Abstract
Intradural spinal arachnoid cysts with cord compression are rare. When becoming symptomatic they cause variable symptoms involving gait disturbance, paraparesis or tetraparesis and neuropathic pain, decreasing significantly the patients’ life quality. The extension of such cysts averages 3.7 vertebral bodies. The diagnosis is clinical and radiological with the use of MRI, CT myelography or a combination of both. The best treatment option is complete removal of the cyst. However, even when paresis is regressing there is no good recovery from neuropathic pain. Laminectomy approach can cause postoperative complications especially when the cyst(s) expand(s) in more than one level. Alternatively, a cyst fenestration can be performed, including the levels of the maximal spinal cord compression. The clinical outcome is as good as after the cyst resection enabling the patient to walk again. The neuropathic pain may persist and require medication. A clinical case is presented, and the literature is reviewed. In the present case we report a patient with intradural arachnoid cysts extending from T6 to L2 and causing severe gait ataxia as well as neuropathic pain and hypaesthesia. The spinal-cord was compressed at T8 and T12. Surgical treatment with partial cyst resection in the compressed levels with an interlaminar approach brought similar results as complete resection. The patient was able to walk without help which was not possible before surgery. The cysts’ extension is impressive as well as the minimal operative procedure.
Electronic supplementary material
The online version of this article (doi:10.1007/s00586-009-1156-9) contains supplementary material, which is available to authorized users.
Keywords: Intradural arachnoid cysts, Myelopathy, CT-myelography, Cyst resection
Introduction
Thoracic spinal cord compression caused by intradural arachnoid cysts is occasionally reported, but still rare [8]. Most often compression occurs because of cystic neoplastic lesions, acquired arachnoid cysts after trauma or inflammation after meningitis causing subarachnoid adhesions and parasitic lesions [26]. Other cerebrospinal fluid-containing cysts such as arachnoid diverticulum, extradural arachnoid cysts or extradural pseudomeningocele have also been described [29]. Nevertheless, very few of them cause such a spinal cord compression as the intradural arachnoid cysts do.
Idiopathic arachnoid cysts in children are associated with neural tube defects [7] and in adults with spinal deformities [1]. The aetiology of cyst formation is still unknown. Dorsal cysts could arise from diverticula of the septum posticum [22]. This theory is, however, not valid for ventrally located cysts [21]. Intradural spinal arachnoid cysts appear to result from an alteration of the arachnoid trabeculae; some of them are ascribed anecdotally to previous trauma or arachnoiditis [18], whereas the majority are idiopathic [11]. Other causes are considered to be postoperative complications, including lumbar myelography [13], meningitis with adhesions in the subarachnoidal space, epidural haematoma after surgical removal [3, 9, 13].
The majority of cases occur in the thoracic and cervical regions with a varied range of symptoms [13]. Clinical manifestations include paraparesis, neuropathic pain, gait ataxia, headaches—if in the cervical region—or incontinence.
Patients present mostly with signs of spinal cord compression. CT-myelography, MRI as well as cine-mode MRI are diagnostic procedures of choice [5, 10].
Literature review
In September 2008, we performed a literature search of MEDLINE for spinal arachnoidal cysts with no limitation for language or publication date. The search was conducted through http://www.pubmed.com, a worldwide known internet medical address.
The first search for arachnoid spinal cysts revealed 105 results (out of 500), including multiple extradural arachnoidal cysts and arachnoiditis, as a complication of infection [20], or formation of cysts as a complication of haematomas or surgery [9]. In our search we excluded children with other neural tube deformities.
The reports for intradural arachnoid cysts revealed 133 results, including, however, again arachnoiditis, syringomyelia [12], and also intradural extramedullary arachnoid cysts [2–4, 14, 22, 24, 30, 31]. Precise searches for idiopathic arachnoid spinal cysts got 18 matches (Table 1).
Table 1.
Idiopathic and non-idiopathic arachnoid cyst(s)
| Idiopathic | Non-idiopathic | |
|---|---|---|
| Yayama | Yes | |
| Wenger | Yes | |
| Papavlasopoulos | Yes | |
| Holly | Yes | |
| Jea | Syringe-subarachnoid shunt for syringomyelia | |
| Endo | Epidural haematoma | |
| Sharma | Yes | |
| Bassiouni | Major spinal trauma | |
| Takahashi | Yes | |
| Quinones-Hinojosa | Yes | |
| Wang | Yes | |
| Shibata | Spinal compression fracture | |
| Andrews | Trauma, syringomyelia | |
| Bellavia | Yes | |
| Kazan | Yes | |
| Takanashi | Yes | |
| Rivierez | Yes | |
| Kuroiwa | Traumatic |
Analysis
The analysis of the cases published revealed interesting results. Children with other spinal deformities were excluded as well as patients with arachnoid cysts other than intradural ones. The number of the reported patients who were either treated surgically or with aspiration of the cyst under MRI guidance was 74. Most cases included idiopathic cysts [4, 6, 12, 14, 16, 20, 23, 24, 28, 30–32]. Jea et al. reported the formation of an arachnoidal cyst as a complication after syringo-subarachnoid shunt operation in syringomyelia. Endo et al. reported an arachnoid cyst after the operation of an epidural spinal haematoma, whereas Bassiouni et al. after a major spinal trauma. Other causes of arachnoid spinal intradural cysts included also traumatic causes such as vertebral fracture [25] or traumatic syringomyelia [2, 16].
The clinical manifestation of the arachnoid cysts included paraparesis–quadriparesis in 51/74 patients (68.9%); 33 patients suffered from radicular neuropathic pain (44.5%); 24 patients had hypaesthesia or dysaesthesia (32.4%); 11 had severe gait ataxia (14.8%). Headache was the main symptom in a patient with a cervical arachnoid cyst (1.35%). 22 patients experience urinary incontinence (29.7%) (Table 2).
Table 2.
Clinical symptoms of the patients having arachnoidal spinal cyst(s) and underwent operation
| Paraparesis–quadriparesis (%) | Radicular pain (%) | Hypaesthesia–paraesthesia (%) | Ataxia (%) | Headaches (%) | Incontinence (%) | N | |
|---|---|---|---|---|---|---|---|
| Yayama | 100 | 6 | |||||
| Wenger | 100 | 1 | |||||
| Papavlasopoulos | 100 | 1 | |||||
| Holly | 12.5 | 87.5 | 8 | ||||
| Endo | 100 | 1 | |||||
| Sharma | 100 | 1 | |||||
| Bassiouni | 55 | 45 | 18 | ||||
| Takahashi | 100 | 1 | |||||
| Quinones-Hinojosa | 100 | 1 | |||||
| Wang | Yes | Yes | Yes | Yes | 21 | ||
| Caruso | 100 | 100 | 100 | 100 | 100 | 1 | |
| Bellavia | 100 | 1 | |||||
| Kazan | 100 | 2 | |||||
| Takanashi | 100 | 100 | 1 | ||||
| Rivierez | 100 | 100 | 1 | ||||
| Kuroiwa | 100 | 1 | |||||
| Andrews | 100 | 5 | |||||
| Shibata | 100 | 1 | |||||
| Kumar | 50 | 2 |
The diagnostic methods of choice included MRI of the spinal cord in all cases (gold standard). Four authors also used the CT myelography to prove the communication of the cysts with the subarachnoid space. The MRI has, therefore, a great diagnostic value, but we should also not forget its general limitations in patients with pacemakers or severe claustrophobia. CT myelography, on the other hand, is more invasive but with almost no complications or limitations (contrast medium allergy).
After the diagnosis is made, the choice of treatment should take into consideration following parameters: the extension of the cyst(s), the point of maximal compression of the myelon, the communication between the cyst(s) and the subarachnoid space. If the cyst is small with no communication with the subarachnoid space, an aspiration of the cyst under MRI guidance can be attempted [4]. If the cyst’s expansion is not so long and large, a cyst excision should be performed. All authors report a good-to-excellent outcome with almost no recurrence. When the cyst is multiseptated and extends throughout many vertebral bodies, a cyst fenestration should be taken into consideration to avoid an extended laminectomy with instability of the vertebral column. As the cyst is being reduced and the myelon takes its normal space, the possibility of recurrence is very low.
Case
Clinical presentation
A 44-year-old female presented at our hospital with symptoms of intermittent pain radiating to both legs and multiple falls. In the last 10 years, she had gait disturbance which in the last months became worse. The neurological examination revealed a spastic paraparesis and exaggerated reflexes in the lower limbs with bilateral positive Babinski’s sign and diffuse hypaesthesia of the left lower limb. No specific dermatome was involved. No history of trauma or inflammation of the spine. Mild kyphoscoliosis was present. There were no symptoms of incontinence.
Electrophysiology revealed decreased amplitudes for muscles of the left lower limb.
Imaging
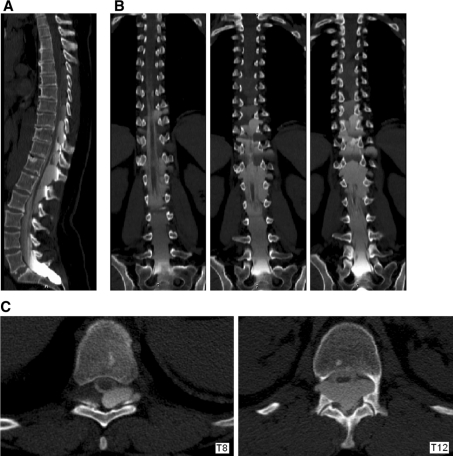
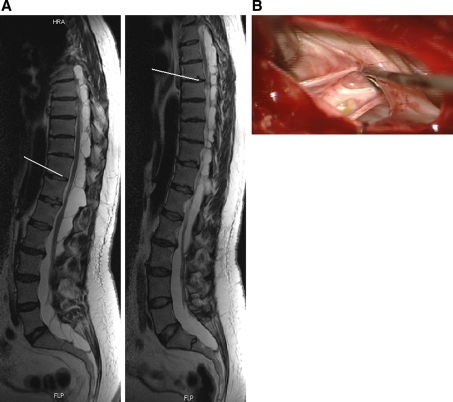
CT-myelography showed multiple cysts intradurally and extramedullary which communicated with the subarachnoid space. Dorsal compression of the spinal cord could be seen (Fig. 1). MRI of the thoraco-lumbar spine showed CSF iso-intense intradural cysts from T6 to L2 with compression of the spinal cord at T8 and T12 and positive myelopathy signs. The cysts were multiple and septated (Fig. 2a).
Fig. 1.
CT-myelography in multiply septated arachnoid cysts. a Sagittal CT reconstruction showing the filing of cysts with contrast material. b Coronal reconstructions showing the cyst contact to the dural sac. c Transverse images of the thoracic spine in the levels T8 and T12 showing a cord compression
Fig. 2.
MRI in arachnoid spinal cysts. a Sagittal MRI of the spine showing very extensive arachnoidal cysts from T6 to L2 which are multiply septated. The spinal cord is compressed in T8 and T12 (white lines). In T12 myelopathy sign can be seen which is not possible with CT. b Intraoperative image showing the septa of the cysts as well as fenestrations (at T12 level). We performed an interlaminary approach to avoid laminoplasty or laminectomy. Partial cyst removal has been performed at levels T8 and T12
Treatment
In our case, puncture of the cysts at the level of T12 with evacuation of 20 ml of cystic fluid brought an immediate recovery. Cystic fluid contained only three cells and no signs of inflammation. Nevertheless, 2 months later, progression of lower limb weakness occurred. Surgical decompression of the spinal cord has been performed with cyst extirpation at T8 and T12. Fenestration of the cysts has also been performed. Because of multiple septa, a complete extirpation of the cysts could not be performed (Fig. 2b). An interlaminar approach has been chosen avoiding laminectomy. Because of multiple adhesions only partial resection in the given levels could be performed.
Post-operatively the patient reported a good recovery. With intense physiotherapy the patient, who before the operation could not stand and go more than 3 min, was able to walk short distances with the use of a walker. The results were less satisfying regarding lower limb pain so that we added special medication such as GABA analogues. This had probably to do with the long duration of symptoms which was approximately many months before pain was evident and was expressed with residual falls.
Discussion
There are not so many published cases of intradural arachnoid cysts. It is agreed among almost all authors that the majority of the arachnoid cysts are located in the dorsal thoracic spine. In average, posterior cysts have a cranio-caudal extension of 3.7 vertebral bodies [3]. Very few cases reported findings in the craniocervical junction or the cervical spine [14, 16, 28].
The most usual clinical findings are paraparesis, neuropathetic pain, gait ataxia, hypaesthesia or dysaesthesia, rarely incontinence [30] and also unusual symptoms, including headaches in cervical cysts [27] and angina in thoracic ones [17]. Paraparesis and severe gait disturbance lead to residual falls. Clinical symptoms occur almost always after cord compression, and weakness is always present (Table 2).
MRI and CT-myelography is crucial for the diagnostic evaluation [10, 30]. In many cases where the cysts extend over multiple levels of the spine, MRI shows where a spinal cord compression occurs and leads to an accurate cyst resection and decompression in the involved levels avoiding extensive laminectomy.
The treatment of choice for the intradural spinal arachnoid cysts includes total cyst removal. Many authors propose a preoperative aspiration of the cyst under CT or MRI guidance [4]. If there is a communication, however, with the subarachnoidal space, the cyst fills again with cerebrospinal fluid and the symptoms come back.
The cyst removal is performed through a laminectomy for dorsal cysts. If they lie ventrally a fenestration through a posterolateral laminectomy can be performed [29].
If, however, the cysts are many and expand through many vertebras, as in our case, it should be taken into consideration that laminectomies in many segments would negatively influence the spinal column stability. At this point, the MRI findings contribute the most (myelopathy signal). If this is the case, the cyst extirpation is to be performed in the levels of maximum pressure and the smaller cysts have to be fenestrated.
Results after resection of cysts are excellent. Additionally cyst-to-peritoneum/-atrium shunting is also possible. Poor results can be associated with extensive laminoplasty or laminectomy approach [2, 15]. This is also the reason why only a limited resection of the cysts had been performed in our case. Simple needle aspiration has been proven in most cases inadequate [19] (Table 3).
Table 3.
The treatment of choice includes cyst excision, cyst fenestration with laminectomy/hemilaminectomy or cyst drainage with or without MRI guidance
| Cyst excision (%) | Cyst fenestration (%) | Cyst aspiration/drainage (%) | |
|---|---|---|---|
| Yayama | Yes | Yes | |
| Wenger | 100 | ||
| Papavlasopoulos | 100 | ||
| Holly | 100 | ||
| Endo | 100 | ||
| Sharma | 100 | ||
| Bassiouni | 100 | Yes | |
| Takahashi | 100 | ||
| Quinones-Hinojosa | 100 | ||
| Wang | Yes | Yes | |
| Caruso | Yes | Yes | |
| Bellavia | 100 | ||
| Kazan | Yes | Yes | |
| Takanashi | 100 | ||
| Rivierez | 100 | ||
| Kuroiwa | 100 | ||
| Andrews | 100 | ||
| Shibata | 100 | ||
| Kumar | 100 |
Neuropathic pain and hypaesthesia is less likely to improve [30]. Even if the postoperative time is not long enough to make conclusions, we observed that weakness had improved fast, whereas pain still exists.
Here we reported another case of idiopathic thoracic intradural arachnoid cysts. The size of the multiply septated cysts is impressive extending from T6 to L2 with dorsal spinal cord compression at T8 and T12.
Conclusion
In the present case, intradural arachnoidal cysts extending from T6 to L2 are treated with minimal resection in areas of spinal cord compression. Even though partial resection without laminectomy approach has been performed, the patient had an immediate improvement of her condition and was able to walk without help again.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
Footnotes
A. K. Petridis and A. Doukas contributed equally to this work.
References
- 1.Alvisi C, Cerisoli M, Giulioni M, Guerra L. Long-term results of surgically treated congenital intradural spinal arachnoid cysts. J Neurosurg. 1987;67:333–335. doi: 10.3171/jns.1987.67.3.0333. [DOI] [PubMed] [Google Scholar]
- 2.Andrews BT, Weinstein PR, Rosenblum ML, Barbaro NM. Intradural arachnoid cysts of the spinal canal associated with intramedullary cysts. J Neurosurg. 1988;68(4):544–549. doi: 10.3171/jns.1988.68.4.0544. [DOI] [PubMed] [Google Scholar]
- 3.Bassiouni H, Hunold A, Asgari S, et al. Spinal intradural juxtamedullary cysts in the adult: surgical management and outcome. Neurosurgery. 2004;55:1352–1360. doi: 10.1227/01.NEU.0000143031.98237.6D. [DOI] [PubMed] [Google Scholar]
- 4.Bellavia R, King JT, Jr, Naheedy MH, Lewin JS. Percutaneous aspiration of an intradural/extradural thoracic arachnoid cyst: use of MR imaging guidance. J Vasc Interv Radiol. 2000;11(3):369–372. doi: 10.1016/S1051-0443(07)61432-8. [DOI] [PubMed] [Google Scholar]
- 5.Boisserie-Lacroix M, Bouin H, Joullie M, Laurent F, Biset JM, Drouillard J, Grelet PH. The value of MRI in the study of spinal extradural arachnoid cysts. Comput Med Imaging Graph. 1990;14:221–223. doi: 10.1016/0895-6111(90)90065-J. [DOI] [PubMed] [Google Scholar]
- 6.Caruso G, Germano A, Caffo M, Belvedere M, La Rosa G, Divitiis O, Tomasello F. Anterior thoracic intradural arachnoid cysts. Case report and review of the literature. Neurosurg Focus. 1999;6(5):e8. doi: 10.3171/foc.1999.6.5.11. [DOI] [PubMed] [Google Scholar]
- 7.Duncan A, Hoare R. Spinal arachnoid cysts in children. Neuroradiology. 1978;126:423–429. doi: 10.1148/126.2.423. [DOI] [PubMed] [Google Scholar]
- 8.Dyck P. Myelopathy due to spinal arachnoid cyst. Spine. 1986;11:80–82. doi: 10.1097/00007632-198601000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Endo H, Takahashi T, Shimizu H, Tominaga T. Thoracic intradural arachnoid cyst associated with surgical removal of epidural hematoma—case report. Neurol Med Chir Tokyo. 2004;44(11):607–610. doi: 10.2176/nmc.44.607. [DOI] [PubMed] [Google Scholar]
- 10.Fujimura M, Tominaga T, Koshu K, Shimizu H, Yoshimoto T. Cine-mode magnetic resonance imaging of a thoracic intradural arachnoid cyst: case report. Surg Neurol. 1996;45:533–536. doi: 10.1016/0090-3019(95)00479-3. [DOI] [PubMed] [Google Scholar]
- 11.Gelabert-González M, Cutrín-Prieto JM, García-Allut A. Spinal arachnoid cyst without neural tube defect. Childs Nerv Syst. 2001;17(3):179–181. doi: 10.1007/s003810000367. [DOI] [PubMed] [Google Scholar]
- 12.Holly LT, Batzdorf U. Syringomyelia associated with intradural arachnoid cysts. J Neurosurg Spine. 2006;5(2):111–116. doi: 10.3171/spi.2006.5.2.111. [DOI] [PubMed] [Google Scholar]
- 13.Jea A, Navarro R, Green BA. Rapid expansion of a ventral arachnoid cyst after syringo-subarachnoid shunting in the thoracic spinal cord: case report. Surg Neurol. 2005;64(1):86–89. doi: 10.1016/j.surneu.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 14.Kazan S, Ozdemir O, Akyüz M, Tuncer R. Spinal intradural arachnoid cysts located anterior to the cervical spinal cord. Report of two cases and review of the literature. J Neurosurg. 1999;91(Suppl 2):211–215. doi: 10.3171/spi.1999.91.2.0211. [DOI] [PubMed] [Google Scholar]
- 15.Kriss TC, Kriss VM. Symptomatic spinal intradural arachnoid cyst development after lumbar myelography. Case report and review of the literature. Spine. 1997;22:568–572. doi: 10.1097/00007632-199703010-00023. [DOI] [PubMed] [Google Scholar]
- 16.Kuroiwa T, Takeuchi E, Yamada K, Ohta T, Miyaji Y, Onomura T. An intradural arachnoid cyst of the craniovertebral junction: a case report. No Shinkei Geka. 1991;19(11):1097–1099. [PubMed] [Google Scholar]
- 17.Kumar K, Malik S, Schulte PA. Symptomatic spinal arachnoid cysts: report of two cases with review of the literature. Spine. 2003;28(2):E25–E29. doi: 10.1097/00007632-200301150-00019. [DOI] [PubMed] [Google Scholar]
- 18.Lee HJ, Cho DY. Symptomatic spinal intradural arachnoid cysts in the pediatric age group: description of three new cases and review of the literature. Pediatr Neurosurg. 2001;35(4):181–187. doi: 10.1159/000050419. [DOI] [PubMed] [Google Scholar]
- 19.Osenbach RK, Godersky JC, Traynellis VC, et al. Intradural extramedullary cysts of the spinal canal: clinical presentation, radiographic diagnosis and surgical management. Neurosurgery. 1992;30:35–42. doi: 10.1227/00006123-199201000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Papavlasopoulos F, Stranjalis G, Kouyialis AT, Korfias S, Sakas D. Arachnoiditis ossificans with progressive syringomyelia and spinal arachnoid cyst. J Clin Neurosci. 2007;14(6):572–576. doi: 10.1016/j.jocn.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 21.Paramore C. Dorsal arachnoid web with spinal cord compression: variant of an arachnoid cyst. J Neurosurg. 2000;93:287–290. doi: 10.3171/spi.2000.93.2.0287. [DOI] [PubMed] [Google Scholar]
- 22.Perret G, Green D, Keller J. Diagnosis and treatment of intradural arachnoid cysts of thoracic spine. Radiology. 1962;79:424–429. doi: 10.1148/79.3.425. [DOI] [PubMed] [Google Scholar]
- 23.Quinones-Hinojosa A, Sanai N, Fischbein NJ, Rosenberg WS. Extensive intradural arachnoid cyst of the lumbar spinal canal: case report. Surg Neurol. 2003;60(1):57–59. doi: 10.1016/S0090-3019(03)00150-2. [DOI] [PubMed] [Google Scholar]
- 24.Sharma A, Sayal P, Badhe P, Pandey A, Diyora B, Ingale H. Spinal intramedullary arachnoid cyst. Indian J Pediatr. 2004;71(12):e65–e67. doi: 10.1007/BF02829825. [DOI] [PubMed] [Google Scholar]
- 25.Shibata T, Nakamura H, Yamano Y. Intradural arachnoid cyst associated with thoracic spinal compression fracture: 7-year follow up after surgery. Spinal Cord. 2001;39(11):599–601. doi: 10.1038/sj.sc.3101217. [DOI] [PubMed] [Google Scholar]
- 26.Sklar E, Quencer R, Green B, Montalvo B, Post M. Acquired spinal subarachnoid cysts. Am J Neuroradiol. 1989;10:1097–1104. [PMC free article] [PubMed] [Google Scholar]
- 27.Takahashi S, Morikawa S, Egawa M, Saruhashi Y, Matsusue Y. Magnetic resonance imaging-guided percutaneous fenestration of a cervical intradural cyst. Case report. J Neurosurg. 2003;99(Suppl 3):313–315. doi: 10.3171/spi.2003.99.3.0313. [DOI] [PubMed] [Google Scholar]
- 28.Takanashi Y, Mochimatsu Y, Shyudo T, Yamamoto I. A case report of an arachnoid cyst in the craniovertebral junction. No To Shinkei. 1995;47(1):68–70. [PubMed] [Google Scholar]
- 29.Tarlov E, Geyer C (1998) Intraspinal cerebrospinal-fluid cysts, in operative neurosurgical techniques, 5th edn. Schmidek & Sweet, pp 477–483
- 30.Wang MY, Levi ADO, Barth A, Green MD. Intradural spinal arachnoid cysts in adults. Surg Neurol. 2003;60:49–55. doi: 10.1016/S0090-3019(03)00149-6. [DOI] [PubMed] [Google Scholar]
- 31.Wenger M, Zobor N, Markwalder R, Vogt E, Markwalder T-M. Intradural extramedullary arachnoid cyst of the thoracic spine associated with cord compression. J Clin Neurosci. 2007;14:693–696. doi: 10.1016/j.jocn.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 32.Yayama T, Kobayashi S, Uchida K, Kokubo Y, Nakajima H, Sato R, Bangirana A, Takamura T, Baba H. Insidious progression of paraparesis secondary to type III spinal meningeal cyst: a study of six difficult cases. Spinal Cord. 2008;46(2):159–161. doi: 10.1038/sj.sc.3102079. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.