Abstract
The authors investigated the effect of neck dimension upon cervical range of motion. Data relating to 100 healthy subjects, aged between 20 and 40 years, were recorded with respect to age, gender and range of motion in three planes. Additionally, two widely used methods of measuring neck motion, chin-sternal distance and uniplanar goniometer, were assessed against a validated measurement tool, the ‘CROM goniometer’. Using multiple linear regression analysis it was determined that sagittal flexion (P = 0.002) and lateral rotation (P < 0.0001) were most closely related to neck circumference alone whereas lateral flexion (P < 0.0001) was most closely related to a ratio of circumference and length of neck. Hence, assessing cervical range of motion as outcome variable or as a measure at posttreatment follow-up, neck circumference was shown to be one of the factors influencing total neck motion, particularly sagittal flexion and lateral tilt. Comparison of cervical range of motion assessed with a validated measurement tool, the CROM goniometer, with results of both frequently applied clinician’s instruments, the uniplanar goniometer and measurement of chin-sternal distance, showed low reliability with the latter techniques, and motion values measured with these techniques should be interpreted with caution if using them for comparison of cervical range of motion of alike groups. We demonstrated that neck dimension should be incorporated into cervical functional outcome assessment and one should be wary about recorded values for neck motion from non-validated measurement tools.
Keywords: Cervical spine, Goniometer, Neck dimension, Morphology, Range of motion
Introduction
In Norway, Bovim et al. [4] found a prevalence of neck pain of 13.8% in a random sample of 10,000 persons aged 18–67 years. In Finland [15], neck pain occurred in 9.5% of males and 13.5% of females while in Northern England there was a prevalence of reported neck pain for greater than 1 week per month in 16.5% of females and 10.7% of males [24]. In contrast to lumbar back pain, neck pain is frequently associated with previous injury [9, 15]. In the United States the National Highway Safety Administration estimates over 8,00,000 people suffering whiplash-injuries every year and related costs have been calculated at $5.2 billion. In light of the impaired cognitive and psychological functions [19] found in subjects complaining of whiplash such individuals are difficult to assess quantifiably. One of the few objective measurements in neck pain and whiplash-associated disorders is with neck stiffness [20]. Thus accurate measurement of cervical range of movement (CROM) is essential in objective assessment of neck symptomology and the effects of any intervention [14, 21].
Cervical range of movement is difficult to measure accurately. In an attempt to address this, a number of techniques have been developed to measure CROM reproducibly. Many of these are limited by their complexity or the requirement of radiographs [2, 13], but with these techniques researchers have been able to tabulate CROM in normal subjects [7] and show that neck stiffness increases with age. These studies do not address the effect of the shape of the neck on CROM.
We set out to test the hypothesis that neck morphology affects CROM and in conjunction compare the accuracy of commonly used methods of measuring CROM in comparison to a validated measuring device.
Materials and methods
Patient sample
Fifty one men and 49 women aged between 20 and 40 years (mean 28.1 years) volunteered for the study after providing informed consent to participate. All subjects with a history of previous cervical spine injury or recent shoulder girdle injury were excluded.
Measurement techniques
Assessment of neck morphology
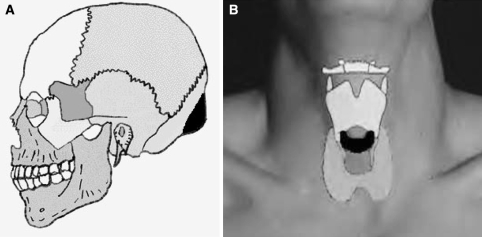
We defined neck morphology using a measuring tape. We recorded the length of the cervical spine from the external occipital protuberance (Fig 1a) to the vertebra prominens as well as the circumference at the level of the cricoid cartilage (Fig 1b) anteriorly and spinous process of the sixth cervical vertebra posteriorly. Neck morphology was expressed as the ratio between circumference and length. The seventh cervical vertebra was determined to be that with the most cephalad, prominent spinous process (vertebra prominens) and the sixth cervical vertebra as being that immediately cephalad on deep palpation.
Fig. 1.
Cricoid cartilage and external occipital protuberance marked in black
Measuring devices
The instruments used to assess CROM were a tape measure, a classic orthopaedic handheld goniometer and a CROM goniometer (Performance Attainment Associates, Roseville, MN). The tape measure is easily available and widely used in physical therapy. The handheld goniometer is an easily accessible and convenient clinical tool but is limited by an inability to record complex movements with greater than one centre of rotation. It is, however, one that is familiar to the non-specialised clinician and used in several clinical studies to objectivate the outcome [18]. The CROM goniometer is a validated [22, 25] tool for measuring CROM. It consists of a headpiece incorporating three inclinometers and a magnetic yolk (Fig. 2); examination with CROM goniometer is quick, taking under 5 min. The CROM goniometer's relatively large size, cost of approximately $500 and bulky packaging, however, is a limiting factor when compared to a simple goniometer and tape measure which are relatively inexpensive and user friendly.
Fig. 2.
CROM goniometer (Performance Attainment Associates, Roseville, MN)
Measurement process
Subjects were placed in a straight, high-backed chair with their feet flat on the floor and hands relaxed by their sides. They were then asked to sit up straight and position their head in neutral as described by Christensen and Nilsson [8] with subsequent confirmation of the reproducibility of the individual to accurately achieve neutral alignment [3].
The following movements were recorded—sagittal flexion/extension, lateral flexion and lateral rotation. In sagittal flexion and extension, the subjects were required to make a “double chin” (suboccipital flexion) then flex fully forward followed by nodding the head back and then fully extending. In lateral flexion, the subjects fixed their gaze on a set point directly ahead and were observed whilst laterally flexing both to the right and then to the left. In lateral flexion, the subject looked to the right and then left whilst holding a horizontal gaze parallel to the floor.
Prior to the measuring process, a demonstration of the movements to be studied was given prior to definitive measurement and then repeated by the subject. This served to facilitate the examination and allowed the neck muscles and ligaments to “warm up”. Maximal movement was recorded as that achieved at onset of tightness, discomfort, or secondary movement, e.g. shoulder tilt or head rotation when assessing lateral flexion.
The measuring process started with the assessment of the chin to sternal notch distance recorded with a tape measure with the head aligned in neutral, full sagittal flexion and full sagittal extension. Each movement was then assessed in turn using the handheld goniometer. To improve reproducibility we set specific landmarks for measurement. For sagittal flexion/extension, a vertical line was taken from the acromioclavicular joint to the centre of rotation at the level of the sixth cervical vertebra. For lateral flexion a vertical line was drawn from the sternal notch with centre of rotation at the cricoid cartilage. Lateral rotation was taken from the vertex. The movements were then repeated measuring with the CROM goniometer as per the instructions issued with the CROM goniometer.
The first author and a junior doctor under his supervision assessed all participants.
Data analysis
The data were analysed by an independent professional statistician. Age, gender and functions of circumference and length of the neck were compared with the sums of flexion-extension, lateral flexion and rotation recorded by the CROM goniometer using multiple linear regression.
The readings obtained with the tape measure and the handheld goniometer were compared to those obtained by the CROM goniometer with the Pearson Correlation Coefficient.
Results
The mean cervical sagittal active range of movement was 125° ± 19.3° (range 61°–166°). Cervical sagittal active range of movement most closely correlated to neck circumference alone with no other significant contributor to the regression model (Table 1). Taking the single variable, circumference, 9% (r2 = 0.09) of the variance observed with lateral rotation could be explained (P = 0.002) (Table 2).
Table 1.
Multiple linear regression models produced for the three cervical ranges of movement (in degrees)
| Linear regression model |
|---|
| Lateral flexion = 140 – 0.6 × (age) – 17.8 × (circumference/length) |
| Rotation (total) = 186 − 1.5 × (circumference) cm |
| Sagittal CROM = 179 − 1.5 × (circumference) cm |
Table 2.
Summary of statistical data for sagittal active range of movement
| Source | Degrees of freedom | Sum of squares | Mean square | F value | P > F |
|---|---|---|---|---|---|
| Model | 1 | 3,384 | 3,384 | 9.95 | 0.0021 |
| Error | 98 | 33,329 | 340 | ||
| Corr. total | 99 | 36,713 |
| Variable | Parameter estimate | Standard error | Type II SS | F value | P > F |
|---|---|---|---|---|---|
| Intercept | 178.79 | 17.22 | 36,624 | 107.69 | <0.0001 |
| Circumf. | −1.492 | 0.473 | 3,384 | 9.95 | 0.0021 |
The mean cervical lateral flexion was 79.8° ± 15.1° (range 57°–130°). Cervical lateral flexion most closely correlated with a combination of age (P = 0.02, r = −0.24) and the ratio of circumference/length (P < 0.0001, r = −0.39) (Table 1). When the variables were considered together, 20% (r2 = 0.2) of the total variance observed with lateral flexion could be accounted for (P < 0.0001) (Table 3).
Table 3.
Summary of statistical data for lateral flexion
| Source | Degrees of freedom | Sum of squares | Mean square | F value | P > F |
|---|---|---|---|---|---|
| Model | 2 | 4,525 | 2,263 | 12.13 | <0.0001 |
| Error | 97 | 18,097 | 186.57 | ||
| Corr. Total | 99 | 22,623 |
| Variable | Parameter estimate | Standard error | Type II SS | F value | P > F |
|---|---|---|---|---|---|
| Intercept | 140.24 | 12.4 | 23,856 | 127.87 | <0.0001 |
| Age | −0.624 | 0.266 | 1,026 | 5.5 | 0.0211 |
| CdivL | −17.78 | 4.25 | 3,259 | 17.47 | >0.0001 |
The mean cervical rotation was 131° ± 15.6° (range 100°–172°). Lateral rotation most closely correlated with circumference alone with no other significant contributor to the regression model (Table 1). Taking the single variable, circumference, 15% (r2 = 0.146) of the variance observed with lateral rotation could be explained (P < 0.0001) (Table 4).
Table 4.
Summary of statistical data for rotation
| Source | Degrees of freedom | Sum of squares | Mean square | F value | P > F |
|---|---|---|---|---|---|
| Model | 1 | 3,497 | 3,497 | 16.74 | <0.0001 |
| Error | 98 | 20,474 | 208.92 | ||
| Corr. Total | 99 | 23,972 |
| Variable | Parameter estimate | Standard error | Type II SS | F value | P > F |
|---|---|---|---|---|---|
| Intercept | 185.66 | 13.5 | 39,494 | 189.04 | <0.0001 |
| Circumf. | −1.52 | 0.371 | 3,497 | 16.74 | <0.0001 |
A summary of cervical spine range of motion elaborated using the CROM goniometer, the handheld goniometer and chin-chest distance measurements in 100 healthy individuals is illustrated in Table 5.
Table 5.
Cervical ROM of 100 healthy individuals using the CROM groniometer (in degree)
| Movement | ROM (mean, SD, range) | ROM (mean, SD, range) | Distance (in cm) (mean, SD, range) |
|---|---|---|---|
| CROM goniometer | Handheld goniometer | Chin-chest distance | |
| Flexion-extension | 125 ± 19.3, 61–166 | 121.8 ± 29.8, 56–174 | 17.1 ± 2.58, 10.5–27.5 |
| Lateral flexion | 79.8 ± 15.1, 57–130 | 78.2 ± 41.9, 48–140 | |
| Rotation | 131 ± 15.6, 100–172 | 126.0 ± 51.7, 80–174 |
Reliablilty of the handheld goniometer and chin-sternal distance
The correlation coefficients comparing measurements of CROM taken with a handheld goniometer and tape measure with those taken with a CROM goniometer are displayed in Table 6. The acceptable levels for reliability have been determined by previous authors [25] as 0.90–0.99, high reliability; 0.80–0.89, good reliability; 0.70–0.79, fair reliability and 0.69 and below, poor reliability. Utilising the CROM goniometer as a validated measurement tool the handheld uniplanar goniometer was a “fairly reliable” tool for assessing sagittal CROM and lateral flexion and “poorly reliable” for rotation. Similarly, in our hands, the use of chin-sternal distance measured with a tape measure was “poorly reliable” in the sagittal plane.
Table 6.
Correlation coefficients comparing CROM measurements of handheld goniometer and tape measure against those taken with a CROM goniometer
| Pearson correlation coefficient | P | |
|---|---|---|
| Rotation (CROM vs. handheld) | 0.59 | <0.0001 |
| Sagittal AROM (CROM vs. handheld) | 0.78 | <0.0001 |
| Lateral flexion (CROM vs. handheld) | 0.78 | <0.0001 |
| Sagittal AROM (CROM vs. tape) | 0.42 | <0.0001 |
Discussion
When assessing the neck and cervical spine, knowledge of an individual’s expected cervical range of motion is useful. Physiological standards exist for the age-related CROM in normals [6, 10]. However, this study is the first to investigate the relationship between neck dimension and neck mobility. Besides, we investigated the reliability of commonly used techniques in the clinical setting for the assessment of CROM as compared to a more sophisticated, but increasingly accurate measuring device.
Our study population is comparable in terms of measured neck ROM with those enlisted in previous studies [1, 11, 23]. We expected to observe a reduction in the ROM measured in the three planes when comparing “long, thin” necks with “short, fat” necks. This hypothesis was only borne out by lateral flexion whereas sagittal CROM and rotation are more closely related to circumference alone, i.e. thick necks. Utilising the statistically significant linear regression models (Table 1) in conjunction with our observations of neck dimension the variation in expected neck mobility across our study population may be calculated. We may expect to see a 35° variation in lateral flexion and a 27° variation in both rotation and sagittal ROM due to neck dimension variability. These figures compare favourably to the variation in range of movement described when considering advanced age or gender [6, 11, 23]. These variations may also help to explain the inconsistent findings where gender has been assessed previously.
Utilising the CROM goniometer as a validated measurement tool [5, 12, 16, 17], we found that the handheld uniplanar goniometer is a “fairly reliable” tool for assessing sagittal ROM and lateral flexion and “poorly reliable” for lateral rotation. Similarly, in our hands, the use of chin-sternal distance measured with a tape measure is “poorly reliable” in the functional assessment of the cervical spine. Despite the use of clearly defined anatomical landmarks in this study the handheld goniometer could not respond to the changing centres of rotation found in the multisegmental cervical spine. Additionally, the CROM goniometer leaves the assessors hands free to control secondary movement in the shoulders or trunk. The chin-sternal distance is simply too insensitive a tool for meaningful measurements. Hence, studies that use clinically assessed cervical range of motion as an outcome factor using a simple handheld goniometer or even just assessing chin-sternal distance should be interpreted with caution.
In addition, the assessment of cervical range of motion is incomplete without giving consideration to neck dimension. Examination of a larger subject group of healthy individuals with a wider range of ages should be undertaken to establish more accurate normal range of motion charts for use in both clinical or research settings.
A handheld goniometer should be considered as no more than a useful screening tool for the approximate measurement of sagittal ROM and lateral flexion (but not rotation) where defined anatomical landmarks are used. Measurement of chin-sternal distance has little role if an accurate assessment of CROM is desired. For comparison of similar cases in clinical studies that concern functional outcome and motion as a significant outcome marker, a validated measurement tool with increased accuracy should be applied.
Acknowledgment
Dr Peter Williams, Department of Mathematics, Surrey University, Guildford.
References
- 1.Alaranta H, Hurri H, Heliovaara M, Soukks A, Harju R. Flexibility of the spine: normative values of goniometric and tape measurements. Scand J Rehabil Med. 1994;24:147–154. [PubMed] [Google Scholar]
- 2.Antonaci F, Ghirmai S, Bono G, Nappi G. Current methods for cervical spine movement evaluation: a review. Clin Exp Rheumatol. 2000;18:S45–S52. [PubMed] [Google Scholar]
- 3.Armstrong B, McNair P, Taylor D. Head and neck position sense. Sports Med. 2008;38:101–117. doi: 10.2165/00007256-200838020-00002. [DOI] [PubMed] [Google Scholar]
- 4.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine. 1994;19:1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Capuano-Pucci D, Rheault W, Aulai J, Bracke M, Day R, Pastrick M. Intratester and intertester reliability of the cervical range of motion device. Arch Phys Med Rehabil. 1991;72:338–340. [PubMed] [Google Scholar]
- 6.Castro WH, Sautmann A, Schilgen M, Sautmann M. Noninvasive three-dimensional analysis of cervical spine motion in normal subjects in relation to age and sex. An experimental examination. Spine. 2000;25:443–449. doi: 10.1097/00007632-200002150-00009. [DOI] [PubMed] [Google Scholar]
- 7.Chen J, Solinger A, Poncett F, Lantz C. Meta-analysis of normative cervical motion. Spine. 1999;24:1571–1578. doi: 10.1097/00007632-199908010-00011. [DOI] [PubMed] [Google Scholar]
- 8.Christensen H, Nilsson N. The ability to reproduce the neutral zero position of the head. J Manipulative Physiol Ther. 1999;22:26–28. doi: 10.1016/S0161-4754(99)70102-8. [DOI] [PubMed] [Google Scholar]
- 9.Cote P, Cassidy JD, Carroll L. The factors associated with neck pain and its related disability in the Saskatechewan population. Spine. 2000;25:1109–1117. doi: 10.1097/00007632-200005010-00012. [DOI] [PubMed] [Google Scholar]
- 10.Demaille-Wlodyka S, Chiquet C, Lavaste J-F, Skalli W, Revel M, Poiraudaeau Cervical range of motion and cephalic kinesthesis—ultrasonographic analysis by age and sex. Spine. 2007;32:E254–E261. doi: 10.1097/01.brs.0000259919.82461.57. [DOI] [PubMed] [Google Scholar]
- 11.Feipel V, Rondelet B, Le Pallec J-P, Rooze M. Normal global motion of the cervical spine: an electrogoniometric study. Clin Biomech (Bristol, Avon) 1999;14:462–470. doi: 10.1016/S0268-0033(98)90098-5. [DOI] [PubMed] [Google Scholar]
- 12.Hole DE, Cook JM, Bolton JE. Reliability and concurrent validity of two instruments for measuring cervical range of motion: effects of age and gender. Man Ther. 1995;1:36–42. doi: 10.1054/math.1995.0248. [DOI] [PubMed] [Google Scholar]
- 13.Jordan K. Assessment of published reliability studies for cervical spine range-of-motion measurement tools. J Manipulative Physiol Ther. 2000;23:180–195. doi: 10.1016/S0161-4754(00)90248-3. [DOI] [PubMed] [Google Scholar]
- 14.Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, Staehelin Jensen T. Headache, neck pain, and neck mobility after acute whiplash injury: a prospective study. Radiologic, and psychosocial findings. Spine. 2001;26(11):1246–1251. doi: 10.1097/00007632-200106010-00014. [DOI] [PubMed] [Google Scholar]
- 15.Makela M, Heliovaara M, Sievers K, Impivaara O, Knekt P, Aromaa A. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991;134:1356–1367. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 16.Nilsson N. Measuring passive cervical motion: a study of reliability. J Manipulative Physiol Ther. 1995;18:293–297. [PubMed] [Google Scholar]
- 17.Nilsson N, Christinse HW, Hartvigsen J. The interexaminer reliability of measuring passive cervical range of motion, revisited. J Manipulative Physiol Ther. 1996;19:302–305. [PubMed] [Google Scholar]
- 18.Platzer P, Thalhammer G, Ostermann R, Wieland R, Vecsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32:1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 19.Radonov BP, Dvorak J. Impaired cognitive functioning after whiplash injury of the cervical spine. Spine. 1996;21:392–397. doi: 10.1097/00007632-199602010-00029. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E. Scientific monograph of the Quebec task force on whiplash-associated disorders: redefining “whiplash” and its management. Spine. 1995;20:S1–S73. [PubMed] [Google Scholar]
- 21.Squires B, Gargan MF, Bannister GC. Soft tissue injuries of the cervical spine 15 year follow up. J Bone Joint Surg Br. 1996;78-B:955–957. doi: 10.1302/0301-620X78B6.1267. [DOI] [PubMed] [Google Scholar]
- 22.Tousignant M, Bellefeuille L, O’Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension. Spine. 2000;25:324–330. doi: 10.1097/00007632-200002010-00011. [DOI] [PubMed] [Google Scholar]
- 23.Trott P, Pearcy M, Ruston S, Fulton I, Brien C. Three-dimensional analysis of active cervical: the effect of age and gender. Clin Biomech (Bristol, Avon) 1996;11:201–206. doi: 10.1016/0268-0033(95)00072-0. [DOI] [PubMed] [Google Scholar]
- 24.Webb R, Brammah T, Lunt M, urwin M, Allison T, Symmons D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine. 2003;28:1195–1202. doi: 10.1097/00007632-200306010-00021. [DOI] [PubMed] [Google Scholar]
- 25.Youdas J, Garrett T, Suman V, Bogard C, Hallman H, Carey J. Normal range of motion of the cervical spine: an initial goniometric study. Phys Ther. 1992;72:770–779. doi: 10.1093/ptj/72.11.770. [DOI] [PubMed] [Google Scholar]