Abstract
Abstract
Surgery in late stage ankylosing spondylitis (AS) most often tends to correct the sagittal balance with an extension osteotomy of the spine. In the literature, extension osteotomy was first described as an open wedge osteotomy but recently closed wedge osteotomy resecting the pedicles and posterior elements have become more popular. Only a limited number of cases have been reported in the literature and with limited focus on outcome of this major surgery. In this study, we reported the results of a large series of extension osteotomy in a population of patients with AS focusing on the technical aspects, complication rates, correction obtained and outcome evaluation using newer spine outcome measuring instruments. In the period from 1995 to 2005, 36 consecutive patients fulfilled the criteria where the files, radiographs and patients were available for further studies. The following data were recorded: Age, sex, comorbidity, indication, operation time and blood loss, level of osteotomy and estimated Correction. Furthermore, perioperative complications and all late complications were registered. The average follow-up was 50 months (3–128). Twenty-one patients also filled out questionnaires (SF36 and Oswestry Disability Index) preoperatively. At the end of the period all patients were contacted and filled out the same questionnaires. Fifteen of the patients had two pedicular resection osteotomies performed, 21 had one, and two had polysegmental osteotomies. Mean operation time was 180 min, bleeding was mean 2,450 ml, stay at the hospital was 13 days. One patient had partial paresis of the lower extremities all other complications were minor. The median correction was 45°. The median Oswestry score improved significantly from 54 (range 20–94) preoperatively to 38 (range 2–94) postoperatively. The SF-36 score significantly increased, when evaluated on the major components Physical Component Summary (PCS) and Mental Component Summary (MCS). The thoracolumbar closed wedge pedicular resection osteotomy used in this series was a safe method for correction of incapacitating kyphosis in AS. There was an acceptable rate of perioperative complications and no mortality. The correction obtained was in average 45°. All of the patients except one maintained their good correction and restored function. Outcome analysis showed a significant improvement in SF-36 and Oswestry Disability Index, and the mental component of the SF-36 showed improvement to values near the normative population. It is concluded that corrective osteotomy of the thoracolumbar spine in AS is an effective and safe treatment with improvements in quality of life.
Keywords: Ankylosing spondylitis, Closed wedge osteotomy, Bechterew, Spine, Outcome analysis
Introduction
The later stage of ankylosing spondylitis (AS) is often associated with severe postural deformities. The chronical inflammation results in progressive ossification of the ligaments of the spine and major joints with ankylosis of the spine. Eventually the spine becomes stiff and often in a position with loss of the normal sagittal alignment. The most common deformity is a loss of the lumbar lordosis. This together with a fixed ankylosis of the thoracic spine results in imbalance and poor posture. With an added involvement of the cervical spine the result can be even more invalidating.
The clinical results of this increasing deformity are loss of sagittal balance and impairment of the ability to stand upright. The vision in an upright position becomes impaired with inability to look ahead seeing the horizon resulting in problems in walking. The poor posture results in endurance strain to the spinal muscles and pain. The kyphotic deformity of the trunk increases pressure on the abdominal cavity with symptoms from organs and referred symptoms from the pressure on the diaphragm and reduced lung capacity [15, 18].
With progression of the ankylosis and deformity the indication for surgery may be considered absolute [4, 7, 19, 20]. The goal of surgery in late stage AS most often is a correction of the sagittal balance with an extension osteotomy of the spine. In the literature, extension osteotomy was first described as an open wedge osteotomy, where the posterior parts of the spine were resected, and the spine forcefully put in lordosis by opening of the anterior part of the ossified disc using the posterior column of the body as a fulcrum [9, 12, 14, 19].
In closed wedge osteotomy [10, 22, 25], the pedicles and posterior elements are resected together with the interpedicular part of the body. Both procedures have been seen as technically demanding and potentially hazardous with high complication rates. The modern development in spinal implants has resulted in improved methods of stabilizing the spine after an osteotomy reducing the technical problems, thereby allowing a more liberal attitude towards operative treatment of this category of patients.
Only a limited number of cases have been reported in the literature and with various techniques used. Only a few studies have have shown the results of larger series of closing wedge osteotomies and with limited focus on outcome of this major surgery [1, 11, 16].
We have found it of relevance to report the results of a large series of extension osteotomy in a population of patients with AS focusing on the technical aspects, complication rates, correction obtained and outcome evaluation using modern spine outcome parameters.
Materials methods
Patients
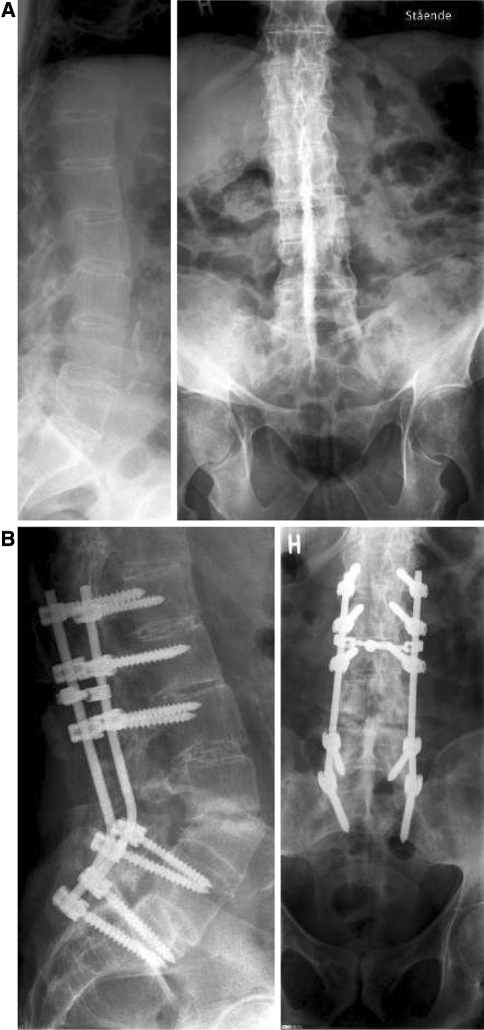
In the period from 1995 to 2005, 55 patients were operated on with closed wedge osteotomy (Fig. 1) of the thoraco–lumbar spine at our department. Sixteen of these patients were operated on for other conditions than AS. In three cases, the X-rays were not available for further studies due to loss during digitalization process of the X-ray archive. In 36 cases, the files, radiographs and patients were available for further studies.
Fig. 1.
The lateral view of the margins of the vertebral resection (left) and the corrected spine with pedicular screws implanted above and below the osteotomy (right)
The 36 patients (seven females and 29 males) were operated on because of an AS related kyphosis of the thoracolumbar spine by the same surgeon. The files and radiographs of each patient were reviewed. The average follow-up was 50 months (3–128). The patients in the later part of the period filled out questionnaires (SF-36 and Oswestry Disability Index) preoperatively. At the end of the study period all patients were contacted and filled out the same questionnaires.
The indication for surgery in all cases was inability to stand upright in a balanced position and inability to look straight forward and see the horizon, compression of the viscera due to kyphosis and pain due to muscle strain and stress on endurance of the back muscles.
Radiographic and clinical data
All patients had pre and postoperative standing radiographs of their spines. A minor subgroup had an MR scan performed, mostly because of suspicion of a narrowing of the spinal canal. The pre and postoperative radiographs were reviewed and the Cobb angle of kyphosis was measured. The Cobb angle of the lumbar curve were measured form the upper end plate of L1 to the lower endplate of L5. The pre and postoperative angle was measured in each case also in cases where the instrumentation passed the thoraco–lumbar junction.
From the patients files the following data were recorded: Age, sex, comorbidity, indication, operation time, blood loss, level of osteotomy and estimated correction. Furthermore, perioperative complications and all late complications were registered. The patients were all regularly followed with clinical and radiographic control after 3, 12 and 24 months and complications in this period were recorded. Only radiographs obtained at the routine controls were used in this study and no radiographs were taken at the final contact.
Planning and surgical technique
The indication for surgery was in all cases inability to stand upright, loss of visual field and decreased quality of life. The level of correction was planned following analysis of clinical and radiographic appearance. The clinical exam is often more informative than the radiographs due to the compensation not inevitably seen on films. The normal upper limit of thoracic kyphosis is 60–70° but a certain amount of exceeding kyphosis can be accepted without any clinical problem. Loss of lumbar lordosis has more severe impact on sagittal balance in uncompensated kyphosis as AS. Thus, a correction of the lumbar spine was addressed as the primary goal, and thoracic correction secondarily. Often, the stiff thoracic cage impede correction of the thoracic spine and this together with more sensible nature of the cord compared to the more distal levels of the cauda motivates approach distal for L1 if possible, and this will give the best result in terms of balance.
The amount of correction needed was planned from these considerations with the goal to obtain sagittal balance, after measuring the patient’s clinical degree of kyphosis when standing upright against a wall. One osteotomy can result in 40° of correction, if more than this was needed, a double osteotomy or one resection combined with polysegmental osteotomies was considered. Also the type of kyphosis was evaluated. If a sharp sagittal angulation was found the resection need to be done close to or in this deformity.
The patients were placed in a prone position with the operating table in a V-shaped position. Later in the study, a special frame allowed to apply support to the severe kyphotic spine and simultaneously correct the spine following the osteotomy. The patients were placed with the site of the spine where the osteotomy was planned, exactly over the intersection of the table where angulation of the different parts of the table was possible to correct subsequent to the osteotomy. The spine was approached by a posterior midline exposure with dissection laterally to the transverse process.
Pedicular screws were inserted in the levels proximal and distal to the osteotomy. In low lumbar osteotomies (L4) the sacral hold was evaluated and in cases of poor bone stock, a sacral plate with iliac extension was used.
Following the instrumentation, one or two osteotomies were performed. The whole vertebra including the discs was exposed from the outside by cutting the transverse process at the base, displacing them laterally. The roots from the segment above and below the ossified disc were exposed and protected. The soft tissues were released from the outside of the lateral parts of the spine and a tissue retractor was placed protecting the roots and the soft tissue laterally and frontally of the spine.
Following this the spinal canal was opened, and the dura mobilized. All the lamina was resected and the pedicle was excised with a rongeur or an osteotome. The dura was now retracted to the midline and with an osteotome a V-shaped cut was performed from the lateral cortex to the midline including all the base of the pedicle, and ending just posteriorly to the anterior cortex of the vertebral body.
Subsequently a rod was inserted in the pedicular screws but without tightening. The operating table was repositioned to the normal prone position and the spine was brought in extension closing the wedge. The bone from the osteotomy was used as a graft placing it postero-laterally next to the osteotomy. The amount of correction obtained was evaluated from the appearance of the spine estimating the pelvic tilt compared to the position of the head. Furthermore, a C-arm was used to measure the angulation of the osteotomy and exclude sagittal subluxation at the site.
The spine was fixed in the corrected position and the wound was closed (Fig. 2).
Fig. 2.
a, b Spine with ankylosing spondylitis before and after osteotomy at L4
Spinal cord monitoring was used measuring somato-evoked potentials. Further motor-evoked potentials were monitored from roots at the osteotomy site. A cell saver was used to decrease the need of allogenic blood transfusions.
The osteotomy was planned as low as possible, since this gives the best correction of the upper part of the spine.
All patients were treated with an orthosis without leg immobilisation in 3 months, most of the patients with a 3 points orthosis with a pilot on the sternum.
Outcome analysis
The outcome analysis was based on the SF-36 and the Oswestry Pain Disability score. The SF-36 defines 10 categories with a PCS (physical component summary) and MCS (mental component summary). The SF36 answers were compared using pre- and postoperative data and the normative healthy adult Danish populatin. The Oswestry pain disability score was analysed using the standard subgroups comparing pre and postoperative values.
Statistical analysis
The data were described as median (min and max value). The SF-36 data were analyzed using the SPSS package for scoring of SF36. Non-parametric statistics (Wilcoxons test) and t-test were used for statistical analysis and a value of P < 0.05 was considered significant.
Results
Fifteen of the patients had two pedicular resection osteotomies performed; 21 had one. Two patients had supplementary polysegmental wedge osteotomies. The most frequent level of osteotomy was L4 (26 cases) followed by L2 (15 cases). The rest of the levels distributed as shown in Table 1.
Table 1.
The principal data of 36 patients treated with pedicular resection closed wedge osteotomy of the thoraco–lumbar spine
| Age | Sex | Op-date | No Ost. | Level | Instrum. | OP-time | Bleeding | Hosp. Stay | Lord. Pre. | Lord. Post | Kyph. Pre. | Kyph. Post | Lumbar Correct. | F-UP-M. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 55 | F | 24-04-1991 | 1 + PS | L4 | L3-S2 | 420 | 4,000 | 58 | 70 | −15 | 40 | 40 | −85 | 128 | |
| 44 | F | 15-06-1995 | 2 | L2,L4 | Th7-L5 | 225 | 3,000 | 14 | 10 | −45 | 62 | 62 | −55 | 127 | |
| 46 | M | 31-08-1995 | 1 | L2 | Th12-S1 | 180 | 1,630 | 20 | −5 | −40 | 40 | 40 | −35 | 125 | |
| 35 | M | 06-12-1995 | 2 | L3,L5 | Th12-S1 | 210 | 2,050 | 14 | 13 | −57 | 60 | 60 | −70 | 121 | |
| 51 | M | 01-02-1996 | 1 | Th8 | Th6-L1 | 150 | 1,200 | 12 | −25 | −25 | 95 | 70 | 0 | 120 | |
| 48 | F | 06-03-1997 | 2 | L2,L4 | Th10-S1 | 240 | 2,800 | 11 | 2 | −48 | 59 | 59 | −50 | 107 | |
| 39 | M | 11-12-1997 | 2 | L2,L4 | Th11-S1 | 225 | 2,700 | 11 | 12 | −48 | 68 | 68 | −60 | 97 | |
| 62 | F | 14-05-1998 | 1 | L1 | Th10-S1 | 150 | 1,200 | 14 | 10 | −35 | 40 | 40 | −45 | 92 | Secondary fracture repaired |
| 55 | M | 19-10-1998 | 2 | L1,L3 | Th7-S1 | 240 | 2,700 | 30 | −4 | −44 | 96 | 51 | −40 | 87 | |
| 55 | M | 10-05-1999 | 2 | L2,L4 | Th8-S1 | 180 | 3,500 | 20 | 17 | −48 | 60 | 60 | −65 | 80 | |
| 48 | M | 26-08-1999 | 2 | L2,L4 | Th8-S1 | 150 | 500 | 6 | −13 | −47 | 52 | 52 | −34 | 77 | |
| 41 | M | 07-03-2002 | 2 | L2,L4 | Th9-S2 | 180 | 4,300 | 7 | 10 | −48 | 60 | 60 | −58 | 47 | |
| 32 | M | 08-04-2002 | 2 | L1,L3 | Th9-S1 | 210 | 750 | 10 | 10 | −48 | 70 | 70 | −58 | 46 | |
| 41 | F | 17-06-2002 | 6 | L1 | Th1-L3 | 450 | 2,600 | 13 | −5 | −47 | 65 | 65 | −42 | 44 | Loose implant reinserted |
| 44 | M | 12-09-2002 | 2 | L2,L4 | Th10-S1 | 200 | 1,100 | 19 | 20 | −32 | 48 | 48 | −52 | 41 | |
| 27 | M | 03-10-2002 | 2 | L2,L4 | Th10-S1 | 120 | 500 | 18 | 5 | −32 | 69 | 69 | −37 | 40 | |
| 49 | M | 28-10-2002 | 2 | L2, L4 | T10-S1 | 210 | 2,500 | 23 | −1 | −47 | 52 | 52 | −46 | 39 | Removal hardware Loss correction |
| 40 | M | 14-11-2002 | 2 | L2,L4 | Th10-S1 | 240 | 3,600 | 14 | −22 | −67 | 60 | 60 | −45 | 38 | |
| 53 | M | 13-01-2003 | 1 | L2 | Th9-L5 | 165 | 2,100 | 9 | −16 | −53 | 76 | 76 | −37 | 36 | |
| 61 | M | 14-01-2003 | 1 | L2 | Th9-L5 | 180 | 1,600 | 6 | 2 | −43 | 44 | 44 | −45 | 36 | |
| 33 | M | 22-09-2003 | 2 | L2,L4 | Th8-S1 | 210 | 3,900 | 7 | −16 | −61 | 60 | 60 | −45 | 28 | |
| 45 | F | 17-11-2003 | 1 | L4 | L1-S1 | 210 | 1,100 | 13 | −14 | −58 | 59 | 59 | −44 | 26 | Pneumothorax |
| 59 | M | 14-01-2004 | 1 | L4 | Th11-S1 | 205 | 3,200 | 8 | −9 | −45 | 44 | 44 | −36 | 24 | |
| 37 | M | 17-02-2004 | 1 | L4 | L1-S1 | 180 | 4,500 | 9 | −17 | −67 | 64 | 64 | −50 | 23 | |
| 60 | M | 08-03-2004 | 1 | L4 | Th12-S1 | 150 | 2,200 | 25 | −15 | −47 | 59 | 59 | −32 | 22 | |
| 46 | M | 17-03-2004 | 1 | L4 | L1-S1 | 210 | 3,200 | 13 | −23 | −62 | 58 | 58 | −39 | 22 | |
| 54 | M | 19-04-2004 | 1 | L4 | Th10-S1 | 180 | 2,000 | 8 | −14 | −60 | 65 | 65 | −46 | 21 | Pseudarthrosis |
| 57 | M | 20-09-2004 | 2 | L2,L4 | Th11-S1 | 210 | 2,400 | 16 | −15 | −63 | 72 | 72 | −48 | 16 | |
| 52 | M | 30-09-2004 | 1 | L4 | L1-S1 | 180 | 500 | 9 | −10 | −60 | 53 | 53 | −50 | 16 | |
| 48 | M | 22-11-2004 | 1 | L4 | L1-S1 | 150 | 3,300 | 10 | −21 | −68 | 44 | 44 | −47 | 14 | |
| 46 | M | 20-12-2004 | 1 | L4 | L1-S1 | 195 | 4,600 | 9 | −23 | −68 | 56 | 56 | −45 | 13 | |
| 34 | M | 03-02-2005 | 1 | L4 | L1-S1 | 105 | 3,800 | 7 | −27 | −64 | 65 | 65 | −37 | 12 | |
| 45 | M | 24-02-2005 | 1 | L4 | L1-S1 | 180 | 2,900 | 9 | −23 | −63 | 71 | 71 | −40 | 12 | |
| 63 | M | 01-06-2005 | 1 | L4 | Th12-S1 | 180 | 1,250 | 14 | −18 | −50 | 66 | 66 | −32 | 7 | |
| 58 | M | 24-08-2005 | 1 | L4 | L2-S1 | 165 | 2,000 | 19 | −17 | −50 | 55 | 55 | −33 | 5 | |
| 43 | F | 15-12-2005 | 1 | L1 | Th10-L5 | 150 | 2,300 | 7 | −31 | −48 | 77 | 77 | −17 | 3 |
In cases with single level osteotomy at L4, the instrumentation was always extended to the sacrum; proximally the instrumentation was always extended 3 levels above the most proximal level of osteotomy.
The median operation time was 180 min (105 and 450 min) and the operation time decreased steadily during the period. The median bleeding was 2,450 ml (500 and 4600 ml). The median length of stay at the hospital was 13 days (6 and 58 days).
Early complications
The complications included one patient with motor weakness (ASIA D) of the lower extremities and temporary loss of bladder control due to a dural tear with partial filament damage. One patient had pneumothorax treated with drainage for 3 days. One patient complained of temporary loss of color vision on one eye probably due to difficulties in the positioning. One patient was reoperated after 3 days because of a thoracic hook loosening and a fracture of the part of the lamina seating the hook. Due to the extensive manipulation of the roots at site of osteotomy several of the patients complained of root pain and a temporary weakness of the L3 and L4 root was seen in several cases.
Late complications
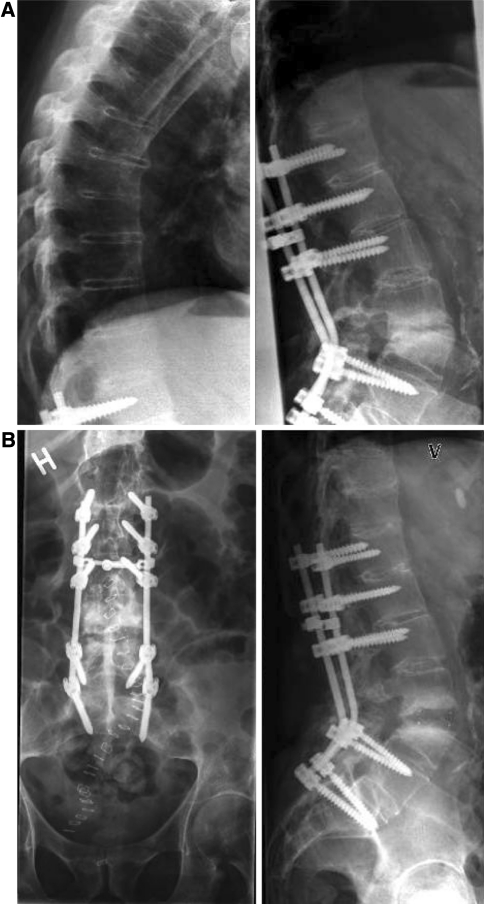
Three patients had healing problems, 1 with an anterior psedarthrosis without loss of correction, which healed following anterior bone grafting (Fig. 3). One had loosening of the implant due to poor bone stock and had the hardware removed after 16 months followed by gradually loss of correction.
Fig. 3.
ab Follow-up showing non union repaired by anterior approach with a cage
Radiographic result
The median correction was 45° with a preoperative lumbar lordosis of −11°. The postoperative lordosis averaged −48°. The preoperative thoracic kyphosis was in most cases above the normal and added the value of lumbar kyphosis the result was an imbalance.
Outcome
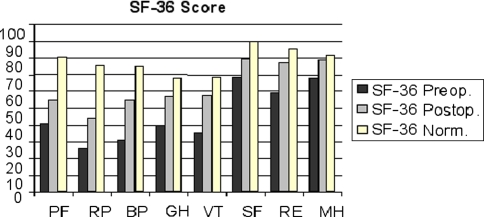
Thirty-five patients returned the questionnaire with Oswestry Diasability Index and SF-36. Since the evaluation forms was not used as a routine in the whole consecutive series only 21 filled out the forms prior to the operations. The median Oswestry score was 54 (range 20–94) preoperatively. This value was in the follow-up series after median 37 month reduced to mean 38 (range 2–94). Testing the pairwise samples where a pre- and postoperative value was valid, there was a significant reduction in Oswestry score at follow-up (P < 0.05, Fig. 4).
Fig. 4.
The SF-36 preoperatively, postoperatively and for the normative population. The difference between preoperative and postoperative value was significant P < 0.001
The SF-36 score increased for all of the different elements of the score (Fig. 4). This difference was also statistically significant, when evaluated on the major components Physical Component Summary (PCS) and Mental Component Summary (MCS) with P < 0.001. Compared to the normative data from the Danish norm population the patients in this series scored low both preoperatively and postoperatively for PCS, which illustrates the chronical inflammatory condition of AS. However, at follow-up, the mental component was not different from the normal population.
All patients except three answered that they were satisfied with the operation and that they would have the operation performed again if given the choice.
Discussion
Developments in implant technology have profoundly changed the surgical treatment of late stage AS. The goal of the surgery is correction of sagittal imbalance, which can only be obtained by a destabilization of the spine at the site of the osteotomy. It is thus extremely important to have methods for stabilization of the osteotomy site. Furthermore, due to recent developments in in-patient resources most patients are discharged from the hospital early, and old traditions to immobilize the spine by keeping the patients in bed in a spine plaster are not used today.
Correction of severe spinal deformities thus relies on possibilities for stable internal fixation and this proved useful in our cases. Extension osteotomies with pedicular wedge resection are well stabilized with the use of pedicular screws above and below the level and we had no cases of initial failure of the instrumentation or early loss of correction. However, this category of patients is characterized by osteopenia, which can impede the possibility of spinal instrumentation. Adding iliac extension of the instrumentation and elongation proximally to obtain solid fixation solved this problem [2, 9, 22]. All cases were mobilized early and a mean hospital stay of 13 days in our material seems acceptable in light of the extent of the surgery and the necessary rehabilitation following the operation.
The preoperative planning of the surgery very often depends on the clinical examination [24]. The radiographs give an indication of the kyphotic angle of the total spine and this shall be compared with the normal values of sagittal angulation in the different parts of the spine. However, it is not possible from the radiographs to estimate how much correction is necessary to result in a balanced upright position. This is often clearly indicated by measuring the total kyphosis of the spine when the patient is standing upright with fully extended knees and hips. The position of the head in this posture will give an indication of how much correction is necessary to obtain balance.
The level of the osteotomy has been discussed in the literature [6, 16]. In the beginning of this series the upper lumbar levels were chosen because of the easier access for pedicular screws below the osteotomy. However, since the kyphosis is often more global we gradually relied on the experience that the most correction was obtained by choosing the lowest level possible, since the resulting correction of the position of the head is more pronounced, the lower the osteotomy. In the later cases of the series most corrections was done at the L4 level and the distal fixation was obtained by using sacral plates or iliac screws in cases with poor bone stock.
One closing wedge osteotomy results in maximally 40° of correction as an average. Therefore, it is often necessary with more than one osteotomy if the deformity exceeds this value. On the other hand, two osteotomies results in higher blood loss, and a seriously increased surgical trauma and in the later part of the series, we obtained as much correction as possible at one level and reserved the two level osteotomies for the most severe cases. In the table there are four cases above 45° correction with one osteotomy. This may be explained by shifting from manual to digital measurement in several cases and due to inaccuracy of measurements in these not standardized radiographs taken as a part of a routine clinical set-up.
In the clinical examination it often seems compulsory to correct the cervical deformity but most often the lumbar osteotomy resulted in a global correction, which made further correction. We therefore, always advised the patient to receive a low lumbar osteotomy at first place and after this consider further correction if advisable.
In the literature three principal methods of correction are described; the open wedge (OW), the closed wedge (CW) and polysegmental osteotomies (PSO) [2, 13, 21, 23]. It has been advocated that it is difficult to find any preference for the methods. Polysegmental osteotomies have been reported with insufficient correction and loss of correction has been reported both for PSO and OWO. In OWO, an increased mortality has been reported due to vascular lesions during the correction procedure [17]. The CWO has a low rate of secondary loss of correction probably due to the nature of the osteotomy where the two cancellous surfaces interact with a rapid healing. Furthermore the closed wedge osteotomy is initially stable due to tension band nature of the posterior instrumentation and the full anterior support. It is well known that in cases with loss of anterior support (fracture cases and neoplastic conditions) loss of correction is very common and therefore, it is often advocated to do secondary insertion of bone if a deficiency of the anterior column is present. Due to these considerations, it appears safer to do the closed wedge resection osteotomy. In this series, only a few cases were seen with a loss of correction and in this series secondary kyphosis was only seen in the case where the instrumentation was removed. With this technique, loss of correction was always a result of implant failure either due to broken implants of loosening or migration of the screws.
During the observation period we had no cases with secondary proximal kyphosis at level above the end vertebra of the instrumentation. This is quite often seen in instrumented cases with osteopenia due to vertebral compression and this complication is difficult to address. Since we did not perform routine radiographs after 24 months, this complication could have occurred in our material without disclosure. On the other hand, all patients were under medical supervision by rheumatologist or their own doctors and clinical important late loss of correction would probably have been acknowledged.
The rate of neurological complications was generally low compared to the profound interventions when performing vertebral osteotomy. In this study, we had one case with a partial neurological deficit [6]. This was due to a technical problem with damage to the dura and shows the importance of respecting the delicate features of the nervous tissue. However, in patients with AS the dura is often extremely thin due to the chronic inflammation adherent to the surroundings, especially in the midline. It can therefore be extremely difficult to avoid leakages from the dura. There will thus always be a risk for the nervous tissue and due to that, the rate of neurological complication was found modest.
The general perioperative mortality in all kind of osteotomies for this condition was 4% in the literature (1.3% in closed wedge osteotomies) [6, 25]. We did not see any fatalities, which could be due to a higher safety of the closed wedge technique and the general evolution in perioperative care.
There was a high median blood loss in this series, and it is clear that this problem should be addressed. The operation time fell gradually during the period and this will probably also affect the blood loss in a positive direction. But a continuous effort to reduce the loss should be planned with improvement in hypotensive anesthesia focusing on positioning and hemostasis during the operation.
There are very few previous studies reporting outcome of surgery in AS [3, 5, 11, 16, 25]. Most studies have been technically oriented and have reported methods, complications and correction grades. One study [11] reported outcome using modified Arthritis Impact Measurement Scales (AIMS) [8] at follow-up with no preoperative registration. The conclusion of this study was thus based on the patient memorized considerations, which can be questionable.
This is the only study using newer outcome analysing tools which have become widespread used in general spine surgery. It is also to our knowledge the only study with prospective examination (before and after the surgery). The remarkable improvement in general function measured both by the Oswestry and the SF-36 method is to us, a validation of this type of surgery. However, not all of the cases were represented with a concurrent pre- and postoperative questionnaire. The primary cause of this was the long period of prospective follow-up, where the preoperative outcome instruments were not used as a routine at start. Furthermore, a few cases did not fill out the questionnaires preoperatively or their data was lost. In the follow-up, four patients refused to fill out the questionnaires, two of them because of poor cooperation. These patients answered in writing instead.
The outcome analysis of the patients with both preoperative and postoperative questionnaires filled out, still showed a highly significant improvement in their function and general health condition as measured by the SF-36. This difference shows the benefits of surgical treatment of this severe condition. Especially for the psychological part of SF-36 the result is interesting because the postoperative result is not very different from the normative data of the Danish standard population. This indicates a serious physiological effect of a kyphosis and how much this restricts the quality of life for this group of patients.
Conclusions
The thoracolumbar closed wedge pedicular resection osteotomy used in this series was a safe method for correction of incapacitating kyphosis in AS. There was an acceptable rate of perioperative complications and no mortality. The correction obtained was in average 45°. All the patients except one maintained their good correction and restored function.
Outcome analysis showed a significant improvement in SF-36 and Oswestry Disability Index, and the mental component showed improvement to values near the normative population.
It is concluded that corrective osteotomy of the thoracolumbar spine in AS is an effective and safe treatment with major possible improvements of life quality.
References
- 1.Abbott CA, Helliwell PS, Chamberlain MA. Functional assessment in ankylosing spondylitis: evaluation of a new self-administered questionnaire and correlation with anthropometric variables. Br J Rheumatol. 1994;33:1060–1066. doi: 10.1093/rheumatology/33.11.1060. [DOI] [PubMed] [Google Scholar]
- 2.Adams JC. Technique, dangers and safeguards in osteotomy of the spine. J Bone Joint Surg Br. 1952;34-B:226–232. doi: 10.1302/0301-620X.34B2.226. [DOI] [PubMed] [Google Scholar]
- 3.Bradford DS, Schumacher WL, Lonstein JE, Winter RB. Ankylosing spondylitis: experience in surgical management of 21 patients. Spine. 1987;2:238–243. doi: 10.1097/00007632-198704000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Camargo FP, Cordeiro EN, Napoli MM. Corrective osteotomy of the spine in ankylosing spondylitis. Experience with 66 cases. Clin Orthop Relat Res. 1986;208:157–167. [PubMed] [Google Scholar]
- 5.Chang KW, Chen YY, Lin CC, Hsu HL, Pai KC. Closing wedge osteotomy versus opening wedge osteotomy in ankylosing spondylitis with thoracolumbar kyphotic deformity. Spine. 2005;30(14):1584–1593. doi: 10.1097/01.brs.0000170300.17082.49. [DOI] [PubMed] [Google Scholar]
- 6.Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis inankylosing spondylitis: experience with 78 patients. Spine. 2001;26(16):E354–E360. doi: 10.1097/00007632-200108150-00010. [DOI] [PubMed] [Google Scholar]
- 7.Goel MK. Vertebral osteotomy for correction of fixed flexion deformity of the spine. J Bone Joint Surg Am. 1968;50-A:287–294. doi: 10.2106/00004623-196850020-00007. [DOI] [PubMed] [Google Scholar]
- 8.Halm H, Metz-Stevenhagen P, Zielke K. Results of surgical correction of kyphotic deformities of the spine in ankylosing spondylitis on the basis of the modified arthritis impact measurement scales. Spine. 1995;20:1612–1619. doi: 10.1097/00007632-199507150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hehne HJ, Zielke K, Böhm H. Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis. Report on 177 cases. Clin Orthop Relat Res. 1990;258:49–55. [PubMed] [Google Scholar]
- 10.Jaffray D, Becker V, Eisenstein S. Closing wedge osteotomy with transpedicular fixation in ankylosing spondylitis. Clin Orthop Relat Res. 1992;279:122–126. [PubMed] [Google Scholar]
- 11.Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine. 2002;27(6):612–618. doi: 10.1097/00007632-200203150-00010. [DOI] [PubMed] [Google Scholar]
- 12.Law WA. Osteotomy of the spine. Clin Orthop Relat Res. 1969;66:70–76. doi: 10.1097/00003086-196909000-00010. [DOI] [PubMed] [Google Scholar]
- 13.McMaster PE. Osteotomy of the spine for fixed flexion deformity. J Bone Joint Surg Am. 1962;44-A:1207–1216. [PubMed] [Google Scholar]
- 14.McMaster MJ. A technique for lumbar spinal osteotomy in ankylosing spondylitis. J Bone Joint Surg Br. 1985;67-B:204–210. doi: 10.1302/0301-620X.67B2.3980526. [DOI] [PubMed] [Google Scholar]
- 15.McMaster MJ, Coventry MB. Spinal osteotomy in ankylosing spondylitis: technique, complications, and long-term results. Mayo Clin Proc. 1973;48:476–487. [PubMed] [Google Scholar]
- 16.Niemeyer T, Hackenberg L, Bullmann V, Liljenqvist U, Halm H. [Technique and results of monosegmental transpedicular subtraction osteotomy inpatients with ankylosing spondylitis and fixed kyphotic deformity of the spine] Z Orthop Ihre Grenzgeb. 2002;140(2):176–181. doi: 10.1055/s-2002-31537. [DOI] [PubMed] [Google Scholar]
- 17.Simmons EH (1994) Relation of vascular complication to the level of lumbar extension osteotomy in ankylosing spondylitis. In: Presented at 61st Annual meeting of the American Academy of Orthopedic Surgeons, New Orleans
- 18.Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop Relat Res. 1977;128:65–77. [PubMed] [Google Scholar]
- 19.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg. 1945;27:1–11. [PubMed] [Google Scholar]
- 20.Thiranont N, Netrawichien P. Transpedicular decancellation closed wedge vertebral osteotomy for treatment of fixed flexion deformity of spine in ankylosing spondylitis. Spine. 1993;18:2517–2522. doi: 10.1097/00007632-199312000-00023. [DOI] [PubMed] [Google Scholar]
- 21.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–152. [PubMed] [Google Scholar]
- 22.Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br. 1995;77-B:117–121. [PubMed] [Google Scholar]
- 23.Royen BJ, Kleuver M, Slot GH. Polysegmental lumbar posterior wedge osteotomies for correction of kyphosis in ankylosing spondylitis. Eur Spine J. 1998;7:104–110. doi: 10.1007/s005860050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Royen BJ, Toussaint HM, Kingma I, Bot SDM, Caspers M, Harlaar J, et al. Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur Spine J. 1998;7:408–412. doi: 10.1007/s005860050098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Royen BJ, Gast A. Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis. 1999;58(7):399–406. doi: 10.1136/ard.58.7.399. [DOI] [PMC free article] [PubMed] [Google Scholar]