Abstract
Vertebral endplate signal changes (VESC), also known as Modic changes, have been reported to be associated with low back pain (LBP). However, little is known about predisposing factors for the development of new VESC. The aim of this study was to investigate the predictive value of lifestyle factors and disc-related magnetic resonance imaging (MRI) findings in relation to the development of new VESC. This prospective observational study included 344 people from the Danish general population who had an MRI and completed LBP questionnaires at the age of 40 and again at 44 years. Potential predictors of new VESC were female gender, disc-related MRI findings (disc degeneration, disc bulges, disc herniation, and other endplate changes) and lifestyle factors [high physical work or leisure activity, high body mass index (BMI), and heavy smoking]. Bivariate and multivariate logistic regressions were used to identify predictors of new VESC. New VESC at the age of 44 appeared in 67 of the 344. The majority (84%) of these new signal changes were type 1 VESC and almost half (45%) were only in the endplate and did not extend into the vertebral body. In the multivariate analysis, lumbar disc levels with disc degeneration, bulges or herniations at 40 were the only predictors of new VESC at age 44. Therefore, the development of new VESC at the age of 44 appears to be based on the status and dynamics of the disc, rather than being the result of gender or lifestyle factors such as smoking and physical load.
Keywords: Endplate (Modic) changes, Magnetic resonance imaging, General population, Predictors, Lumbar spine
Introduction
Vertebral endplate signal changes (VESC), also known as Modic changes [28], have been reported to be associated with low back pain (LBP) in people from the general [18], working [21, 35], and clinical populations [2, 5, 6, 13, 43]. Seven out of ten studies included in a recent systematic review displayed significant positive associations between VESC and LBP, with odds ratios (OR) ranging from 2.0 to 20 [16].
Although the literature shows that the prevalence of VESC increases after a (symptomatic) disc herniation, little is known about the aetiology of this condition [2, 3, 20]. Therefore, there is a need to study possible predisposing factors for the development of VESC.
In a descriptive study of VESC, Modic et al. [28] investigated 474 patients referred for lumbar magnetic resonance imaging (MRI). They described two types of signal changes: type 1 seen as hypointensity on T1-weighted images and hyperintensity on T2, and type 2 seen as hyperintensity on both T1 and T2-weighted images. Later, type 3 was described as hypointensity on T1- and T2-weighted images representing sclerosis as seen on radiographs [27]. On the basis of further investigation it was established that type 1 changes could be the initial “destructive” stage with histological samples showing fissured endplates and vascular granulation tissue adjacent to the endplates whereas type 2 changes indicated the “regenerative” stage as fatty degeneration of the adjacent bone marrow were identified in the histological samples [28]. The two stages can co-exist in the same vertebra and the boundaries between the two are not always distinct [5, 15, 20].
How and why the initial type 1 stage occurs is not clear. One explanation is that disruption of the internal architecture of the disc causes increased loading and leads to micro fractures of the endplates. However, not all people with a degenerated disc develop VESC. It may be that there are other influential factors, such as gender, physical work load, level of leisure activity, and body weight, which can affect the loading of the lumbar spine [11, 24, 25]. Moreover, vertebral bone strength in adults is influenced by gender and smoking [12, 37, 38].
Therefore, the purpose of this study was to investigate whether: (1) increased loading of the spine [high physical work activity, high physical leisure activity, high body mass index (BMI)], (2) decreased vertebral bone strength (female gender, heavy smoking), and (3) MRI findings (disc degeneration, bulges and herniations) are predictors for the development of new lumbar spine VESC.
Materials and methods
Study sample
In this prospective longitudinal study, people sampled from the Danish general population had a MRI-scan and completed LBP questionnaires at the age of 40 (in 2000/2001) and again at age 44. Details of the original study cohort have been previously described [18].
Permission for the study was granted by the local ethics committee (ref. no. 20000042) and for the database by the Danish Data Protection Agency (ref. no. 2000-53-0037).
MRI
Magnetic resonance imaging was performed with a 0.2 T MRI-system (Magnetom Open Viva; Siemens AG, Erlangen, Germany). A body spine surface coil was used with the participants in the supine position. The following sequences were used:
A localizer sequence of five images, 40°/10°/40° (TR/TE/flip angle) consisting of two coronal and three sagittal images in orthogonal planes
Sagittal T1-weighted spin echo, 621/26 (TR/TE), 144 × 256 matrix, 300 mm field of view, 11 slices of 4 mm thickness, 2 acquisitions, 6 min 1 s scan time
Sagittal T2-weighted turbo spin echo 4609/134 (TR/effective TE), 210 × 256 matrix, 300 mm field of view, 11 slices of 4 mm thickness, 2 acquisitions, 8 min 42 s scan time
Axial T2-weighted turbo spin echo 6415/134 (TR/effective TE), 180 × 256 matrix, 250 mm field of view, 15 slices of 5 mm thickness, 2 acquisitions, 7 min 49 s scan time. Slices were placed in the planes of the five lower discs.
The MRI evaluation was performed by a musculoskeletal radiologist and two chiropractors with extensive MRI experience using standardized evaluation protocols [17, 39]. VESC was evaluated according to the Nordic Modic Consensus Group classification [17]. Definitions of the other MRI variables are included in Table 1. The evaluation protocols used in this study have been shown to result in substantial to almost perfect reproducibility for the evaluation of MRI findings, with Kappa values for intra- and inter-observer reproducibility ranging from 0.78 to 1.0 and 0.66 to 0.91, respectively [17, 19, 39].
Table 1.
Definitions and prevalence of potential predictors of new VESC at the age of 44 in 1720 disc levels in 344 people from the Danish general population
| Predictor variables at age 40 | Definition | Prevalence |
|---|---|---|
| Number of people (%) | ||
| Female gender | Female | 183 (53%) |
| High physical work activity (yes/no) | Heavy physical work, heavy lifting either now or previously [22] | 101 (29%) |
| High physical leisure activity (yes/no) | Active in sports/hard physical load in leisure time activity at least 3 h/week or participating in competitive sports [22] | 129 (38%) |
| High BMI (>25) | Body mass index above 25, based on self-reported height and weight [weight (kg)/height (m)2] | 140 (41%) |
| Heavy smoking (yes/no) | More than 20 cigarettes a day [32] | 57 (17%) |
| Predictor variables at age 40 | Definition | Prevalence |
|---|---|---|
| Number of people (%) | ||
| Disc level (upper/lower) | Upper lumbar (L1/2–L3/4) | 1,032 (60%) |
| Lower lumbar (L4/5–L5/S1) | 688 (40%) | |
| Disc degeneration (yes/no) | Defined as a hypointense disc (grade 3) [8, 42] or reduced disc height (grades 2 or 3) [31, 33, 42] | 375 (22%) |
| Bulging disc (yes/no) | Bulging disc [9] | 192 (11%) |
| Disc herniations (yes/no) | Protrusions, extrusions, and sequestrations [9] | 108 (6%) |
| Endplate changes (yes/no) | Irregular endplates, Schmorl’s nodes, and/or local defects [41] | 140 (8%) |
Variables of interest and the rationale for their choice
The following MRI findings and lifestyle factors (Table 1) were investigated for the reasons described below:
Gender and lifestyle
Female gender: women are often subjected to lower physical loads at work and are more active in their leisure time than men [11]. Women have lower bone strength than men [37].
High physical work activity: heavy physical loading is a risk factor for injury to vertebral bone and/or disc [25].
High physical leisure activity: see rationale for item 2.
High BMI: excessive body weight may accelerate the development of disc degeneration and/or delay its recovery [24]. Also, see rationale for item 2.
Heavy smoking: heavy smoking may reduce the strength of the vertebral bone, thus accelerating the development of VESC or delaying healing [10, 14, 30].
MRI findings
Disc level: the lower part of the lumbar spine (L4/5–L5/S1) is subjected to greater load than the upper part, and thus is more prone to repetitive stress/injury [4].
Disc degeneration: disc degeneration leads to abnormal load forces [1] that can be transmitted to the endplate and make it more prone to injury.
Disc contour: disc bulges and herniations represent advanced degeneration and/or acute injury to the discovertebral junction [36], and are likely to be accompanied by abnormal load forces of the endplate, increasing the risk of injury.
Endplate changes: injury to the vertebral endplate can lead to abnormal load forces in the disc [1].
Data analysis
The current study included only people who were scanned and completed the questionnaires at both points in time. A drop-out analysis was performed between people who participated in the study at both the age of 40 and 44 (responders) and those who only participated in the original study at age 40 (non-responders). The proportions of the following baseline variables were analysed at age 40: gender, presence of VESC, disc contour, disc degeneration, spondylolisthesis, LBP, heavy smoking, heavy physical workload, BMI, highest educational level, employment status, and the back beliefs questionnaire score.
All predictor data were transformed into variables for each lumbar level (L1/2–L5/S1) and descriptively reported. Differences in prevalence rates were examined using McNemar’s test of symmetry. People or disc levels with new VESC at the age of 44 were defined as such if VESC of any type or size had not been visualized on the MRI taken at age 40. Logistic regression analysis was used to determine which variables were predictors for the occurrence of new VESC at age 44. A single regression model included the five disc levels from all participants. Potential predictors were dichotomized at predetermined relevant cut-points (Table 1). Because of the limited number of events (new VESC at age 44), the number of predictor variables in the multivariable analysis was limited to those with a p value below 0.05 in the bivariate analyses. Data were analysed with STATA 10.1 (StataCorp, College Station, TX, USA) and to account for the dependency of disc levels within people, the cluster-option in STATA was used in the regression analyses. Associations were expressed as OR. OR for which the 95% confidence interval (CI) did not include 1 were considered significant.
Results
Study sample
Eighty-three percent (n = 344, 161 men and 183 women) of the original cohort of 412 people (199 men and 213 women) had an MRI and completed the questionnaires at the age of 44 and were included in the present study. In the drop-out analysis, the only significant difference between non-responders (n = 68) and those who participated in the follow-up study was their employment status. Nineteen percent of the non-responders were unemployed as compared with only 7% among those who participated in the follow-up study.
Descriptive data
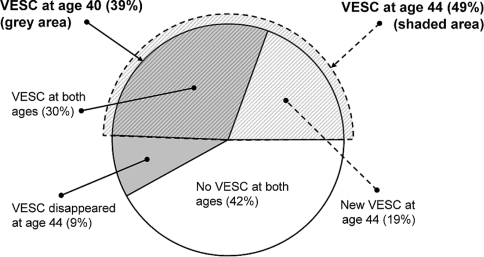
The prevalence of VESC increased from the age of 40–44. The number of people with VESC increased by 37 from 133 (39%) to 170 (49%) (p < 0.001) (see Fig. 1). New VESC had developed in 67 (19%) people at the time of the follow-up, whereas 42% did not have VESC at both points in time.
Fig. 1.
The proportion of persons with VESC at the age 40 (grey area) and age 44 (shaded area) in 344 persons from the Danish general population
New VESC appeared in 141 (8%) of all 1720 disc levels. The majority (84%) of these signal changes were VESC of type 1 and almost half (45%) were observed only in the endplate and did not extend into vertebral body. The prevalence rates of the potential risk factors are shown in Table 1.
Predictors of new VESC at age 44
The results of the bivariate analyses indicate that disc degeneration, bulges, and herniations were associated with the development of new VESC over time and were therefore included in the multivariate analysis (Table 2). Disc level, endplate changes, physical work load, leisure activity, BMI, and smoking failed to reach significance in the bivariate analyses.
Table 2.
The number of disc levels with new VESC at age 44, and the association of potential predictors for VESC at 44 expressed as odds ratios from bivariate analysis of 1720 disc levels in 344 people from the Danish general population
| Outcome variable | Prevalence No. of discs |
New VESC (any type) at age 44 | ||
|---|---|---|---|---|
| No (n = 1579) | Yes (n = 141) | Odds ratios (95% CI) | ||
| Gender (women)a | 915 (53%) | 851 (54%) | 64 (45%) | 0.7 (0.5–1.0) |
| High physical work activity (yes)a | 505 (29%) | 456 (29%) | 49 (35%) | 1.3 (0.9–2.0) |
| High physical leisure activity (yes)a | 645 (38%) | 588 (37%) | 57 (40%) | 1.1 (0.8–1.7) |
| High BMI (>25)a | 700 (41%) | 631 (40%) | 69 (49%) | 1.4 (0.9–2.1) |
| Heavy smoking (yes)a | 285 (17%) | 265 (17%) | 20 (14%) | 0.8 (0.5–1.4) |
| Disc level (lower) | 688 (40%) | 621 (39%) | 67 (48%) | 1.4 (0.9–2.0) |
| Disc degeneration (yes) | 375 (22%) | 310 (20%) | 65 (46%) | 3.5 (2.4–5.1) |
| Bulging disc (yes) | 192 (11%) | 160 (10%) | 32 (23%) | 2.6 (1.7–3.9) |
| Disc herniations (yes | 108 (6%) | 87 (6%) | 21 (15%) | 3.0 (1.8–4.9) |
| Endplate changes (yes) | 140 (8%) | 121 (8%) | 19 (14%) | 1.9 (1.1–3.3) |
Odds ratios in bold are significant at the 0.05 level, see data analysis
aFor the variables gender, high physical work activity, high physical leisure activity, BMI > 25, and heavy smoking, the number of people were multiplied by five to get the number of disc levels that were potentially influenced by each of these factors
In the multivariate analysis, disc levels with disc degeneration, bulges or herniations at 40 had twice the odds of new VESC occurring at age 44 compared with disc levels with normal disc contours or no degeneration (Table 3).
Table 3.
Odds ratios (95% CI) of possible predictors of new VESC at age 44 in 1720 disc levels in 344 people from the general Danish population
| Predictor variables at the age of 40 | Odds ratio (95% CI) |
|---|---|
| Disc degeneration (yes/no) | 2.5 (1.6–4.0) |
| Bulging disc (yes/no) | 1.7 (1.04–2.9) |
| Disc herniations (yes/no) | 2.1 (1.1–3.7) |
Results from multivariable logistic regression analysis
Discussion
This is the first study to investigate whether increased loading of the spine, risk factors of decreased vertebral bone strength and disc-related MRI findings are predictors in the development of new VESC in people from the general population. The main finding was that disc-related MRI findings (i.e. degeneration, bulges and herniations) at age 40 were predictive of new VESC 4 years later. Gender, disc level, endplate changes and all of the lifestyle factors (high physical work activity, high physical leisure activity, high BMI or heavy smoking) did not predict the development of new VESC. In other words, the development of new VESC at the age of 44 seems to be pre-programmed, based on the status and dynamics of the disc, rather than being the result of any of the lifestyle factors measured at the age of 40.
That disc-related MRI findings predict new VESC and lifestyle factors and gender do not, is in line with the results from two previous studies of patients with sciatica treated non-surgically. In a Finnish study of 60 patients with sciatica, who had MRI-scans at baseline and 3 years later, the development of new VESC at follow-up was not predicted by physical work load or age. Rather, they were located at the L5/S1 level and co-localized with symptomatic disc herniations [20]. In a Danish study of 166 patients with sciatica, who had MRI-scans at baseline and after 14 months, all new VESC at follow-up were located at the same level as the symptomatic disc herniations at baseline [2].
The association between disc degeneration/bulges/herniations and the development of new VESC may involve multiple pathoanatomic pathways that could be either slow- or fast-acting.
The first possibility is that the disc is degenerated (degeneration and/or bulges) and the internal architecture of the disc has changed. In such cases, the damaged disc cells produce mediators that can stimulate inflammation and tissue degradation in the disc and adjacent bone marrow [34]. In addition, changes in the internal architecture of the disc have been reported to produce peak forces within the disc instead of a more evenly distributed force [1]. It is possible that such peak forces in the disc can be transmitted to the endplate and produce fractures. The fracture in itself might result in the oedema seen as VESC on the MRI. It is also possible that these mediators from the disc seep through endplate fissures and stimulate an inflammatory response [34]. All of these mechanisms could be relatively slow-acting.
The second possibility is linked to disc herniations (not bulges) and might represent a more fast-acting type of VESC. Here, the herniation and the circumstances associated with this event initiate changes in the disc and/or vertebral bone that produce the oedema seen as VESC on the MRI. In a study of 51 patients with herniations treated surgically, there was an association between the presence of endplate cartilage in the extracted disc material and the presence of VESC [36], indicating direct damage to the discovertebral complex in certain types of herniations. Animal studies on baboons, rats, and sheep support this theory as injury to the disc has been seen to induce changes in the adjacent vertebrae with subsequent bone marrow depletion and a process of degeneration and regeneration of the bone [26, 29, 40].
Regarding the association between VESC and LBP, this will be addressed in a separate manuscript.
This study has some weaknesses. First, the relatively small number of people in this study (n = 344) makes it difficult to analyse interactions between the lifestyle factors in the multivariable analysis. This was relevant, as a previous study of the baseline cohort of the current study [23] reported a stronger association between high physical work activity plus either heavy smoking or overweight than for each of these lifestyle factors analysed separately. Second, although the study was conducted in a research setting, and time was spent in optimizing the MRI sequences to suit the purpose of this study, the use of a low field MRI system could have been potentially problematic. The low resolution (256 × 256 matrix) of the images may have reduced the sensitivity of the evaluation of the MRI findings, especially for endplate changes. This might explain why endplate changes were the only MRI finding that was not significant in the analyses.
On the other hand, there are several elements that strengthen the results from this study. First, the proportion of people with new VESC in our study (19% over a 4-year period) is equivalent to that which has been reported in previous studies, where the proportions ranged from 15–24% over periods of 14–62 months [2, 7, 20]. Second, three lifestyle factors (high physical work activity, high physical leisure activity, and high BMI) were used as a form of triangulation to investigate whether physical load was associated with new VESC, thereby increasing confidence in the finding that physical load was not a risk factor. Third, the study sample of ethnically homogenous people of the same age from the general population precluded the need to adjust for the factors of ethnicity and age. Finally, the results from the drop-out analysis showed that non-responders only differed from the responders in relation to one parameter, i.e. employment status. This confirms that bias due to drop-out was unlikely to have an affect on the final results of the study.
Consequences
As disc degeneration and abnormal disc contour are risk factors for the development of VESC, they can be used by clinicians to identify patients who are at increased risk. For the research community, it is worth noting that the association between lifestyle factors and VESC, previously reported [23], was not found in this study. Further studies could aim at identifying the association between lifestyle factors and VESC in different age groups.
Conclusion
Disc degeneration, disc bulges, and disc herniations were all predictive of the development of VESC over a 4-year period, from the age of 40–44, in people from the general population. Female gender and the lifestyle factors of physical load and smoking were not found to be risk factors of new VESC in this age group.
Acknowledgments
Supported by grants from the Danish Foundation of Chiropractic Research and Postgraduate Education (Tue Secher Jensen).
References
- 1.Adams MA, Freeman BJ, Morrison HP, Nelson IW, Dolan P. Mechanical initiation of intervertebral disc degeneration. Spine. 2000;25:1625–1636. doi: 10.1097/00007632-200007010-00005. [DOI] [PubMed] [Google Scholar]
- 2.Albert HB, Manniche C. Modic changes following lumbar disc herniation. Eur Spine J. 2007;16:977–982. doi: 10.1007/s00586-007-0336-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barth M, Diepers M, Weiss C, Thome C. Two-year outcome after lumbar microdiscectomy versus microscopic sequestrectomy: part 2: radiographic evaluation and correlation with clinical outcome. Spine. 2008;33:273–279. doi: 10.1097/BRS.0b013e31816201a6. [DOI] [PubMed] [Google Scholar]
- 4.Bazrgari B, Shirazi-Adl A, Arjmand N. Analysis of squat and stoop dynamic liftings: muscle forces and internal spinal loads. Eur Spine J. 2007;16:687–699. doi: 10.1007/s00586-006-0240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braithwaite I, White J, Saifuddin A, Renton P, Taylor BA. Vertebral end-plate (Modic) changes on lumbar spine MRI: correlation with pain reproduction at lumbar discography. Eur Spine J. 1998;7:363–368. doi: 10.1007/s005860050091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cvitanic OA, Schimandle J, Casper GD, Tirman PF. Subchondral marrow changes after laser discectomy in the lumbar spine: MR imaging findings and clinical correlation. Am J Roentgenol. 2000;174:1363–1369. doi: 10.2214/ajr.174.5.1741363. [DOI] [PubMed] [Google Scholar]
- 7.Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N. Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine. 2002;27:125–134. doi: 10.1097/00007632-200201150-00002. [DOI] [PubMed] [Google Scholar]
- 8.Eyre D, Nemya P, Buckwalter J, Caterson N, Heinegard D, Oegema T, et al. Intervertebral disk: basic science perspectives. In: Frymoyer JW, Gordon SL, et al., editors. New perspectives on low back pain. Park Ridge: American Academy of Orthopaedic Surgeons; 1989. pp. 147–207. [Google Scholar]
- 9.Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 10.Heliovaara M. Risk factors for low back pain and sciatica. Ann Med. 1989;21:257–264. doi: 10.3109/07853898909149202. [DOI] [PubMed] [Google Scholar]
- 11.Hildebrandt VH, Bongers PM, Dul J, Dijk FJ, Kemper HC. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. 2000;73:507–518. doi: 10.1007/s004200000167. [DOI] [PubMed] [Google Scholar]
- 12.Hopper JL, Seeman E. The bone density of female twins discordant for tobacco use. N Engl J Med. 1994;330:387–392. doi: 10.1056/NEJM199402103300603. [DOI] [PubMed] [Google Scholar]
- 13.Ito M, Incorvaia KM, Yu SF, Fredrickson BE, Yuan HA, Rosenbaum AE. Predictive signs of discogenic lumbar pain on magnetic resonance imaging with discography correlation. Spine. 1998;23:1252–1258. doi: 10.1097/00007632-199806010-00016. [DOI] [PubMed] [Google Scholar]
- 14.Iwahashi M, Matsuzaki H, Tokuhashi Y, Wakabayashi K, Uematsu Y. Mechanism of intervertebral disc degeneration caused by nicotine in rabbits to explicate intervertebral disc disorders caused by smoking. Spine. 2002;27:1396–1401. doi: 10.1097/00007632-200207010-00005. [DOI] [PubMed] [Google Scholar]
- 15.Jensen TS, Bendix T, Sorensen JS, Manniche C, Korsholm L, Kjaer P. Characteristics and natural course of vertebral endplate signal (Modic) changes in the Danish general population. BMC Musculoskelet Disord. 2009;10:81. doi: 10.1186/1471-2474-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17:1407–1422. doi: 10.1007/s00586-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jensen TS, Sorensen JS, Kjaer P. Intra- and interobserver reproducibility of vertebral endplate signal (modic) changes in the lumbar spine: the Nordic Modic Consensus Group classification. Acta Radiol. 2007;48:748–754. doi: 10.1080/02841850701422112. [DOI] [PubMed] [Google Scholar]
- 18.Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T. Magnetic resonance imaging and low back pain in adults: a diagnostic imaging study of 40-year-old men and women. Spine. 2005;30:1173–1180. doi: 10.1097/01.brs.0000162396.97739.76. [DOI] [PubMed] [Google Scholar]
- 19.Kovacs FM, Royuela A, Jensen TS, Estremera A, Amengual G, Muriel A, et al. Agreement in the interpretation of lumbar magnetic resonance images. Acta Radiol. 2009;50:497–506. doi: 10.1080/02841850902838074. [DOI] [PubMed] [Google Scholar]
- 20.Kuisma M, Karppinen J, Niinimaki J, Kurunlahti M, Haapea M, Vanharanta H, et al. A three-year follow-up of lumbar spine endplate (Modic) changes. Spine. 2006;31:1714–1718. doi: 10.1097/01.brs.0000224167.18483.14. [DOI] [PubMed] [Google Scholar]
- 21.Kuisma M, Karppinen J, Niinimaki J, Ojala R, Haapea M, Heliovaara M, et al. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine. 2007;32:1116–1122. doi: 10.1097/01.brs.0000261561.12944.ff. [DOI] [PubMed] [Google Scholar]
- 22.Kuorinka I, Jonsson B, Kilbom A, Biering-Sorensen F, Andersson G, Jørgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 23.Leboeuf-Yde C, Kjaer P, Bendix T, Manniche C. Self-reported hard physical work combined with heavy smoking or overweight may result in so-called Modic changes. BMC Musculoskelet Disord. 2008;9:5. doi: 10.1186/1471-2474-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liuke M, Solovieva S, Lamminen A, Luoma K, Leino-Arjas P, Luukkonen R, et al. Disc degeneration of the lumbar spine in relation to overweight. Int J Obes (Lond) 2005;29:903–908. doi: 10.1038/sj.ijo.0802974. [DOI] [PubMed] [Google Scholar]
- 25.Luoma K, Riihimaki H, Raininko R, Luukkonen R, Lamminen A, Viikari-Juntura E. Lumbar disc degeneration in relation to occupation. Scand J Work Environ Health. 1998;24:358–366. doi: 10.5271/sjweh.356. [DOI] [PubMed] [Google Scholar]
- 26.Malinin T, Brown MD. Changes in vertebral bodies adjacent to acutely narrowed intervertebral discs: observations in baboons. Spine. 2007;32:E603–E607. doi: 10.1097/BRS.0b013e31815574e7. [DOI] [PubMed] [Google Scholar]
- 27.Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–186. doi: 10.1148/radiology.168.1.3289089. [DOI] [PubMed] [Google Scholar]
- 28.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 29.Moore RJ, Vernon-Roberts B, Osti OL, Fraser RD. Remodeling of vertebral bone after outer anular injury in sheep. Spine. 1996;21:936–940. doi: 10.1097/00007632-199604150-00006. [DOI] [PubMed] [Google Scholar]
- 30.Papaioannou A, Kennedy CC, Cranney A, Hawker G, Brown JP, Kaiser SM, et al. Risk factors for low BMD in healthy men age 50 years or older: a systematic review. Osteoporos Int. 2009;20:507–518. doi: 10.1007/s00198-008-0720-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raininko R, Manninen H, Battie MC, Gibbons LE, Gill K, Fisher LD. Observer variability in the assessment of disc degeneration on magnetic resonance images of the lumbar and thoracic spine. Spine. 1995;20:1029–1035. doi: 10.1097/00007632-199505000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Rasmussen C. [Lumbar disk prolapse. Alcohol, tobacco and prognosis] Ugeskr Laeg. 1998;160:5189–5192. [PubMed] [Google Scholar]
- 33.Roberts N, Gratin C, Whitehouse GH. MRI analysis of lumbar intervertebral disc height in young and older populations. J Magn Reson Imaging. 1997;7:880–886. doi: 10.1002/jmri.1880070517. [DOI] [PubMed] [Google Scholar]
- 34.Salo J, Mackiewicz Z, Indahl A, Konttinen YT, Holm AK, Sukura A, et al. Plasmin-matrix metalloproteinase cascades in spinal response to an experimental disc lesion in pig. Spine. 2008;33:839–844. doi: 10.1097/BRS.0b013e31816b1f1d. [DOI] [PubMed] [Google Scholar]
- 35.Schenk P, Laubli T, Hodler J, Klipstein A. Magnetic resonance imaging of the lumbar spine: findings in female subjects from administrative and nursing professions. Spine. 2006;31:2701–2706. doi: 10.1097/01.brs.0000244570.36954.17. [DOI] [PubMed] [Google Scholar]
- 36.Schmid G, Witteler A, Willburger R, Kuhnen C, Jergas M, Koester O. Lumbar disk herniation: correlation of histologic findings with marrow signal intensity changes in vertebral endplates at MR imaging. Radiology. 2004;231:352–358. doi: 10.1148/radiol.2312021708. [DOI] [PubMed] [Google Scholar]
- 37.Sigurdsson G, Aspelund T, Chang M, Jonsdottir B, Sigurdsson S, Eiriksdottir G, et al. Increasing sex difference in bone strength in old age: the age, gene/environment susceptibility-Reykjavik study (AGES-REYKJAVIK) Bone. 2006;39:644–651. doi: 10.1016/j.bone.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 38.Slemenda CW, Christian JC, Reed T, Reister TK, Williams CJ, Johnston CC., Jr Long-term bone loss in men: effects of genetic and environmental factors. Ann Intern Med. 1992;117:286–291. doi: 10.7326/0003-4819-117-4-286. [DOI] [PubMed] [Google Scholar]
- 39.Solgaard SJ, Kjaer P, Jensen ST, Andersen P. Low-field magnetic resonance imaging of the lumbar spine: reliability of qualitative evaluation of disc and muscle parameters. Acta Radiol. 2006;47:947–953. doi: 10.1080/02841850600965062. [DOI] [PubMed] [Google Scholar]
- 40.Ulrich JA, Liebenberg EC, Thuillier DU, Lotz JC. ISSLS prize winner: repeated disc injury causes persistent inflammation. Spine. 2007;32:2812–2819. doi: 10.1097/BRS.0b013e31815b9850. [DOI] [PubMed] [Google Scholar]
- 41.Videman T, Battie MC, Gill K, Manninen H, Gibbons LE, Fisher LD. Magnetic resonance imaging findings and their relationships in the thoracic and lumbar spine. Insights into the etiopathogenesis of spinal degeneration. Spine. 1995;20:928–935. doi: 10.1097/00007632-199504150-00009. [DOI] [PubMed] [Google Scholar]
- 42.Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 43.Weishaupt D, Zanetti M, Hodler J, Min K, Fuchs B, Pfirrmann CW, et al. Painful lumbar disk derangement: relevance of endplate abnormalities at MR imaging. Radiology. 2001;218:420–427. doi: 10.1148/radiology.218.2.r01fe15420. [DOI] [PubMed] [Google Scholar]