Abstract
The aim of this study is to review our experience with the transoral surgical management of anterior craniovertebral junction (CVJ) lesions with particular attention to the decision making and to the indication for a consecutive stabilization. During 10 years (1998–2007), 52 consecutive patients presenting exclusively fixed anterior compression at the cervicomedullary junction underwent transoral surgery. Mean age was 55.85 years (range 17–75 years). Encountered lesions were: malformation (32 cases), rheumatoid arthritis (11 cases), tumor (5 cases) or trauma (4 cases). A total of 79% of patients presented with chronic/recurrent headache (cranial and/or high-cervical pain), 73% with varying degrees of quadrip aresis, and 29% with lower cranial nerve deficits. All of the patients but two, with posterior stabilization performed elsewhere, underwent synchronous anterior decompression and posterior occipitocervical fixation. Adjuncts to the transoral approach (Le Fort I with or without splitting of the palate), tailored to the local anatomy and to the extension of the lesions, were performed in seven cases. Follow-up ranged between 4 and 96 months. Of 35 patients with severe preoperative neurological deficits, 33 improved. The remaining 15 patients who presented with mild symptoms, healed throughout the follow-up. Perioperative mortality occurred in two cases and surgical morbidity in eight cases (dural laceration, cerebrospinal fluid leak with meningitis, malocclusion, oral wound dehiscence and occipital wound infection). Delayed instability occurred in one patient because of cranial settling of C2 vertebral body. A successful surgery achieving a stable decompression at the CVJ is an expertise demanding procedure. It requires accurate preoperative evaluation and, appropriate choice of decompression technique and stabilization instruments. Enlarged transoral approaches (despite higher morbidity) are a supportive means in cases of severe basilar invagination, cranial extension of the lesion or limited jaw mobility.
Keywords: Craniocervical junction, Transoral odontoidectomy, Maxillotomy, Occipitocervical fusion
Introduction
Anterior compression at the craniovertebral junction (CVJ) can occur in many types of pathology: malformation (basilar invagination, atlas assimilation, os odontoideum, atlantoaxial fixed dislocation), tumor, trauma, chronic inflammatory diseases (most frequently rheumatoid arthritis), osteomyelitis [9–13, 27]. In all these cases, transoral approaches (TOAs) consent to reach directly the site of the lesion and thus decompress the cervicomedullary junction staying away from laterally placed neurovascular structures [4, 15, 26, 27, 29]. By reporting surgical results and complications of this 52 treated patient series, the aim of this study is to revise the technical strategies, to identify the conditions requiring additional maxillotomies and to evaluate the necessity and the timing of postoperative stabilization.
Materials and methods
All patients with anterior lesions compressing the cervicomedullary tract who underwent transoral surgery during 10 years (1998–2007) were included in this study. Radiographic imaging, previous and postoperative evaluations as well as outpatient archives were retrospectively checked. Thirty-two patients presented CVJ malformation (odontoid basilar invagination, atlas assimilation, atlanto-axial dislocation), 11 presented rheumatoid arthritis, 5 lesions were tumoral and 4 were trauma victims. The mean age at the time of treatment was 55.85 years (range 17–75 years); 28 females and 24 males were included in this study.
In one case, previous transoral decompression and occipitocervical stabilization, in one other case posterior stabilization alone and in two cases laminectomy were performed in other hospitals.
Local pain referred as cervical and/or cranial pain was present in 40 patients. Manifest quadriparesis of different grade was detected in 37 cases (motor/sensory). Cerebellovestibular signs were detected in nine patients. The lower cranial nerves were affected in 15 patients. Pathognomic physical marks such as short neck, low hairline and facial asymmetry were observed in 18 cases of CVJ malformation. Duration of symptoms at admission was 6 months to 4 years.
Atlantoaxial mobility was checked by means of dynamic X-ray (atlantodental interval, clivodental interval, spinal canal diameter) in cases of CVJ malformation. MRI and 3D-CT scan were used to detect the site of compression, the extension of the lesion (in case of tumor or rheumatoid pannus, gadolinium contrast was used), to determine the position of the vertebral artery (in order to prepare the posterior stabilization). The indications for surgery were: tumor, compressing pannus, irreducible compression (fracture, malformation), tip of the odontoid process at least 2.5 mm above the Chamberlain’s line.
Standard transoral approach was used in 45 patients, Le Fort I osteotomy was required in 5 patients (platybasia, odontoid tip more than 20 mm above Chamberlain’s line) and two cases required palate split. All patients but two with posterior stabilization performed elsewhere underwent posterior fixation consecutively in the same sitting.
Operative tips
The duration of consecutively performed transoral decompression and posterior stabilization was 5–8 h. We routinely employ a hot air blanket for temperature regulation and pneumatic foot compression to prevent deep venous thrombosis. Tracheostomy, used in the first 12 cases, has been abandoned (except 7 cases in which maxillotomy was performed) and fiberoptic nasotracheal intubation is preferred [17]. Intravenous prophylactic antibiotics is given in all cases. Patient is put in mild Trendelemburg position with the head stabilized in a Mayfield holder. The retraction of the soft palate is performed by means of two rubber catheters sutured to the soft palate, through the nostrils, and fixed cranially to the Mayfield holder.
During decompression, when C1 is not interested, the anterior arch is spared by using a bottom-up dens-drilling technique (by drilling the base of the dens until it is possible to clasp the tip with a rongeur and to remove the apical ligaments). In all cases, tumor, pannus or even CVJ malformation, the cruciate ligament was cut and the dura mater was exposed. Antibiotic wax is always placed in the operative cavity right before mucosa and pharyngeal muscles are sutured in single layer [5, 23, 24, 26].
Subsequently, the patient is turned prone. To achieve occipitocervical stabilization, interlaminar hooks and occipital screws were used in the first 20 cases. More recently, we use a system with a precontoured plate fixed to the occiput with bicortical screws and independent rods fixed by screws to the lateral masses of the subaxial cervical spine. Autologous bone harvested from the local spinous processes and/or from the iliac crest are used for fusion. For an operative facilitation, the stabilization system is applied in a head flexed position without blocking the connectors. In fact, these are blocked only after having re-extended the head to regain a position most proximal to a preoperative X-ray performed in a standing position.
Postoperatively all patients are transitorily transferred to an intensive care unit. Cold fluid is allowed starting from the third postoperative day. CT scans are usually performed 3–7 days after surgery and in the same period of time, patients start mobilization (Fig. 1). An MRI is always performed within 1 month from surgery. 3-, 6- and 12-month outpatient checks are performed by X-ray and neurological examinations. Additional CT scans are also performed at the last check. Successively, patients are yearly checked through outpatient visits. Decompression status (including tumor control), fusion, stability in addition to neurological status are always detected.
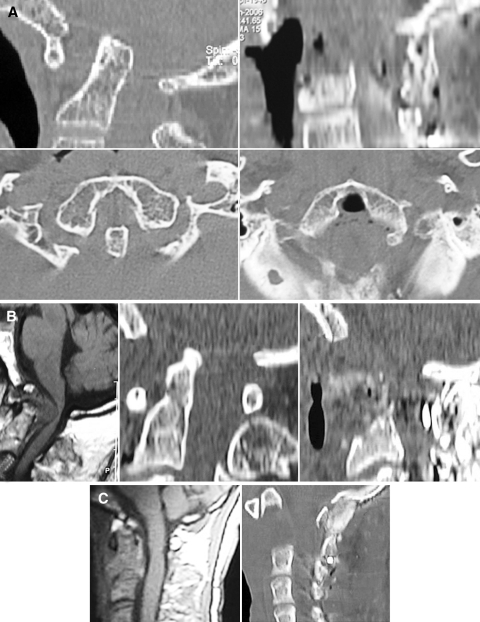
Fig. 1.
Three types of cases requiring a transoral surgical decompressive approach and synchronus posterior fusion. a Preoperative (left) sagittal (up) and axial (down) reformatted CT scans illustrating a basilar invagination associated to atlantoaxial dislocation and atlas assimilation with postoperative results (right) in sagittal (up) and axial (down) reformatted CT scans. b Sagittal T1-weighted MRI (left) and sagittal CT scans (middle) presenting a case of rheumatoid arthritis with abundant pannus behind the dens compressing and deviating the cerviomedullary junction with surgical results illustrated by a postoperative sagittal CT scan. c A preoperative T1-weighted MRI (left) and postoperative sagittal CT scan (right) of a giant cell tumor of axis that was totally removed
Results
Mortality directly correlated to surgery did not occur; however, pulmonary embolism in two cases of severe spastic quadriplegia conducted to death within 20 days (Table 1).
Table 1.
A short review of the presented series including presentation, surgery and follow-up
| Age, sex | Lesion | Previous surgery | Approach | Complications | Revision | Mean preop symptoms | Neurological results | Follow-up (months) | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 62, M | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 90 |
| 2 | 65, F | RA | No | TO | – | No | Headache, low nerves | = | 96 |
| 3 | 17, M | TUM | No | TO | Urinary infection | No | Headache | = | 72 |
| 4 | 67, F | Malf | No | TO | Dural laceration, urinary infection | No | Headache, quadriparesis | ↑ | 86 |
| 5 | 56, F | Malf | Posterior decompression | TO | – | No | Headache, quadriparesis, low nerves | = | 89 |
| 6 | 63, F | Malf | No | TO | Pulmonary embolism | No | Headache, quadriparesis | – | Death 7 days |
| 7 | 61,M | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 88 |
| 8 | 53, F | Malf | TO + Posterior fusion | TO | – | No | quadriparesis | ↑ | 85 |
| 9 | 56, M | Malf | No | TO | Oral wound dehiscence | Oral wound revision | quadriparesis, low nerves | = | 72 |
| 10 | 54, M | Malf, KF | No | TO | – | No | Headache, quadriparesis | ↑ | 70 |
| 11 | 45, F | TUM | No | TO | DVT | No | Headache, quadriparesis | ↑ | 73 |
| 12 | 50, M | Malf | No | TO | Pseudoarthrosis | TO revision for cranial settling | Headache, quadriparesis | ↑ | 66 |
| 13 | 26, M | TR | No | TO | – | No | – | = | 12 |
| 14 | 69, F | Malf | No | ODM | Velopharyngeal dysfunction, DVT | No | Headache, quadriparesis | ↑ | 52 |
| 15 | 58, M | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 48 |
| 16 | 37, M | Malf | No | TO | – | No | Headache, quadriparesis, low nerves | ↑ | 45 |
| 17 | 65, F | TUM | No | TO | Pulmonary embolism | No | Headache | – | Death 15 days |
| 18 | 59, F | Malf | No | TO | DVT | No | Quadriparesis | ↑ | 42 |
| 19 | 32, M | Malf | No | TO | – | No | Headache | = | 37 |
| 20 | 72, F | RA | No | LFO | Malocclusion | No | Headache, quadriparesis, low nerves | ↑ | 44 |
| 21 | 70, M | TR | No | TO | CSF fistula, meningitis | No | Headache | = | 12 |
| 22 | 66, F | RA | No | TO | – | No | Headache | = | 26 |
| 23 | 75, M | Malf | No | ODM | Pressure sore | No | Headache, quadriparesis, low nerves | ↑ | 24 |
| 24 | 50, M | TUM | No | TO | DVT | No | Headache, quadriparesis | ↑ | 36 |
| 25 | 64, F | Malf, KF | No | TO | – | No | Headache, quadriparesis | = | 18 |
| 26 | 66, F | Malf | No | TO | – | No | Headache, quadriparesis, low nerves | ↑ | 17 |
| 27 | 47, F | Malf, KF | No | TO | – | TO revision | Quadriparesis, low nerves | ↑ | 14 |
| 28 | 62, F | RA | No | LFO | – | No | Headache | = | 15 |
| 29 | 50, F | Malf | No | TO | – | No | Headache, quadriparesis, low nerves | ↑ | 13 |
| 30 | 74, F | Malf | No | TO | DVT | No | Headache, quadriparesis | ↑ | Death 20 months |
| 31 | 67, F | RA | No | TO | – | No | quadriparesis | ↑ | 13 |
| 32 | 42, F | Malf | No | TO | – | No | Headache | = | 12 |
| 33 | 67, M | TR | No | TO | Pressure sore | No | Headache | = | 11 |
| 34 | 64, F | Malf | Posterior decompression | TO | Urinary infection | No | Headache, quadriparesis, low nerves | ↑ | 6 |
| 35 | 18, M | RA | No | TO | – | No | Headache | = | 7 |
| 36 | 57, M | TR | No | TO | – | No | quadriparesis | ↑ | 5 |
| 37 | 56, F | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 6 |
| 38 | 57, F | RA | No | TO | – | No | Headache | = | Death 8 months |
| 39 | 66, M | Malf | No | LFO | Screw lose | No | Headache, quadriparesis, low nerves | ↑ | 7 |
| 40 | 75, F | RA | No | TO | DVT | No | Quadriparesis, low nerves | ↑ | 6 |
| 41 | 23, M | Malf, DS | No | TO | – | No | Headache | = | 6 |
| 42 | 68, F | RA | No | TO | Vertebral artery perforation | No | Headache, low nerves | ↑ | 4 |
| 43 | 62, F | Malf | No | TO | – | To revision | Headache, quadriparesis | ↑ | 5 |
| 44 | 67, M | RA | No | LFO | – | No | Quadriparesis, low nerves | = | 4 |
| 45 | 44, M | TUM | No | TO | Urinary infection | No | Quadriparesis | ↑ | 6 |
| 46 | 66, M | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 5 |
| 47 | 46, F | Malf, KF | No | LFO | – | No | quadriparesis | ↑ | 6 |
| 48 | 18, M | Malf, DS | No | TO | – | No | Headache, | = | 6 |
| 49 | 52, F | RA | No | TO | – | No | Headache, quadriparesis | ↑ | 5 |
| 50 | 71, M | Malf | Posterior fusion | TO | – | No | Headache, low nerves | ↑ | 5 |
| 51 | 68, M | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 4 |
| 52 | 59, F | Malf | No | TO | – | No | Headache, quadriparesis | ↑ | 4 |
52 patients with craniovertebral junction lesions surgically treated by a transoral approach
Malf craniovertebral malformation (atlantoaxial dislocation, basilar invagination, Atlas assimilation), KF Klippel-Feil anomaly, DS down syndrome,DVT deep venous thrombosis, LFO Le Fort I osteotomy, ODM open-door maxillotomy; preop preoperative, postop postoperative, TO transoral, ↑ improved, = stable, M male, F female
Complications directly related to surgery were vertebral artery perforation in one case, dural tear in one case, superficial occipital wound infection in two cases, CSF fistula in one case which leads to meningitis, malocclusion in one case of Le Fort maxillotomy, posterior pharyngeal wall dehiscence in one patient, articular screw lose due to malpositioning in one case of CVJ malformation associated with severe scoliosis.
Other systemic complications occurred: six deep vein thrombosis, four urinary infection, one chest infection and one pressure sore.
The mean duration of follow-up after surgery was 31 months (≈2.5 years) and ranged from 4 to 96 months. On postoperative neuroradiological checks, decompression was considered satisfactory in all cases but two who needed a transoral revision. Fusion was considered proper in all surviving cases. Two patients who had postoperatively presented stable conditions in one case and initial improvement in the other, died at, respectively, 8 and 20 months from surgery due to causes unrelated with surgery. None of the patients deteriorated at follow-up. Neurological conditions in 33 of the 35 surviving patients with different level of quadriparesis improved. One case of adjunctive maxillotomy presented postoperative velopharyngeal dysfunction and needed pharyngoplasty. Postoperatively, swallowing function improved in seven patients and did not change in one.
Discussion
Transoral decompression
Posterior approaches at the CVJ have been successful for posterior fusion and thus play a role only in cases of reducible compression [9–11, 20–22, 27, 30]. Nevertheless, progressive understanding of the craniocervical dynamics and innovative techniques to determine the site of encroachment, lead to conclusion that the transoral approach, with addition of the proper type of stabilization, is the gold standard in the treatment of pathologies causing irreducible anterior compression of the cervicomedullary segment [6, 7, 20–22]. Also lateral approaches are practicable but they require an extensive dissection, risk of injury of the vertebral artery, of the jugular bulb, and of the hypoglossal nerve and we prefer to reserve them to massive tumor masses involving lateral structures [1, 27, 30, 31].
Over time, our surgical treatment philosophy evolved and we adopted several technical variations for transoral operations. In fact, we have started using a prophylactic broad-spectrum antibiotic therapy to all patients instead of basing our antibiotic coverage on preoperative pharyngeal flora, as advocated by some authors. Preoperative tracheostomy has been abandoned except for cases of transoral extended maxillotomy approach [17, 32]. Le Fort I maxillotomy, permitting sufficient rostral exposition of the clivus and the tip of invaginated dens as in severe basilar invagination or in voluminous tumor masses, has surrogated soft palate incision [2, 4, 12, 27, 28]. By this way, complications related to soft palate wound dehiscence are avoided [4, 13]. Careful neuroimaging preoperative study of the pathologic anatomy of this area is crucial to select the appropriate approach and to avoid catastrophic complications [13]. Other approaches that can assist the transoral approach include the open-door maxillotomy approach, the transoral–translabiomandibular approach, the transoral bilateral sagittal split mandibular osteotomy approach and the mandibular swing-transcervical approach [6, 7, 17, 32].
In patients with limited jaw mobility we favor use of the open-door maxillotomy approach [3, 7, 14, 17]. The open-door maxillotomy approach should be restricted to the needs of the individual patients because of its inherent morbidity including potential dental malocclusion, velopharyngeal dysfunction and palatal fistulas [3, 17–19].
Instability after transoral approaches
No diagnostic means are available to correlate the transoral odontoidectomy extension with the CVJ instability [8]. Nonetheless, most authors advocate posterior fusion following transoral decompression [8]. Significantly, we reported one postoperative death from acute dislocation of the axis on the day before a planned posterior fixation in a previous report of 25 CVJ malformations treated by TOA [10]. In order to eliminate the risk of acute postoperative instability and to early mobilize the patients we have moved from performing a planned posterior fixation as a second procedure to a one-stage transoral decompression and occipitocervical fixation. Based on biomechanical studies, the integrity of C1-ring and lateral masses minimizes the risk of cranial settling [8, 23, 24]. In this series, one patient experienced symptomatic cranial settling of C2 vertebral body after one-stage transoral decompression despite occipitocervical fixation and required a second anterior decompression. In our subsequent patients, in order to conserve the ring of C1 anteriorly, we used the bottom-up C1 sparing drilling technique. More recently, we have been using precontoured plate rod systems with screws in the occipital bone, C2 pedicles and lateral masses of the cervical spine which, accordingly to recent biomechanical studies, has resulted in major stability and resistance to cranial settling [16, 25].
Conclusions
One-stage transoral decompression and posterior occipitocervical fixation are feasible and effective in patients with CVJ anterior fixed compression, including malformation, tumor, trauma, inflammatory diseases. The transoral approaches must be tailored to a particular patient’s pathological findings with a thorough understanding of the malformed anatomy of the CVJ. Severe basilar invagination, cranially extended lesions or cases of limited mandibular excursion may require a transmaxillay approach. Successful transoral decompression of complex CVJ malformations remains a major neurosurgical challenge and requires an adequate learning curve.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Al-Mefty O, Borba LA, Aoki N, Angtuaco E, Pait G. The transcondylar approach to extradural nonneoplastic lesions of the craniovertebral junction. J Neurosurg. 1996;84:1–6. doi: 10.3171/jns.1996.84.1.0001. [DOI] [PubMed] [Google Scholar]
- 2.Ammirati M, Bernardo A. Analytical evaluation of complex anterior approaches to the cranial base: an anatomic study. Neurosurgery. 1998;43:1398–1407. doi: 10.1097/00006123-199812000-00081. [DOI] [PubMed] [Google Scholar]
- 3.Anand VK, Harkey HL, Al-Mefty O. Open-door maxillotomy approach for lesions of the clivus. Skull Base Surg. 1991;1:217–225. doi: 10.1055/s-2008-1057101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balasingam V, Anderson GJ, Gross ND, Cheng CM, Noguchi A, Dogan A, McMenomey SO, Delashaw JB, Andersen PE. Anatomical analysis of transoral surgical approaches to the clivus. J Neurosurg. 2006;105:301–308. doi: 10.3171/jns.2006.105.2.301. [DOI] [PubMed] [Google Scholar]
- 5.Cantore GP, Guidetti B, Moscatelli G (1969) A new antibiotic “mastic” in neurosurgery. Fourth International Congress of Neurological Surgery, New York, New York, September 20–27. Exerpta Medica International Congress Series, no. 193, p 46
- 6.Crockard HA, Calder I, Ransford AO. One-stage transoral decompression and posterior fixation in rheumatoid atlanto-axial subluxation. J Bone Joint Surg Br. 1990;72:682–685. doi: 10.1302/0301-620X.72B4.2380227. [DOI] [PubMed] [Google Scholar]
- 7.Crockard HA. Transoral surgery some lessons learned. Br J Neurosurg. 1995;9:283–293. doi: 10.1080/02688699550041304. [DOI] [PubMed] [Google Scholar]
- 8.Dickman CA, Locantro J, Fessler RG. The influence of odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992;77:525–530. doi: 10.3171/jns.1992.77.4.0525. [DOI] [PubMed] [Google Scholar]
- 9.Di Lorenzo N, Fortuna A, Guidetti B. Craniovertebral junction malformations. Clinicoradiological findings, long-term results and surgical indications in 63 cases. J Neurosurg. 1982;57:603–608. doi: 10.3171/jns.1982.57.5.0603. [DOI] [PubMed] [Google Scholar]
- 10.Di Lorenzo N. Transoral approach to extradural lesions of the lower clivus and upper cervical spine: an experience of 19 cases. Neurosurgery. 1989;24:37–42. doi: 10.1097/00006123-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Di Lorenzo N. Craniocervical junction malformation treated by transoral approach. A survey of 25 cases with emphasis on postoperative instability and outcome. Acta Neurochir (Wien) 1992;118(11):2–116. doi: 10.1007/BF01401296. [DOI] [PubMed] [Google Scholar]
- 12.Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88:962–968. doi: 10.3171/jns.1998.88.6.0962. [DOI] [PubMed] [Google Scholar]
- 13.Hadley MN, Spetzler RF, Sonntag VKH. The transoral approach to the superior cervical spine. A review of 53 cases of extradural cervicomedullary compression. J Neurosurg. 1989;71:16–23. doi: 10.3171/jns.1989.71.1.0016. [DOI] [PubMed] [Google Scholar]
- 14.Harkey HL, Crockard HA, Stevens JM, Smith R, Ransford AO. The operative management of basilar impression in osteogenesis imperfecta. Neurosurgery. 1990;27:782–786. doi: 10.1097/00006123-199011000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Harris JP, Godin MS, Krekorian TD, Alksne JF. The transoropalatal approach to the atlanto-clival region: considerations of the head and neck surgeon. Laryngoscope. 1989;99:467–474. doi: 10.1288/00005537-198905000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Hurlbert RJ, Crawford NR, Choi WG, Dickman CA. A biomechanical evaluation of occipitocervical instrumentation: screw compared with wire fixation. J Neurosurg. 1999;90(1 Suppl):84–90. doi: 10.3171/spi.1999.90.1.0084. [DOI] [PubMed] [Google Scholar]
- 17.James D, Crockard HA. Surgical access to the base of skull and upper cervical spine by extended maxillotomy. Neurosurgery. 1991;29:411–416. doi: 10.1097/00006123-199109000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Jones DC, Hayter JP, Vaughan ED, Findlay GF. Oropharyngeal morbidity following transoral approaches to the upper cervical spine. Int J Oral Maxillofac Surg. 1998;27:295–298. doi: 10.1016/S0901-5027(05)80618-6. [DOI] [PubMed] [Google Scholar]
- 19.Kingdom TT, Nockels RP, Kaplan MJ. Transoral-transpharyngeal approach to the craniocervical junction. Otolaryngol Head Neck Surg. 1995;113:393–400. doi: 10.1016/S0194-5998(95)70074-9. [DOI] [PubMed] [Google Scholar]
- 20.Menezes AH, VanGilder JC, Graf CJ, McDonnell DE. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980;53:444–455. doi: 10.3171/jns.1980.53.4.0444. [DOI] [PubMed] [Google Scholar]
- 21.Menezes AH, VanGilder JC. Transoral–transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988;69:895–903. doi: 10.3171/jns.1988.69.6.0895. [DOI] [PubMed] [Google Scholar]
- 22.Menezes AH, Traynelis VC, Gantz BJ. Surgical approaches to the craniovertebral junction. Clin Neurosurg. 1994;41:187–203. [PubMed] [Google Scholar]
- 23.Naderi S, Crawford NR, Melton MS, Sonntag VK, Dickman CA (1999) Biomechanical analysis of cranial settling after transoral odontoidectomy. Neurosurg Focus 6(6) Article 7 [DOI] [PubMed]
- 24.Naderi S, Pamir N. Further cranial settling of the upper cervical spine following odontoidectomy. Report of two cases. J Neurosurg (Spine) 2001;95:246–249. doi: 10.3171/spi.2001.95.2.0246. [DOI] [PubMed] [Google Scholar]
- 25.Oda I, Abumi K, Sell LC, Haggerty CJ, Cunningham BW, McAfee PC. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine. 1999;15:2377–2382. doi: 10.1097/00007632-199911150-00015. [DOI] [PubMed] [Google Scholar]
- 26.Pásztor E, Vajda J, Piffkó P, Horváth M, Gádor I. Transoral surgery for craniocervical space-occupying processes. J Neurosurg. 1984;60:276–281. doi: 10.3171/jns.1984.60.2.0276. [DOI] [PubMed] [Google Scholar]
- 27.Perrini P, Benedetto N, Di Lorenzo N (2008) The transoral approaches to the craniovertebral junction malformations: surgical strategies and results in a series of 34 consecutive patients. Neurosurgery (accepted) [DOI] [PubMed]
- 28.Sasaki CT, Lowlicht RA, Tokashiki R. Horizontal maxillotomy for exposure of the central skull base: the Yale experience. J Neurooncol. 2001;55:173–177. doi: 10.1023/A:1013877728476. [DOI] [PubMed] [Google Scholar]
- 29.Spetzler RF, Dickman CA, Sonntag VKH. The transoral approach to the anterior cervical spine. Contemp Neurosurg. 1991;13:1–6. [Google Scholar]
- 30.Stevenson GC, Stoney RJ, Perkins RK, Adams JE. A transcervical transclival approach to the ventral surface of the brain stem for removal of a clivus cordoma. J Neurosurg. 1966;24:544–551. doi: 10.3171/jns.1966.24.2.0544. [DOI] [PubMed] [Google Scholar]
- 31.Türe U, Pamir N. Extreme lateral-transatlas approach for resection of the dens of the axis. J Neurosurg (Spine 1) 2002;96:73–82. doi: 10.3171/spi.2002.96.1.0073. [DOI] [PubMed] [Google Scholar]
- 32.Vishteh AG, Beals SP, Joganic EF, Reiff JL, Dickman CA, Sonntag VKH, Spetzler RF. Bilateral sagittal split mandibular osteotomies as adjunct to the transoral approach to the anterior craniovertebral junction. Technical note. J Neurosurg (Spine 2) 1999;90:267–270. doi: 10.3171/spi.1999.90.2.0267. [DOI] [PubMed] [Google Scholar]