Abstract
Several studies have evaluated quantitative anatomic data for direct lateral mass screw fixation. To analyze anatomic landmarks and safe zones for optimal screw placement through the posterior arc of the human atlas, morphometric parameters of 41 adult native human atlas specimens were quantitatively measured. Internal dimensions of the atlas (lateral mass, maximum and minimum intraosseous screw length), minimum height and width of the posterior arc and optimal screw insertion angles were defined on pQCT scans. By this, an optimal posterior screw insertion point (OIP) and a preferable screw direction (PSD) through the posterior arch into the lateral mass of C1 were defined. External dimensions (transverse and sagittal diameter) as well as the width of the mid-portion of C1 lateral mass were significantly higher in male specimens. The mean height of the posterior arch at the vertebral artery groove was 4.1 ± 0.8 mm in female and 4.6 ± 0.9 mm in male specimens. The optimal screw insertion point was located 21.6 ± 1.7 mm in female and 23.6 ± 2.3 mm in male lateral from the posterior tubercle of C1 (P < 0.01). The preferable screw direction was a mean medial inclination of 7.9 ± 1.9° in female and 7.3 ± 2.7° in male specimens and a mean rostral direction of 2.4 ± 1.8° in female and 3.1 ± 1.7° in male specimens. In conclusion, the presented study provides information for the use and design of upper cervical spine instrumentation techniques, such as screw placement to C1 via the posterior arch. The characterization of working areas and safe zones (OIP, PSD) might contribute to a minimization of screw malposition in this highly demanding instrumentation technique.
Keywords: Atlas, Posterior screw placement, Transpedicular, Lateral mass
Introduction
Fusion of the occipitocervical or atlantoaxial spine is an accepted treatment option in upper cervical spine instability caused by trauma or various disorders [7, 8, 11, 16–18]. Posterior screw placement techniques to the atlas lateral mass have been recently introduced to avoid the inevitable loss of occipitocervical motion in occipitocervical fusion and to enable posterior C1–C2 fusion in patients who are not suitable for transarticular screw fixation due to anatomic variations, as for instance, of the vertebral artery [8, 9, 11, 18]. Goel reported the first clinical application of atlantal lateral mass screws in 1994 followed by description by Harms of a posterior C1–C2 fusion technique with a polyaxial screw and rod fixation system in 2001 [7, 8]. To support this technique, during the last years pertinent anatomic data for C1 lateral mass screw placement has been gained [1–6, 9, 10, 18–21]. Biomechanical studies have demonstrated that C1 lateral mass screws in conjunction with C2 pedicle screws achieve a similar biomechanical stability of the atlantoaxial fusion as compared with Magerl’s technique [15, 18].
To further improve posterior C1–C2 fusion techniques, some recent publications evaluated the application of screws to C1 via the posterior arch [12–14, 20]. Two of these studies focused on a morphometric characterization of the atlas to minimize intraoperative malposition of the so-called C1 ‘pedicle screws’ (Fig. 1) [13, 20]. However, these studies explicitly differ in the results concerning some key anatomic measurements, necessitating an additional evaluation of anatomic landmarks and safe zones for the screw placement through the posterior arch of C1.
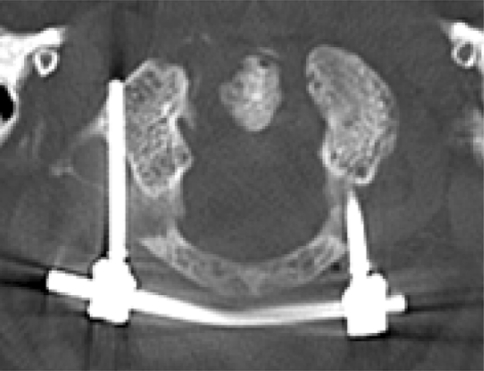
Fig. 1.
Postoperative horizontal CT image of the atlas of a 78-year-old woman who sustained an unstable non-displaced Gehweiler type III fracture. Notice the malposition of the right screw crossing the transverse foramen
Materials and methods
Specimens
This study was carried out according to the existing rules and regulations of Hamburg University School of Medicine. All patients had died in accidents or of acute diseases.
The complete atlas was removed from 41 adult patients aged 18–88 years at autopsy (20 female specimens, mean age 52.2 ± 20.5 years; 21 male specimens, mean age, 48.1 ± 15.9). All specimens were dissected free of all soft tissue following maceration in hydrogen peroxide solution for 72 h. Multiple morphometric measurements of the atlas specimens were taken using a digital caliper and goniometer (see below).
Peripheral quantitative computed tomography
For all 41 atlas specimens, Peripheral quantitative computed tomography (pQCT) sectional images were established and evaluated using an automated computer routine (XCT960, Stratec, Pforzheim, Germany). Scans were performed in the horizontal and sagittal plane and for determination of the height of the posterior arch in the frontal plane at the thinnest portion, located underneath the vertebral artery groove (Fig. 2). Inner dimensions of the atlas (lateral mass, maximum and minimum intraosseous screw length), minimum height and width of the posterior arc and optimal screw insertion angles through the posterior arch were defined on the scans. By this, an optimal posterior screw insertion point [(OIP), i.e. the distance from the posterior tubercle of C1 to the screw entry point (D8)] and a preferable screw direction (PSD) into the lateral mass of C1 [i.e., the optimal direction angle of screw projection through the posterior arch (A3)] were defined.
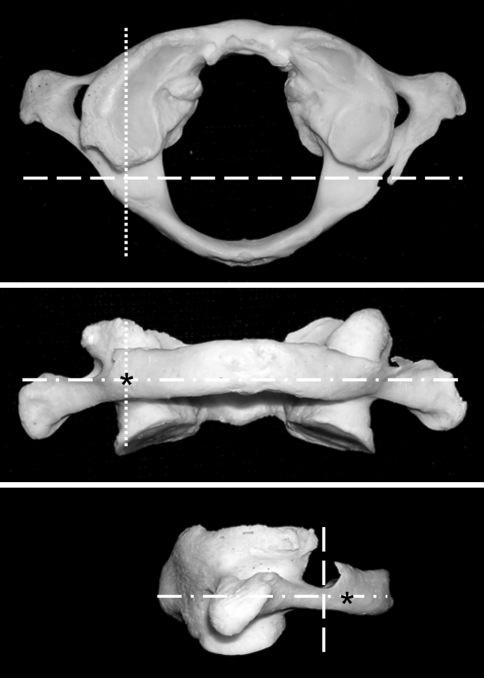
Fig. 2.
Cranial, posterior and lateral macroscopic views of a C1 specimen following maceration in hydrogen peroxide solution. PQCT scans were performed in the horizontal (white dashed/dotted line), sagittal (white dotted line) and frontal plane at the vertebral artery groove (white dashed line). The optimal screw insertion point is marked with a black asterisk
Morphometric measurements
The following morphometric measurements of the C1 specimens and the pQCT sectional images were taken (Figs. 3, 4, 5): transverse diameter of C1 (D1), sagittal diameter of C1 (D2), width of the posterior arch at the vertebral artery groove (D3), height of the posterior arch at the vertebral artery groove (D4), length of the C1 lateral mass (D5), width of the mid-portion of the C1 lateral mass (D6), height of the mid-portion of the C1 lateral mass (D7), distance from the posterior tubercle of C1 to the screw entry point (D8), length of screw projection through the posterior arch of C1 (D9), length of screw projection through the lateral mass of C1 (D10), maximum medial direction angle of screw projection (A1), maximum lateral direction angle of screw projection (A2), optimal direction angle of screw projection through the posterior arch (A3), rostral direction of screw projection through the posterior arch (A4), medial inclination angle of the cranial facet of C1 (A5), medial inclination angle of the caudal facet of C1 (A6).
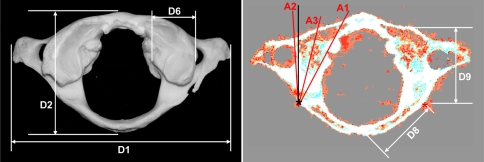
Fig. 3.
Cranial macroscopic view (left panel) and corresponding horizontal pQCT sectional image (right panel) of a dissected specimen. D1 transverse diameter, D2 sagittal diameter, D6 width of mid-portion of C1 lateral mass, D8 distance from posterior tubercle to optimal screw insertion point (OIP, marked with a black asterisk); D9 length of screw projection through posterior arch of C1; A1 maximum medial direction angle of screw projection; A2 maximum lateral direction angle of screw projection A3 optimal direction angle of screw projection through the posterior arch
Fig. 4.
Posterior macroscopic view (left panel) and corresponding frontal pQCT sectional image through the posterior arch of C1 at the vertebral artery groove (right panel) of a dissected specimen. D3 width of the posterior arch at the vertebral artery groove; D4 height of the posterior arch at the vertebral artery groove, D7 height of mid-portion of C1 lateral mass, D8 distance from the posterior tubercle to optimal screw insertion point, red dotted line (OIP, marked with a black asterisk); A5 medial inclination angle of the cranial facet of C1; A6 medial inclination angle of the caudal facet of C1
Fig. 5.
Lateral macroscopic view (left panel) and corresponding sagittal pQCT sectional image at the optimal screw insertion point (right panel) of a dissected specimen. D5 length of the C1 lateral mass; D9 length of screw projection through the posterior arch of C1; D10 length of screw projection through the lateral mass; optimal screw insertion point (OIP) marked with a black asterisk; A4 rostral direction of screw projection through the posterior arch
Statistical analysis
Statistical significance of the morphometric data was determined by the use of a Student’s t test at a 95% level of significance. A P value of < 0.05 was considered to be significant and a P value of <0.01 highly significant.
Results
As much as 41 human adult C1 specimens were studied. For each specimen, measurements were performed for the left and the right region of the atlas vertebra, and the mean of these two measurements was calculated for further statistical analysis. The mean value, standard deviation and range of the morphometric measurements are listed in Table 1 according to gender.
Table 1.
Summary of the morphometric measurements of 41 atlas specimens
| Parameters | Female | Male | ||
|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | |
| Age (years) | 52.2 ± 20.5 | 20–88 | 48.1 ± 15.9 | 18–74 |
| Weight (kg) | 66.2 ± 15.0** | 40.4–91.6 | 84.8 ± 14.2 | 59.8–118.0 |
| Height (m) | 1.66 ± 0.07** | 1.55–1.75 | 1.78 ± 0.09 | 1.61–1.97 |
| D1 (mm) | 74.2 ± 4.5** | 65.0–84.0 | 82.8 ± 4.6 | 72.0–93.0 |
| D2 (mm) | 44.8 ± 2.5** | 39.0–49.0 | 49.6 ± 3.7 | 46.0–61.0 |
| D3 (mm) | 8.9 ± 0.7* | 7.8–10.3 | 9.8 ± 1.7 | 6.8–12.4 |
| D4 (mm) | 4.1 ± 0.8 | 2.9–6.0 | 4.6 ± 0.9 | 2.8–6.6 |
| D5 (mm) | 17.6 ± 1.7 | 14.0–20.0 | 18.3 ± 1.3 | 16.2–21.0 |
| D6 (mm) | 13.9 ± 1.2** | 12.1–16.8 | 15.2 ± 1.3 | 13.2–17.9 |
| D7 (mm) | 11.3 ± 1.1 | 9.8–14.0 | 11.8 ± 1.2 | 10.1–14.1 |
| D8 (mm) | 21.6 ± 1.7** | 17.8–24.0 | 23.6 ± 2.3 | 18.2–27.9 |
| D9 (mm) | 28.0 ± 1.9 | 25.4–31.6 | 28.9 ± 1.8 | 25.8–32.8 |
| D10 (mm) | 17.6 ± 1.7 | 14.0–20.0 | 18.3 ± 1.3 | 16.2–21.0 |
| A1 (°) | 22.6 ± 3.1 | 16.0–30.0 | 23.9 ± 3.6 | 18.0–32.0 |
| A2 (°) | −6.6 ± 3.0** | −14.0–−2.0 | −9.7 ± 3.0 | −16.0–−4.0 |
| A3 (°) | 7.9 ± 1.9 | 5.0–12.0 | 7.3 ± 2.7 | 3.0–13.0 |
| A4 (°) | 2.4 ± 1.8 | 0–5.6 | 3.1 ± 1.7 | 0–6.0 |
| A5 (°) | 26.8 ± 5.2 | 20.0–38.0 | 30.0 ± 5.0 | 18.0–40.0 |
| A6 (°) | 22.8 ± 3.9 | 15.0–28.0 | 25.0 ± 4.9 | 12.0–32.0 |
The data are specified as mean value ± SD; a P value of < 0.05 (*) was considered to be significant, and a P value < 0.01 (**) was highly significant
As expected, the mean body weight as well as the mean body height was significantly higher in male specimens (P < 0.01) compared to the female specimens. The transverse (D1) as well as the sagittal (D2) diameters of C1, the width of the posterior arch at the groove of the vertebral artery (D3) and the width of the mid-portion of the C1 lateral mass (D6) were significantly lower (D1, D2, D6: P < 0.01; D3: P < 0.05) in the female specimens (Figs. 3, 4). The mean height of the posterior arch at the vertebral artery groove (D4) was also lower in the female specimens (4.1 ± 0.8 vs. 4.6 ± 0.9 mm); nevertheless, this difference was not of statistical significance. In 8 (5 female and 3 male) of the 41 specimens (19.5%), the height of the posterior arch at the vertebral artery groove was lower than 3.5 mm and in 13 (8 female and 5 male) of the 41 specimens (31.7%) lower than 4.0 mm. The optimal screw insertion point (OIP, black asterisk in Figs. 2, 3, 4, 5) for C1 instrumentation through the posterior arch was located 2.0 mm cranial from the inferior border of the posterior arch, and 21.6 ± 1.7 mm in female and 23.6 ± 2.3 mm in male lateral from the posterior tubercle of C1 (D8, Fig. 4). This difference between the female and the male group was highly significant (P < 0.01). Regarding the intraosseous screw length, the mean length of the screw projection through the posterior arch of C1 (D9; 28.0 ± 1.9 mm in female, 28.9 ± 1.8 mm in male) was about 10 mm longer than the screw projection through the lateral mass of C1 (D10; 17.6 ± 1.7 mm in female, 18.3 ± 1.3 mm in male). Starting at the optimal screw insertion point, the preferable screw direction (PSD) was a mean medial inclination (A3) of 7.9 ± 1.9° in female and 7.3 ± 2.7° in male specimens (Fig. 3), and a mean rostral direction (A4) of 2.4 ± 1.8° in female and 3.1 ± 1.7° in male specimens (Fig. 5). The maximum lateral direction angle of the screw projection through the posterior arch (A2) was significantly higher in male specimens as compared to female specimens (P < 0.01).
Discussion
Current posterior fixation techniques at the upper cervical spine might include C1 lateral mass screws as well as stabilization techniques through the posterior arch of C1. Regarding the biomechanical characteristics of C1–C2 instrumentation techniques, recent investigations proved that C1 lateral mass screws in conjunction with C2 pedicle screws achieved a similar stability compared with Magerl’s C1–C2 transarticular screw fixation technique [15, 18].
Unicortical and bicortical lateral mass screws are inserted into the atlas directly underneath the base of the posterior arch. Even though bicortical C1 lateral mass screws have a higher pullout strength than unicortical lateral mass screws, one has to consider the potential risk of an injury of the hypoglossal nerve or the internal carotid artery from a bicortical screw [2, 6]. Screws inserted through the posterior arch of C1 into the lateral mass have a longer trajectory compared to lateral mass screws. Due to this, the so-called ‘pedicle screws’ inserted through the posterior arch of C1 have a superior biomechanical stability than lateral mass screws [14]. In addition to the larger pullout strength of screws placed through the posterior arch into C1, a main argument for preferring this instrumentation technique is to avoid an excessive venous bleeding from the venous plexus around the C2 root during the classical subarcuate procedure during the placement of lateral mass screws.
To elucidate the anatomical conditions for the instrumentation technique through the posterior arch, in two recent studies by Tan and Ma, morphometric measurements of 50 human C1 specimens of Asian origin were performed independently [13, 20]. Both researchers concluded that a screw placement through the posterior arch of C1 was possible, and they defined anatomic landmarks to reduce the risk of intraoperative malposition of these screws. Unfortunately, the results of Tans’s study significantly differ from those of Ma’s, though both researchers focused on an equal number of adult C1 specimens of Asian origin. Tan recommended a screw entry point 19.01 mm lateral from the midline, and he suggested the direction of screw trajectory to be perpendicular and about 5° cephalad to the transverse plane. In his study, the mean height of the posterior arch at the vertebral artery groove was 4.58 mm on the left and 4.72 mm on the right side [20]. On the contrary, Ma’s anatomic considerations for the screw placement through the posterior arch to C1 determined the distance from the screw entry point to the midline of C1 to be 22.15 mm [13]. Ma proposed a medial inclination of the screw trajectory by about 10°, to enhance the safety of the procedure and to avoid vertebral artery injury in the C1 transverse foramen (Fig. 1). Additionally, one has to assume that a more medial screw direction might protect the internal carotid artery and the hypoglossal nerve, which are located in close proximity to the anterior aspect of C1 [2, 6]. Ma measured a mean height of the posterior arch at the vertebral artery groove of 5.83 ± 0.75 mm. None of these two investigations determined a safe sector for a preferable screw direction in the horizontal or the sagittal plane of C1.
Obviously, none of the two studies distinguished between male and female specimens, though C1 exhibits significant sex-related geometrical differences (e.g., transverse and sagittal diameters, Table 1). Thus, to specify sex-related differences of anatomic landmarks for a safe instrumentation technique via the posterior arch into C1, the presented study was performed.
In our study, the average width of the posterior arch of C1 at the groove of the vertebral artery (D3) was 8.9 mm in the female and 9.8 mm in the male specimens. Thus, the mediolateral width could accommodate a 3.5 or 4-mm screw. In contrast, the mean height of the posterior arch of C1 underneath the groove of the vertebral artery (D4) was 4.1 mm in the female and 4.6 mm in the male specimens. This would be sufficient to accommodate at least a 3.5-mm screw. Nevertheless, in our study the height of the posterior arch of C1 underneath the groove of the vertebral artery (D4) was lower than 3.5 mm in eight (19.5%) and lower than 4.0 mm in 13 of the 41 specimens (31.7%). In Tan’s study, the same parameter averaged 4.65 mm, and in 8% of his specimens it was lower than 4.0 mm [20].
The internal dimensions of the lateral mass of the atlas (D5–D7) were much more than 9.8 mm, and for this reason would easily allow the placement of a 3.5-mm screw.
The optimal screw insertion point (OIP) was located 21.6 mm in female and 23.6 mm in male specimens, lateral from the posterior tubercle of C1, which is in line with Ma’s results [13]. From this insertion point on the safe zone, for a secure intraosseous screw, the direction through the posterior arch was specified, which has not been performed in previous studies. On average, the sector comprised 29.2° (−6.6° to 22.6°) in female specimens and 33.6° (−9.7° to 23.9°) in male specimens. To avoid malposition of the screw medial into the spinal canal or lateral into the transverse foramen, the preferable screw direction (PSD) should be determined. The preferable medial inclination of the screw was determined to be 7.9 ± 1.9° in female and 7.3 ± 2.7° in male specimens. Furthermore, the screw should be inserted at the OIP in a slightly cephalad direction (A4) of 2.4 ± 1.8° in female and 3.1 ± 1.7° in male specimens to achieve a central orientation of the screw within the lateral mass.
In summary, the presented characterization of working areas and safe zones for the posterior instrumentation technique to C1 via the posterior arch provides information, which might contribute to an increased accuracy of this highly demanding instrumentation technique. Additionally, to further minimize the risk of an intraoperative lesion of neurovascular structures by a malpositioned screw, one has to recommend a preoperative CT study of the upper cervical spine to show the course of the internal carotid and the vertebral artery, as well as the hypoglossal nerve.
Acknowledgments
The manuscript submitted does not contain information about medical devices or drugs. No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article.
Footnotes
M. Gebauer and F. Barvencik contributed equally to this study and therefore share the first authorship.
References
- 1.Christensen DM, Eastlack RK, Lynch JJ, Yaszemski MJ, Currier BL. C1 anatomy and dimensions relative to lateral mass screw placement. Spine. 2007;32:844–848. doi: 10.1097/01.brs.0000259833.02179.c0. [DOI] [PubMed] [Google Scholar]
- 2.Currier BL, Maus TP, Eck JC, Larson DR, Yaszemski MJ. Relationship of the internal carotid artery to the anterior aspect of the C1 vertebra: implications for C1–C2 transarticular and C1 lateral mass fixation. Spine. 2008;33:635–639. doi: 10.1097/BRS.0b013e318166e083. [DOI] [PubMed] [Google Scholar]
- 3.Doherty BJ, Heggeness MH. The quantitative anatomy of the atlas. Spine. 1994;19:2497–2500. doi: 10.1097/00007632-199411001-00001. [DOI] [PubMed] [Google Scholar]
- 4.Dong Y, Xia Hong M, Jianyi L, Yuan Lin M. Quantitative anatomy of the lateral mass of the atlas. Spine. 2003;28:860–863. doi: 10.1097/00007632-200305010-00004. [DOI] [PubMed] [Google Scholar]
- 5.Ebraheim NA, Xu R, Ahmad M, Heck B. The quantitative anatomy of the vertebral artery groove of the atlas and its relation to the posterior atlantoaxial approach. Spine. 1998;23:320–323. doi: 10.1097/00007632-199802010-00007. [DOI] [PubMed] [Google Scholar]
- 6.Eck JC, Walker MP, Currier BL, Chen Q, Yaszemski MJ, An KN. Biomechanical comparison of unicortical versus bicortical C1 lateral mass screw fixation. J Spinal Disord Tech. 2007;20:505–508. doi: 10.1097/BSD.0b013e318031af8b. [DOI] [PubMed] [Google Scholar]
- 7.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002;51:1351–1357. doi: 10.1097/00006123-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 9.Hong X, Dong Y, Yunbing C, Qingshui Y, Shizheng Z, Jingfa L. Posterior screw placement on the lateral mass of atlas: an anatomic study. Spine. 2004;29:500–503. doi: 10.1097/01.BRS.0000113874.82587.33. [DOI] [PubMed] [Google Scholar]
- 10.Lee MJ, Cassinelli E, Riew KD. The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine. 2006;31:2798–2801. doi: 10.1097/01.brs.0000245902.93084.12. [DOI] [PubMed] [Google Scholar]
- 11.Levine AM, Edwards CC. Fractures of the atlas. J Bone Joint Surg Am. 1991;73:630–691. [PubMed] [Google Scholar]
- 12.Li L, Wang H, Cui S. Application of atlas pedicle screw system fixation and fusion for treatment of upper cervical disease. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2007;21:461–464. [PubMed] [Google Scholar]
- 13.Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ. Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine. 2005;30:1519–1523. doi: 10.1097/01.brs.0000168546.17788.49. [DOI] [PubMed] [Google Scholar]
- 14.Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Xiang M, Zhao WD, Zhong SZ. C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine. 2009;34:371–377. doi: 10.1097/BRS.0b013e318193a21b. [DOI] [PubMed] [Google Scholar]
- 15.Melcher RP, Puttlitz CM, Kleinstueck FS, Lotz JC, Harms J, Bradford DS. Biomechanical testing of posterior atlantoaxial fixation techniques. Spine. 2002;27:2435–2440. doi: 10.1097/00007632-200211150-00004. [DOI] [PubMed] [Google Scholar]
- 16.Oda I, Abumi K, Sell LC, Haggerty CJ, Cunningham BW, McAfee PC. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine. 1999;24:2377–2382. doi: 10.1097/00007632-199911150-00015. [DOI] [PubMed] [Google Scholar]
- 17.Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the C1–C2 complex for pedicle screw fixation. Spine. 2002;27:1494–1498. doi: 10.1097/00007632-200207150-00003. [DOI] [PubMed] [Google Scholar]
- 18.Richter M, Schmidt R, Claes L, Puhl W, Wilke HJ. Posterior atlantoaxial fixation: biomechanical in vitro comparison of six different techniques. Spine. 2002;27:1724–1732. doi: 10.1097/00007632-200208150-00008. [DOI] [PubMed] [Google Scholar]
- 19.Rocha R, Safavi-Abbasi S, Reis C, Theodore N, Bambakidis N, Oliveira E, Sonntag VK, Crawford NR. Working area, safety zones, and angles of approach for posterior C-1 lateral mass screw placement: a quantitative anatomical and morphometric evaluation. J Neurosurg Spine. 2007;6:247–254. doi: 10.3171/spi.2007.6.3.247. [DOI] [PubMed] [Google Scholar]
- 20.Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, Wei H, Yang F. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine. 2003;28:888–895. doi: 10.1097/00007632-200305010-00010. [DOI] [PubMed] [Google Scholar]
- 21.Wang MY, Samudrala S. Cadaveric morphometric analysis for atlantal lateral mass screw placement. Neurosurgery. 2004;54:1436–1440. doi: 10.1227/01.NEU.0000124753.74864.07. [DOI] [PubMed] [Google Scholar]