Abstract
The clinical outcome of patients with symptomatic lumbar spinal stenosis (LSS) was assessed during a follow-up period of 2 years after X-Stop implantation. The X-Stop is the most commonly used interspinous distraction device in patients with neurogenic intermittent claudication due to LSS. Between 2003 and 2007, more than 1,000 patients were examined in our centre with symptoms of intermittent claudication due to spinal stenosis. Between February 2003 and June 2007, in 175 of these patients an X-Stop device was implanted in one or two levels. Patients were clinically evaluated regularly during a follow-up period of up to 4 years using the VAS (leg pain) score and the Oswestry disability index. The mean VAS (leg pain) score in these 175 patients was reduced from 61.2% preoperatively to 39.0% at the first clincal follow-up examination at 6 weeks postoperatively. The mean VAS score at 24 months postoperatively was 39.0%. Oswestry score was 32.6% preoperatively, 22.7% at 6 weeks, and 20.3% at 24 months postoperatively on average. In eight out of the implanted 175 patients, the X-Stop had to be removed and a microsurgical decompression had to be performed because of unsatisfactory effect of the interspinous distraction device. Our single-centre results indicate not only a satisfactory short-term, but also a good long-term effect during a follow-up period of 2 years. Functional MRI examinations provide helpful, positional-dependent preoperative information. More than any radiological feature, the typical clinical picture of positional-dependent claudication with a relief of symptoms during flexion is the most important factor for appropriate patient selection. The interspinous device does not replace microsurgical decompression in patients with massive stenosis and continuous claudication, but offers a save, effective and less invasive alternative in selected patients with spinal stenosis. Concerning the operative technique, a minimally invasive implantation with preservation of the interspinous ligament is appropriate. Functional (upright-) MRI examinations were able to demonstrate the positional-dependent stenosis. If available, fMRI represents the most helpful radiologic examination in assessing the outcome of interspinous spacer implantation.
Keywords: X-Stop, Lumbar spinal stenosis (LSS), Upright MRI, Interspinous process decompression
Introduction
Lumbar spinal stenosis (LSS) is the most common indication for lumbar spinal surgery in the elderly population. A combination of disc degeneration, bulging of the annulus, facet joint hypertrophy [3] and thickening of the ligamentum flavum [1, 5] contribute to narrowing of the spinal canal and/or lateral foraminal recesses.
Symptoms are typically exacerbated on extension of the spine, e.g. on standing or walking when the canal is further narrowed, and alleviated on flexion [3].
The X-Stop is an interspinous decompression device that has already been evaluated for the management of neurogenic intermittent claudication (NIC) secondary to LSS [8–11, 13, 14].
The device has specific European CE Mark for the treatment of LSS with NIC, facet syndrome, spondylolisthesis (to Grade 1) with NIC, ‘kissing’ spine, axial load induced back pain, degenerative disc syndrome and unloading of a disc adjacent to a lumbar fusion procedure. The product has FDA approval for use in the USA.
Here we present a single-centre study experience with 184 X-Stop implantations in 175 patients.
Methods
Between 2003 and 2007, more than 1,000 patients were examined in our centre with symptoms of intermittent claudication due to spinal stenosis. Most of these patients were treated conservatively with medication (NSAP, Cortisol), physiotherapy and epidural/periradicular injections (group A). In 326 patients with lumbar stenosis a microsurgical decompression operation was performed (group B). In these patients a severe mono/bisegmental stenosis was present with permanent and markedly reduced walking distance. Patients in group B may report an increase of symptoms in extension, but with flexion of the lumbar spine the pain did not go away completely. When claudication symptoms occurred in both legs, a bilateral decompression was performed via a unilateral approach, using an ipsi-contralateral, “undercutting” technique. If symptoms were present in one leg, a unilateral approach was performed. In the third group of patients (group C), the leg pain disappeared completely during flexion of the lumbar spine. Some of these patients were able to ride the bike (spine flexed) for miles while they were not able to walk “around the corner”. Positional claudication with relief of symptoms in flexion was the inclusion criteria for spacer implantation, independent of the severity and the shape (central/lateral) of the stenosis.
Between February 2003 and June 2007, in 175 of these patients an X-Stop device was implanted in one or two levels. Patients were clinically evaluated regularly during a follow-up period of up to 2 years using the VAS (leg pain) score and the Oswestry disability index.
All patients were diagnosed with NIC due to LSS at 1 or 2 levels confirmed by MRI. In some [5] patients a functional (Upright-) MRI examination in flexion and extension was performed pre- and postoperatively. Patients had symptoms of radiating leg/buttock/groin pain, with or without back pain. Only patients without previous fusion, laminectomy and <grade I spondylolisthesis were included. The most important inclusion criterium was a reproductible alleviation of symptoms on flexion and exacerbation of symptoms in extension of the lumbar spine.
It is recommended that patients undergo at least 6 months of conservative management before being considered for interspinous spacer (ISS) implantation. The device is contraindicated in patients with titanium allergy, severe osteoporosis, spondylolisthesis (more than Grade 1), cauda equina syndrome, severe scoliosis (Cobb angle > 25°), an ankylosed segment at the affected level(s), acute fracture of the spinous processes or pars interarticularis, cauda equina syndrome, and systemic infection at the time of surgery.
Surgical technique
The patient is positioned on a radiolucent table in the prone position with hips and knees flexed. There must be sufficient flexion of the lumbar spine to open the interspinous space for implant insertion.
The stenosed target level is confirmed by fluoroscopy and marked. The surgeon stands on the left side of the patient and the patient is prepped and draped. A 4-cm incision is made in the midline with one-third of the incision length in the cranial direction above the symptomatic level and two-thirds in the caudal direction to allow for the concave structure of the spinous process. The supraspinous ligament is exposed and a 2–3-cm incision is made approximately 1.0 cm on either side through the fascia of the spinous process. The supraspinous ligament is preserved. The paraspinal muscles are then cleared off the processes and lamina by blunt dissection with care to avoid dissection through the muscle.
The small dilator is introduced parallel to the vertebral spine with the tip in the cranial direction on the right side of the spinous process, rotated medially through 90° and advanced through the interspinous ligament from right to left to create a 1–5-mm pilot hole or perforation. The perforation in the interspinous space should be as anterior as possible to minimise the risk of dislodgement and to maximise flexion of the vertebral bodies. In some patients, hypertrophied facet joints project posteriorly to the lamina and limit the available space for the device, and in these circumstances the excess facet tissue should be excised.
It is essential to avoid over-distraction which can result in spinous process fracture or the insertion of an implant which is too large, leading to kyphosis [12]. The aim of implantation is the recreation of the normal interspinous distance and normal spinal alignment.
The dilator is removed and the tips of the sizing distractor are introduced to the pilot hole from the right side and brought through the interspinous ligament until they are visualised on the left side. After a few seconds it should be released and tension in the ligament relaxed. This cycle of tension and relaxation should be repeated two or three times. Once optimal distraction has been achieved the locking nut is adjusted to fix the tips and the appropriate size of device is determined by the analogue indicator on the handles. Fluoroscopy should be repeated to show the amount of distraction; one should not go over a parallel outlining of the endplates [12].
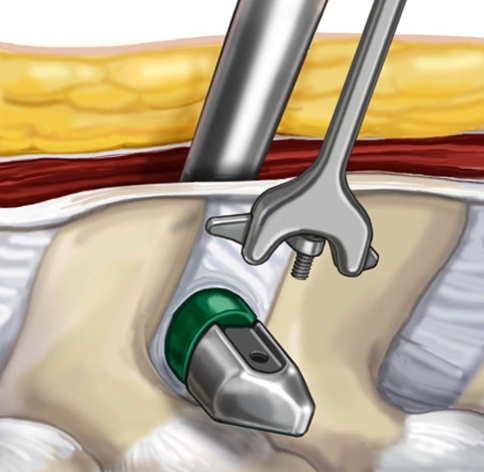
Once the spacer is mounted it is introduced to the right side of the spinous process. The implant is guided through the perforation (Fig. 1), and the surgeon should palpate for the spacer with the left index finger as it passes through the interspinous ligament on the left side. As the distractor device has been removed, it may be necessary to increase flexion of the hips to open the interspinous space to allow easier insertion. The implant is directed through the pilot hole with consideration of the oval shape of the X-Stop and the concavity of the adjacent spinous processes. Once the spacer is in place, the insertion instrument should remain attached as this will assist in the attachment of the wing. It is important to ensure that there is no tissue overlying the threaded hole of the spacer device before attempting to secure the wing, otherwise the screw will not engage. The wing is then engaged with the screw hole and secured with a torque limiting hexagonal screw driver. At the end of the procedure the correct placement of the implant(s) should be confirmed by fluoroscopy. The wound is closed in the standard manner and typically a drain is not required (Fig. 2).
Fig. 1.
Implantation of the X-Stop device
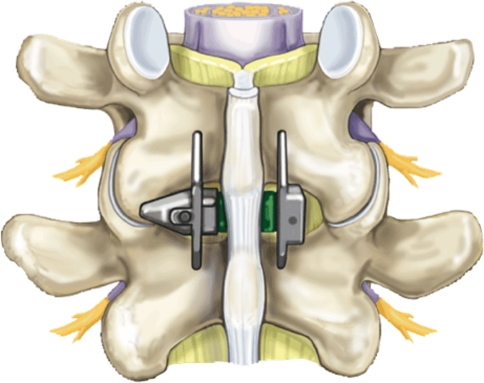
Fig. 2.
X-Stop in place at the affected level (L 4/5 in most cases). The implant should be positioned as anterior as possible. Please note that the supraspinous ligament is preserved throughout the procedure
Statistical analysis
The clinical outcome was rated using self-assessment questionnaires at the following time points: preoperative, postoperative at 6 weeks, 6 months, 12 months and 24 months. Linear mixed models were used to estimate differences in VAS (resp ODI) before and after operation. Model with random intercept and random effect for time was used. This allows time slopes and intercepts to vary across observations and, thus, observation-specific regression lines to be fitted. In VAS (leg pain) analysis covariates included in the model were: time of measurement, indicator for baseline/follow-up measurement, age by operation, sex, level of implantation and implant size (10–16 mm). Model with random intercept and random effect for time of measurement was used. In ODI analysis covariates included in the model were: time of measurement, indicator for baseline/follow-up measurement, sex, interaction of sex and indicator for baseline/follow-up measurement, age by operation, level of implantation and implant size. Statistical analyses were performed with SPSS 11.0 (SPSS, Chicago, IL, USA). A P value <0.05 was considered significant.
Results
A total of 175 patients with lumbar stenosis and positional-dependent neurologic claudication were included in the study. The age distribution was 41–91 years and the mean age at implantation was 69.4 years. 108 male and 67 female patients were operated. In most of the cases (112 out of 175 patients), the L4/5 level was affected. In 47 patients L3/4, in 13 patients L2/3, in 2 patients the L1/2 level, and in 6 patients the L5/S1 level was implanted. The X-Stop was implanted bisegmentally in nine patients. The size of the implanted X-Stop was 10 mm in 10, 12 mm in 37, 14 mm in 103, 16 mm in 34 cases.
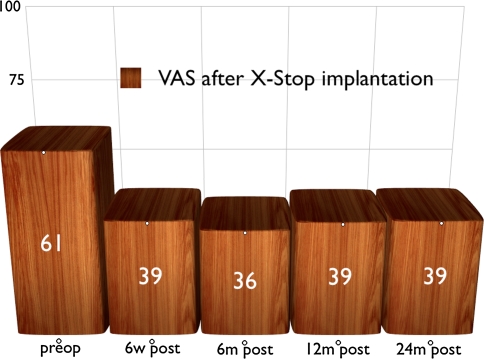
Patients were clinically evaluated regularly during a follow-up period of 2 years using the VAS (leg pain) score and the Oswestry disability index. VAS was 61.1 preoperatively on average (range 20–100, SD: 29.8) and fell to 39.0 (0–100, SD: 39.0) at 6 weeks postoperatively (Table 1; Fig. 3). The VAS (leg pain) decrease of 22.1 (range 20–100, SD: 30.0) on average preoperative to postoperative is highly significant (P < 0.005). This effect remained remarkably stable throughout the follow-up period of 2 years. Mean VAS at 6 months postoperative was 35.8 (0–100, SD: 29.6), mean VAS at 12 months postoperative was 38.6 (0–100, SD: 30.6) and mean VAS at 24 months postoperative was 39.0 (0–75, SD: 28.3). Interestingly, male patients had a significantly lower VAS (leg pain) both before and after the operation.
Table 1.
Visual analogue scale measurements (VAS) in the long-term follow-up after X-Stop implantation
| Time point | Mean | Std. Dev. | Range |
|---|---|---|---|
| Preoperative | 61.163 | 29.799 | 20–100 |
| 6 weeks po. | 38.965 | 30.040 | 0–100 |
| 6 months po. | 35.854 | 29.616 | 0–100 |
| 12 months po. | 38.571 | 30.659 | 0–100 |
| 24 months po. | 39.000 | 28.326 | 0–75 |
Fig. 3.
Visual analogue scale in the long-term follow-up after X-Stop implantation
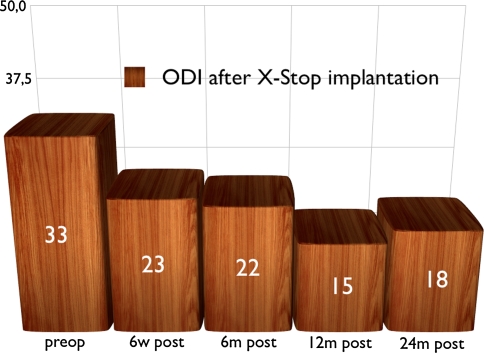
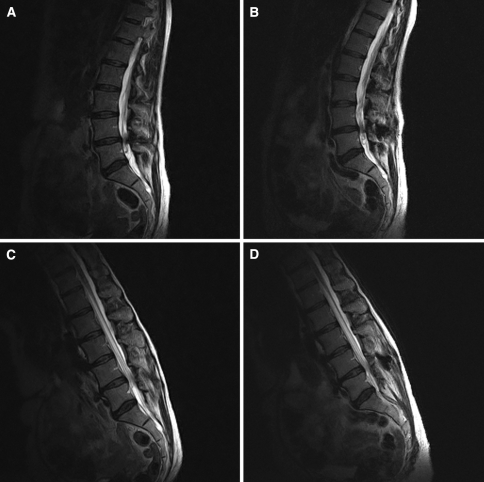
ODI measurements were preoperatively 32.6 on average (8–80, SD: 16.0) and fell to 22.7 on average (0–85, SD: 15.6) at 6 weeks postoperatively. Mean ODI score at 6 months postoperative was 21.5 (0–66, SD: 17.4), mean ODI score at 12 months postoperative was 15.3 (0–44, SD: 13.7) and mean ODI score at 24 months postoperative was 20.3 (0–42, SD: 17.5) (Table 2; Fig. 4). Furthermore, males had initially a slightly lower mean ODI score than females. However, the significant gender difference in ODI was detectable only preoperatively and was not present in the postoperative measurements. No statistical difference of pre- and postoperative VAS (leg pain) and ODI numbers were found when comparing the L5/S1 patients with patients implanted in other levels (mostly L4/5). In three out of five patients, a marked improvement of the “soft” stenosis could be demonstrated postoperatively in the functional (flexion/extension) MRI studies (Fig. 5). Changes were visible only in the saggital sections; the axial scans were performed in the neutral sitting position and did not show a change pre/postoperatively. Patients with an improvement of the diameter of the lumbar channel also reported a satisfactory clinical effect after spacer implantation. In two patients, no significant effect could be demonstrated radiologically, although also these patients reported some clinical improvement postoperatively.
Table 2.
Oswestry disability index (ODI) measurements in the long-term follow-up after X-Stop implantation
| Time point | Mean | Std. Dev. | Range |
|---|---|---|---|
| Preoperative | 32.600 | 16.007 | 8–80 |
| 6 weeks po. | 22.745 | 15.646 | 0–85 |
| 6 months po. | 21.463 | 17.415 | 0–66 |
| 12 months po. | 15.263 | 13.649 | 0–44 |
| 24 months po. | 20.333 | 17.501 | 0–42 |
Fig. 4.
Oswestry disability index (ODI) in the long-term follow-up after X-Stop implantation
Fig. 5.
Functional Upright MRI in a 71-year-old female patient with monosegmental lumbar stenosis at L4/5 and position-dependent neurologic claudication (exacerbation in extension and relief in flexion). Preoperative sagittal scans in extension (a) and flexion (c) were shown with the corresponding postoperative fMRI scans (b, d). The position-dependent “soft” lumbar stenosis in extension is reduced after implantation of the X-Stop. No change is seen in the flexion scans, where the patient is asymptomatic. Radiologic findings corresponded to the satisfactory postoperative outcome with a markedly increased walking distance and relief of symptoms
In summary, both VAS (leg pain) and ODI are reduced postoperatively, and this effect remained quite stable throughout the follow-up period of 2 years. In 8 out of the implanted 175 patients, the X-Stop had to be removed and a microsurgical decompression had to be performed because of unsatisfactory effect of the interspinous distraction device.
Discussion
Conservative treatment of LSS includes physiotherapy, analgesia and steroid injections. Historically, failure of conservative measures was an indication for surgical decompression by laminectomy with or without fusion, often with the use of pedicle screws and anterior interbody fusion. An analysis of 74 published studies found a success rate from 26 to 100% [4–6, 14]. Microsurgical decompression is indicated in patients with severe stenosis and leg pain that persists also in flexion of the spine.
In positional-dependent claudication, ISS may represent an alternative to open surgical decompression in selected cases. ISS apply distraction between the spinous processes of the degenerated segment, thereby unloading the posterior annulus fibrosus and the facet joints. ISS limit or block extension in the functional spinal unit (FSU) which may reduce compression of the spinal canal and the foramina. ISS unfold and stretch the ligamentum flavum which can enlarge the spinal canal by reducing “soft” compression [8].
There were no complications associated with the use of the X-Stop in our patients. Other authors have reported spinous process fractures, usually either associated with poor bone stock (osteoporosis) or over-distraction.
A prospective randomised multi-centre study has been carried out, and the data for 1-year and 2-year clinical results have been published by Zucherman et al. [17, 18]. Patients were randomised to conservative management with epidural injection (91 patients) or X-Stop insertion (100 patients). At 1 year, clinically significant improvement was achieved in 59% of the X-Stop group compared with 12% of the conservative group. Seventy-eight percent were satisfied with the outcome of their surgery. At 2 years, 73.1% of patients were satisfied with the outcome of their surgery compared with 35.9% in the non-operative group. Symptom severity scores improved by 45.4% over the mean baseline and physical function scores improved in 44.3% of patients. In a recent evaluation of the first 18 patients in the X-Stop group who had returned for 4-year follow-up, 78% of patients had a successful outcome according to the ODI. [7]. The results reported here demonstrate a similar effect in the largest European single-centre study.
The device is implanted between the spinous processes of the affected level(s) and restricts extension at that level but allows full flexion, axial rotation and lateral flexion [5]. Because the device does not require fixation to bone, or removal of bone or soft tissues, there is minimal damage to soft tissue structures. Its effects are reversible if removal is required (secondary operative decompression with or without removal of the X-Stop was performed successfully in 8 out of 175 patients included in this study). Siddiqui et al. [11] observed a 26% increase of the cross-sectional area of the dural sac after X-Stop implantation. A pressure reduction at the facet joints of 55% was documented using the X-Stop device [13, 15]. Also a decrease of intradiscal pressure of up to 63% due to a restoration of disc height was reported [11]. Swanson et al. [13] also speculate that this may be stimulating some disc regeneration.
Cavusoglu et al. [1, 2] in 2007 presented their results after unilateral laminectomy for bilateral decompression in LSS. In a prospective study 50 patients with 98 levels were assessed. Surgical decompression resulted in a dramatic reduction in VAS from 69.2 (10.4) mean preoperative to 24.0 (07.9) at 3 months and 21.6 (0.81) at 24 months postoperatively. Mean ODI scores fell from 31.1 (9.27) preoperative to 14.22 (9.88) at 3 months and 14.02 (9.27) at 24 months postoperatively. Nevertheless, surgical decompression studies were not able to show a statistical relationship between the extent of decompression and the clinical outcome [2]. The clinical effect of open surgical decompression and spacer implantation is comparable and proves the benefit for selected patients with lumbar stenosis. Nevertheless, the effect on VAS and ODI in our spacer study is not so pronounced when compared with the open decompression studies in the literature (23 point VAS reduction in our study when compared to 45 points VAS reduction in the Cavusoglu study). This may be in part attributed to the patients who did not benefit from spacer implantation and the eight patients in whom the spacer was removed and a secondary open microsurgical decompression was performed. On the other hand, there were no surgical complications in the spacer group (dural tears, etc.) and the operative time was much shorter when compared to the open decompression group. This may be important in older instable patients with internistic problems. Finally, in any case the spacer implantation is a fully reversible operation.
The overall VAS (leg pain) level of male patients that were included in our study was significantly lower on all time points pre- and postoperatively when compared to the female patients. This suggests a different subjective pain perception in male and female patients in our study group. Outcome of patients implanted at the L5/S1 level did not differ significantly from patients implanted at other levels of the lumbar spine. In addition to the inclusion criteria mentioned above, for a L5/S1 implantation, a prominent spinous process of S1 has to be present to prevent implant migration. The preoperative evaluation with plain lateral X-rays to document the presence and anatomy of the S1 spinous process is mandatory.
Upright MRI examinations have proven to be of diagnostic value in different positional-dependent problems of the lumbar spine. Zamani et al. [16] found an increased disc bulge in 27% of discs (40% of those with desiccation) with extension. Central canal size (50%) and foraminal size (27%) decreased with extension, especially at levels with disc desiccation. Images obtained with our open-configuration MR unit were diagnostically adequate, although of inferior resolution compared with those obtained with a conventional unit. Our preliminary results with upright positional MRI in ISS patients show the feasibility of obtaining diagnostic images with additional functional information of the erect lumbar spine with flexion and extension.
Conclusions
Implantation of the X-Stop device is a minimally invasive, effective and safe procedure. Improvement in symptom severity and physical functioning was maintained throughout the follow-up period of 2 years. Patients improved significantly (P < 0.001) on all outcome measurements at all time points when compared to the preoperative status. The results of this study are consistent with those found in the U.S. randomised study in patients with moderately severe lumbar stenosis. The X-Stop offers an alternative to both conservative and more invasive surgical therapies in selected cases with functional NIC due to LSS.
More than any radiological feature, the typical clinical picture of positional-dependent claudication with a relief of symptoms during flexion is the most important factor for appropriate patient selection. In contrast to other publication, we also see an indication for X-Stop implantation at the L5/S1 level in selected cases. The interspinous device does not replace microsurgical decompression in patients with massive stenosis and continuous claudication, but offers a safe, effective and less invasive alternative in selected patients with spinal stenosis. Concerning the operative technique, a minimally invasive implantation with ventral placement and preservation of the interspinous ligament is appropriate. Functional (upright-) MRI examinations are able to demonstrate the positional-dependent stenosis. If available, fMRI represents the most helpful radiologic examination in assessing the outcome of ISS implantation. In our experience, it is not helpful to define radiologic criteria for patient selection, especially if no functional MRI examinations were available. The positional claudication with relief of symptoms in flexion was the inclusion criteria for the study, independent of the severity and the shape (central/lateral) of the stenosis.
Acknowledgments
Dr. Pascal Niggemann, upright MRI Centre Cologne for multi-position MRI scans.
References
- 1.Cavusoglu H, Kaya RA, Türkmenoglu ON, Tuncer C, Colak I, Aydin Y. Midterm outcome after unilateral approach for bilateral decompression of lumbar spine stenosis: 5-year prospective study. Eur Spine J. 2007;16(12):2133–2142. doi: 10.1007/s00586-007-0471-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cavusoglu H, Türkmenoglu O, Kaya RA, Tuncer C, Colak I, Sahni Y, Aydin Y. Efficacy of unilateral laminectomy for bilateral decompression in lumbar spinal stenosis. Turk Neurosurg. 2007;17(2):100–108. [PubMed] [Google Scholar]
- 3.Chung SS, Lee CS, Kim SH. Effect of low back posture on the morphology of the spinal canal. Skeletal Radiol. 2000;29:217–223. doi: 10.1007/s002560050596. [DOI] [PubMed] [Google Scholar]
- 4.Dunlop RB, Adams MA, Hutton WC. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br. 1984;66:706–710. doi: 10.1302/0301-620X.66B5.6501365. [DOI] [PubMed] [Google Scholar]
- 5.Johnsson KE, Rosen I, Uden A. The natural course of lumbar spinal stenosis. Clin Orthop Relat Res. 1992;279:82–86. [PubMed] [Google Scholar]
- 6.Katz JN, Lipson SJ, Chang LC, Levine SA, Fossel AH, Liang MH (1996) Seven to 10-year outocme after decompressive surgery for degenerative lumbar spinal stenosis. Spine 21(1):92–98 [DOI] [PubMed]
- 7.Kondrashov DG, Hannibal M, Hsu KY, Zucherman JF. Interspinous process decompression with the XSTOP® device for lumbar spinal stenosis: a 4-year follow-up study. J Spinal Disord Tech. 2006;19:323–327. doi: 10.1097/01.bsd.0000211294.67508.3b. [DOI] [PubMed] [Google Scholar]
- 8.Lindsay DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby S. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003;28(19):2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 9.Richards JC, Majumdar S, Lindsay DP, Beaupre GS, Yerby SA. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine. 2005;30(7):744–749. doi: 10.1097/01.brs.0000157483.28505.e3. [DOI] [PubMed] [Google Scholar]
- 10.Shonauer C, Boccheti A, Barbagallo A, Albanese V, Moraci A. Positioning on the surgical table. Eur Spine J. 2004;13(S1):S50–S55. doi: 10.1007/s00586-004-0728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siddiqui M, Nicol M, Karadimas E, Smith F, Wardlaw D. The positional magnetic resonance imaging changes in the lumbar spine following insertion of a novel interspinous process distraction device. Spine. 2005;30(23):2677–2682. doi: 10.1097/01.brs.0000187878.79676.26. [DOI] [PubMed] [Google Scholar]
- 12.Simons P. Dekompression bei spinaler claudicatio intermittens. Orthopaedie Rheuma. 2006;4:50–53. [Google Scholar]
- 13.Swanson KE, Lindsay DP, Hsu KY, Zucherman JF, Yerby S. The effects of an interspinous implant on intervertebral disc pressures. Spine. 2003;28(1):26–32. doi: 10.1097/00007632-200301010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Turner JA, Ersek M, Herron L. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine. 1992;17:1–8. doi: 10.1097/00007632-199201000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Wiseman CM, Lindsey DP, Frederick AD, Yerby SA. The effect of an interspinous process implant on facet loading during extension. Spine. 2005;30(8):903–907. doi: 10.1097/01.brs.0000158876.51771.f8. [DOI] [PubMed] [Google Scholar]
- 16.Zamani AA, Moriatry T, Hsu L, et al. Functional MRI of the lumbar spine in erect postition in a superconducting open-configurator MR system: preliminary results. J Magn Reson Imaging. 1998;8:1329–1333. doi: 10.1002/jmri.1880080622. [DOI] [PubMed] [Google Scholar]
- 17.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, et al. A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1 year results. Eur Spine J. 2004;13:22–31. doi: 10.1007/s00586-003-0581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, et al. Multicenter, prospective randomized trial evaluating the XSTOP® interspinous process decompression system for the treatment of neurogenic intermittent claudication. Spine. 2005;30(12):1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]