite these methodological differences, there appears to be converging evidence that LBP beliefs can be effectively altered with evidence-based information delivered by a variety of mediums.
The relevance of the observed improvement in LBP beliefs is an important consideration when interpreting the results of this trial; yet definitive clinically important thresholds for BBQ change have not been reported. We utilized a BBQ change criterion based on the initial Buchbinder et al. [6, 7] studies that reported that a 2-year mean BBQ change of 1.9 was associated with decreased rates of compensation claims [7]. In contrast, we reported a smaller mean improvement of 1.5 in BBQ scores at 12 weeks. This smaller magnitude of change and earlier outcome assessment indicate a smaller potential for affecting future reports of disability and pain [7]. One reason for a smaller effect size in the current trial could be that the previously reported study [7] utilized quasi-experimental methodology, which has the potential to overestimate treatment effects [4]. Other equally plausible reasons for the smaller effect size observed in our study include the previously mentioned differences in study populations, and the mass media campaign by Buchbinder et al. [7] was more effective than a single session PSEP.
Another part of our analysis was to determine if demographic predictors of success existed, suggesting the potential for responder subgroups to exist. These analyses indicated that soldiers of race other than white were less likely to report a BBQ improvement (OR = 0.82), while those with college education or higher were more likely to report a BBQ improvement (OR = 1.23). These results suggest the potential of cultural or socioeconomic influences on the alteration of LBP beliefs. We are hesitant to speculate further on these influences, because these findings are preliminary and their theoretical implications are beyond the scope of the current manuscript. The only other available report is from Buchbinder et al. [5], who have reported similar levels of BBQ improvement across most demographic factors, with only upper white-collar workers having larger BBQ changes. Additional research is necessary to replicate these findings and determine if race or education status can be used to identify LBP belief responder subgroups.
Previous studies have not considered psychological factors, and our study suggests that fear of pain and depression was predictive of BBQ follow-up scores. However, these associations were quite small, suggesting these baseline psychological factors have only a minimal influence on BBQ outcome. Contrary to our expectations, baseline psychological factors were not associated with BBQ change greater than two. Psychological distress has been consistently associated with the development of chronic LBP [17, 26], and we expected those with higher pre-morbid levels of anxiety, depression, and fear of pain to have a stronger association with BBQ improvement. However, this was not the case in the current trial, as only weak statistical associations with follow up scores existed. A possible explanation for these unexpected findings could be that psychological distress levels were very low in this particular setting (Table 1), and these low levels had minimal potential to influence LBP beliefs. Another explanation is that the psychological factors of interest have a strong influence on LBP beliefs but only when individuals are actively experiencing LBP. Overall the responder analyses suggest that for this setting the PSEP intervention should not be considered for targeted application to psychological subgroups. However, future studies in different primary prevention cohorts with wider ranges of psychological distress are necessary to further investigate this issue.
The primary limitation of this study is that we did not investigate the LBP beliefs after 12 weeks or the effect of the PSEP on subsequent reports of pain, disability, and health care utilization. Pain, disability, and health care utilization are important outcomes to consider and these will be considered as 2-year endpoints in the ongoing POLM trial [11]. PSEP effect on LBP beliefs was an important factor to establish before determining pain, disability, and health care utilization as distal outcomes, because previous studies on the topic had not used randomized trial methodology. Another limitation is that this study was performed in a military setting, while the other studies in this area were performed with general populations. Although disability from LBP is a major problem across both of these settings, caution should be used when attempting to generalize our results to the general population. The use of a CG allowed us to determine the 12-week natural history of LBP beliefs, but it is also another limitation of this study. The effects of this particular PSEP are in reference to the CG, not a comparison education session.
Conclusion
This is the first randomized trial to show positive influence on LBP beliefs following a PSEP implemented in a primary prevention setting. In contrast, LBP beliefs slightly deteriorated for those in the CG. Though only small effect sizes were observed, these findings have potentially important public health implications for prevention of LBP. Future study will involve continuing the POLM trial to collect reports of LBP occurrence, severity, and health care utilization over the next 2 years [11]. These endpoints will allow us to make broader conclusions about the effectiveness of the PSEP for clinical presentation of LBP. Future study will also involve providing the same PSEP to health care providers and determine whether it positively influences professional advice given for treatment of LBP. Last, the same PSEP could be investigated to determine if it has public health implications for environments outside of the military, for example its effects on LBP beliefs in schools, universities, occupational, or clinical settings.
Acknowledgments
SZG, JDC, DST, SSW, ACW, JLD, and MER were supported by the peer-review medical research program of the Department of Defense (PR054098). Christopher Barnes, Erik Henrikson, and Yang Li were responsible for the creation and management of the database. Donna Cunningham provided administrative assistance during this phase of the study. The institutional review boards at the Brooke Army Medical Center (Fort Sam Houston, Texas) and the University of Florida (Gainesville, FL) granted approval for this project.
References
- 1.Albaret MC, Munoz Sastre MT, Cottencin A, Mullet E. The Fear of Pain questionnaire: factor structure in samples of young, middle-aged and elderly European people. Eur J Pain. 2004;8(3):273–281. doi: 10.1016/j.ejpain.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993;9(3):174–182. doi: 10.1097/00002508-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Asche CV, Kirkness CS, dam-Marx C, Fritz JM. The societal costs of low back pain: data published between 2001 and 2007. J Pain Palliat Care Pharmacother. 2007;21(4):25–33. doi: 10.1300/J354v21n04_06. [DOI] [PubMed] [Google Scholar]
- 4.Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342(25):1878–1886. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- 5.Buchbinder R, Jolley D. Effects of a media campaign on back beliefs is sustained 3 years after its cessation. Spine. 2005;30(11):1323–1330. doi: 10.1097/01.brs.0000164121.77862.4b. [DOI] [PubMed] [Google Scholar]
- 6.Buchbinder R, Jolley D, Wyatt M. 2001 Volvo award winner in clinical studies: effects of a media campaign on back pain beliefs and its potential influence on management of low back pain in general practice. Spine. 2001;26(23):2535–2542. doi: 10.1097/00007632-200112010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Buchbinder R, Jolley D, Wyatt M. Population based intervention to change back pain beliefs and disability: three part evaluation. BMJ. 2001;322(7301):1516–1520. doi: 10.1136/bmj.322.7301.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine. 1999;24(23):2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 9.Chibnall JT, Tait RC. The short form of the Beck Depression Inventory: validity issues with chronic pain patients. Clin J Pain. 1994;10(4):261–266. doi: 10.1097/00002508-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Coudeyre E, Tubach F, Rannou F, Baron G, Coriat F, Brin S, Revel M, Poiraudeau S. Effect of a simple information booklet on pain persistence after an acute episode of low back pain: a non-randomized trial in a primary care setting. PLoS ONE. 2007;2(1):e706. doi: 10.1371/journal.pone.0000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.George SZ, Childs JD, Teyhen DS, Wu SS, Wright AC, Dugan JL, Robinson ME. Rationale, design, and protocol for the prevention of low back pain in the military (POLM) trial ( NCT00373009) BMC Musculoskelet Disord. 2007;8:92. doi: 10.1186/1471-2474-8-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28(23):2551–2560. doi: 10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 13.Gross DP, Ferrari R, Russell AS, Battie MC, Schopflocher D, Hu RW, Waddell G, Buchbinder R. A population-based survey of back pain beliefs in Canada. Spine. 2006;31(18):2142–2145. doi: 10.1097/01.brs.0000231771.14965.e4. [DOI] [PubMed] [Google Scholar]
- 14.Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine. 1998;23(23):2625–2630. doi: 10.1097/00007632-199812010-00018. [DOI] [PubMed] [Google Scholar]
- 15.Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine. 1995;20(4):473–477. doi: 10.1097/00007632-199512150-00006. [DOI] [PubMed] [Google Scholar]
- 16.Lincoln AE, Smith GS, Amoroso PJ, Bell NS. The natural history and risk factors of musculoskeletal conditions resulting in disability among US Army personnel. Work. 2002;18(2):99–113. [PMC free article] [PubMed] [Google Scholar]
- 17.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25(9):1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 18.Malmivaara A, Hakkinen U, Aro T, Heinrichs ML, Koskenniemi L, Kuosma E, Lappi S, Paloheimo R, Servo C, Vaaranen V. The treatment of acute low back pain—bed rest, exercises, or ordinary activity? N Engl J Med. 1995;332(6):351–355. doi: 10.1056/NEJM199502093320602. [DOI] [PubMed] [Google Scholar]
- 19.Mantyselka P, Kumpusalo E, Ahonen R, Kumpusalo A, Kauhanen J, Viinamaki H, Halonen P, Takala J. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain. 2001;89(2–3):175–180. doi: 10.1016/S0304-3959(00)00361-4. [DOI] [PubMed] [Google Scholar]
- 20.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, Sullivan SD. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656–664. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 21.McNeil DW, Rainwater AJ. Development of the Fear of Pain Questionnaire–III. J Behav Med. 1998;21(4):389–410. doi: 10.1023/A:1018782831217. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. J Am Podiatr Med Assoc. 2001;91(8):437–442. doi: 10.7547/87507315-91-8-437. [DOI] [PubMed] [Google Scholar]
- 23.Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ornstein S, Jenkins RG, Nietert PJ, Feifer C, Roylance LF, Nemeth L, Corley S, Dickerson L, Bradford WD, Litvin C. A multimethod quality improvement intervention to improve preventive cardiovascular care: a cluster randomized trial. Ann Intern Med. 2004;141(7):523–532. doi: 10.7326/0003-4819-141-7-200410050-00008. [DOI] [PubMed] [Google Scholar]
- 25.Osman A, Breitenstein JL, Barrios FX, Gutierrez PM, Kopper BA. The Fear of Pain Questionnaire-III: further reliability and validity with nonclinical samples. J Behav Med. 2002;25(2):155–173. doi: 10.1023/A:1014884704974. [DOI] [PubMed] [Google Scholar]
- 26.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002;27(5):E109–E120. doi: 10.1097/00007632-200203010-00017. [DOI] [PubMed] [Google Scholar]
- 27.Roland M, Waddell G, Klaber-Moffett J. The Back Book, 1996. Norwich, United Kingdom: The Stationery Office; 1996. [Google Scholar]
- 28.Schotte CK, Maes M, Cluydts R, Doncker D, Cosyns P. Construct validity of the Beck Depression Inventory in a depressive population. J Affect Disord. 1997;46(2):115–125. doi: 10.1016/S0165-0327(97)00094-3. [DOI] [PubMed] [Google Scholar]
- 29.Songer TJ, LaPorte RE (2000) Disabilities due to injury in the military. Am J Prev Med 18(3)(Suppl):33–40. doi:10.1016/S0749-3797(00)00107-0 [DOI] [PubMed]
- 30.Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the state and trait anxiety inventory (form Y) Palo Alto, CA: Consulting Psychologists Press; 1993. [Google Scholar]
- 31.Stang P, Korff M, Galer BS. Reduced labor force participation among primary care patients with headache. J Gen Intern Med. 1998;13(5):296–302. doi: 10.1046/j.1525-1497.1998.00094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sternbach RA. Pain and ‘hassles’ in the United States: findings of the Nuprin pain report. Pain. 1986;27(1):69–80. doi: 10.1016/0304-3959(86)90224-1. [DOI] [PubMed] [Google Scholar]
- 33.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 34.Symonds TL, Burton AK, Tillotson KM, Main CJ. Absence resulting from low back trouble can be reduced by psychosocial intervention at the work place. Spine. 1995;20(24):2738–2745. doi: 10.1097/00007632-199512150-00016. [DOI] [PubMed] [Google Scholar]
- 35.Symonds TL, Burton AK, Tillotson KM, Main CJ. Do attitudes and beliefs influence work loss due to low back trouble? Occup Med (Lond) 1995;46(1):25–32. doi: 10.1093/occmed/46.1.25. [DOI] [PubMed] [Google Scholar]
- 36.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 37.Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine. 1987;12(7):632–644. doi: 10.1097/00007632-198709000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Waddell G. Low back pain: a twentieth century health care enigma. Spine. 1996;21(24):2820–2825. doi: 10.1097/00007632-199612150-00002. [DOI] [PubMed] [Google Scholar]
- 39.Waddell G, O’Connor M, Boorman S, Torsney B. Working Backs Scotland: a public and professional health education campaign for back pain. Spine. 2007;32(19):2139–2143. doi: 10.1097/BRS.0b013e31814541bc. [DOI] [PubMed] [Google Scholar]
- 40.Walker BF, Muller R, Grant WD. Low back pain in Australian adults: prevalence and associated disability. J Manipulative Physiol Ther. 2004;27(4):238–244. doi: 10.1016/j.jmpt.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 41.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Watson L, Small R, Brown S, Dawson W, Lumley J. Mounting a community-randomized trial: sample size, matching, selection, and randomization issues in PRISM. Control Clin Trials. 2004;25(3):235–250. doi: 10.1016/j.cct.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 43.Werner EL, Ihlebaek C, Laerum E, Wormgoor ME, Indahl A. Low back pain media campaign: no effect on sickness behaviour. Patient Educ Couns. 2008;71(2):198–203. doi: 10.1016/j.pec.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 44.Whisman MA, Perez JE, Ramel W. Factor structure of the Beck Depression Inventory-Second Edition (BDI-II) in a student sample. J Clin Psychol. 2000;56(4):545–551. doi: 10.1002/(SICI)1097-4679(200004)56:4<545::AID-JCLP7>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]