Abstract
Grob et al. (Eur Spine J 5:281–285, 1996) illustrated a new fixation technique in inveterate cases of grade 2–3 spondylolisthesis (degenerative or spondylolytic): a fusion without reduction of the spondylolisthesis. Fixation of the segment was achieved by two cancellous bone screws inserted bilaterally through the pedicles of the lower vertebra into the body of the upper slipped vertebra. Since 1998 we have been using this technique according to the authors’ indications: symptomatic spondylolisthesis with at least 25% anterior slippage and advanced disc degeneration. Afterwards this technique was used also in spondylolisthesis with low reduction of the disc height and slippage less than 25%. In every case we performed postero-lateral fusion and fixation with two AO 6.5 Ø thread 16 mm cancellous screws. From 1998 to 2002 we performed 62 fusions for spondylolisthesis with this technique: 28 males (45.16%) and 34 females (54.84%), mean age 45 years (14–72 years). The slipped vertebra was L5 in 57 cases (92%), L4 in 2 cases (3.2%), L3 in 1 case (1.6%), combined L4 and L5 in 2 cases (3.2%). In all cases there was an ontogenetic spondylolisthesis with lysis. Lumbar pain was present in 22 patients and lumbar-radicular pain was present in 40 patients. The mean preoperative VAS was 6.2 (range 5–8) for lumbar pain, and 5.5 (range 4–7) for leg pain. The fusion area was L5–S1 in 53 cases (85.5%), L3–L4 in 1 case (1.6%), L4–S1 in 8 cases (12.9%). A decompression of the spinal canal by laminectomy was performed in 33 procedures (53%). When possible a bone graft was done from the removed neural arc, and from the posterior iliac crest in the other cases. The mean blood loss was about 254 ml (100–1,000). The mean operative time was 75 min (range 60–90). The results obtained by computerized analysis at follow-up at least 5 years after surgery showed a significant improvement in preoperative symptoms. The patients were asymptomatic in 52 cases (83.9%); strained-back pain was present in 8 cases (12.9%), and there was persistent lumbar-radicular pain in 2 cases (3.2%). The mean ODI score was 2.6%, the mean VAS back pain was 1.3, the mean VAS leg pain 0.7. Some complications were observed: a nerve root compression by a screw invasion of intervertebral foramen, resolved by screw removal; an iliac artery compression by a lateral exit screw from pediculo, resolved by screw removal; a deep iliac vein phlebitis with thrombosis caused by external compression due to a wrong intraoperative position, treated by medicine. Two cases of synthesis mobilization and two cases of broken screws was detected. No cases of pseudoarthrosis and immediate or late superficial or deep infection were observed. The analysis of the long-term results of the spondylolisthesis surgical treatment with direct pediculo-body screw fixation and postero-lateral fusion gave a very satisfactory response. The technique is reliable in allowing an optimal primary stability, creating the best biomechanical conditions to obtain a solid fusion.
Keywords: Spondylolisthesis, Spinal fusion, Back pain, Radicular pain
Introduction
Lumbar spondylolisthesis is a disease with several etiopathogenesis. The stage of pathologic anatomy and radiological appearance, the age and the clinical aspect of the patients are different when they are diagnosed. When the symptoms are persistent and conservative treatment fails, a surgical solution may be taken. The surgical technique and the type of fixation must be chosen according to clinical and radiological findings.
The direct pediculo-body fixation suggested by Grob et al. [9], in which two AO cancellous bone screws are inserted bilaterally through the pedicles of the lower vertebra into the body of the upper slipped vertebra with postero-lateral fusion, is an option. This procedure can be associated with decompression or another fusion at the superior level. The indications are fairly limited: a significant reduction in the height of the interposed disc and a vertebral slippage of at least 25%, together with a good balance of the spine on the sagittal plane, are necessary. The advantages of this technique are that it is easy and low cost.
The aim of this study is to bring the long-term results we have obtained with this technique into surgical treatment of lumbar spondylolisthesis.
Materials and methods
Our study was made by a non-randomized prospective study in patients operated for lumbar spondylolisthesis at Galeazzi Orthopaedic Institute in Milan. Among them 62 operated cases between 1998 and 2002, with a follow-up of at least 5 years (follow-up on average 7.2 years) were selected and analysed by computer.
They were symptomatic patients resistant to conservative treatment. All patients had radiological appearance of advanced disc degeneration and slippage of the vertebra of at least 25%.
All patients underwent standard X-rays in antero-posterior, lateral projections and flexion/extension. In all patients RNM was performed. In some cases, standing AP and LL X-rays were also performed for the sagittal spine balance evaluation. We performed EMG only in the presence of neurological damage.
The surgical approach was performed through a standard posterior exposure to the involved segment, exposing its posterior bony elements. Adequate decompression of the spinal canal was performed in patients with stenotic symptoms. Fixation of the slipped vertebra was achieved by two AO 6.5 cancellous bone screws with 16-mm threads in titanium. As described by Grob et al. [9], the screws were placed under fluoroscopic control, the entry point corresponding to the posterior extension of the lower margin of the pedicle in the lateral projection. The screws were inserted diagonally, caudal-rostrally, through the pedicle of the inferior vertebra, and an inward angle 5–10° was maintained in sagittal direction. When necessary a laminectomy was performed as an additional procedure to decompress nerve roots. Additionally, postero-lateral fusion with autologous bone graft from iliac crest or from the removed neural arc was performed. Patients were mobilized on the first postoperative day; a soft brace was worn for 4 months. The mean operative time was 75 min (range 60–90). The mean blood loss was 254 ml (range 100–1,000 ml).
All patients were monitored with clinical evaluation and X-rays at 4 months, 1 year, 2 years and 5 years after surgery. Postero-lateral spinal fusion mass was evaluated according to the Christensen et al. [5] classification. They were also requested to fill in a questionnaire for ODI and VAS, directly or by mail, to which 43 patients responded.
Results
There were 28 males (45.2%) and 34 females (54.8%); the mean age was 45 years (range 14–72). The slipped vertebra was the L5 in 57 cases (92%), L4 in 2 cases (3.2%), L3 in 1 case (1.6%) and combined (L4 and L5) in 2 cases (3.2%). In all cases there was an ontogenetic spondylolisthesis with lysis. All patients suffered from lumbar back pain (22 cases) or lumbar and radicular pain (40 cases). The mean preoperative VAS was 6.2 (range 5–8) for lumbar pain, and 5.5 (range 4–7) for leg pain. No neurological root deficit was noted (Table 1).
Table 1.
Patient characteristics
| Sex (female/male) | 34/28 |
| Age (years) | 45 (14–72) |
| Diagnosis | |
| Spondylolisthesis L5 | 57 |
| Spondylolisthesis L4 | 2 |
| Spondylolisthesis L3 | 1 |
| Spondylolisthesis L4 and L5 | 2 |
| Lumbar back pain | 22 (VAS 6.2) |
| Lumbar and radicular pain | 40 (VAS 5.5) |
The evaluation of pre-operative X-rays was made according to the Boxall et al. [3] measurement criteria; the mean slippage was 38%, the mean sacral inclination 42°, the mean lumbar index 67% and the mean lumbar lordosis 53°.
The fusion area was L5–S1 in 53 cases (85.5%), L3–L4 in 1 case (1.6%) and L4–S1 in 8 cases (12.9%). When fusion was done at two levels, translaminar screws were placed at upper level and pediculo-body screw fixation in the lower segment (four cases); a postero-lateral fusion without instrumentation was associated in one case, and a dynamic stabilization in two cases. In one case, the pediculo-body screw fixation was performed on two levels.
Decompression of neurological elements was made by removing the posterior neural arc en-block in 33 cases (53.2%). The bone graft was taken from the iliac crest (29 cases) or from the en-block removed posterior neural arc (33 cases) (Table 2).
Table 2.
Operated level(s)
| One level | 54 |
| Two levels | 8 |
| L5–S1 | 53 |
| L3–L4 | 1 |
| L4–S1 | 8 |
| Supplementary neural decompression | 33 |
The results obtained by computerized analysis at follow-up at least 5 years after surgery, showed a significant improvement in preoperative symptoms. The patients were asymptomatic in 52 cases (83.9%), while strained-back pain was present in 8 cases (12.9%). There was a persistence of lumbar radicular pain in two patients (3.2%), but we were unable to find a justification for the symptoms.
The overall result of the questionnaire, which 43 patients answered (out of 62) gave a 2.6% ODI score (0–20% = minimal disability), a VAS back pain rating of 1.3 and a VAS leg pain average 0.7 (0 = no pain/10 = maximum pain) (Table 3).
Table 3.
Clinical results
| Asymptomatic | 52 (83.9%) |
| Back pain | 8 (12.9%) |
| Radicular pain | 2 (3.2%) |
| ODI score | 2.6% |
| VAS back pain | 1.3 |
| VAS leg pain | 0.7 |
Unfortunately it was not possible to compare ODI results with the pre-operative results, as our prospective study started before the publication and the diffusion of the same [8].
The standard and dynamic X-ray showed a postero-lateral spinal fusion mass that was judged a fusion in all cases according to the Christensen et al. classification. Pediculo-body fixation technique allows a good evaluation of the postero-lateral fusion mass since nothing is hidden by instrumentation.
Some complications were observed. We had a symptomatic deep vein thrombosis, probably caused by bad patient-positioning on the operative table, resolved with medical treatment. In one case there was a neurological deficit resolved by removing the screw that had created a conflict with the corresponding nerve root. In one case there was a compression of the iliac artery by the screw; there was complete regression of symptoms after removing the screw. In two cases there was a mobilisation of synthesis with back pain, in both cases removed and two cases of broken screws, of which one case with back pain required removal.
No cases of pseudoarthrosis and no cases of immediate or late superficial or deep infections were observed (Table 4).
Table 4.
Complications
| Complications | No. | Treatment | Results |
|---|---|---|---|
| Deep vein thrombosis | 1 | Medical | Recovery |
| Neurological deficit | 1 | Screw removal | Recovery |
| Compression of the iliac artery | 1 | Screw removal | Recovery |
| Mobilisation of synthesis | 2 | Screw removals | Recovery |
| Broken screw | 2 | 1 Screw removal | Recovery |
Discussion
Lumbar spondylolisthesis is a disease with several etiopathogenetic origins, as shown by Marchetti and Bartolozzi [12]. The aspect of pathologic anatomy and radiological findings, the age and clinical appearance of the patients are different when they are diagnosed. If conservative treatment fails this may be an indication for surgery. The different surgical techniques used must be selected on the basis of the etiology, symptoms and radiological findings.
The gold standard of the spondylolisthesis surgical treatment is fusion. The different techniques for fusion discussed in literature have advantages and disadvantages [2], with mixed and variable results and with the possibility of having several complications [7], which must be taken into account in the choice of treatment.
The postero-lateral fusion without instrumentation presents a fairly high risk of pseudoarthrosis and loss of correction, particularly if there is significant slippage of the vertebra and a local kyphosis. The use of an internal fixation gives a lower rate of non-fusion, thanks to the improvement of primary stability [4], but increases the risk of infection and possible iatrogenic damage. The reduction of spondylolisthesis presents considerable advantages, such as the restoration of normal anatomy with the correction of local kyphosis and sagittal balance, improved decompression of the neurological elements and a favourable condition for fusion. However, a postero-lateral fusion, after reduction, has a high risk of instrumentation failure with the possibility of breakage or loss of correction. That is why we need circumferential fusion (PLIF) or associated anterior approach, but this increases the surgical time and intra-and post-operative risks.
One option is a postero-lateral “in situ” fusion proposed by Grob et al. This technique combines the simplicity and speed of fixation with the advantage of a three-column stabilization [11]. The technique can also associate other surgical procedures, which may be necessary such as decompression or another fusion at the superior level [1]. Further advantages of this technique are the limited space occupied by the implant with a greater surface for fusion area, reduction of infection risk and low cost (Fig. 1).
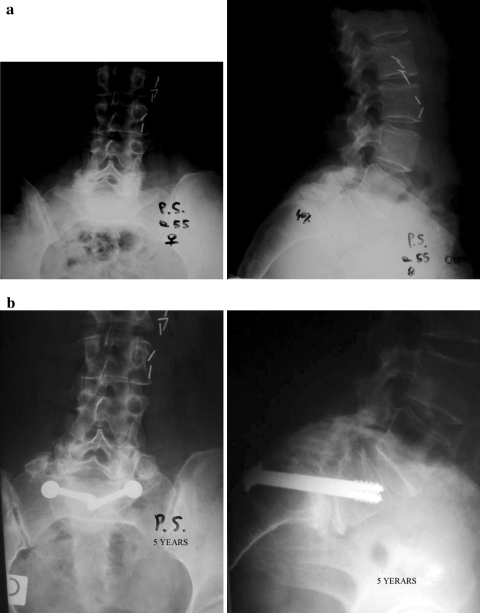
Fig. 1.
a A 55-year-old female with L5/S1 ontogenetic spondylolisthesis with isthmic lysis, 40% of slippage and severe back pain. b The same patient 5 years after pediculo-body screw fixation and postero-lateral fusion L5/S1, good fusion—the patient is pain free
The limit of this technique is a sagittal spine imbalance [6–10], which would require a reduction of the spondylolisthesis.
The purpose of this study was to report the long-term results obtained with this surgical technique in the treatment of lumbar spondylolisthesis.
From an analysis of the literature we did not find any studies on the use of this technique, except those described by the authors, who had proposed it [1–9].
The analysis of our results with a follow-up of at least 5 years (average 7.2), showed that the clinical results are excellent or good in 96.8% of the cases, with a 2.6 ODI score, a 1.3 average VAS back pain and 0.7 average VAS leg pain. The complications were numerically small, and without consequences to the clinical and radiological outcomes.
Conclusion
The analysis of the long-term results of the spondylolisthesis surgical treatment with direct pediculo-body screw fixation and postero-lateral fusion gave a very satisfactory response. The technique is reliable in allowing an optimal primary stability and creating the best biomechanical conditions to obtain a solid fusion. The advantages of this technique are: few complications, the simplicity and speed of execution, the versatility and the low cost of synthesis. The success of the surgery is due to the correct indication.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Abdu WA, Wilber R, Emery SE. Pedicular transvertebral screw fixation of the lumbosacral spine in spondylolisthesis. Spine. 1994;19:710–715. doi: 10.1097/00007632-199403001-00011. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardt M, Swartz D, Clothiaux P, Crowell R, White A. Posterolateral lumbar and lumbosacral fusion with or without pedicle screw fixation. Clin Orthop. 1992;284:109–114. [PubMed] [Google Scholar]
- 3.Boxall D, Bradford DS, Winter RB, et al. Management of severe spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1979;61:479–495. [PubMed] [Google Scholar]
- 4.Carson WL, Duffield RC, Arendt M, Ridgely BJ, Gaines RW. Internal forces and moments in transpedicular spine instrumentation: the effect of pedicle screw angle and transfixation-the 4R–4Bar linkage concept. Spine. 1990;15:893–901. doi: 10.1097/00007632-199009000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Christensen FB, Laursen M, Gelineck J, Eiskjaer SP, Thomasen K, Bunger CE. Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detalied classification system in posterolateral spinal fusion. Spine. 2001;1:538–543. doi: 10.1097/00007632-200103010-00018. [DOI] [PubMed] [Google Scholar]
- 6.Duval-Beupère G, Boisaubert J, Hequet J, et al. Sagittal profile of normal spine changes in spondylolisthesis. In: Harms J, Sturs H, et al., editors. Severe spondylolisthesis. Darmstadt: Springer; 2002. pp. 21–32. [Google Scholar]
- 7.Esses SI, Sachs BI, Drezyn V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS member. Spine. 1993;18:2231–2239. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Fairbank JCT, Pynsent PB. The Oswestry disability index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 9.Grob D, Humke T, Dvorak J. Direct pediculo-body fixation in cases of spondylolisthesis with advanced intervertebral disc degeneration. Eur Spine J. 1996;5:281–285. doi: 10.1007/BF00301335. [DOI] [PubMed] [Google Scholar]
- 10.Jackson RP, Phipps T, Hales C, et al. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28:151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Krag MH. Biomechanics of thoracolumbar spinal fixation. Spine. 1991;16:S84–S99. doi: 10.1097/00007632-199103001-00014. [DOI] [PubMed] [Google Scholar]
- 12.Marchetti PG, Bartolozzi P (1986) Spondylolisthesis-classification and etiopathogenesis. Progress in spinal pathology: spondylolisthesis II. Italian Scoliosis Research Group, Bologna