Abstract
The objective of this retrospective study was to analyze the relationship between the type of destructive spondyloarthropathy (DSA) and its 10 years ago cervical spine alignment. DSA was reported as a serious complication of long-term hemodialysis. Although previous reports in regard to risk factor of DSA dealt with the period of hemodialysis and the patient’s age upon commencement of hemodialysis, we could not find any reports of the relationship between the type of DSA and its 10 years ago cervical spine alignment. In 96 DSA patients who were the subjects of our study, 8 patients were defined as stage 1, 39 patients as stage 2, 5 patients as stage 3 type A, 11 patients as stage 3 type B, and 33 patients as stage 3 type D. The C2/C7 angle of stage 3 type B was statistically low. The number of the abnormal local cervical alignment was larger in stage 3 types A and B. Multivariate analysis revealed that the risk factors of stage 3 types A and B were the C2/C7 angle and the existence of local abnormal alignment. Fifty-four patients were symptomatic due to DSA and treated at our hospital. Forty-four patients were treated conservatively with medications, physiotherapy, or wearing cervical brace. Ten patients underwent surgical treatment. The loss of physiological lordosis of cervical spine promoted the progression of DSA. Furthermore, the number of the abnormalities of local cervical alignment was statistically larger in stage 3 types A and B; they were the crucial factor promoting the progression of DSA stage 3 types A and B.
Keywords: Destructive spondyloarthropathy (DSA), Hemodialysis, Cervical spine
Introduction
The recent advances in hemodialysis have prolonged the patients’ life span and increased the number of the hemodialysis patients. However, the incidence of complications has increased, too. Several complications, e.g., bone cyst, tenosynovitis, renal osteodystrophy, synovitis, and soft tissue calcification, occur in the musculoskeletal tissue.
Destructive spondyloarthropathy (DSA), which makes the spine destructive change is also one of these complications. DSA was reported as a serious complication of long-term hemodialysis by Kunz et al. [7] for the first time in 1984. It is radiographically characterized by severe narrowing of the intervertebral disk space and erosions and cysts of the adjacent vertebral plates with minimal osteophyte formation.
DSA often causes severe neurological deficits with negative impact on the patients’ quality of life.
The pathogenesis and natural history of DSA are still not fully understood, but it is a well-known amyloidosis, which consists of β2-microglobulin and plays an important role in the development of DSA [2, 3, 15–17].
The incidence of DSA is reportedly around 20%. Fiocchi et al. [3] reported 18.0%, and Leone et al. [8] reported 19.4%. In our previous study [20], the incidence of DSA was 20.8% (123 of 616 patients), and almost corresponded to the former studies.
In addition, Maruyama et al. [10] suggested that the DSA lesions were mostly detected in the highly mobile areas, such as C5–C7 and L3–L5. Ohashi et al. [14] explained this phenomenon by describing that the collagen degenerated by mechanical stress has a high affinity for β2-microglobulin.
In regard to risk factor of DSA dealt with the period of hemodialysis and the patient’s age upon commencement of hemodialysis, we could not find any reports of the relationship between the type of DSA and its 10 years ago cervical spine alignment. We presume that previous disorder of cervical spine alignment facilitates progression of DSA in hemodialysis patients. The purpose of this study is to analyze the relationship between the type of DSA and its 10 years ago cervical spine alignment.
Materials and methods
We investigated cervical plain radiographs of 616 patients who underwent hemodialysis in our hospital. 123 patients had DSA lesions at present. All of these 123 DSA patients had over 10 years hemodialysis experience, and 21 patients who had already suffered from DSA 10 years ago were excluded from this study. So, we included 96 patients with whom cervical X-ray 10 years ago was available. All patients did have X-rays routinely at least one time a year.
However, the excluded 21 patients were analyzed whether their DSA lesions were deteriorated to date. The subjects of our study were 96 patients (45 males and 51 females) whom cervical plain radiographs 10 years ago were available and had not shown the feature of DSA at that time. The mean patient’s age was 52 years upon commencement of hemodialysis (range: 15–88 years). The mean period of hemodialysis was 12.9 years at the end of the study (range: 10–29.6 years) (Table 1). Six orthopedic surgeons (over 8 years experienced spine surgeons) evaluated the radiographs, and regarded the presence of erosions and destruction of the vertebrae, intervertebral disk space narrowing, and spondylolisthesis without apparent osteophyte formation as DSA. We classified all cases with DSA into three stages according to Maruo’s criteria as follows [9]: stage 1 is defined as a case exhibiting only vertebral erosion, stage 2 is defined as a case exhibiting intervertebral disk space narrowing without osteophyte, and stage 3 is defined as a case exhibiting destruction of the vertebra and instability of the spine. In addition, stage 3 was divided into four subtypes as follows: type A is defined as a case exhibiting kyphosis due to vertebral destruction, type B is defined as a case exhibiting instability of spine due to spondylolisthesis, type C is defined as a case exhibiting canal stenosis due to amyloid deposition, type D is defined as a case exhibiting stability of spine due to spontaneous fusion of vertebras. However, type C is excluded in our study because it cannot be identified by only plain radiograph and its diagnosis needs magnetic resonance imaging (MRI).
Table 1.
Summary of all patients
| DSA | |
|---|---|
| n | 96 |
| Sex (male/female) | 45/51 |
| Age (mean ± SD years) | 52.0 ± 13.0 |
| The period of hemodialysis (mean ± SD years) | 12.9 ± 6.9 |
DSA destructive spondyloarthropathy
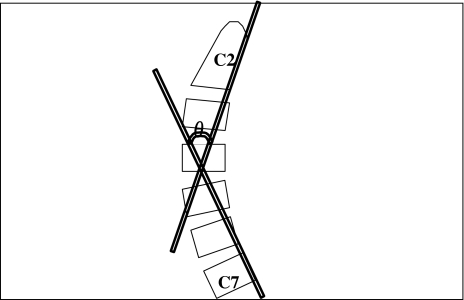
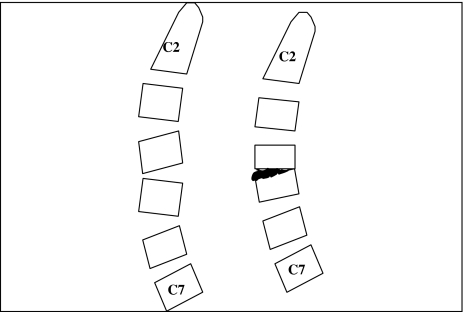
The whole cervical alignment is represented by C2/C7 angle which is defined as the angle between posterior side of second cervical vertebra and seventh cervical vertebra in lateral plain radiographs of the cervical spine (Fig. 1). The abnormality of local cervical alignment is represented by local cervical kyphosis, fusion, and deformity except for DSA lesion (Fig. 2).
Fig. 1.
Whole cervical alignment (C2/C7 angle). C2/C7 angle was defined as the angle between posterior side of second and seventh cervical vertebra in lateral plain radiographs of cervical spine 10 years ago
Fig. 2.
Abnormality of local cervical alignment. Local cervical kyphosis, fusion, and deformity except for DSA lesion shown in lateral plain radiographs of cervical spine 10 years ago
Statistical analysis was performed using the Student’s t test and Fisher’s exact probability test for comparing the each factor. Furthermore, multivariate analysis, dependent variable during logistic regression analysis was performed to define the risk factors of DSA. For all tests, P values less than 0.05 were considered significant.
Results
There were 21 patients who had already suffered from DSA 10 years ago. Four patients were defined as stage 1, 16 patients as stage 2, 1 patient as stage 3 in cervical plain radiographs 10 years ago. Two of four patients who were defined as stage 1 had been deteriorated to stage 2. Five of 16 patients who were defined as stage 2 had been aggravated to stage 3. One patient who was defined as stage 3 had not changed. They were removed from this study.
Of 96 patients who were the subjects of our study, 8 patients were defined as stage 1, 39 patients as stage 2, 5 patients as stage 3 type A, 11 patients as stage 3 type B, and 33 patients as stage 3 type D (Table 2).
Table 2.
Classification of DSA (Maruo’s criteria) and details
| n | Intitial age at hemodialysis | Period of hemodialysis | C2/C7 angle | Existence of local kyphosis (%) | |
|---|---|---|---|---|---|
| Stage 1 | 8 | 52.0 ± 9.0 | 11 ± 3.4 | 13.1 ± 2.3 | 0 (0) |
| Stage 2 | 39 | 51.4 ± 6.0 | 10 ± 2.9 | 14.2 ± 3.4 | 2 (5.1) |
| Stage 3 type A | 5 | 49.0 ± 8.0 | 12 ± 7.8 | 10.2 ± 2.0 | 5 (100)* |
| Stage 3 type B | 11 | 53.0 ± 7.2 | 15 ± 2.1 | 6.0 ± 1.5* | 11 (100)* |
| Stage 3 type D | 33 | 52.2 ± 8.0 | 13 ± 6.8 | 13.4 ± 2.4 | 5 (15.2) |
| Total | 96 | Average: 52.0 ± 13.0 | Average: 12.9 ± 6.9 |
*P < 0.001
C2/C7 angle and local abnormal alignment of these patients were analyzed 10 years ago. The mean C2/C7 angle was 13.1° at stage 1, stage 2: 14.2°, stage 3 type A: 10.2°, stage 3 type B: 6.0°, and stage 3 type D: 13.4°. The angle of stage 3 type B was statistically low (Table 2).
The abnormalities of local cervical alignment were detected in stage 1: 0 case, stage 2: 2 cases (5.1%), stage 3 type A: 5 cases (100%), stage 3 type B: 11 cases (100%), and stage 3 type D: 5 cases (15.2%).
In statistical analysis, the number of the abnormal local cervical alignment was larger in stage 3 types A and B (P < 0.01) (Table 2).
Multivariate logistic regression analysis revealed that the risk factors of stage 3 types A and B were the C2/C7 angle and the existence of local abnormal alignment (Table 3).
Table 3.
The risk factors of DSA stage 3 types A and B
| Odds ratio | P value | |
|---|---|---|
| Initial age at hemodialysis | 0.34 | 0.63 |
| Period of hemodialysis | 0.58 | 0.58 |
| C2/C7 angle | 1.99 | <0.001 |
| Existence of local kyphosis | 0.87 | <0.01 |
Fifty-four patients were symptomatic due to DSA and treated at our hospital. Of symptomatic 54 cases, 44 patients were treated conservatively with medications, physiotherapy, or wearing cervical brace. Ten patients underwent surgical operation. Concerned about symptomatic cases, 14 cases of stage 2, 5 cases of stage 3 type A, 11 cases of stage 3 type B, and 24 cases of stage 3 type D had clinical symptoms. Of ten operative cases, four were stage 3 type A and six were stage 3 type B. In statistical analysis, there were more number of symptomatic and operative cases in stage 3 types A and B (P < 0.001).
Case presentation
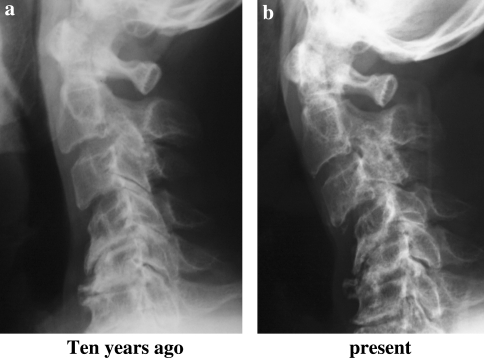
A 72-year-old man underwent hemodialysis since he was 60 years old (Fig. 3). The pathophysiology requiring hemodialysis was chronic glomerulonephritis (CGN). In lateral plain radiograph of cervical spine 10 years ago, the abnormality of local cervical alignment was apparent by vertebral disk space narrowing, kyphosis, and osteophyte formation in fourth, fifth, and sixth cervical spines (Fig. 3a). Furthermore, as his C2/C7 angle was −17°, the abnormality of whole cervical alignment was confirmed. In the lateral plain radiograph of cervical spine at present time, DSA lesion of stage 3 type B was detected and the C2/C7 angle deteriorated into −30° (Fig. 3b). Therefore, it was thought that the abnormality of his local and whole cervical alignment led to severe type of DSA.
Fig. 3.
A case of deterioration of DSA
The clinical symptom was gait disturbance with spasticity and undergone with cervical laminoplasty with instrumentation.
Discussion
Since Kunz et al. [7] reported the concept of DSA, many research projects were initialized to elucidate its pathogenesis. Some reports referred to deposition of aluminum, hydroxyapatite crystals, and secondary hyperparathyroidism as possible causes of DSA [1, 5, 11, 18], but there was no convincing evidence that they were definite etiological factors in the development of DSA.
In the recent years, it has been clarified that the hemodialysis patients suffer from spinal canal stenosis due to soft tissue proliferation, e.g., intraspinal ligamentous hypertrophy and disk protrusion because of amyloid deposition [12, 13]. The dialysis-related amyloidosis can induce both destructive spinal change and intraspinal soft tissue proliferation. It is difficult to diagnose the latter only with plain radiography. MRI examination is necessary to diagnose them. Therefore, they were excluded from this study.
The incidence of DSA is reportedly around 20%. Fiocchi et al. [3] reported 18.0% (9 of 50 patients) and Leone et al. [8] reported 19.4% (6 of 31 patients). In our study [20], the incidence of DSA was 20.8% (123 of 616 patients) and almost corresponded to the former studies.
The period of hemodialysis has been considered as the main predictive factor for DSA. Fukutake et al. [4] analyzed lateral plain radiographs of the cervical spine of 193 patients treated by hemodialysis, and reported the mean hemodialysis period for the patients with DSA (12.8 years) was longer than that of the patients without DSA (7.7 years).
In our previous study [20], we also found that the incidence of DSA in the patients who underwent hemodialysis for more than 15 years was significantly high (38.6%), and that the period of hemodialysis was a risk factor for the development of DSA.
Similarly, the patient’s age upon commencement of hemodialysis was a risk factor for the development of DSA in our study, and this agrees with almost all previous studies [6, 19].
Although previous reports in regard to risk factor of DSA dealt with the period of hemodialysis and the patient’s age upon commencement of hemodialysis, we could not find any reports of the relationship between the type of DSA and its 10 years ago cervical spine alignment.
Patients with DSA in stage 1 and stage 2 hardly exhibit any symptoms, whereas patients in stage 3 exhibit severe neurological deficits. But patients in stage 3 type D do not exhibit severe symptoms. To the contrary, patients in stage 3 types A and B exhibit severe symptoms. Therefore, it is crucial clinically to predict which patients tend to progress to stage 3 type A or stage 3 type B.
The C2/C7 angle, which represents whole cervical alignment, was statistically low in DSA patients of stage 3 type B. It was suggested that the loss of physiological lordosis of cervical spine promoted the progression of DSA stage 3 type B. Furthermore, because the number of the abnormalities of local cervical alignment was statistically larger in stage 3 types A and B, they were speculated to be crucial factors promoting the progression of DSA stage 3 types A and B. We demonstrated the risk factor of DSA stage 3 types A and B were low C2/C7 angle and kyphotic cervical spine alignment. If the case would progress to be in stage 3 type A or stage 3 type B with clinical symptom, this case would have prophylactic surgery.
References
- 1.Adler JS, Cameron DC. Erosive spondylo-arthropathy and tertiary hyperparathyroidism. Australas Radiol. 1989;33:90–92. doi: 10.1111/j.1440-1673.1989.tb03243.x. [DOI] [PubMed] [Google Scholar]
- 2.Baldrati L, Brunetti L, Rocchi A. Osteo-articular amyloidosis caused by dialysis. Clinical and radiologic aspects. Minerva Med. 1990;81:679–682. [PubMed] [Google Scholar]
- 3.Fiocchi O, Bedani PL, Orzincolo C, et al. Radiological features of dialysis amyloid spondyloarthropathy. Int J Artif Organs. 1989;12:216–222. [PubMed] [Google Scholar]
- 4.Fukutake T, Takagi K, Kuwabara S. Destructive spondyloarthropathy of the cervical spine in hemodialyzed patients. No To Shinkei. 1997;49:713–722. [PubMed] [Google Scholar]
- 5.Kaplan P, Resnick D, Murphey M, et al. Destructive noninfectious spondyloarthropathy in hemodialysis patients: a report of four cases. Radiology. 1987;162:241–244. doi: 10.1148/radiology.162.1.3786769. [DOI] [PubMed] [Google Scholar]
- 6.Kessler M, Netter P, Azoulay E, et al. Dialysis-associated arthropathy: a multicentre survey of 171 patients receiving haemodialysis for over 10 years. The Co-operative Group on Dialysis-associated Arthropathy. Br J Rheumatol. 1992;31:157–162. doi: 10.1093/rheumatology/31.3.157. [DOI] [PubMed] [Google Scholar]
- 7.Kunz D, Naveau B, Bardun T, et al. Destructive spondyloarthropathy in hemodialyzed patients: a new syndrome. Arthritis Rheum. 1984;27:369–375. doi: 10.1002/art.1780270402. [DOI] [PubMed] [Google Scholar]
- 8.Leone A, Sundaram M, Cerase A, et al. Destructive spondyloarthropathy of the cervical spine in long-term hemodialyzed patients: a five-year clinical radiological prospective study. Skeletal Radiol. 2001;30:431–441. doi: 10.1007/s002560100389. [DOI] [PubMed] [Google Scholar]
- 9.Maruo S, Taniguchi M, Otsuka S, et al. The pathogenesis and treatment for DSA on long-term hemodialysed patients. Sekitsui Sekizui J. 1997;10:1065–1070. [Google Scholar]
- 10.Maruyama H, Gejyo F, Arakawa M. Clinical studies of destructive spondyloarthropathy in long-term hemodialysis patients. Nephron. 1992;61:37–44. doi: 10.1159/000186832. [DOI] [PubMed] [Google Scholar]
- 11.McCarthy JT, Dahlberg PJ, Kriegshauser JS, et al. Erosive spondyloarthropathy in long-term dialysis patients: relationship to severe hyperparathyroidism. Mayo Clin Proc. 1988;63:446–452. doi: 10.1016/s0025-6196(12)65640-7. [DOI] [PubMed] [Google Scholar]
- 12.Niwa T. Dialysis-related amyloidosis: pathogenesis focusing on AGE modification. Semin Dial. 2001;14:123–126. doi: 10.1046/j.1525-139x.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- 13.Nokura K, Koga H, Yamamoto H, Kimura A, et al. Dialysis-related spinal canal stenosis: a clinicopathological study on amyloid deposition and its AGE modification. J Neurol Sci. 2000;178:114–123. doi: 10.1016/S0022-510X(00)00377-4. [DOI] [PubMed] [Google Scholar]
- 14.Ohashi K, Hara M, Kawai R. Cervical discs are most susceptible to beta 2-microglobulin amyloid deposition in the vertebral column. Kidney Int. 1992;41:1646–1652. doi: 10.1038/ki.1992.237. [DOI] [PubMed] [Google Scholar]
- 15.Orzincolo C, Bedani PL, Scutellari PN, et al. Osteoarticular amyloidosis caused by dialysis. Radiol Med (Torino) 1988;76:38–43. [PubMed] [Google Scholar]
- 16.Sebert JL, Fardellone P, Deramond H, et al. Destructive spondylarthropathy with amyloid deposits in 3 patients on chronic hemodialysis. Rev Rhum Mal Osteoartic. 1986;53:459–465. [PubMed] [Google Scholar]
- 17.Sulkova S, Votruba T. Dialysis amyloidosis and beta-2-microglobulin. Cas Lek Cesk. 1989;13(128):68–73. [PubMed] [Google Scholar]
- 18.Sundaram M, Dessner D, Ballal S. Solitary, spontaneous cervical and large bone fractures in aluminum osteodystrophy. Skeletal Radiol. 1991;20:91–94. doi: 10.1007/BF00193817. [DOI] [PubMed] [Google Scholar]
- 19.Ypersele De Strihou C, Jadoul M, Malghem J, et al. Effect of dialysis membrane and patient’s age on signs of dialysis-related amyloidosis. Kidney Int. 1991;39:1012–1019. doi: 10.1038/ki.1991.128. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto T, Matsuyama Y, Tuji T, Nakamura H, Yanase M, Ishiguro N. Destructive spondylo Arthoropathy (DSA) in hemodialysis patients—comparison between patients with and those without DSA. J Spinal Disord Tech. 2005;18(3):283–285. [PubMed] [Google Scholar]