Abstract
The most common cervical abnormality associated with rheumatoid arthritis (RA) is atlantoaxial subluxation, and atlantoaxial transarticular screw fixation has proved to be one of the most reliable, stable fixation techniques for treating atlantoaxial subluxation. Following C1–C2 fixation, however, subaxial subluxation reportedly can bring about neurological deterioration and require secondary operative interventions. Rheumatoid patients appear to have a higher risk, but there has been no systematic comparison between rheumatoid and non-rheumatoid patients. Contributing radiological factors to the subluxation have also not been evaluated. The objective of this study was to evaluate subaxial subluxation after atlantoaxial transarticular screw fixation in patients with and without RA and to find contributing factors. Forty-three patients who submitted to atlantoaxial transarticular screw fixation without any concomitant operation were followed up for more than 1 year. Subaxial subluxation and related radiological factors were evaluated by functional X-ray measurements. Statistical analyses showed that aggravations of subluxation of 2.5 mm or greater were more likely to occur in RA patients than in non-RA patients over an average of 4.2 years of follow-up, and postoperative subluxation occurred in the anterior direction in the upper cervical spine. X-ray evaluations revealed that such patients had a significantly smaller postoperative C2–C7 angle, and that the postoperative AA angle correlated negatively with this. Furthermore, anterior subluxation aggravation was significantly correlated with the perioperative atlantoaxial and C2–C7 angle changes, and these two changes were strongly correlated to each other. In conclusion, after atlantoaxial transarticular screw fixation, rheumatoid patients have a greater risk of developing subaxial subluxations. The increase of the atlantoaxial angel at the operation can lead to a decrease in the C2–C7 angle, followed by anterior subluxation of the upper cervical spine and possibly neurological deterioration.
Keywords: Atlantoaxial transarticular screw fixation, Atlantoaxial subluxation, Subaxial subluxation, Rheumatoid arthritis, Operative complications
Introduction
Rheumatoid arthritis (RA) infamously presents joint inflammation, bone and cartilage destruction and ligament laxity, all of which lead to joint instability. The cervical spine is one of the most frequently affected and the most severely damaged part in RA patients [20]. The resulting neurological impairment can lead to even a shortened life expectancy [14]. The most common cervical abnormality associated with RA is atlantoaxial subluxation, representing two-thirds of rheumatoid cervical subluxations [4], and if evidence of spinal cord compromise exists at the atlantoaxial level on MRI, neurological deterioration requiring surgical intervention is more likely to happen than with subaxial lesions [9]. Therefore, serious consideration should be paid to the treatment of such instabilities, and an operative intervention is frequently inevitable.
Atlantoaxial transarticular screw fixation, first introduced by Magerl and Seemann [13], has proved to be one of the most reliable, stable fixation techniques for treating atlantoaxial subluxation [7, 16]. However, this operation has its own risks, notably one of which is an intraoperative injury to the vertebral artery [17, 18]. Another early complication could be non-union of either the atlantoaxial facets or the posterior bone graft, if combined, and we recently reported that this complication largely depends on the RA status of the patient and the material used for the posterior bone graft fixation [10].
On the other hand, late complications of atlantoaxial transarticular screw fixation have not been fully reported so far. Yoshimoto et al. [23] previously showed that hyperlordotic fixation of C1–C2 would eventually lead to the development of subaxial kyphosis. This was supplemented by a report that constant inclination of C1 and anterior shift of C2 are also associated with subaxial sagittal alignment changes after C1–C2 transarticular screw fixation [15]. While Kraus et al. [12] reported that subaxial subluxation requiring surgery did not develop in patients after C1–C2 fusion compared with those after occipitocervical fusion, there have been a few reports dealing with subaxial cervical spine instability following C1–C2 arthrodesis. Agarwal et al. [1] reported that 3 of 55 patients who had required C1–C2 fusion developed subaxial subluxation and had a second procedure after a mean interval of 9 years. Clarke et al. [3] also showed that 39% of their patients with atlantoaxial subluxation developed non-symptomatic or symptomatic/unstable subaxial subluxations after C1–C2 fusion. Furthermore, while the rigidity of any fixation can presumably affect biomechanical environment on the other levels that can lead to subluxations, only Mukai et al. [15] have reported subaxial subluxation after atlantoaxial transarticular screw fixation. They showed that neurological deterioration recurred in four patients because of the postoperative development of subaxial subluxation but with no details of those patients. So far, how the subaxial subluxastion progresses and what factors contribute to the development after C1–C2 fusions have not fully been analyzed, and, moreover, whether RA status affects the incidence rate remains to be proved.
In this study, we evaluated subaxial subluxation after atlantoaxial articular fixation in a consecutive series of patients who had RA as well as non-RA backgrounds, aiming to find radiological factors that might contribute to the subluxations.
Materials and methods
All of RA patients included in this study fulfilled the revised criteria of American College of Rheumatology [2]. From September 1994 to February 2006, a consecutive series of RA and non-RA patients who had atlantoaxial subluxation and intractable pain or progressive neurological involvement were evaluated medically and radiologically. Of these, 11 patients (7 RA, 4 non-RA) underwent the occipitocervical fixation and 1 (non-RA) did the atlantoaxial fixation combined with subaxial fixation because of, at least, one of the following reasons; substantial vertical and/or subaxial subluxation, irreducible atlantaxial subluxation or osseous fusion between the occiput and the altas. An RA patient received the atlantoaxial fixation only with posterior wiring and strut autograft. In the remaining patients, 56 underwent elective atlantoaxial transarticular screw fixation with a posterior strut autograft, and 12 patients (6 RA, 6 non-RA) went back to their local hospitals or were lost to follow-up within 1 year after the operation. One patient underwent concomitant cervical laminoplasty and was excluded from this study. The remaining 43 patients (33 RA, 10 non-RA) were closely followed up for more than 1 year by functional lateral X-rays and were included in this study. The mean follow-up period was 4.2 years (range 1–11 years and 8 months).
All operations were performed under fluoroscopic guidance. For transarticular screw fixation, the Reunion bone screw system (Surgical Dynamics Inc., Norwalk, CT) or the Universal cannulated screw system (SofamorDanek, Memphis, TN) was used. All types of screw had a diameter of 4 mm. In case of substantial destructive atlantoaxial instability, the Olerud cervical system with an atlas claw was used (NordOpedic AB, Uppsala, Sweden) in two cases. A unicortical iliac bone strut was fixed on C1–C2 supported with morselized bone chips, mostly according to Gallie [6] using a metal wire or cable, or a polyethylene cable (Secure Strand; Surgical Dynamics Inc.). In cases when we used an atlas claw to fix the C1–C2 arches, only bone chips were grafted. The detail of the overall surgical techniques has been described elsewhere [17, 19].
All patients were asked to wear hard or soft collars for 3 months and were closely followed up by clinical examinations and functional X-rays that were performed 3 and 6 months after the operation and every 6 months thereafter. We did not observe any intraoperative complication directly related to the initial atlantoaxial transarticular screw fixation in any of the 43 cases. However, two patients developed substantial subaxial subluxation after certain periods of time (5 years and 1 month, and 6 years and 5 months, respectively) and submitted to an operative correction because of neurological deterioration (Fig. 1). In these cases, the last X-ray dates before the reoperation were defined as the latest follow-up. Two patients developed non-fused C1–C2 with only slight motion between them and were included in this study [10]. Neutral lateral radiographs were taken with the patients standing or sitting in their natural posture before and 3 months after the operation and at the latest follow-up. Flexion-extension radiographs were taken by asking each patient to achieve his or her maximum effort at flexion and extension at the same time. All of the patients’ records and the radiographs were blindly evaluated and measured by the author (H. I.) who was not the responsible operator in this series of operations. The atlantoaxial angle (AA angle) was defined as the angle between an extended line connecting the centres of the anterior and the posterior arches of the atlas (C1) and an extended line connecting the inferior endplate of the axis (C2). The C2–C7 angle was defined as the angle subtended by the lines of the inferior endplate of C2 and the superior endplate of C7 [21]. A vertebral subluxation was measured on the upright lateral radiographs as the anteroposterior distance from the posteroinferior corner of the upper vertebra to the posterosuperior corner of the inferior vertebra on the superior endplate line of the inferior vertebra [21]. A distance of more than 1 mm was recorded and evaluated later. A distance of 2.5 mm or greater was defined as a subluxation, and a change of 2.5 mm or greater between the preoperative and the follow-up distances was defined as an aggravation of a subluxation. Anterior and posterior atlantodental intervals (AADI and PADI, respectively) were also measured. The intraobserver reliability was calculated from three independent measurements and was less than 0.2 mm in distance and 1° or less in angle, respectively. Two patients who had unsuccessful C1–C2 fusion were excluded in the postoperative AA angle measurement. Two patients preoperatively had substantial posterior subluxations whose levels were non-operatively fused at follow-up and were classified as no subluxation, even though it could have meant an anterior correction of the subluxation.
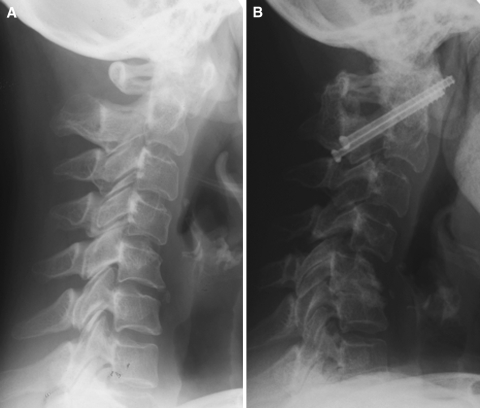
Fig. 1.
a A 64-year-old RA woman who had severe anterior atlantoaxial subluxation underwent the atlantoaxial transarticular screw fixation. b She developed a substantial anterior subluxation in C4–C5 with severe neurological deterioration 6 years and 5 months after the operation
To examine the effect of RA status on the subaxial subluxation rate, we divided the patients into two groups: RA (33 patients) and non-RA (10 patients). We then subdivided them into groups with an anterior, posterior, anteroposterior (a combination of anterior and posterior subluxations), or no subluxation. The non-RA group consisted of four patients with os odontoideum, five with degenerative spondylosis, and one with odointoid fracture. Data are expressed as the mean ± SD. Ratios between groups were evaluated by Fisher’s exact probability or by a 2 × 2 χ2 test. Any difference in the means between two groups was assessed using Mann–Whitney non-parametric U test. Correlation and regression analysis was performed using Spearman’s correlation approach. Significance was set at P < 0.05.
Results
The follow-up periods of the RA and non-RA groups were 4.2 ± 2.4 and 3.7 ± 2.1 years, respectively, which does not yield a statistical difference. First, pre- and postoperative subaxial subluxations were compared between the RA and non-RA groups. Preoperative subluxations were more frequent in the RA group, but the difference was not significant. However, after the operation, the difference became statistically significant (Table 1). Any aggravation of the subluxation was then assessed. It was more likely to happen in RA patients than non-RA patients (Table 2). Substantial subluxation aggravation (3 mm or more) was more likely to happen in the RA (8/33 patients, 9/165 levels) than in the non-RA group (0/10, 0/45), but smaller subluxations between 2 to 2.4 mm occurred similarly in the RA (12/33 patients, 9/165 levels) and in the non-RA group (2/9, 2/45), indicating that RA patients had a greater risk of developing substantial subaxial subluxation after this operation than non-RA patients.
Table 1.
Comparison of the pre- and postoperative subaxial subluxation (slip) between RA and non-RA patients
| n | Preop. | Postop. | |||
|---|---|---|---|---|---|
| Slip | Rate (%) | Slip | Rate (%) | ||
| RA | 33 | 8 | 24.2 | 19 | 57.6* |
| Non-RA | 10 | 1 | 10.0 | 1 | 10.0 |
* P < 0.05
Table 2.
Comparison of the slip aggravation rate in terms of patient numbers and levels, between RA and non-RA patients
| Patient | Level | |||||
|---|---|---|---|---|---|---|
| n | Slip aggravation | Rate (%) | n | Slip aggravation | Rate (%) | |
| RA | 33 | 13 | 39.4* | 165 | 15 | 9.1* |
| Non-RA | 10 | 0 | 0 | 50 | 0 | 0 |
* P < 0.05
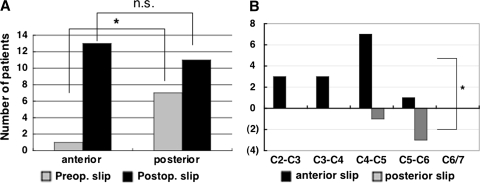
Next, the direction and level of the subluxation was assessed in RA patients. The preoperative subluxation was dominantly in the posterior direction (7/33 patients, 21.2%: 9/165 levels) rather than in the anterior direction (1/33 patients, 3.0%: 1/165 levels, P = 0.023 and 0.010, respectively, Fig. 2a). In contrast, the postoperative subluxation rates were similar between posterior and anterior subluxation directions (13 patients in the anterior vs. 11 in the posterior direction: 15 levels in the anterior vs. 13 in the posterior direction: Fig. 2a). Thus, the aggravation of the subluxation was more likely to happen in the anterior direction (11/33 patients) than in the posterior (4/33, P = 0.040). Evaluation of the subluxation level revealed that an increase of the anterior subluxation was more likely to happen in the upper cervical lesions (P = 0.024; Fig. 2b). Taken together, postoperative subluxation was more likely to occur in the anterior direction in the upper cervical spine after atlantoaxial transarticular fixation in RA patients.
Fig. 2.
a Pre- and post-operative subluxation (slip) in RA. b The level of the increased anterior and posterior slip. * P < 0.05
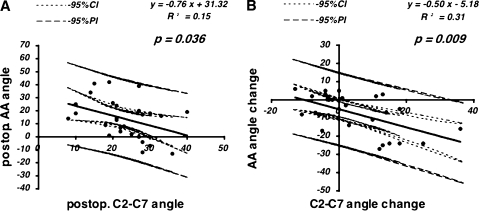
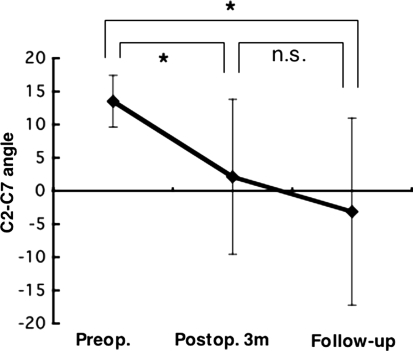
To find any associated factors leading to the subluxation aggravation, preoperative AADI and PADI, and pre- and postoperative AA and C2–C7 angles were evaluated in RA patients. Table 3 shows that the incidence of anterior subluxation aggravation did not have any significant correlation with any of the preoperative AADI, PADI values or with AA, or C2–C7 angle. However, these cases did have significantly smaller postoperative C2–C7 angle and showed a tendency to have a bigger postoperative AA angle. The postoperative AA angle negatively correlated with the postoperative C2–C7 angles (Fig. 3a), although those measured preoperatively did not (data not shown). More importantly, the anterior subluxation aggravation cases had significantly bigger AA and smaller C2–C7 angle changes, respectively (Fig. 4). These two changes strongly correlated with each other (Fig. 3b), indicating that an increase in the AA angle led to a decrease in the C2–C7 angle, probably followed by subaxial subluxation. Indeed, in those patients who had an anterior subaxial subluxation aggravation, the C2–C7 angle significantly decreased in the immediate postoperative period (3 months after operation) without any aggravation of the subluxation but did not significantly change after that time even with the occurrence of the aggravation (Fig. 5). Thus, 67.9% of the total incidence of a decreased C2–C7 angle occurred during the first 3 months after the operation. On the contrary, no correlation was found between the postoperative AA and C2–C7 angles in non-RA group (data not shown).
Table 3.
Differences of preoperative AADI and PADI, and the pre- and postoperative AA and C2–C7 angles between patients with anterior subaxial subluxation (slip) and those with no slip
| Preop | Postop | |||||
|---|---|---|---|---|---|---|
| AADI | PADI | AA angle | C2–C7 angle | AA angle | C2–C7 angle | |
| Ant. slip. aggravation | 10.6 ± 2.4 | 12.0 ± 3.5 | 16.3 ± 10.3 | 13.5 ± 3.9 | 24.8 ± 6.0 | −3.1 ± 14.1* |
| No aggravation | 8.7 ± 3.2 | 12.8 ± 3.3 | 18.2 ± 12.3 | 20.5 ± 13.5 | 21.2 ± 6.1 | 15.3 ± 13.6 |
| Total | 9.1 ± 3.0 | 12.6 ± 3.2 | 19.0 ± 12.6 | 18.1 ± 11.3 | 23.0 ± 7.5 | 10.6 ± 15.0 |
Of note, the total averages were calculated from all four groups (anterior, posterior, combination, and no slip groups)
* P < 0.05
Fig. 3.
a Correlation between the postoperative AA and C2–C7 angles. b Correlation between the AA and C2–C7 angle changes
Fig. 4.
a Difference in AA angle changes between patients with anterior subluxation (slip) and those with no slip. b Difference in C2–C7 angle changes between patients with anterior slip and those with no slip
Fig. 5.
C2–C7 angle changes at the preoperative, the immediate postoperative (3 months after the operation) and the latest follow-up in patients with anterior subluxation (slip). * P < 0.05; n.s. not statistically significant
Discussion
Atlantoaxial transarticular screw fixation combined with posterior bone graft has established itself as a reliable surgical management for atlantoaxial subluxation [5, 7, 8] with a few serious problems, including intraoperative vascular impairments [17, 18] and non-union of bone grafts between C1 and C2 spinous processes and/or non-fused C1–C2 facets [10]. However, only a few of the late complications have been reported, one of which is subaxial sagittal alignment change [11, 15, 23]. We have encountered several patients with serious subaxial subluxations, two of whom presented with progressive neurological deterioration and required operative interventions. From this retrospective study, we found that RA patients have a greater risk of developing subaxial subluxations after atlantoaxial transarticular screw fixation. Moreover, a perioperative increase in the AA angle leads to a decrease in the C2–C7 angle, followed by new or aggravated anterior subluxations of the upper cervical spine and possibly neurological deterioration.
One reason why such a complication has not been reported is that RA patients are not the majority of the reported cases using atlantoaxial transarticular screw fixation. RA consisted of only one-third of 191 [7] and 75 patients [8] in two of representative cohort studies, respectively. Even in one report that included 35 RA patients only, subaxial subluxation was not a major focus even though it was mentioned that the subluxation led to neurological deterioration [15], and there has been no comparative report between RA and non-RA patients. However, 13 of 33 RA cases in our series showed unmistakable, worrisome subaxial subluxation after a certain period of time (4.2 years in average) in this study. Indeed, two patients required subsequent corrective operations, and several needed further attention, while non-RA patients did not develop this instability after the operation.
The non-RA group surprisingly did not show even any correlation between the postoperative AA and C2–C7 angles, although the number in this group may be insufficient to draw a clear conclusion. One possibility is that non-RA patients would have had a similar risk but tended to have fewer biomechanical compensatory changes caused by rigidity. In contrast, the cervical spines of RA patients are susceptible to biomechanical changes caused by local instability, leading to a disruption of the cervical alignment. Mukai et al. [15] reported, indeed, an example of biomechanical compensation after C1–C2 fixation, namely an increase in C1–C2 lordosis, a progressive ventral shift of C2 relative to C7, a progressive decrease in C2–C7 lordosis and a tendency for C1 inclination to return to preoperative inclination. However, none of the previous reports analyzed more crucial subaxial subluxations. Here, we demonstrate for the first time the importance of perioperative AA angle changes along with subsequent changes in C2–C7 angles, possibly leading to subaxial subluxation.
Another reason may be that causative factors of subaxial subluxation are too many to dray any conclusion from a cohort study. For one, an argument could be that subaxial subluxation is one of the possible deformities associated with RA in the natural course, similar to atlantoaxial subluxation, and is not a late complication. In RA patients, anterior subaxial subluxation does indeed tend to occur in the lower cervical spine without C1–C2 fixation, compared with posterior subluxation in patients with cervical spondylosis [22]. However, before the operations in this study, RA patients predominantly had posterior rather than anterior subluxations and developed new or aggravated anterior subluxations after the operation (Fig. 1), and the change occurred within a relatively short time (3 months) after the operation but not thereafter (Fig. 5). Moreover, the anterior subluxation followed a significant decrease in the perioperative C2–C7 angle (Fig. 5), not vice versa. In addition, the levels of anterior subluxation were significantly different between pre- and postoperative changes (Fig. 2b), as previously reported [22]. Thus, those sequential changes indicate that anterior subluxation should be considered as a late complication of this operation or, at least, can be accelerated by C1–C2 fixation. This complication probably results from the broken balance of the entire cervical alignment if an inadvertent correction of anterior atlantoaxial subluxation is performed.
On the other hand, one can easily name some of the possible causative factors such as osteoporosis in rheumatoid arthritis, the activity of the disease, the effect of medication, or the age of the patient. Indeed, Yonezawa et al. [22] reported that anterior subaxial slip significantly correlated with the average daily dose of corticosteroid and the class or stage of RA among RA patients without any operation during their follow-up period. However, we have found no difference in the medical treatment between anterior slip and no slip patients (data not shown), and the sequential changes after the operation described above strongly indicate the direct relationship between the C1–C2 fusion and the subaxial subluxation. Indeed, Yoshimoto et al. [23] demonstrated that postoperative AA and C2–C7 angles showed a negative linear correlation and that C2–C7 angle changes showed a negative correlation with AA angle changes, and Yonezawa et al. [22] demonstrated a positive association between a lordo-kyphotic deformity and anterior slip occurrence, both of which supports our finding of the sequential changes that an increase of AA angle leads to a decrease of C2–C7 angle, resulting in anterior subaxial subluxation. With all possible factors taken into account, not denied are the probable effects from the disease activity and the medication to cervical deformities in RA patients, and even preventive contributions from recently developed or developing medications such as biologics are expectable. We have no definite data or published reports on that issue, but it is hopeful that sufficient subsidence of the disease by medication will enables the cervical spine of RA patients to resist any deformative forces and to behave as if the one of non-RA patients, as described in this study.
One of the limitations of this study was the definition of a subluxation. One could define a subluxation as 2.0, 2.5, or 3.0 mm and possibly draw different statistical results. However, Yonezawa et al. [22] reported that even 2 mm of anterior subluxation is more likely to occur in RA patients than non-RA patients, and the present study clearly showed that more substantial subluxations (3 mm or more) than smaller subluxations (2–2.4 mm) were observed in RA patients. Thus, RA patients will probably be shown to have a greater risk of postoperative subaxial subluxation if a sufficient number of cases are collected and if the degree of the subluxation is defined broadly enough. As Yonezawa et al. [22] showed that even 2 mm of anterior subluxation can lead to damage in the cervical spinal cord in RA patients, the higher rate of subluxation among RA patients must not be underrated. Taken together, our study apparently indicates that AA angle should be carefully decided with reference to C2–C7 angle when C1–C2 fixation is performed in RA patients. Otherwise, subaxial subluxation is likely to occur within several years of follow-up, and neurological deterioration can be expected.
Conclusions
RA patients are more likely than non-RA patients to develop subaxial subluxations after atlantoaxial transarticular screw fixation. The increase in the AA angle occurring during the operation can lead to a decrease in the C2–C7 angle followed by anterior subluxation of the upper cervical spine and possibly neurological deterioration.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial company related directly or indirectly to the subject of this manuscript.
References
- 1.Agarwal AK, Peppelman WC, Kraus DR, Pollock BH, Stolzer BL, Eisenbeis CH, Jr, et al. Recurrence of cervical spine instability in rheumatoid arthritis following previous fusion: Can disease progression be prevented by early surgery? J Rheumatol. 1994;19:1364–1370. [PubMed] [Google Scholar]
- 2.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 3.Clarke MJ, Cohen-Gadol AA, Ebersold MJ, Cabanela ME. Long-term incidence of subaxial cervical spine instability following cervical arthrodesis surgery in patients with rheumatoid arthritis. Surg Neurol. 2006;66:136–140. doi: 10.1016/j.surneu.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 4.Dreyer SJ, Boden SD. Natural history of rheumatoid arthritis of the cervical spine. Clin Orthop Relat Res. 1999;366:98–106. doi: 10.1097/00003086-199909000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Eleraky MA, Masferrer R, Sonntag VK. Posterior atlantoaxial facet screw fixation in rheumatoid arthritis. J Neurosurg. 1998;89:8–12. doi: 10.3171/jns.1998.89.1.0008. [DOI] [PubMed] [Google Scholar]
- 6.Gallie WE. Fractures and dislocations of the upper cervical spine. Am J Surg. 1939;46:495–499. doi: 10.1016/S0002-9610(39)90309-0. [DOI] [Google Scholar]
- 7.Gluf WM, Schmidt MH, Apfelbaum RI. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications and lessons learned in 191 adult patients. J Neurosurg Spine. 2005;2:155–163. doi: 10.3171/spi.2005.2.2.0155. [DOI] [PubMed] [Google Scholar]
- 8.Haid RW, Jr, Subach BR, McLaughlin MR, Rodts GE, Jr, Wahlig JB., Jr C1–C2 transarticular screw fixation for atlantoaxial instability: a 6-year experience. Neurosurgery. 2001;49:65–68. doi: 10.1097/00006123-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton JD, Johnston RA, Madhok R, Capell HA. Factors predictive of subsequent deterioration in rheumatoid cervical myelopathy. Rheumatology. 2001;40:811–815. doi: 10.1093/rheumatology/40.7.811. [DOI] [PubMed] [Google Scholar]
- 10.Ito H, Neo M, Fujibayashi S, Miyata M, Yoshitomi H, Nakamura T. Atlantoaxial transarticular screw fixation with posterior wiring using polyethylene cable: facet fusion despite of posterior graft resorption in rheumatoid patients. Spine. 2008;33:1655–1661. doi: 10.1097/BRS.0b013e31817b5c07. [DOI] [PubMed] [Google Scholar]
- 11.Kato Y, Itoh T, Kanaya K, Kubota M, Ito S. Relation between atlantoaxial (C1/2) and cervical alignment (C2–C7) angles with Magerl and Brooks techniques for atlantoaxial subluxation in rheumatoid arthritis. J Orthop Sci. 2006;11:347–352. doi: 10.1007/s00776-006-1033-x. [DOI] [PubMed] [Google Scholar]
- 12.Kraus DR, Peppelman WC, Agarwal AK, DeLeeuw HW, Donaldson WF., III Incidence of subaxial subluxation in patients with generalized rheumatoid arthritis who have had previous occipital cervical fusions. Spine. 1991;16:S486–S489. doi: 10.1097/00007632-199110001-00006. [DOI] [PubMed] [Google Scholar]
- 13.Magerl F, Seeman PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Werdner PA, editors. Cervical spine I. Vienna: Springer; 1987. pp. 322–327. [Google Scholar]
- 14.Matsunaga S, Sakou T, Onishi T, Hayashi K, Taketomi E, Sunahara N, et al. Prognosis of patients with upper cervical lesions caused by rheumatoid arthritis: comparison of occipitocervical fusion between c1 laminectomy and nonsurgical management. Spine. 2003;28:1581–1587. doi: 10.1097/00007632-200307150-00019. [DOI] [PubMed] [Google Scholar]
- 15.Mukai Y, Hosono N, Sakaura H, Fujii R, Iwasaki M, Fuchiya T, et al. Sagittal alignment of the subaxial cervical spine after C1–C2 transarticular screw fixation in rheumatoid arthritis. J Spinal Disord Tech. 2007;20:436–441. doi: 10.1097/BSD.0b013e318030ca3b. [DOI] [PubMed] [Google Scholar]
- 16.Naderi S, Crawford NR, Song GS, Sonntag VK, Dickman CA. Biomechanical comparison of C1–C2 posterior fixations. Cable, graft, and screw combinations. Spine. 1998;23:1946–1955. doi: 10.1097/00007632-199809150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Neo M, Matsushita M, Iwashita Y, Yasuda T, Sakamoto T, Nakamura T. Atlantoaxial transarticular screw fixation for a high-riding vertebral artery. Spine. 2003;28:666–670. doi: 10.1097/00007632-200304010-00009. [DOI] [PubMed] [Google Scholar]
- 18.Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T. Vertebral artery injury during cervical spine surgery. Spine. 2008;33:779–785. doi: 10.1097/BRS.0b013e31816957a7. [DOI] [PubMed] [Google Scholar]
- 19.Neo M, Sakamoto T, Fujibayashi S, Nakamura T. A safe screw trajectory for atlantoaxial transarticular fixation achieved using an aiming device. Spine. 2005;30:E236–E242. doi: 10.1097/01.brs.0000160998.53282.3f. [DOI] [PubMed] [Google Scholar]
- 20.Shen FH, Samartzis D, Jenis LG, An HS. Rheumatoid arthritis: evaluation and surgical management of the cervical spine. Spine J. 2004;4:689–700. doi: 10.1016/j.spinee.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 21.White AP, Biswas D, Smart LR, Haims A, Grauer JN. Utility of flexion-extension radiographs in evaluating the degenerative cervical spine. Spine. 2007;32:975–979. doi: 10.1097/01.brs.0000261409.45251.a2. [DOI] [PubMed] [Google Scholar]
- 22.Yonezawa T, Tsuji H, Matsui H, Hirano N. Subaxial lesions in rheumatoid arthritis: radiographic factors suggestive of lower cervical myelopathy. Spine. 1995;20:208–215. doi: 10.1097/00007632-199501150-00015. [DOI] [PubMed] [Google Scholar]
- 23.Yoshimoto H, Ito M, Abumi K, Kotani Y, Shono Y, Takeda T, et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1–C2 fusion. Spine. 2004;29:175–181. doi: 10.1097/01.BRS.0000107225.97653.CA. [DOI] [PubMed] [Google Scholar]