Abstract
Pedicle screw fixation enables enhanced three-dimensional correction of spinal deformities and effectively shortens the distal fusion level. However, the choice of distal fusion level is still controversial in single thoracic idiopathic scoliosis with the lumbar compensatory curve not crossing the middle line (Lenke type 1 with modifier A or King type III and IV curves).The authors retrospectively analyzed 31 patients treated by segmental pedicular instrumentation alone, affected by a single thoracic adolescent idiopathic scoliosis with a compensatory lumbar curve not crossing the midline (Lenke 1A), with an average age of 16.3 years (range 10–22 years). The patients with regard to the King classification were also assessed. A statistical analysis was performed to determine whether the two groups (King III, King IV) presented differences concerning the level of the stable vertebra (SV), end vertebra (EV), and neutral vertebra (NV) and were also analyzed the results at follow-up regarding the relationships between the SV, EV, and lowest instrumented vertebra (LIV). The statistical analysis showed a significant difference between the two curve types. In the King III type curve the SV, EV, and NV appeared to be more proximal than those of the King IV type curve and the segments between the SV, EV, and NV appeared to be reduced in King III curves compared with King IV curves. At a follow-up of 3.2 years (range 2.2–5) the thoracic curve showed a correction of 58.4% (from 62.3° to 26.6°) and compensatory lumbar curve an average spontaneous correction of 52.4% (from 38.1° to 18.1°).The position of the LIV was shorter than the position of the SV in 30 patients (97%) with an average “salvage” of 2.1 (from 1 to 4) distal fusion levels. Four cases (13%), all affected by a King IV type curve, presented at follow-up an unsatisfactory results due to an “adding on” phenomenon. The statistical analysis confirmed that this phenomenon was correlated with The King IV curve (P = 0.043; Chi-square test) and that the only predictive parameter for its onset was the LIV–SV difference (odds ratio = 0.093; with a confidence interval of 0.008–1): every time that in King IV curve type the LIV was three or more levels shorter than the stable vertebra at follow-up the “adding on” phenomenon was present. The authors conclude that Lenke’s type 1 with modifier A includes two kinds of curves, King III and King IV and that the Lenke’s type 2 curves and King V with the lumbar curve not crossing the middle line have a similar behavior. Therefore, it is of authors’ opinion that “the adding on phenomenon” could be prevented by more rigidly defining K. IV versus K. III curves. In Lenke’s 1/2 A-K. IV/V type with the rotation of the first vertebra just below the thoracic lower EV in the same direction as the thoracic curve, and when SV and EV show more than two levels of difference, it is necessary to extend the lower fusion down to L2 or L3 (not more than two levels shorter than the SV). Whereas in Lenke’s 1/2 A-K. III/V with the rotation of the first proximal vertebra of lumbar curve in the opposite direction to the thoracic apex and when SV and EV show not more than two level gap differences, the position of the lowest instrumented vertebra can be two or three levels shorter than the stable vertebra with satisfactory postoperative spinal balance. Therefore, the stable vertebra and the rotation of lumbar curve are considered to be a reliable guide for selecting the lower level of fusion.
Keywords: Thoracic scoliosis, Selective fusion, Lenke’s classification, King’s classification
Introduction
In 1983, King and Moe [6] introduced a radiographic classification system for adolescent idiopathic scoliosis in which five different curve types were described to help surgeons identify which curve should be included in the fusion and which distal vertebra could be safely selected as the last instrumented segment. Soon after with the evolution of multiple hook or screw implant systems in the late 1980s [5, 11], which allowed for increased three-dimensional curve correction, several shortcomings became evident in the descriptions and recommendations provided by the King classification system [8]. Because of these concerns, Lenke [9] developed a new classification system for AIS that specifically quantified the curve pattern, lumbar apical vertebral translation, and sagittal alignment. This newer classification system, currently known as the Lenke’s classification system, is based on measurements of curves in both the frontal and sagittal planes and on three main variables: curve type, lumbar spine modifiers, and thoracic sagittal modifiers. The curves in which the compensatory lumbar curve does not cross the midline are type 1, with lumbar modifier (A). In King’s classification, the similar single main thoracic AIS curves, with a compensatory lumbar curve not crossing the midline, were classified as either type III (defined as a C-shaped single thoracic curve with a compensatory lumbar curve that does not cross the midline) or type IV (defined as a long single thoracic curve with the tilt of the fourth lumbar vertebra into the curve). For the first time in 1983 King [6] observed that in type III and IV curves the common error in selecting the fusion levels was to end the lower level of fusion at the neutral vertebra, being shorter than the stable vertebra. Although modern instrumentation systems have dramatically increased the ability to correct the three-dimensional deformity in adolescent idiopathic scoliosis [11, 16], the selected fusion of the thoracic curve with the compensatory lumbar curve not crossing the middle line (Lenke 1A, or King III, King IV type curves) still presents difficulties, as reported by Se-Il Suk’s [17, 18].
The purpose of the present study was: (1) to determine whether Lenke’s type 1, modifier A curve group includes two kinds of curve classified by King, type III and type IV, (2) to determine whether there is a statistical difference between, King’s type III or IV curves, and (3) to assess the better distal fusion level in single thoracic curves with a compensatory curve not crossing the midline (Lenke 1A, King III and IV) with reference to the position of stable vertebra (SV) and to the rotation of compensatory lumbar curve.
Materials and methods
A retrospective review, based on a database search, was performed on a consecutive series of 110 patients, affected by thoracic adolescent idiopathic scoliosis, surgically treated at our ward by selective fusion, using either hybrid instrumentation (pedicle screws and hooks) or segmental pedicle screw instrumentation alone between 2000 and 2005. A total of 31 consecutive patients met our inclusion criteria: (1) diagnosis of AIS, (2) adolescent age at surgery, (3) presence of single main thoracic curves with a compensatory curve not crossing the midline—Lenke 1A, (4) surgical treatment based on the one-stage posterior instrumentation by segmental pedicle screws alone, (5) results considered at a minimum clinical and radiographic follow-up of 2 years. Preoperative long-cassette standing upright anteroposterior (AP) and lateral radiographs, as well as right and left bending coronal radiographs, were independently reviewed. Standing long-cassette AP and lateral radiographs from three different time periods (preoperative, immediate postoperative, and latest follow-up) were evaluated to determine changes in radiographic characteristics over time. The stable (SV), neutral (NV), lower end (EV) and lowest instrumented vertebrae (LIV) were identified for all curves [14]. We considered the vertebra stable when bisected or most closely bisected by CSVL [6]. Both the Lenke’s [9] and King’s [6] surgical classifications of AIS were used to describe curve patterns. Besides the values of major thoracic (MT) and compensatory lumbar (TL/L) curves, the global coronal balance as the distance (cm) between the C7 plumb line and CSVL, the translation of the apical thoracic vertebra (AVT), as the distance (cm) between C7 plumb line and the centre of the apical thoracic vertebral body or disc were also calculated. The lowest instrumented vertebra tilt angle (LIV tilt) on the coronal plane (angle between a horizontal line and the lower endplate of LIV) was also computed in degrees. For statistical analysis, a vertebral labeling system was established: T12 = 12, L1 = 13, L2 = 14, and so forth. This identification permitted the calculation of the vertebra position for the SV, EV, NV, and the difference between the vertebra position of the SV, EV, and NV on preoperative radiographs, whereas the differences between the vertebra position for the LIV and SV were computed on postoperative radiographs. In conclusion, these calculations assessed whether the two groups (King III, King IV) presented statistical differences concerning the level of SB, EV, NV and defined the mean position of the LIV with respect to the SV. Lastly, we considered without a statistical analysis the rotation of the first lumbar vertebra just below the lower thoracic end vertebra.
Statistical analysis
All continuous data are expressed in terms of mean and standard deviation of the mean. In uninvariate analysis, the Mann Whitney test evaluated by Monte Carlo method for small samples was performed to test continuous data differences between groups. The paired t test was performed to investigate the differences between the preoperative situation and follow-up time. The Wilcoxon was used to check t test results. Logistic regression (with backward Wald Statistics) was performed as multivariate analysis to define independent predictor factor test and also to identify the relative effect (odds ratio), in increasing the risk for the onset of the “adding-on” phenomenon. For all tests, P < 0.05 was considered significant. Statistical analysis was carried out by the Statistical Package for the Social Sciences (SPSS) software version 15.0 (SPSS Inc., Chicago, USA).
Results
Preoperative evaluation
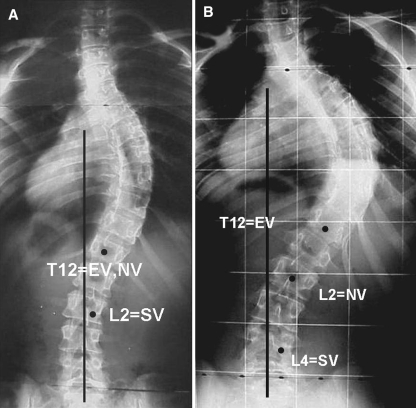
Of the 31 patients, 26 were female and 5 male with average age of 16.3 years (range 10–22 years). At the time of surgery, skeletal maturity according to Risser’s sign was 0 in 6 cases, 1 in 1, 2 in 4, 3 in 8, 4 in 10, and 5 in 2 with a mean of 2.6. The Lenke’s classification showed a type 1 curve in 20 cases and a type 2 curve in 11 [9]. The classification with regard to the King’s principles showed 11 cases with a King type III curves, 5 with a V type curves (the lumbar curve had a behavior similar to King III curves), 9 with a King type IV curve, 6 with a King V type curve with behavior similar to King type IV curve. In all 31 patients the centre sacral vertical line CSVL fell between the pedicles of each lumbar vertebra from the sacrum up to SV (Lenke’s modifier A).The analysis confirmed a statistically significant difference between the two curves in almost all parameters examined (Table 1). In type III/V curves the mean position of the SV was more frequent in L2, and of NV in T12, whereas in type IV/V curves the mean position of SV was more frequent in L4 and that of NV in L3. Then the two curve groups showed the gap differences of NV–EV, SV–EV to be significantly different. Among the King type III/V curve group (16 cases), preoperative NV was at the same level as the EV in ten patients (62%), one level distal to EV in six; among type IV/V curves the NV was at the same level of the EV in one patient, one level below in three, two levels in eight, and three levels in three. Similarly, the SV was not more than two segments distal to EV in King III/V but more than three segments in King IV. Lastly, we observed that in King III/V type the rotation of the first vertebra just below the thoracic lower EV was rotated in the opposite direction to the thoracic curve, whereas in King type IV/V the same vertebra appeared rotated in the same direction as the thoracic curve (Fig. 1a, b).
Table 1.
Statistical analysis of mean position of vertebrae and gap difference
| King III/V | King IV/V | Mann–Whitney | |
|---|---|---|---|
| Mean position of vertebra | |||
| SV | 14.6 (±0.47) (L2–L3) | 15.9 (±0.45) (L3–L4) | P < 0.0005 |
| NV | 12.5 (±0.63) (T12-L1) | 14.4 (±0.8) (L2–L3) | P < 0.0005 |
| EV | 12 (±0) (T12) | 12.47 (±0.74) (T12–L1) | P = 0.019 |
| Difference (segments) | Difference (segments) | ||
|---|---|---|---|
| NV–EV | 0.5 (±0.5) | 1.9 (±0.7) | P < 0.0005 |
| SV–EV | 1.6 (±0.4) | 3.4 (±0.6) | P < 0.0005 |
| SV–NV | 2.18 (±0.6) | 1.53 (±0.6) | P = 0.011 |
SV stable vertebra, NV neutral vertebra, EV lower thoracic end vertebra
Bold values indicate more frequent
Fig. 1.
a Lenke’s type 1, modifier A-King III type curve: the compensatory lumbar curve not crossing the middle line. The rotation of the vertebra just below the lower thoracic end vertebra is in the opposite direction of lower thoracic EV, the gap difference of SV–EV is three levels lesser than the SV, the EV and NV are the same. b Lenke’s type 2, modifier A-King V type curve: the compensatory lumbar curve not crossing the middle line. The rotation of the vertebra just below the lower thoracic end vertebra is in the same direction of thoracic curve, the gap difference of SV–EV is three levels more than SV, the NV is two levels below the EV
Postoperative evaluation
At the most recent follow-up the MT curve showed an average correction of 58.4% (±7), and TL/L curve an average spontaneous correction of 52.4%; the global coronal balance improved from 1 cm (±0.6) to 0.4 cm (±0.2), the AVT for the MT curve improved from 2.3 cm (± 0.7) to 1.7 cm (± 0.2) (Table 2). Both the coronal displacement and coronal tilt of the LIV showed a statistically significant improvement. In comparing the lowest instrumented vertebra (LIV) position to the SV, we found (Table 3) a better average “salvage” of distal fusion levels in King IV group. Among the 31 patients, regardless the type of curve, the distal fusion was down to L3 in 1 patient, L2 in 10, L1 in 16, and T12 in 4, corresponding to three levels shorter than stable vertebra in eight patients, two levels in 18, one level in 4, and down to SV in 1 patient. Therefore, the LIV was identified above the level of SV in 30 patients (97%) with an average “salvage” of 2.1 (from 1 to 4) distal fusion levels.
Table 2.
Preoperative follow-up and overall percent correction of main thoracic, secondary lumbar and coronal balance indexes
| Preop | FU | Corr. (%) | Sign | |
|---|---|---|---|---|
| MT (°) | 62.3 (±14) | 26.6 (±12) | 58.4% (±7) | >0.0001 |
| Lumbar curve (°) | 38.1 (±7.5) | 18.1 (±4.5) | 52.4% (±11.5) | >0.0001 |
| Global coronal balance (cm) | 1 (±0.6) | 0.4 (±0.2) | 52% (±8.7) | >0.0001 |
| AVT (MT curve) (cm) | 2.3 (±0.7) | 1.7 (±0.2) | 55.5% (±6.4) | >0.0001 |
| LIV translation | 2 (±0.5) | 0.7 (±0.15) | 65% (±9.15) | >0.0001 |
| LIV Tilt | 21.3 (±11.5) | 5.2 (±5.6) | 76.5% (±11.0) | >0.0001 |
MT main thoracic curve, LIV lowest instrumented vertebra, AVT apical thoracic vertebra translation
Table 3.
Mean difference between stable, end, and neutral vertebra with respect to the lowest instrumented vertebra
| King III/V | King IV/V | Mann–Whitney | |
|---|---|---|---|
| Difference (segments) | Difference (segments) | ||
| LIV–NV | 0.5 (±0.7) | −0.9 (±0.59) | P < 0.0005 |
| LIV–EV | 1 (±0.7) | 1 (±0.6) | n.s. |
| LIV–SV | −1.6 (±0.7) | −2.4 (±0.5) | P = 0.0001 |
LIV lowest instrumented vertebra, NV neutral vertebra, EV end vertebra, SV stable vertebra
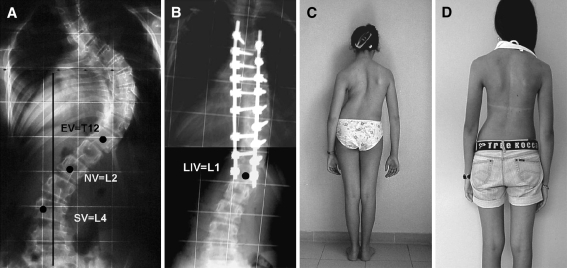
Unsatisfactory results were detected in four cases (13%) for the presence at follow-up of a progression of the main thoracic curve in compensatory lumbar curve, currently known as “adding on phenomenon”: none in King type III/V, and four (25%) out of the 15 cases with King type IV/V curve. The presence of the “adding-on” phenomenon was statistically correlated with King curve type IV (P = 0.043; Chi-square test). The multivariate analysis, performed with logistic regression in backward Wald method, revealed that the only predictive parameter for the onset of the “adding-on” phenomenon was the LIV–SV difference (odds ratio = 0.093, with a confidence interval 0.008–1); meaning that every single level of shorter fusion was exposed to a 89.7% higher risk for the onset of “adding-on” phenomenon in King type IV curves.
Discussion
Our understanding of optimal adolescent idiopathic scoliosis fusion techniques and results continues to evolve [4]. The primary goal of surgical treatment in adolescent idiopathic scoliosis (AIS) remains the arrest of further curve progression by obtaining a solid arthrodesis mass, long-term balance of the spine both in the sagittal and in the coronal plane, with preservation of the maximum number of motion segments [2, 7, 12]. With the introduction of more powerful instrumentation systems for the correction of scoliosis, such as segmental pedicle screws [5, 10, 15, 16] there is a growing interest in selective thoracic fusion which provides for the correction of the major curve while maintaining mobile lumbar motion segments. According to these advancements, an effort for more comprehensive curve classification and better instrumentation techniques has been observed. However, even with the most powerful devices and new classifications, the reduction of fusion extent often is complicated by postoperative decompensation [1, 3, 13, 19] and “adding on” of compensatory lumbar curves, particularly for King type III and IV curves [17]. King [6] observed, after the correction by Harrington implants, that in type III and IV curves the common error in selecting the fusion levels was to end the lower level of fusion at the neutral vertebra, being shorter than the stable vertebra. This error resulted in additional levels being added to the thoracic curve (adding on phenomenon) in 62% of cases. The author therefore suggested that the neutral vertebra did not seem to be a reliable guide for selecting the lower level of fusion and recommended in type III and IV curves ending the fusion at the first vertebra bisected by the centre sacral line (SV). Lenke [9] provided better criteria to help distinguish compensatory lumbar curves that are amenable to selective thoracic fusion from the double major curve pattern that should be managed with fusion of both curves. However, in Lenke’s type 1 curve or 2 with modifier A (thoracic curve with compensatory lumbar curve not crossing the middle line) two groups of curves are included, such as King III and IV type curves, not equivalent in terms of end, neutral, and stable vertebra levels. A paper by Se-Il Suk’s [17, 18] in the era of pedicle screws instrumentation alone, first focused on the same difficulties to obtain satisfactory results by selective fusion in single thoracic curve with the compensatory lumbar curve not crossing the middle line (Lenke’s type 1 or 2 with modifier A or King III, King IV) and concluded that the gap differences of NV–EV and LIV–NV were significantly different between satisfactory and unsatisfactory results. This author also recommended fusing to the NV or NV-1, when the NV and EV were the same or one level different, whereas when the NV and EV were two or more levels apart, fusion down to NV-2 or -3 presented unsatisfactory results (adding on). The purpose of our study was to confirm that the two groups (King III, King IV) presented statistical differences concerning the level of SB, EV, and NV. Our results confirmed this; the King type III/V curves presented constantly a more proximal position of the SV, and NV than King type IV/V curves, whereas for the EV we did not find a significant difference. Furthermore, we found that the two curve groups showed the gap differences of NV–EV, SV–EV to be significantly different. In King III/V, the EV and NV were frequently in the same position (62%); conversely, in King IV/V only in one case the two vertebrae were same, whereas in the remaining patients the NV was two levels or more distal. We observed a similar pattern in the gap difference of SV–EV. Our statistical analysis also confirmed that the relationship between the LIV and the SV is an important factor to obtain a balanced fusion and that this relationship has to be considered preoperatively regarding the type of curve (K3 or K4). When the gap difference of SV–EV is more than three levels (K4/5), the extent of fusion shorter by three levels or more than SV carries a higher risk of unsatisfactory results. Four (57%) of 7 patients with King type IV/5 curve on which the extent of distal fusion was three levels shorter (L1) than the SV showed at follow-up a progression of the main thoracic curve in compensatory lumbar curve (Fig. 2a–d). In the remaining eight patients similar for King type curve (IV/V) but with distal fusion extended down two levels shorter (L2) than SV, we had satisfactory balance at follow-up. Our findings also confirmed that pedicle screw fixation in AIS offers an enhanced three-dimensional deformity correction and preservation of motion segments by reducing the number of levels fused [18]. In our series the LIV, regardless of the type of curve, was identified above the level of SV in 30 patients (97%) with an average “salvage” of 2.1 (from 1 to 4) distal fusion levels. Lastly, a careful review of the preoperative radiographs showed constantly that in King III/V type the first vertebra just below the thoracic lower EV was rotated in the opposite direction to the thoracic curve, whereas in King type IV/V the same vertebra appeared to be rotated in the same direction as the thoracic curve. After this study we consider the rotation of the first proximal vertebra of the lumbar curve to be an important element in defining the curve (K3 or K4) and so for determining fusion levels.
Fig. 2.
a Preoperative standing anteroposterior radiograph of a 14.8-year-old girl with a thoracic curve Lenke’s 2 type modifier A-King V with compensatory lumbar curve not crossing the middle line. The rotation of the vertebra just below the lower thoracic end vertebra is in the same direction of thoracic curve, the gap difference of SV–EV is more three levels than SV. b Anteroposterior radiograph taken 3 years after surgery. The distal fusion was extended down to L1 (three levels proximal to the stable vertebra). The compensatory curve shows an extension of the thoracic curve into the lumbar segments through adding on. c, d The postoperative adding-on, however, is related to a moderate clinical imbalance
Conclusion
The authors conclude that Lenke’s type 1/2 with modifier A include two kinds of curves, King III/V and King IV/V and that the Lenke’s type 2 curves and King V with the lumbar curve not crossing the middle line have a similar behavior. Therefore, it is of authors’ opinion that “the adding on phenomenon” could be prevented by more rigidly defining K. IV/V versus K. III/V curves. In Lenke’s 1/2 A-K. IV/V type with the rotation of the first vertebra just below the thoracic lower EV in the same direction as the thoracic curve, and when SV and EV show more than two level gap differences, it is necessary to extend the lower fusion down to L2 or L3 (not more than two levels shorter than the SV).Whereas in Lenke’s 1/2 A-K. III/V with the rotation of the first proximal vertebra of lumbar curve in the opposite direction to the thoracic apex and when SV and EV show not more than two level gap differences, the position of the lowest instrumented vertebra can be two or three levels shorter than the stable vertebra with satisfactory postoperative spinal balance Therefore, after this study we consider the rotation of the lumbar vertebra just below the lower thoracic EV an important factor like the stable vertebra position for determining fusion levels in the single thoracic curves with the lumbar compensatory curve not crossing the middle line.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Benli IT, Tüzüner M, Akalin S, Kiş M, Aydin E, Tandoğan R. Spinal imbalance and decompensation problems in patients treated with Cotrel- Dubousset instrumentation. Eur Spine J. 1996;5:380–386. doi: 10.1007/BF00301965. [DOI] [PubMed] [Google Scholar]
- 2.Dobbs MB, Lenke LG, Kim YJ, Yongjung J, Kamath G, Peelle M, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks vs. screws. Spine. 2006;31:2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, McAllister JW, Betz RR, Huss G, Clancy M, Schoenecker PL. Coronal decompensation produced by Cotrel-Dubousset “derotation” manoeuvre for idiopathic right thoracic scoliosis. Spine. 1991;16:769–777. doi: 10.1097/00007632-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH. Surgical treatment of idiopathic adolescent scoliosis. Spine. 1999;24:2607–2616. doi: 10.1097/00007632-199912150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 6.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 7.Lenke LG, Betz R, Bridwell KH, Harms J, Clements D, Lowe T. Spontaneous lumbar curve coronal correction after selective anterior or posterior thoracic fusion in adolescent idiopathic scoliosis. Spine. 1999;24(16):1663–1672. doi: 10.1097/00007632-199908150-00007. [DOI] [PubMed] [Google Scholar]
- 8.Lenke LG, Betz RR, Bridwell KH, Clements DH, Harms J, Lowe TG, Shufflebarger HL. Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1998;80:1097–1106. doi: 10.2106/00004623-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Lenke L, Betz R, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 10.Liljenqvist UR, Halm HFH, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Liljenqvist UR, Lepsien U, Hackeberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Margulies JY, Floman Y, Robin GC, Neuwirth MG, Kuflik P, Weidenbaum M, Farcy JP. An algorithm for selection of instrumentation levels in scoliosis. Eur Spine J. 1998;7:88–94. doi: 10.1007/s005860050036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marson DE, Carango P. Spinal decompensation in Cotrel-Dubousset instrumentation. Spine. 1991;8:S394–S403. [PubMed] [Google Scholar]
- 14.Potter BK, Rosner MK, Lehman RA, Polly DW, Schroeder TM, Kuklo TR. Reliability of end, neutral, stable vertebrae identification in adolescent idiopathic scoliosis. Spine. 2005;30:1658–1663. doi: 10.1097/01.brs.0000170290.05381.9a. [DOI] [PubMed] [Google Scholar]
- 15.Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke type I adolescent idiopathic scoliosis curves. Spine. 2005;30:1859–1866. doi: 10.1097/01.brs.0000174118.72916.96. [DOI] [PubMed] [Google Scholar]
- 16.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–495. doi: 10.1097/00002517-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Suk S, Lee S, Chung E, Kim J, Kim W, Sohn H. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis in type III an IV curves. Spine. 2003;28:484–491. doi: 10.1097/00007632-200303010-00014. [DOI] [PubMed] [Google Scholar]
- 18.Suk S, Lee S, Chung E, Kim J, Kim S. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 19.Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. Decompensation after Cotrel-Dubousset instrumentation of idiopathic scoliosis. Spine; 1990;15:927–931. doi: 10.1097/00007632-199009000-00017. [DOI] [PubMed] [Google Scholar]