Abstract
Posterior corrective surgery using “all pedicle screw construct” carries risk of neurovascular complications. The study aims were to assess the screw placement in patients with adolescent idiopathic scoliosis using CT with low-radiation dose, and to evaluate the clinical outcome in patients with misplaced pedicle screws. CTs of 49 consecutive patients (873 screws, 79% thoracic) were retrospectively evaluated by two independent radiologists. A new grading system was developed to distinguish between lateral, medial and anterior cortical perforations, endplate perforation and foraminal perforation. The grading system is based on whether the cortical violation is partial or total rather than on mm-basis. The overall rate of screw misplacement was 17% (n = 149): 8% were laterally placed and 6.1% were medially placed. The rates of anterior cortical, endplate and foraminal perforation were 1.5, 0.9, and 0.5%, respectively. Lateral cortical perforation was more frequent in the thoracic spine (P = 0.005), whereas other types of misplacement including medial cortical perforation were more frequent on the left and the concave side of scoliotic curves (P = 0.002 and 0.003). No neurovascular complications were reported. The association between the occurrence of screw misplacement and the Cobb angle was statistically significant (P = 0.037). Misplacements exceeding half screw diameter should be classified as unacceptable. Low-dose CT implies exposing these young individuals to a significantly lower radiation dose than do other protocols used in daily clinical practice. We recommend using low-dose CT and the grading system proposed here in the postoperative assessment of screw placement.
Keywords: Low-dose CT, Neurovascular complications, Medial cortical perforation, Lateral cortical perforation, Anterior cortical perforation
Introduction
Assessment of misplacement of pedicle screws in patients with adolescent idiopathic scoliosis (AIS) has been reported in many studies [1–3]. Computed tomography (CT) is the best method of performing such an assessment and in one study showed ten times as many pedicle violations as did plain radiography [4]. As the prevalence of breast cancer among patients with AIS has been reported to amount to 1.1 [5] radiation protection measures are mandatory. CT with low-radiation dose has been recently shown to be a reliable method in the assessment of pedicle screw placement with substantial interobserver and intraobserver agreements [6]. Furthermore, the radiation dose of plain radiography of spine varies in different reports and in some studies is reported to be as high as 26 mSv [7] compared with 0.37 mSv for the low-dose spine CT in that study [6]. The risk for development of lethal cancer is calculated to be 5% per Sievert [8]. This means that beside the higher diagnostic accuracy, patients undergoing low-dose CT of spine carry at least 70 times lower risk of developing lethal cancer than those examined with plain radiography according to, e.g., the aforementioned report of 26 mSv.
The rate of screw misplacement in the thoracic region has been reported to vary from 5.7 to 50%, whereas the rate of neurovascular complications ranges from 0 to 1% [1, 3, 9–11]. In almost all reports no complications have been reported when pedicle breach was less than 2 mm and a potential for neurological complication was believed to exist only when medial wall perforation exceeds 4 mm [3]. Regarding grading systems for assessment of screw placement, up to 35 methods have been used for this purpose [12]. However, none of them included all possible types of screw misplacement. The pedicular width in the thoracic spine is not unusually less than 3, 2.6 mm in one report [13], which is narrower than the pedicle screws often used in scoliosis surgery.
In the view of the above mentioned facts a new grading system was developed, used and proved to be feasible and practical in the assessment of screw placement [6] with the grading primarily based on whether the cortical violation is partial or total rather than measuring the misplacement in millimeters. To our knowledge, there is no report on assessment of the accuracy of pedicle screw insertion using CT with low-radiation dose.
The aim of this study was to assess the pedicle screw placement in patients with AIS operated on with posterior correction and stabilization, using a spine low-dose CT. The other aims were to study the relationship of misplaced screws to the surrounding anatomical structures and to evaluate the clinical outcome in patients with misplaced pedicle screws.
Materials and methods
Patients
Following the approval of the regional radiation protection committee low-dose CT has been used in the perioperative workup of patients with spinal deformities in our institution since June 2007. To date analysis of a total of 59 consecutive patients with AIS, who had undergone posterior corrective surgery and stabilization with a titanium all-pedicle screw construct, have been examined with low-dose CT. Forty-nine patients have given their written consent to be included in this retrospective analysis. The regional ethical committee approval to conduct this retrospective analysis was obtained. Low-dose spine CT was performed 6 weeks after surgery. Thirty eight patients (78%) were female and 11 patients (22%) were male. The mean and the median values of patient age were 16.8 ± 4.2 (mean ± SD), and 16 years.
Low-dose CT examinations
All examinations were performed on a 16-slice CT-scanner (SOMATOM Sensation 16, Siemens AG Forchheim, Germany) with scan parameters recommended by a previously conducted phantom study [14]. To minimize the streak artifacts from the implants, reformatted 1-mm thick axial images with soft tissue algorithm and 2-mm thick coronal and sagittal reformatted images with the same algorithm have been used for the analysis.
Grading system of screw placement
The type of placement of every individual screw included in the analysis was assessed using a new grading system [6]. The following types of misplacement were included in the analysis: medial cortical perforation (MCP), lateral cortical perforation (LCP), anterior cortical perforation (ACP), endplate perforation (EPP), and foraminal perforation (FP).
Evaluation of screw placement
All examinations included in the analysis were read independently by two senior radiologists (K.A.K., A.S.) of whom one (K.A.K.) performed the analysis at two different occasions with 6 weeks interval. Screws where the two readers disagreed about their position were subjected to a joint evaluation by both readers to reach a consensus about the status of the screw placement.
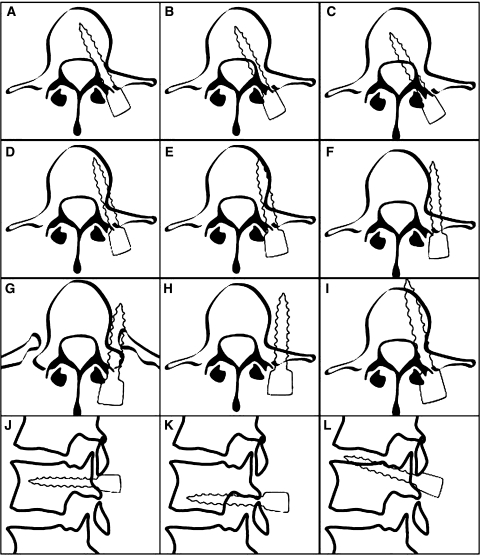
A detailed analysis of the misplaced screws was performed and the relationship of every individual screw to the following structures was studied: (a) concavity or convexity of the scoliotic curve, (b) apex of the major curve, (c) surrounding bony structures: lateral and medial pedicular cortex, vertebral body as well as pedicle rib unit (PRU), and (d) aorta, pleura and the surrounding tissues (Fig. 1). The degree of the spinal canal encroachment was measured in millimeter in cases of medially placed pedicle screws.
Fig. 1.
The types of screw placement according to the new grading system and examples of the relationship between different misplaced screws and the surrounding structures. a Normally placed screw. b Grade 1 MCP. c Grade 2 MCP. d Grade 1 LCP. Screw anchors in the vertebral body. e Grade 1 LCP. Screw passes within the vertebral body and abuts its inner cortex. f Grade 2 LCP. Screw abuts outer cortex of the vertebral body and does not anchor in the vertebral body. g Grade 2 LCP. Screw passes through the PRU and does not anchor in the vertebral body. h Grade 2 LCP. Screw with paravertebral passage. i ACP. j Normally placed screw on sagittal plane. k FP: perforation of underlying neural foramen. l EPP: perforation of upper endplate
Clinical outcome
Finally an outcome-based analysis of the screw placement was performed and the medical records of all patients with total perforation of pedicular cortex were scrutinized. The intraoperative course of events, the medical status in the immediate postoperative period as well as at the outpatient follow-up 8 weeks after surgery were evaluated with respect to the occurrence of symptoms and signs of neurovascular complication that could be related to screw misplacement. At the 8-week follow-up visit all patients were asked about any history of new neurological symptom related to spinal cord or nerve root compromise. Evidence of myelopathy with increased reflexes, abnormal clonus, and Babinski sign were specifically sought for.
Statistical analysis
Statistical analysis was performed by means of SPSS version 15. Chi-square test was performed to test the significance of association between the misplacement in general, MCP, and LCP with the following variables: (1) level of misplacement (thoracic or lumbar), (2) side of misplacement (right or left), (3) curve concavity or convexity, and (d) scoliotic apex. Statistical significance was set to <0.05. Mann–Whitney U test was performed to test the association between screw misplacement, Cobb angle, and the degree of vertebral rotation.
Operative technique
All operations were performed according to a standardized technique through a posterior exposure. The entry points for screws were determined after identification of the bony landmarks. At each assumed entry point, a 1-mm thick and 3-cm-long titanium bone marker was inserted approximately 3 mm deep. By means of a C-arm fluoroscopy in the AP view, the position as well as the degree of rotation was estimated. The position was considered as acceptable when having the marker as the bull’s eye on the screen. The screw canal was prepared with a hand-driven drill. After drilling, a probe or “feeler” was used to palpate the bottom and borders of the screw canal. Thereafter, self-tapping transpedicular screws were sequentially introduced. After completion of screw insertion, a check of screw position was undertaken by means of the C-arm fluoroscopy in oblique views. Curve correction was performed by simple rod derotation as well as direct vertebral rotation (DVR) [15] when having only the concave rod in place. All operations were performed under spinal cord monitoring by means of motor evoked potential.
Results
Curve characteristics and distribution of pedicle screws are shown in Table 1.
Table 1.
Curve characteristics and distribution of pedicle screws
| Type of curves | N (%) |
|---|---|
| Right convex thoracic curve | 34 (69.4) |
| S-formed double curves | 10 (20.4) |
| Left convex thoracic curve | 2 (4.1) |
| Left convex lumbar curve | 3 (6.1) |
| Scoliotic apex (major curve) | |
| T8 or T9 | 43 (87.8) |
| L2 | 3 (6.1) |
| T12 | 2 (4.1) |
| T5 | 1 (2) |
| Distribution of screws | |
| Thoracic | 688 (78.9) |
| Lumbar | 185 (21.1) |
| Distribution of thoracic screws | |
| T1–T6 | 273 (31.2) |
| T7–T10 (at or around scoliotic apex) | 273 (31.2) |
| T11–T13 | 142 (16.5) |
| Cobb angle | |
| Whole study population | 55.1 ± 10.4° (55.5°)* |
| Patients with no misplacement | 54.7 ± 10.4° (55.3°)* |
| Patients with screw misplacement | 56.7 ± 10.3° (57°)*, P = 0.037 |
| The degree of vertebral rotation | |
| Whole study population | 19.8 ± 6.9° (18°)* |
| Patients with no misplacement | 19.7 ± 6.9° (18°)* |
| Patients with screw misplacement | 20.1 ± 6.4° (18°)*, P = 0.438 |
* Mean ± SD (median)
The two readers who performed the assessment of screw placement have agreed about the status of pedicle screws in 832 out of 873 screws (95.3%), which resulted in an almost perfect interobserver agreement with κ 0.83 (95% confidence interval 0.32–1.33). The joint evaluation of the two readers about the status of the remaining 41 pedicle screws resulted in a consensus in 38 pedicle screws, whereas the status of three screws (0.3%) remained questionable.
The results of the radiological assessment of screw placement
The overall rate of misplacement was 17% while the acceptably placed screws amount to 82.7%. The rates of LCP, MCP, ACP, EPP, and FP were 8, 6.1, 1.5, 0.9, and 0.5%, respectively, Table 2. Of the misplaced screws 84% were thoracic, 59% were inserted in pedicles on the left hand side, 56% were inserted in pedicles on the concave side of the scoliotic curves, and 31% were inserted at or around the scoliotic apex. Of the 54 screws with MCP 40 (74%) were on the left side (P = 0.005) (Table 3). Of 70 screws with LCP 65 (93%) were thoracic (P = 0.005). Regarding the side and relation to scoliotic curves, screws with LCP were slightly more frequent on the right side and on the convexity of scoliotic curves (54 and 57%, respectively), whereas other types of screw misplacement were reported 2.5 times and twice as frequent on the left side and the concavity of scoliotic curves respectively (P = 0.002 and 0.003, respectively) (Table 3). The association between the occurrence of screw misplacement and the Cobb angle was statistically significant (P = 0.037) (Table 1).
Table 2.
Results of the radiological assessment of pedicle screw placement
| Total (%) | T (%) | L (%) | Dx (%) | Sin (%) | Cc (%) | Cx (%) | Apex (%) | None-apex (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Medial placement | 54 (6.1) | 44 (81) | 10 (19) | 14 (26) | 40 (74) | 33 (61) | 21 (39) | 15 (28) | 39 (72) |
| Lateral placement | 70 (8) | 65 (93) | 5 (7) | 38 (54) | 32 (46) | 30 (43) | 40 (57) | 26 (37) | 44 (63) |
| Anterior cortical perforation | 13 (1.5) | 13 (100) | 0 (0) | 3 (23) | 10 (77) | 10 (77) | 3 (23) | 2 (15) | 11 (85) |
| Endplate perforation | 8 (0.9) | 1 (12) | 7 (88) | 6 (75) | 2 (25) | 6 (75) | 2 (25) | 2 (25) | 6 (75) |
| Foraminal perforation | 4 (0.5) | 2 (50) | 2 (50) | 0 (0) | 4 (100) | 4 (100) | 0 (0) | 2 (50) | 2 (50) |
| Misplacement: Total | 149 (17) | 125 (84) | 24 (16) | 61 (41) | 88 (59) | 83 (56) | 66 (44) | 47 (31) | 102 (69) |
| Normal placement | 721 (82.7) | 560 (78) | 161 (22) | 253 (35) | 468 (65) | 444 (62) | 277 (38) | 209 (29) | 512 (71) |
| Questionable | 3 (0.3) | 3 (100) | 0 (0) | 2 (67) | 1 (33) | 1 (33) | 2 (67) | 0 (0) | 3 (100) |
| Total (all screws included in analysis) | 873 (100) | 688 (79) | 185 (21) | 316 (36) | 557 (64) | 528 (61) | 345 (39) | 256 (29) | 617 (71) |
T thoracic, L lumbar, Dx right, Sin left, Cc pedicle screws inserted on the concave side of the curve, Cx pedicle screws inserted on the convex side of the curve, Apex pedicle screws inserted at the scoliotic apex, None-apex pedicle screws inserted at levels other than apex
Table 3.
Results of Chi-square test of association between misplacements in general, MCP and LCP with different predictors (shown in the first column)
| Misplacement, all | P value | Misplacement | P value | Misplacement | P value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | MCP | Other | LCP | Other | ||||
| Thoracic | 125 | 560 | 0.091 | 44 | 81 | 0.546 | 65 | 60 | |
| Lumbar | 24 | 161 | 10 | 14 | 5 | 19 | 0.005* | ||
| Right | 61 | 253 | 0.176 | 14 | 47 | 0.005* | 38 | 23 | |
| Left | 88 | 468 | 40 | 48 | 32 | 56 | 0.002* | ||
| Concave | 83 | 444 | 0.181 | 33 | 50 | 0.317 | 30 | 53 | |
| Convex | 66 | 277 | 21 | 45 | 40 | 26 | 0.003* | ||
| Apex | 47 | 209 | 0.533 | 15 | 32 | 0.456 | 26 | 21 | |
| Non-apex | 102 | 512 | 39 | 63 | 44 | 58 | 0.166 | ||
* Statistical significant association
The results of the outcome-based analysis of the screw placement
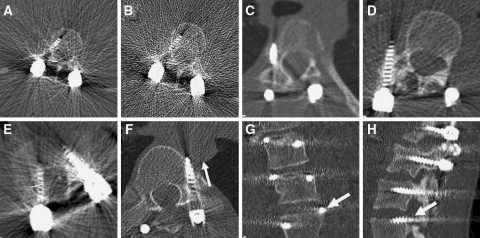
The results of the detailed analysis of the screw placement are shown in Table 4. Regarding medially placed screws, 35 of 37 partially medialised screws (grade 1 MCP) anchor in their vertebral bodies. The degree of encroachment in cases where the screws totally perforated the medial pedicular cortex (grade 2 MCP; Fig. 2e) have been shown to vary from 3–5 mm (n = 14 of 17) to 6–7 mm (n = 3). No electrophysiological abnormalities were reported during the insertion of these misplaced screws and no neurological deficit was reported in the immediate postoperative period or in the outpatient follow-up 8 weeks after the surgery.
Table 4.
Detailed analysis of different types of misplacement, showing the relationship of every individual misplaced screw to the surrounding bony structures, the scoliotic curve and the scoliotic apex
| Misplacement | Remarks | Level | Side | Relation to curve | Relation to apex | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | T | L | Dx | Sin | Cc | Cx | Apex | None | ||
| Grade 1 MCP | Anchor in vertebral body | 35 | 29 | 6 | 10 | 8 | 21 | 14 | 9 | 26 |
| Anchor to vertebral body with 5 mm of the screw tip | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 1 | |
| Total | 37 | 30 | 7 | 10 | 27 | 22 | 15 | 10 | 27 | |
| Grade 2 MCP | 3–4 mm encroachment, abuts medial pedicular cortex and anchor in vertebral body | 9 | 8 | 1 | 1 | 8 | 9 | 0 | 0 | 9 |
| 4 mm encroachment, screw tip in the spinal canal | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | |
| 5 mm encroachment, abuts medial pedicular cortex and anchor in vertebral body | 4 | 3 | 1 | 2 | 2 | 1 | 3 | 3 | 1 | |
| 6 mm encroachment, anchor in vertebral body | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | |
| 7 mm encroachment, screw tip in the spinal canal | 2 | 1 | 1 | 0 | 2 | 0 | 2 | 1 | 1 | |
| Total | 17 | 14 | 3 | 4 | 13 | 11 | 6 | 5 | 12 | |
| Grade 1 LCP | Anchor in vertebral body | 22 | 19 | 3 | 8 | 14 | 15 | 7 | 9 | 13 |
| Passes laterally in the vertebral body and abuts their inner cortex | 8 | 8 | 0 | 5 | 3 | 3 | 5 | 5 | 3 | |
| Total | 30 | 27 | 3 | 13 | 17 | 18 | 12 | 14 | 16 | |
| Grade 2 LCP | Anchor in vertebral body | 2 | 2 | 0 | 0 | 2 | 1 | 1 | 1 | 1 |
| Abuts lateral pedicular cortex and vertebral body. Do not anchor in the vertebral body | 25 | 24 | 1 | 15 | 10 | 9 | 16 | 7 | 18 | |
| Passes through pedicle rib unit (PRU) with screw tip in the PRU | 7 | 7 | 0 | 6 | 1 | 1 | 6 | 2 | 5 | |
| Passes through pedicle rib unit (PRU) with screw anterior to PRU | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | |
| Paravertebral passage | 5 | 4 | 1 | 4 | 1 | 0 | 5 | 1 | 4 | |
| Total | 40 | 38 | 2 | 25 | 15 | 12 | 28 | 12 | 28 | |
| ACP | Pure ACP | 8 | 8 | 0 | 2 | 6 | 6 | 2 | 0 | 11 |
| Associated with LCP | 5 | 5 | 0 | 1 | 4 | 4 | 1 | 2 | 0 | |
| Total | 13 | 13 | 0 | 3 | 10 | 10 | 3 | 2 | 11 | |
| EPP | Upper endplate | 8 | 1 | 7 | 6 | 2 | 6 | 2 | 2 | 6 |
| Lower endplate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | 8 | 1 | 7 | 6 | 2 | 6 | 2 | 2 | 6 | |
| FP | Overlying foramen | 2 | 0 | 2 | 0 | 2 | 2 | 0 | 0 | 2 |
| Underlying foramen | 2 | 2 | 0 | 0 | 2 | 2 | 0 | 2 | 0 | |
| Total | 4 | 2 | 2 | 0 | 4 | 4 | 0 | 2 | 2 | |
| Total number of all misplacements | 149 | 125 | 24 | 61 | 88 | 83 | 66 | 47 | 102 | |
T thoracic, L lumbar, Dx right, Sin left, Cc pedicle screws inserted on the concave side of the curve, Cx pedicle screws inserted on the convex side of the curve, Apex pedicle screws inserted at the scoliotic apex, None-apex pedicle screws inserted at levels other than apex
Fig. 2.
CT images showing some examples of screw placement and abnormal relationship of pedicle screws to the surrounding structures, which were encountered during the detailed analysis of the screw placement. a, b Axial images showing normally placed screw through the right pedicle of L1. Image a is reformatted with soft tissue algorithm, whereas image b is reformatted with skeletal algorithm, thus exhibiting increased noise. Image a with low signal-to-noise ratio was the image used during the evaluation of this study. c Axial image showing grade 2 LCP of a pedicle screw that passes totally lateral to the pedicle of T10 on the right side. d Axial image showing grade 2 LCP with paravertebral passage of pedicle screw which was supposed to pass through the right pedicle of L2. e Axial image showing the way of measurement of the degree of spinal canal encroachment of a medially placed pedicle screw. The encroachment is the distance between the medial pedicular cortex and the medial border of the medially placed screw, given in millimeter. f Axial image showing LCP and ACP of pedicle screw through T8 on the left side with screw tip touching the right and posterior margin of aorta (arrow). g Coronal image showing EPP through the upper endplate of L3 (arrow). h Sagittal image showing FP through the neural foramen above L3 on the left side (arrow)
Among the 30 screws which were partially lateralised (grade 1 LCP) 22 anchored in the respective vertebral bodies while 8 screws passed laterally through the vertebral bodies and abutted their inner cortex resulting in suboptimal hold in the vertebral bodies.
The total number of screws with ACP was 13, of which 5 were associated with LCP. The average perforation of anterior cortex was 2.3 mm (range 1–6 mm). All reported cases of EPP (n = 8) occurred into the upper endplates while the FP (n = 4) occurred equally into the overlying and the underlying neural foramen.
Vicinity of the screw tip to aorta (Fig. 2f) was found in 15 screws (10 patients) of which 6 screws were placed with ACP and 9 with LCP. The average distance between the screw tip and the dorsal or the lateral wall of aorta was 2.9 mm (range 1–4). Figure 2 shows examples of different types of screw misplacement.
Discussion
In this study placement of 873 pedicle screws has been evaluated with low-dose CT. This is the first report in the literature on the assessment of screw placement with low-dose CT. A newly developed grading system [6] was used for evaluation of five types of misplacement: LCP, MCP, ACP, EPP, and FP. However, all screws with total cortical perforation were subsequently evaluated with regard to their relation to the spinal canal and to the surrounding structures.
Literature review of some of the reports of misplacement of pedicle screw based on CT evaluation [1–3, 9, 11, 16–22] is shown in Table 5. The most commonly reported types of misplacements are the LCP and MCP. The overall rate of misplacement reported in this study was 17%. Five of the studies dealing with assessment of pedicular screw placement in scoliosis showed a misplacement rate of 5.7, 50.7, 25, 29.1, and 18.5% [1, 3, 9, 20, 22].
Table 5.
Literature review of some of the reported screw misplacements assessed with postoperative CT
| Patient number | Screw number | Region | Misplacement (%) | Medial (% of total) | Lateral (% of total) | Neurovascular complications (number) | Others remarks | |
|---|---|---|---|---|---|---|---|---|
| Silvestre [1] | 25 | 311 | Thoracic | 5.7 | 1 | 3.8 | 0 | Scoliosis |
| Gertzbein [2] | 40 | 71 | Thoracic | 30 | 25.5 | 4 | 2, resolved spontaneously | Reported MCP 6–7 mm |
| Upendra [3] | 24 | 138 | Thoracic | 50.7 | 24.6 | 24.7 | 2 | Scoliosis |
| Upendra [3] | 34 | 176 | Thoracic | 50 | 31.8 | 11.4 | 0 | Non-scoliosis |
| Liljenqvist [9] | 32 | 120 | Thoracic | 25 | 8.3 | 14.2 | 0 | Scoliosis |
| Belmont [11] | 40 | 279 | Thoracic | 43 | 14 | 29 | 0 | |
| Heary [16] | 27 | 185 | Thoracic | 13.5 | 1.6 | 11.3 | ||
| Lekovic [17] | 37 | 277 | Thoracic | 18 | 2.2 | 13 | 0 | Guided insertion |
| Smorgick [18] | 25 | 112 | Thoracic | 12.5 | 0 | 1.8% aortic abutment | ||
| Kim [19] | 49 | 557 | Thoracic | 6.2 | 1.8 | 4.7 | 0 | |
| Sarlak [20] | 19 | 185 | Thoracic | 29.1 | 10.8 | 18.3 | 0 | Scoliosis |
| Lehman [21] | 60 | 1,023 | T1–L4 | 10.5 | 8.6 | 1.9 | 0 | |
| Halm [22] | 25 | 178 | T5–L4 | 18.5 | 4.5 | 12.4 | 0 | Scoliosis |
| This study | 49 | 873 | T1–L5 | 17 | 6.1 | 8 | 0 | Scoliosis |
This review, including the present study, includes the results of a total of 486 patients (4,485 screws)
From the clinical point of view the screws with MCP represent the most feared types of misplacement, which should be studied in detail because of an attendant risk for neurological complications. Gertzbein et al. [2] suggested that a medial canal encroachment of up to 4 mm between T10 and L4 can be tolerated. Kim et al. [19] have also expressed a tolerant position in this issue suggesting a “definite”, “probable”, and “questionable” safe zones with medial encroachment of <2, 2–4, and 4–8 mm, respectively if there were no abnormal electrophysiological findings during and after the screw insertion. However, Sarlak et al and Vaccaro et al [20, 23] have expressed lower tolerance to spinal canal encroachment. Screws with spinal canal encroachment exceeding 4 mm at the concave side of the scoliotic apex carry higher risk of spinal cord injury, as the dural sac and consequently the spinal cord shift to the concave side at scoliotic apex [24]. One of the screws with encroachment of 5 mm reported in our study was inserted at the concave side of scoliotic apex and one screw with 7 mm encroachment were inserted at convex side of the scoliotic apex. However, these degrees of screw misplacement were, according to our grading system and in accordance with most of the reports, classified as unacceptable despite the absence of evidence of neurovascular complications.
The screw-tip penetration into the neural foramen has not been frequently discussed in literature although it carries a potential risk for nerve root injury. Our study reported FP in four different patients of whom none showed evidence of nerve root injury. In our opinion the EPP has to be considered the least injurious of all types of the screw misplacement discussed here as we are dealing with a surgical procedure whose primary aim is spinal fusion. However, the EPP of the non-fused vertebral levels (i.e., at either end of the operated segment) is specifically important to study and report. We believe that pedicle screws with ACP with the screw tip in the vicinity of aorta need to be followed up with a suitable imaging modality, for example CT-angiography, to exclude the development of pseudoaneurysm.
We believe that adopting the new grading system (based on whether the cortical violation is partial or total rather than measuring the misplacement in millimeters and regarding the screw misplacement of less than half screw diameter as “acceptable”) is more practical and easy to perform for research purposes as well as in clinical practice as: (1) pedicle perforation of ≤2 mm (almost half screw diameter) is considered harmless [3]. (2) The pedicular width in the thoracic spine may be as small as 2.6 mm [13], which means that many pedicle screws are inclined for misplacement regardless of the skilfulness of the operating surgeon as screw diameter varies between 4.5 and 5.5 mm, and (3) avoiding measurements in millimeter and submillimeter reduces the influence of individual variations and avoids the inherent error of measurements when these are performed in the Picture Archiving and Communication System (PACS).
The use of our low-dose CT in the assessment of screw placement has to be considered as one of the major advantages of this study and will hopefully contribute to reduce the risk of cancer development in these young individuals.
Conclusion
This study of the radiological and clinical outcome of screw placement in patients with AIS after posterior corrective surgery using titanium screws showed that screw placement can be evaluated using low-dose spine CT with the advantage of exposing these young patients to markedly reduced radiation dose. The overall rate of misplacement reported in this study was 17%. None of these patients reported symptoms or signs related to neurovascular complications. A spinal canal encroachment of up to 5 mm (almost whole screw diameter) on the concavity and up to 7 mm on the convexity of scoliotic apex might be encountered with no evidence of neurovascular complications. Misplacements exceeding half screw diameter should be classified as unacceptable, whereas misplacement of less than half screw diameter can be regarded as “acceptable” in the absence of evidence of neurovascular complications. However, more studies on screw placement using the grading system proposed here need to be reported to validate our statement that misplacement of less than half screw diameter is “acceptable”. Special attention should be paid to pedicle screws with MCP and ACP, and the relationship of screw tip to the surrounding structures should be studied in detail. Assessment of screw position in relation to neural foramen should be included in the analysis of screw placement.
Conflict of interest statement
No benefits or funds were received in support of this work. No conflicts of interest are known.
References
- 1.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32:1655–1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 2.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Upendra BN, Meena D, Chowdhury B, Ahmad A, Jayaswal A. Outcome-based classification for assessment of thoracic pedicular screw placement. Spine. 2008;33:384–390. doi: 10.1097/BRS.0b013e3181646ba1. [DOI] [PubMed] [Google Scholar]
- 4.Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine. 1995;20:1494–1499. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman DA, Lonstein JE, Morin MM, Visscher W, Harris BS, Boice JD., Jr Breast cancer in women with scoliosis exposed to multiple diagnostic X-rays. J Natl Cancer. 1989;81:1307–1312. doi: 10.1093/jnci/81.17.1307. [DOI] [PubMed] [Google Scholar]
- 6.Abul-Kasim K, Strömbeck A, Ohlin A, Maly P, Sundgren PC. Reliability of low radiation dose CT in the assessment of screw placement after posterior scoliosis surgery, evaluated with a new grading system. Spine. 2009;34:941–948. doi: 10.1097/BRS.0b013e31819b22a4. [DOI] [PubMed] [Google Scholar]
- 7.Antevil JL, Sise MJ, Sack DI, Kidder B, Hopper A, Brown CV. Spiral computed tomography for the initial evaluation of spine trauma: a new standard of care? J Trauma. 2006;61:382–387. doi: 10.1097/01.ta.0000226154.38852.e6. [DOI] [PubMed] [Google Scholar]
- 8.Publication 60. Recommendations of the International Commission on radiological Protection (1990) Annals of the ICRP [PubMed]
- 9.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 11.Belmont PJ, Jr, Klemme WR, Dhawan A, Polly DW., Jr In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 12.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine. 2007;32:E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 13.Parent S, Labelle HL, Skalli W (2002) Thoracic pedicles morphometry in vertebrae from scoliotic spines. Abstract from the SRS Annual Meeting [DOI] [PubMed]
- 14.Abul-Kasim K, Gunnarsson M, Maly P, Ohlin A, Sundgren PC. Radiation dose optimization in CT planning of corrective scoliosis surgery. A phantom study. Neuroradiol J. 2008;21:374–382. doi: 10.1177/197140090802100313. [DOI] [PubMed] [Google Scholar]
- 15.Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine. 2004;29:343–349. doi: 10.1097/01.BRS.0000109991.88149.19. [DOI] [PubMed] [Google Scholar]
- 16.Heary RF, Bono CM, Black M (2004) Thoracic pedicle screws: postoperative computerized tomography scanning assessment. J Neurosurg 100 (4 Suppl Spine):325–331 [DOI] [PubMed]
- 17.Lekovic GP, Potts EA, Karahalios DG, Hall G. A comparison of two techniques in image-guided thoracic pedicle screw placement: a retrospective study of 37 patients and 277 pedicle screws. J Neurosurg Spine. 2007;7:393–398. doi: 10.3171/SPI-07/10/393. [DOI] [PubMed] [Google Scholar]
- 18.Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y. Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech. 2005;18:522–526. doi: 10.1097/01.bsd.0000154448.90707.a8. [DOI] [PubMed] [Google Scholar]
- 19.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 20.Sarlak AY, Tosun B, Atmaca H et al (2009) Evaluation of thoracic pedicle screw placement in adolescent idiopathic scoliosis. Eur Spine J (14 Jun Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 21.Lehman RA, Jr, Lenke LG, Keeler KA, Kim YJ, Cheh G. Computed tomography evaluation of pedicle screws placed in the pediatric deformed spine over an 8-year period. Spine. 2007;32:2679–2684. doi: 10.1097/BRS.0b013e31815a7f13. [DOI] [PubMed] [Google Scholar]
- 22.Halm H, Liljeqvist U, Link T, Jerosch J, Winkelmann W. Computerized tomography monitoring of the position of pedicle screws in scoliosis surgery. Z Orthop Ihre Grenzgeb. 1996;134:492–497. doi: 10.1055/s-2008-1037444. [DOI] [PubMed] [Google Scholar]
- 23.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, et al. Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Jt Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Rauschning W. Anterior surgery of the thoracolumbar junction and the lumbar spine. Anatomy, complications and safeguards. Anterior spine surgery: standards and new techniques. Germany: Berlin; 1995. [Google Scholar]