Abstract
We studied 51 patients with 64 fractures of the thoracolumbar and lumbar spine undergoing the surgical treatment by percutaneous trans-pedicular fixation and stabilization with minimally invasive technique. Patient follow-up ranged from 6 to 28 months (mean 14.2 months) and the patients were assessed by clinical and radiographic evaluation. The results show that percutaneous trans-pedicular fixation and stabilization with minimally invasive technique is an adequate and satisfactory procedure to be used in specific type of the thoracolumbar and lumbar spine fractures.
Keywords: Mini-invasive, Fracture, Spine, Percutaneous
Introduction
Surgical treatment of thoracic and lumbar spine fractures depends on various factors. Pathological features of the vertebral lesion, neurological deficit, general condition of health and the presence or absence of polytrauma affects the treatment and the final result.
Although type B and C fractures following AO-Magerl classification [1] require surgical treatment, most type A fractures without neurological involvement can be safely treated in a conservative way [2, 3].
Conservative treatment is a highly demanding procedure for the patient and the risk of a consequent deformity (vertebral body wedging and subsequent kyphosis) has to be considered. Thoracolumbar or lumbar kyphosis can consistently worsen the quality of life of the patient. Moreover, some situations rule out the chance for a conservative treatment. In case of polytrauma, claustrophobia, psychological disease, venous disease or previous deep venous thrombosis, obesity, bronchopulmonary diseases conservative treatment is not advisable. Attention must also be paid to the fact that younger and active workers refuse the conservative treatment in order to avoid bed rest and an inactive period.
A traditional open surgery may be an overtreatment in all these cases, considering blood loss, possible complications, hospital stay and delayed functional recovery. In this setting, a good option can be a percutaneous minimally invasive surgery [4, 5]. This technique is suggested by the authors every time a conservative treatment is not indicated or advisable and posterior open arthrodesis may represent an overtreatment.
Materials and methods
Fifty-one patient affected by 64 thoracolumbar and lumbar spine fractures have been treated with percutaneous trans-pedicular fixation and stabilization with minimally invasive technique since May 2005 until April 2008. Seventeen patients were females, 34 males; average age was 45 years (range from 21 to 82). The causes of the fractures were motor vehicle in 34 patients (66%) and fall from height in 17 (34%). A total of 11 (21%) were polytrauma patients. Every fracture has been classified following AO-Magerl classification [1]: 57 type A fractures (89%), 4 type B fractures, 3 type C fractures (Table 1). The lesion was localised in thoracic spine (T1–T10) in 6 patients (11%), thoracolumbar spine (T11–L1) in 31 patients (60.7%) and lumbar spine in 14 patients (33.4%). The most involved vertebrae have been the L1 (20 cases, 39%) and the T12 (14 cases, 27%). All the patients have been followed up with clinical and radiological data for 14.2 months on an average (minimum 6 months, maximum 28 months). Surgery time has been calculated in 120 min on average (range from 60 to 240 min). Various instrumentations have been tested: Xia Precision (Stryker) in 4 patients, Viper (DePuy) in 2 patients, Sextant (Medtronic) in 24 patients (Fig. 1), CD Horizon Longitude (Medtronic) in 18 patients (Fig. 2). Nine patients (17%) were performed percutaneous trans-pedicular body augmentation with cement. During the post-operative period, patients did not use external immobilization and there no limitation on walking or rehabilitation, which was performed according to the general condition of the patients and their pain response.
Table 1.
Fractures type following AO classification (adapted from [1])
| A1 | 20 |
| A2 | 10 |
| A3 | 27 |
| B1 | 1 |
| B2 | 3 |
| C1 | 1 |
| C2 | 2 |
Fig. 1.
a A 50-year-old patient with a diagnosis of L3 fracture, type A2 following Magerl classification, no neurological deficit. b Pre-operative CT scan. c Ten months after percutaneous trans-pedicular fixation and stabilization with minimally invasive technique, Sextant instrumentation (Medtronic). d Implant removal, 18 months FU. e Clinical result
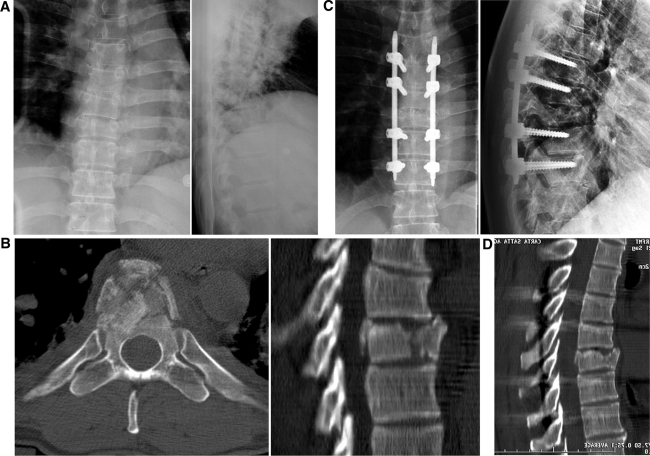
Fig. 2.
a A 32-year-old patient affected by a type A2 fracture involving the T8 vertebral body as a consequence of a car crash. b Pre-operative CT scan. c Eight months after percutaneous trans-pedicular fixation and stabilization with minimally invasive technique, CD Horizon Longitude instrumentation (Medtronic). d Post-operative CT scan
Results
All the cases have been considered healed after a 6 months control. Radiological examinations confirmed good spontaneous reconstruction of the anterior and posterior column. Radiographic evaluation was performed through the measurement of the segmental kyphosis and the wedging deformity of the involved vertebral body [6]. Back pain, evaluated by V.A.S. scale was 1.9 points at FU. Clinical evaluation was performed by subjective evaluation of the final results by patients themselves and every patient was satisfied of surgical procedure. Sixty-three fractures out of 64 reached consolidation. Radiographic evaluation showed a real improvement in the post-operative period (segmental kyphosis 4.2° pre-op, −2.2° post-op, 2.7° F.U. and kyphosis of the fractured vertebral segment 12° pre-op, 5.9° post-op, 8.7° F.U.), but also a worsening of the segmentary kyphosis in the cases treated with CD Horizon Longitude (6.4° pre-op, 3.5° post-op, 7.8° F.U) if implanted with multiaxial screws. (5.7° pre-op, 4.8° post-op, 9.9° F.U.) (Table 2). Some complications occurred. A screw has been positioned in a parapedicular position, falling into the spine canal, without any symptomatologic consequences (Fig. 3). One case (1.9%) developed an infection that requested the remotion of the instrumentation. Two times the instrumented construct showed mechanical failure (3.9%). One fracture did not heal and an anterior arthrodesis through minimally invasive technique has been needed. The instrumentation has been removed in ten patients (19%).
Table 2.
Results of the radiographic evaluation of the segmental kyphosis and the wedging deformity of the involved vertebral body
| Segmental kyphosis | Wedging deformity | |||||
|---|---|---|---|---|---|---|
| Pre-op | Post-op | F.U. | Pre-op | Post-op | F.U. | |
| Sextant + C D longitude | 4.1° | −2.2° | 2.7° | 12.2° | 5.9° | 8.7° |
| Sextant | 3.2° | −4.8° | 0.3° | 11.8° | 4.5° | 8.2° |
| C D longitude | 6.4° | 3.5° | 7.8° | 13.3° | 8.8° | 10° |
| Multiaxial screws | 5.7° | 4.8° | 9.9° | 14.3° | 9.3° | 10.3° |
| Monoaxial screws | 7.5° | 1° | 3.8° | 11.5° | 8° | 9.5° |
Bold value indicates worsening outcome
Fig. 3.
Screw positioned too medial, without pain or neurological problems
Conclusions
The rationale for applying minimally invasive technique in the management of the spine fractures is to reduce the approach-related morbidity associated with the conventional technique (iatrogenic muscle denervation, increased intramuscular pressures, ischaemia, pain and functional impairment) [4, 7] in case of the polytrauma, claustrophobia, psychological disease, venous disease or previous deep venous thrombosis, obesity, bronchopulmonary disease when conservative treatment is not advisable.
Because of the impossibility to perform a fusion, the minimally invasive percutaneous stabilization has been limited to relatively stable vertebral fractures, involving mainly bone component with a high power of spontaneous healing after immobilization; the screws and rods implanted have acted as an internal fixator, which has led to the biological healing of all fractures treated. Wang et al. comparing two groups of patients with thoracolumbar burst fractures, one treated by instrumented fusion, while the other just fixed without fusion, showed that there were no statistically significant differences in the long term between the two groups with a slight advantage, both for clinical than for radiographic parameters, for the group treated only with fixation without fusion [8]. This study further justifies the minimally invasive approach we have taken.
The loss of correction, we observed during the follow-up for the cases treated with multiaxial screws could be explained by the possibility of this type of screws to have slight movement, also after implantation, between the head and the arm of the screw. For this reason, monoaxial screws should be considered for this kind of surgery, when it is possible.
Minimally invasive percutaneous fixation in the treatment of thoracolumbar and lumbar spine fractures represents a good alternative option to conservative treatment. Clinical and functional results are better or comparable, time of recovery is much quicker and the rate of complications is low. Implants need to be removed in case of complications or symptoms referred by the patient. Otherwise system hardware removal is mandatory only when fixation involves L2 or lower segments (Fig. 1).
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1984;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 2.Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of non-operative management. Spine. 1993;18(8):955–970. doi: 10.1097/00007632-199306150-00003. [DOI] [PubMed] [Google Scholar]
- 3.Shen WJ, Shen YS. Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurologic deficit. Spine. 1999;24(4):412–415. doi: 10.1097/00007632-199902150-00024. [DOI] [PubMed] [Google Scholar]
- 4.Rampesaud YR, Annand N, Dekutoski MB. Use of minimally invasive surgical technique in the management of thoracolumbar trauma. Spine. 2006;31(11 Suppl):S96–S102. doi: 10.1097/01.brs.0000218250.51148.5b. [DOI] [PubMed] [Google Scholar]
- 5.Barbanti Brodano G, Iure F, Cappuccio M, Palmisani M, Boriani L, Gasbarrini A, Bandiera S, Scimeca GB, Boriani S. Osteosintesi con tecnica percutanea mininvasiva nel trattamento delle fratture vertebrali toraciche e lombari. Esperienza preliminare. GIOT. 2007;33:78–85. [Google Scholar]
- 6.Kuklo TR, Polly DW, Jr, Owens BD, Zeidman SM, Chang AS, Kiemme WR. Measurement of thoracic and lumbar fracture kyphosis. Spine. 2001;26(1):62–66. doi: 10.1097/00007632-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 7.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: Part 2. Histological and histochemical analyses in humans. Spine. 1994;19:2598–2602. doi: 10.1097/00007632-199411001-00018. [DOI] [PubMed] [Google Scholar]
- 8.Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine. 2006;31(23):2646–2652. doi: 10.1097/01.brs.0000244555.28310.40. [DOI] [PubMed] [Google Scholar]