Abstract
To achieve stable fixation of the upper cervical spine in posterior fusions, the occiput is often included. With the newer techniques, excluding fixation to the occiput will retain the occiput–cervical motion, while still allowing a stable fixation. Harms’s technique has been adapted at our institution and its effectiveness for indications such as C2 complex fractures and tumors using C1 or C2 as endpoints of a posterior fixation are reviewed. Fourteen cases were identified, consisting of one os odontoideum; four acute fractures and four non-unions of the odontoid; three tumors and two complex fractures of C2 vertebral body, and one C2–C3 post-traumatic instability. One misplaced screw without clinical consequences was the only complication recorded. Screw loosening or migration was not observed at follow-up, showing a stable fixation.
Keywords: Cervical spine, Posterior fusion, Pedicle
Introduction
Posterior fusion of the first and second cervical vertebrae (C1–C2) is a well-known technique for the treatment of traumatic, post-traumatic and congenital instability of C1–C2 junction. From an historical perspective, many sublaminar wiring techniques have been developed and are still in use [1–3]. Unfortunately, primary stability following sublaminar wiring and bone grafting is often poor, requiring postoperative immobilization for long periods, and it is also burdened with a considerable rate of non-union. Posterior C1–C2 fusion using either Harms’s or Magerl’s technique represent the most important advancement in upper cervical posterior fusion surgery. Both techniques are quite complex and require an in-depth knowledge of the surgical anatomy to ensure a good technical outcome. Apart from this, both the techniques have shown to result in fusion rates nearing 100%, even without postoperative immobilization [4–6]. Magerl’s technique consists of an “in situ” C1–C2 transarticular screw fixation with posterior wiring to hold the bone graft. In Harms’s technique, polyaxial screws are independently inserted in C1 articular masses and in C2 pedicles and connected by a small diameter rod. Unlike others, Harms’s method allows a direct intraoperative reduction of C1–C2 malalignment and does not require a posterior wiring. Furthermore, the use of polyaxial screws in C1 and C2 allows these two vertebrae to be used as reliable endpoints of a posterior fusion in different diseases, sparing the occiput.
Surgical technique
Patient is put in the prone position and the Mayfield head-holder is used, and any misalignment is corrected. Head is placed in slight flexion to facilitate the surgical approach. After a midline incision, the spine is exposed from the skull to C5. Direction of C2 screws is more parallel to the vertebral endplates in Harms’s than in Magerl’s technique, so avoiding an extension to the cervico-thoracic junction. This technique is also easier to apply in cases of severe thoracic kyphosis.
The inferior surface of the posterior arch of C1 is exposed towards the lateral edges. C1 articular mass screw insertion requires the direct posterior visualization of C1–C2 articular joint. This can be exposed subperiostally using a smooth dissecting probe such as a Freer’s dissector, in order to minimize bleeding from the venous plexus. Fibrin glue on small pieces of hemostatic sponge can be delicately introduced beside the articular joint for a better bleeding control. Once the C1–C2 joint margins are defined by two Freers or Penfields placed on either side, a unicortical starting hole is created on the inferior border of C1 posterior arch using a high speed burr (Fig. 1a). With the aid of the two dissectors as a guide, drill is then directed anteriorly within the C1 lateral mass. Bicortical screw placement can be performed under fluoroscopic guidance with caution, although overall this is reasonably safe as there is some safety margin anteriorly prior to important structures. The screw preferred is partially threaded, to avoid irritation of the C2 root. Careful exposure of the postero-medial border of the C2 pedicle facilitates the drilling and screw placement by the direct visualization of the pedicle (Fig. 1b). The drilling can be performed safely and should start from the lateral part of the articular mass of C2. The pedicle diameter should be measured preoperatively on the computed tomography (CT) scan images and the screw diameter must be 0.5 mm less than the pedicle. If there is a failure of pedicle screw placement, a safe ‘bail-out’ would be to perform unilateral fixation or place a lateral mass screw in C2 instead of the pedicle.
Fig. 1.
Drilling entry point in C1 (a) and C2 (b). Both C1 articular mass and C2 pedicle are defined by Freer’s dissectors
Following the insertion of the screw, further intraoperative reduction can be performed as needed, and the screws are interconnected with pre-cut pre-curved rods. Finally, cancellous bone graft, obtained from the posterior iliac crest, is placed between the C1 and C2 arches to encourage fusion.
Materials and methods (Table 1)
Table 1.
Material and methods: screws below C1 placed in the lateral masses are in brackets
| Case no. | Sex | Age | Diagnosis | Notes | C1 screws | C2 screws | C3–C4 screws | Fixation area | FU mos |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 62 | Dens non-union | Collar failure | 1 | 1 | 0 | C1–C2 | 16 |
| 2 | M | 45 | Dens non-union | Halo failure | 2 | 2 | 0 | C1–C2 | 25 |
| 3 | F | 18 | Dens non-union | Halo failure | 2 | 2 | 0 | C1–C2 | 17 |
| 4 | M | 26 | Dens non-union | Anterior screw failure | 2 | 1 + (1) | 0 | C1–C2 | 17 |
| 5 | M | 58 | Type II dens fracture | Halo refusal | 2 | 2 | 0 | C1–C2 | 21 |
| 6 | F | 31 | Type II dens fracture | Irreducible | 2 | 2 | 0 | C1–C2 | 27 |
| 7 | M | 26 | Type II dens fracture | T7 burst fracture | 2 | 2 | 0 | C1–C2 | 24 |
| 8 | M | 33 | Type II dens fracture | C6–C7 dislocation | 2 | 2 | 0 | C1–C2 | 24 |
| 9 | F | 30 | C2 body fracture | Unstable fracture | 2 | 1 | (2) | C1–C3 | 12 |
| 10 | F | 37 | Hangman’s fracture | Anterior plate failure | 2 | 0 | (2) | C1–C3 | 19 |
| 11 | M | 40 | C1–C2 instability | Os odontoideum | 2 | 2 | 0 | C1–C2 | 12 |
| 12 | M | 18 | C2–C3 osteoblastoma | – | 0 | 2 | (3) | C2–C4 | 26 |
| 13 | F | 14 | C2 osteoblastoma | Occipital paraesthesia | 2 | 1 | (2) | C1–C3 | 23 |
| 14 | M | 78 | C2 chordoma | Previous vertebroplasty | 2 | 0 | (4) | C1–C4 | 13 |
There were 8 men and 6 women, with an average age of 36 (range of 14–78 years). Three patients were classified a polytrauma (thoracic trauma in two and head trauma in one) and the remaining 11 had isolated neck injuries. Two of the polytrauma patients had an American Spinal Cord Injury Association (ASIA) A cord injury due to a T8 burst fracture, as well as a C6–C7 dislocation. A patient with a C2 osteoblastoma suffered from occipital paraesthesia. The Harms technique, as described above, was used in nine cases while a modified technique, using either C1 or C2 as endpoints of fixation, was adopted in the remaining five. In those cases the optimal grip obtained by polyaxial screws allowed us to reduce the posterior area of fixation, and excluding the fixation to the skull.
The CT scans were reviewed preoperatively in all the cases to evaluate the C2 pedicle size and analyzed for screw size acceptance and placement feasibility. Nine of the cases accepted 3.5 mm screws, while the rest had 4 mm screws. Bone graft was used in all the posterior fusions. The patients were followed for an average of 20 months (range of 12–26 months) and checked clinically and radiographically with plain radiographs and CT scans.
Results
In two of the patients, one of the C2 pedicles was too small for a screw placement, requiring a unilateral fixation in one case and a fixation to the articular mass in the other (cases 1 and 4). In two other cases presenting with tumors, either one or both the pedicles had to be removed due to tumor invasion (cases 13 and 14). C1, C3 and C4 bilateral fixation was performed in one of the cases, and the other was stabilized with C1 bilateral, C2 unilateral and C3 bilateral fixation. One more patient had a C1–C3 fusion with a unilateral C2 fixation in the fractured vertebra (Fig. 2, case 9). Overall 25 screws were implanted in the articular masses of C1 and 20 in the pedicles of C2. Postoperative CT scans showed proper placement of all the screws, except for one in C1, which was inserted between the articular mass and the odontoid without mechanical or clinical relevance.
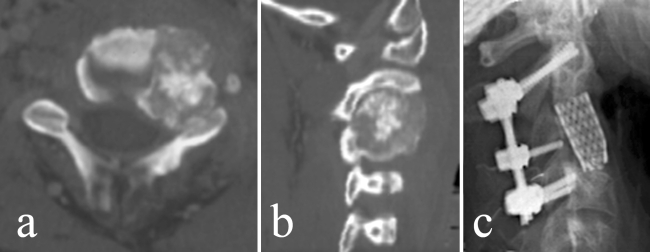
Fig. 2.
C2 vertebral body fracture in a young lady. Spinal canal narrowing is evident on the preoperative CT scans (a). Spinal canal restoration and bone healing 4 month after surgery (b). Standard X-ray control 1 year after surgery (c)
Both 3.5 and 4 mm screws can be used, although the 4 mm screws gave the intraoperative impression of better purchase in the C2 pedicles (although this size may have exceeded the pedicle diameter in some cases). Bleeding from the venous plexus during C1–C2 joint exposure was encountered frequently, and the surgeon must be aware and prepared to achieve hemostasis. Tamponade with fibrin glue on hemostatic sponge has always been an effective countermeasure. Subperiosteal exposure of C1 lateral mass significantly decreased intraoperative bleeding.
Blood transfusions were not required due to surgical blood loss during the fixation, but were needed in the three patients with polytrauma who had low preoperative hemoglobin. There were no neurological complications. The patient with the preoperative occipital paraesthesia recovered her normal sensitivity (Fig. 3). There were no local recurrences in the three patients with primary tumors, at the latest follow up of 12, 23, and 25 months.
Fig. 3.
CT scans of a C2–C3 osteoblastoma in a 18 years old patient nearly touching C2 left pedicle (a, b). C2–C4 posterior fixation after tumor excision and anterior column reconstruction (c)
Posterior fusions were achieved on an average at 4 months, except in one case. This patient developed a posterior non-union evident at 1 year, although the odontoid fracture had healed after the stabilization (case 5). Another patient with an odontoid non-union, had a successful posterior fusion and pseudoarthrosis healing was also achieved at 5 months (case 4). Although none of the patients suffered from occipital paraesthesias from C2 root injury, a small area of reduced sensitivity around the skin incision was common.
Three of the nine patients with C1–C2 fusion reported intermittent neck pain, but did not seem to interfere with their normal activities. In the same group, head rotation impairment after physiotherapy was 40° (20° on each side) compared to normal ROM.
Discussion
In our experience, the Harms’s method showed to be effective and reliable in treating C1–C2 instability with a posterior fusion. Compared to Magerl’s technique, it allows intraoperative reduction of misalignments and does not require posterior wiring. In posterior stabilizations after C2 tumor excision, it avoided an occipito-cervical fusion, giving better functional results.
In treating type 2 acute fractures of the odontoid [7], anterior screw fixation is currently considered the gold standard. Nevertheless, anterior fixation requires intraoperative double fluoroscopy, which is not always available in every hospital and it is not always indicated because of the type of fracture (small cranial fragment; difficult reduction) or because of the age of the patient (lesser healing potential in the elderly) [8, 9]. Harms proposes to stabilize the vertebrae without fusion, and removing the hardware once the fracture is healed [4]. We have always performed bone grafting in conjunction with internal stabilization. As our experience widens, we will attempt such simple stabilizations without grafting in acute fractures and present the data with a prospective study.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Gallie WE. Fractures and dislocations of the cervical spine. Am J Surg. 1939;46:495–499. doi: 10.1016/S0002-9610(39)90309-0. [DOI] [Google Scholar]
- 2.Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60:279–284. [PubMed] [Google Scholar]
- 3.Dickman CA, Sonntag VK. The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg. 1991;74:190–198. doi: 10.3171/jns.1991.74.2.0190. [DOI] [PubMed] [Google Scholar]
- 4.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 5.Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J. 2007;16:479–484. doi: 10.1007/s00586-006-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 8.Andersson S, Rodriguez M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9:56–60. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Apfelbaum RI, Lonser RR, Veres R, et al. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(Suppl 2):227–236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]