Abstract
Multiple myeloma (MM) is a B cell malignancy characterized by important alterations of physiologic bone turnover, wherein increased osteoclastic bone resorption is not accompanied by a comparable increase in bone formation, resulting in diffuse osteopenia, focal lytic lesions, pathologic fractures, hypercalcemia, and bony pain. Consequently, patients with MM frequently require for quality of life’s improvement and pain’s treatment radiation therapy, surgery, and analgesic medication. Minimally invasive surgical procedures such as the kyphoplasty allows patients with pathological osteolytic vertebral lesions to have immediate improvement in their quality of life. This surgical technique provides in myeloma vertebral collapses same quick pain relief as in osteoporotic vertebral fractures, and a minor morphological restoration of the interested vertebra, but sufficient to restore sagittal alignment. The aim of the study was to evaluate the functional and morphological results of kyphoplasty for the treatment of vertebral osteolysis due to MM. We report a retrospective study in 30 such patients (45 vertebral lesions) who were evaluated before and after kyphoplasty, with regard to pain, general condition, quality of life, use of analgesics, by means of evaluation forms: Short-Form-36, Visual Analog Scale, Oswestry Disability Index, and with regard to percentage height restored and reduction of segmental kyphosis. Marked clinical improvement was observed in all patients during the first 12 postoperative months, with gradual a little worsening thereafter from deterioration of their general condition to 60-month follow-up. The restoration of vertebral body mean height was maintained to 5 years clinical and radiographic control. Segmental kyphosis angle correction showed a mean decrease of 1.7° (range 0°–2.5°) at radiographic control at 5-year follow-up, with respect to the immediate postoperative X-ray, although lower than preoperative. The data obtained demonstrated the effectiveness of kyphoplasty in the treatment of vertebral collapse in MM. The results achieved with this minimally invasive technique were clinically and biomechanically satisfactory.
Keywords: Myeloma, Kyphoplasty, Segmental kyphosis
Introduction
Treatment of patients with oncologic disorders has resulted in an increase in quality of life and survival. With increasing longevity, an increased incidence of skeletal involvement and related complications is observed. Multiple myeloma (MM) commonly is characterized from skeletal-related complications that result from a shift in the normal balance between bone formation and bone resorption toward enhanced bone loss [1]. The lytic process observed in MM is different from other carcinomas that metastasize to the bone in which bone destruction is followed by new bone formation [2]. Even when patients respond to anti-MM therapies, they may still have progression of skeletal event without the repair of osteolytic lesions [3, 4]. Possible complications associated with these osteolytic lesions include cord compression, urinary retention, ileus, intractable pain, and pulmonary compromise [5, 6]. Other chronic sequelae include deconditioning, deformity, insomnia, and depression, resulting in substantial physical, functional and psychosocial impairment [4]. Pharmacological therapy, orthesis and radiotherapy alone are usually unable to control pain and/or to restore the integrity and stiffness of the collapsed vertebra, so as to allow a return to early weight-bearing. However, the surgical intervention in this patient group typically is regarded very difficult by the virtue of the comorbid conditions and the poor bone quality. For this reason, balloon kyphoplasty was introduced as a more effective treatment option for these fractures. The technique has shown to provide rapid pain relief, improve rehabilitation and is also capable of preventing further loss of vertebral height, which reduces the risk of increasing spinal kyphosis [7] but there have been only a few studies report on the outcome of kyphoplasty in the treatment of tumorous lesions. We report on the clinical and morphological outcome of 30 patients (45 vertebral osteolytic lesions) with MM in the thoracic and lumbar spine treated with balloon kyphoplasty. To our knowledge, this is the first report in literature to have a 5-year follow-up.
Materials and methods
Patients
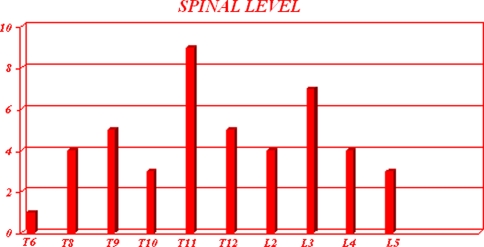
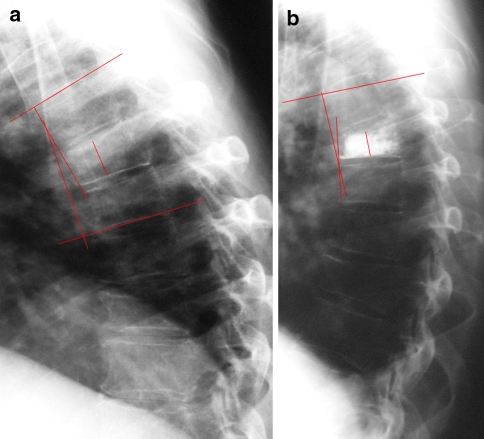
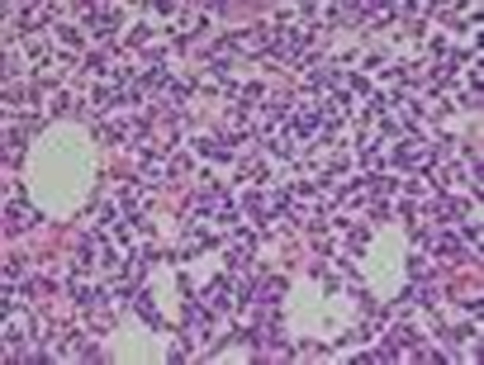
From March 2002 to January 2008 by Spine Surgery Division of Department of Orthopaedic Science and Traumatology of Catholic University 45 kyphoplasty (27 thoracic affected vertebra and 18 lumbar affected vertebra; Fig. 1) were performed in 30 patients with MM, 19 males and 11 females, with a mean age of 63 years (range 54–76 years). All patients presenting with osteolytic vertebral lesion were evaluated by a multidisciplinary team, which included hematologists, radiotherapists, spine surgeons and radiologists. All underwent chemical and hematological examinations (Table 1). The presence of an osteolytic vertebral fracture was evaluated preoperatively by standard radiography (Fig. 2a, b) and MRI (Fig. 3). Preferred fractures were those that could be identified as site of pain, and those that showed marrow edema on the inversion and fat suppression sequences. All patients had one to four levels of kyphoplasty. All were evaluated before and 1, 3, 6, 12 months and annually after kyphoplasty with regard to pain, quality of life and general condition, using the following criteria Visual Analog Scale (VAS), Short-Form-36 (SF-36) General Health Survey questionnaire, Oswestry Disability Index (ODI). Also the type and quantity of drugs taken by the patients to control the pain, during the preoperative and postoperative periods, were recorded. All vertebral collapses were morphologically evaluated with regard to mid-vertebral height restoration and reduction of segmental kyphosis (Cobb angle value) measured on pre- and postoperative lateral X-ray (Fig. 4a, b). At the time of kyphoplasty in all treated vertebra biopsies were performed using the same set of instruments (Kyphon, Medtronic Sofamor Danek, USA; Fig. 5).
Fig. 1.
Bar graph demonstrating the distribution frequency of the spinal affected levels treated by kyphoplasty
Table 1.
Pre-operative chemical and emathological exam conducted for patient’s diagnostic evaluation
| AGEC |
| Hemochrome, leukocytes’ count |
| VES |
| Protein electrophoresis |
| Urinary protein electrophoresis and immunefixation |
| Measuring of β2 microglobulin |
Fig. 2.
a Preoperative antero-posterior radiograph showing a collapsed vertebral body in a myeloma patient. b Preoperative lateral radiograph showing a collapsed vertebral body in a myeloma patient
Fig. 3.

MRI showing a series of collapsed vertebral body in a myeloma patient
Fig. 4.
a Pre-operative lateral X-ray showing the median vertebral height and the segmental kyphosis in a collapsed vertebral body. b Post-operative X-ray showing the partial restoration of the median vertebral height and the segmental kyphosis in the same vertebra
Fig. 5.
Histological findings in a biopsy performed on a myeloma collapsed vertebral body treated with kyphoplasty
Operative technique
According to the general patients’ conditions and the treated level the procedure was performed under general (n = 13 patients), or local anesthesia (n = 17 patients). Patients were positioned in the prone position and a dual portal approach is used in all procedures. In all procedures PMMA was used as filler, the volume of cement used was 4.2 cc per level (range 1.5–8 cc). A bioptic examination of the affected vertebrae was effected prior to injecting the cement. This allows the operator to obtain a small cylindrical sample of tissue. In case of local anesthesia, anesthesia was performed by injection of ropivacaine 7.5 mg (10 cc) mixed with 1% carbocaine (10 cc). The positioning of the cannula and the injection of the cement are constantly fluoroscopically monitored in antero-posterior and lateral projections. Each patient received 2 g of intravenous cefazolin 30 min prior to surgery. The average length of time of the procedure was 45 min. The average hospital stay was 3 days.
Statistics
Descriptive statistics were calculated. The clinical results obtained were analyzed using the chi-squared test and Fisher’s exact test. The morphological results obtained were analyzed using the Student’s t test. Significance was set at P < 0.05.
Results
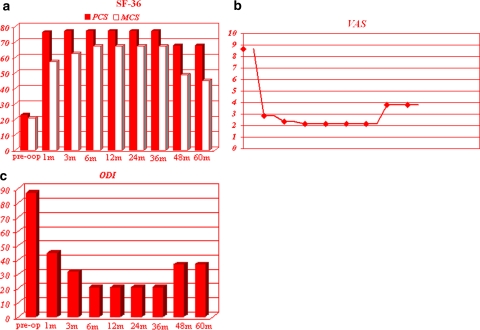
In all patients, mechanical stabilization and reduction of the deformity of the osteolytic lesion was achieved. There were no pathological fractures, and no clinical symptoms related to cement leakage. Two patients reported transiently increased back pain together with pyrexia in the immediate postoperative. In one patient, the cement was partially injected in the disc, in another there was a leakage along the needle track, but there were no clinical manifestations. An overall improvement of the quality of life of the patients was evident, and patients were able to return to their activities of daily living (Fig. 6a–c). The median follow-up was 4 years, with 13 kyphoplasty at 5-year follow-up, 8 at 4 years, 9 at 3 years, 5 at 2 years, 7 at 1 year and 3 at 6-month follow-up. The SF-36 questionnaire showed a marked improvement in physical functions up to 12 months after the surgical treatment, with an average score improving from 23% preoperatively, to 76.5% at 1 month, 77.2% at 3 months, 77.2% at 6 months, unchanged to 36-month follow-up. A little worsening was observed 4 year after the procedure, with an average score of 67.8%, unchanged to 5-year follow-up. A similar trend was observed for pain, measured by the VAS score. Pain improved from an average preoperative score of 8.65 to 2.84 at 1 month, to 2.35 at 3 months, to 2.15 at 6 months, unchanged to 36-month follow-up and to 3.80 at 4 years, unchanged to 5-year follow-up. A minor improvement was observed in mental component with an average score improving only from 21% preoperatively, to 57.2% at 1 month, 62.3% at 3 months, and 67.2% at 6 months, unchanged to 36-month follow-up. A worsening of mental component was observed at 4-year follow-up, with an average score of 48.6%, worsened at 5-year follow-up with an average score of 45%. The ODI index showed an improvement in the ability to carry out standard daily activities autonomously, with a preoperative score of 87% rising to a postoperative score of 45% 1 month after the intervention, which further improved (21%) 3 months after the treatment, unchanged to 36-month follow-up. At 4-year follow-up, a worsening of the general condition was observed, with reduced autonomy, with the average score dropping to 37%, unchanged to 5 years yet still higher than the score recorded preoperatively. We observed a reduction or, in some patient, the cessation of analgesic drug assumption, compared with the preoperative period. It is impossible to quantify the reduction of analgesic drug assumption in patients with systemic neoplastic disease, due to the coexistence of multiple secondary lesions. Nevertheless, a marked reduction of analgesic drug assumption was observed in some of our patients, even when radiotherapy was not effective.
Fig. 6.
a SF-36 data: the histogram shows the physical and mental patients’ outcome from pre-operative time to 5 years follow-up P < 0.005. b VAS data: the diagram shows the outcome of patients’ pain from pre-operative time to 5 years follow-up P < 0.005 c ODI data: the histogram shows the clinical and functional outcome of patients from pre-operative time to 5 years follow-up P < 0.005
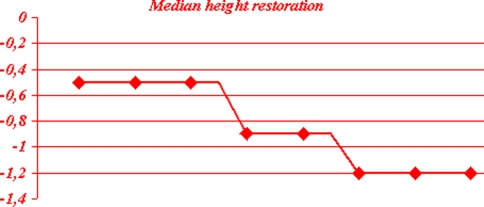
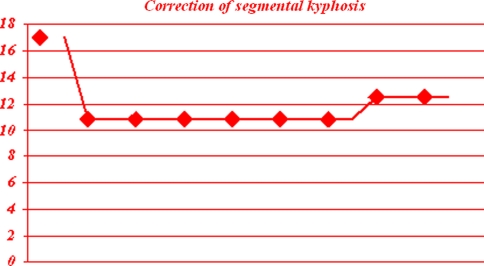
Radiologic height measurement of all 45 levels treated demonstrated that the mean central vertebral height lost was 9 mm (range 2–17.3 mm). The mean percentage of height restored by the procedure was 55% (range 0–100%). At lateral postoperative X-ray, the absolute mean height gain was 3 mm (P < 0.05), maintained unchanged to 5 years radiographic control (Fig. 7). Segmental kyphosis angle correction was calculated in all cases with Cobb angle method. The mean preoperative kyphotic angle was 17° (range 6°–38°), whereas the mean postoperative kyphotic angle was 10.8° (range 3°–30°). We achieved an average of 6.8° improvement of the segmental kyphotic angle after the procedure. Segmental kyphosis angle correction showed a mean decrease of 1.7° (range 0°–2.5°) at radiographic control at 5-year follow-up, with respect to the immediate postoperative X-ray, although lower than preoperative and still statistically significant (P < 0.05; Fig. 8).
Fig. 7.
The diagram shows the median height restoration from pre-operative to 5 years follow-up P < 0.005
Fig. 8.
The diagram shows the correction of the segmental kyphosis from pre-operative to 5 years follow-up P < 0.005
With a mean 18-month follow-up 14 patients sustained subsequent compression fractures for a patient rate of 31.1%. All the patients were treated with a new kyphoplasty, which show substantive benefits.
Bioptic examinations were diagnostic in 42 vertebral collapses for a fractures rate of 93.3%. In 29 patients, we had confirm of the progression of the MM state with bone involvement for a patient rate of 69%, in 13 patients was made a new diagnosis of myeloma with a patient rate of 31%.
In summary, complete pain relief was achieved in 59% of patients (n = 17). Pain reduction was achieved in 13 of 30 patients (41%). The mean duration of pain relief was 36 months (median 18 months). Pain recurred in three patients (10%) between 3 and 12 months. Three patients were subsequently submitted to radiation therapy, because of increasing pain and new vertebral involvement, with the presence of myelomatous tissue also in the posterior elements of the interested vertebrae. One patient died, and 29 patients were still alive at the time of the 5-year follow-up, with none patient lost to follow-up. Morphological restoration of the collapsed vertebra was good in 13 vertebra of the 45 treated (29%), satisfactory in 25 (55%), unsatisfactory in 7 (16%). No major complications occurred. There was transient local pain in some cases, and two cases of cement leakage without clinical consequences.
Discussion
Osteolytic destruction of the vertebral bodies secondary to MM subjects patients to significant morbidity and mortality. With the improved survival times because of contemporary oncologic treatment, timely intervention of effective skeletal reconstruction is of ever-increasing importance [6]. Patients with severe intractable pain caused by myelomatous compression fractures have only a few pain control options. Open surgery, if the best radical choice, is often not an option because these patients are in poor general condition or have a limited life expectancy. Radiotherapy is indicated for bone pain caused either directly or indirectly by malignant lesions. Radiotherapy does not improve the mechanical properties of the affected bone region, and transient osteoporosis is usually observed with the increased risk of pathological fractures [8, 9]. In medical literature, is well-known, the short-term pain relief following kyphoplasty for the treatment of osteoporotic and pathological vertebral compression fractures [7, 10, 11]. Kyphoplasty aims to immediately restore the mechanical properties of the affected skeletal segment, it gives to the treated vertebra an increased resistance to compressive strength resulting in the prevention of continue microtrauma responsible for pain and of an increased fracture’s risk [12]. Thus allowing immediate weight-bearing and preventing worsening of the pathological fractures. Furthermore, the exothermic reaction developed during the polymerization of the cement exerts a local cytotoxic action against the tumor also resulting in the reduction of pain. Pain relief is a result of PMMA properties, but in our series is not correlated with vertebral body volume or amount of bone cement. In our cohort of patients, we found a statistically significant improvement of pain as measured by the VAS and ODI and improvement in independence in daily life activities as shown by SF-36. The 5-year follow-up, to our knowledge, the longest period described for this technique in medical literature, allows the author to sustain the time effective pain improvement of this surgical procedure, dealing with the impact of relatively common comorbid conditions in this type of patients.
The specific advantages of kyphoplasty, in front of other percutaneous techniques, are that it makes cement augmentation of the vertebrae a safer procedure and provides the opportunity for some height restoration and correction of the segmental kyphosis [13]. In our series, cement leakage was of none clinical relevance. The restoration of vertebral body height and correction of segmental kyphosis was 55%. We documented, on an average, an absolute mid-vertebral body height restoration of 3 mm and an absolute segmental kyphosis correction of 6.8°. The height restoration was maintained unchanged to 5-year of follow-up. We instead observed an absolute reduction of segmental kyphosis correction of 2.5° at 5-year follow-up. The loss of correction is often due to the occurring of new vertebral collapses, 14 in our series of patients, with an incidence in myeloma patients higher than in osteoporotic patients [14]. We can hypothesize that myeloma uncontrolled by medical treatment might have been related to augmented bone fragility and new fracture occurrence. Therefore, myeloma patients should be warned: to avoid activities that overload the spine; to sustain frequent and constant hematological controls and adequate chemotherapy; and to indicate few days after a less invasive surgical procedure, such as kyphoplasty. The morphological results obtained are similar to those present in medical literature for the same pathology [13, 15, 16], but inferior to the correction obtained in osteoporotic fracture [14]. Correction of the deformity is, in myeloma collapsed vertebrae, possible because of the soft vascular nature of this pathology, as evidenced by the backflow of blood from the working cannulae during kyphoplasty. The near-fluid consistency of the myeloma’s tissue and the lytic nature of the bone make it easy for the inflatable bone tamp to displace tissue in the act of reducing the fracture and creating the cavity [6]. This then results in impressive cement filling of the vertebra. The effects of potential malignancy cells dissemination, in what already is widespread disease, is nowadays not known. We do not have observed any significant effects in our group and we also were able to proceed safely with the kyphoplasty in all patients simultaneously with any chemotherapy. The minor restoration of prefractured vertebral morphology is in myeloma patients probably due to the difficulty in fully differentiating the effects of bone osteolysis caused by MM versus osteoporosis caused by medications and inactivity, and also to the different fracture configuration, usually biconcave and with a higher loss in height, than those seen in true osteoporotic patients, usually wedge and when recent fewer collapsed.
Another practical advantage of balloon kyphoplasty is its ability to allow the use of a greater than 2.5 mm gauge biopsy needle that has good chances of retrieving sufficient quantity of tissue for histopathological studies. In our series, the success rate was 93.3%, with 69.9% of confirmation of diagnosis and 31% new diagnosis that allowed patients to immediately undergo an immediate adequate systemic medical treatment. These results can be improved, in the future, using technical principles of transpedicular biopsy reported in literature [17, 18].
All patients with MM present skeletal involvement and the majority of these have no neurological involvement. Hence, in MM, the majority of morbidity and mortality is caused by skeletal failure because of bone destruction. Therefore, timely intervention of effective skeletal reconstruction is of increasing importance. Because kyphoplasty have demonstrated, in these years, its safety and efficacy in improvement of pain and function, unchanged over time, and in correction of deformity, in our opinion every recent fractured or collapsed vertebral body in myeloma patients should undergo this surgical treatment, in order to avoid the structural and debilitating functional effects of a progressive spinal kyphotic alignment.
Conclusions
Balloon kyphoplasty is effective and safe in the management of MM vertebral fractures. It led to a diminution of pain, increased function, significant height restoration and reduction of segmental kyphosis, maintained unchanged to a median-time follow-up.
Conflict of interest statement
None of the authors has any potential conflict of interest.
Footnotes
S. Astolfi operated patients, conceived the study; L. Scaramuzzo drafted the manuscript, performed statistical analysis, followed patients; C.A. Logroscino operated patients and coordinated group.
Contributor Information
Stefano Astolfi, Phone: +39-06-30154353, FAX: +39-06-3051161, Email: stefano.astolfi@gmail.it.
Laura Scaramuzzo, Email: laura.scaramuzzo@virgilio.it.
Carlo A. Logroscino, Email: clogroscino@rm.unicatt.it
References
- 1.Mundy GR, Bertoline DR. Bone destruction and hypercalcemia in plasma cell myeloma. Semin Oncol. 1986;13:291–299. [PubMed] [Google Scholar]
- 2.Yeh HS, Berenson JR. Treatment for myeloma bone disease. Clin Cancer Res. 2006;12(20 Pt 2):6279s–6284s. doi: 10.1158/1078-0432.CCR-06-0681. [DOI] [PubMed] [Google Scholar]
- 3.Belch AR, Bergsagel DE, Wilson K, et al. Effect of daily etidronate on the osteolysis of multiple myeloma. J Clin Oncol. 1991;9(8):1397–1402. doi: 10.1200/JCO.1991.9.8.1397. [DOI] [PubMed] [Google Scholar]
- 4.Kyle RA, Jowsey J, Kelly PJ, Taves DR. Multiple myeloma bone desease: the comparative effect of sodium fluoride and calcium carbonate or placebo. N Engl J Med. 1975;293:1334–1338. doi: 10.1056/NEJM197512252932602. [DOI] [PubMed] [Google Scholar]
- 5.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman I, Reinhardt MK. Vertebroplasty and kyphoplasty for osteolytic vertebral collapse. Clin Orthop Relat Res. 2003;415:S176–S186. doi: 10.1097/01.blo.0000093841.72468.a8. [DOI] [PubMed] [Google Scholar]
- 7.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26:1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 8.Gilbert HA, Kagan AR, Nussbaum H, et al. Evaluation of radiation therapy for bone metastases: pain relief and quality of life. AJR Am J Roentgenol. 1977;129(6):1095–1096. doi: 10.2214/ajr.129.6.1095. [DOI] [PubMed] [Google Scholar]
- 9.Shepherd S. Radiotherapy and the management of metastatic bone pain. Clin Radiol. 1988;39(5):547–550. doi: 10.1016/S0009-9260(88)80234-4. [DOI] [PubMed] [Google Scholar]
- 10.Lieberman IH, Dudney S, Reinhardt MK, Bell G. Initial outcome and efficacy of kyphoplasty in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 11.Gaitanis IN, Hadjipavlou AG, Katonis PG, Tzermiadianos MN, Pasku DS, Patwardhan AG. Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J. 2004;14:250–260. doi: 10.1007/s00586-004-0767-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasperk C, Hillmeier J, Noeldge G, et al. Treatment of painful vertebral fractures by kyphoplasty in patients with primary osteoporosis: a prospective nonrandomized study. J Bone Miner Res. 2005;20(4):604–612. doi: 10.1359/JBMR.041203. [DOI] [PubMed] [Google Scholar]
- 13.Dudeney S, Lieberman IH, Reinhardt MK, Hussein M. Kyphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. J Clin Oncol. 2002;20(9):2382–2387. doi: 10.1200/JCO.2002.09.097. [DOI] [PubMed] [Google Scholar]
- 14.Lane JM, Hong B, Koob J, et al. Kyphoplasty enhances function and structural alignment in multiple myeloma. Clin Orthop Relat Res. 2004;426:49–53. doi: 10.1097/01.blo.0000131642.96984.74. [DOI] [PubMed] [Google Scholar]
- 15.Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg Spine. 2003;98:21–30. doi: 10.3171/spi.2003.98.1.0021. [DOI] [PubMed] [Google Scholar]
- 16.Pflugmacher R, Kandziora F, Schroeder RJ, Melcher I, Haas NP, Klostermann CK. Percutaneous balloon kyphoplasty in the treatment of vertebral body fracture and deformity in multiple myeloma: a one year follow-up. Acta Radiol. 2006;47(4):369–376. doi: 10.1080/02841850600570425. [DOI] [PubMed] [Google Scholar]
- 17.Strimgham DR, Hadjipavlou A, Dzioba RB, Lander P. Percutaneous transpedicular biopsy of the spine. Spine. 1991;19:1985–1991. doi: 10.1097/00007632-199409000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Hadjipavlou AG, Arya S, Crow WN, Maggio WW, Lander P, Nardone EM. Percutaneous transpedicular biopsy of the spine. J Interv Radiol. 1996;11:103–108. [Google Scholar]