Abstract
The three-dimensional correction of severe rigid scoliosis has been improved by segmental pedicle screw instrumentation. However, there can be significant difficulty related to the use of a rigid rod, especially in the apex region of severe scoliosis. This study is a retrospective matched cohort study to evaluate the advantages of Nitinol shape memory alloy (SMA) rod-based correction by comparing the clinical and radiographic results obtained from using a temporary SMA rod and those from a standard rod in the correction of severe scoliosis. From May 2004 to September 2006, patients with matched curve type, ages at surgery, operative methods and fusion levels in our institute and instrumented with either SMA rods (n = 14) or traditional correction techniques (n = 16) were reviewed. In SMA group, the SMA rods served as a temporary intraoperative tool for deformity correction and were replaced by standard rods. The blood loss at surgery averaged 778 ± 285 ml in the traditional group and 585 ± 188 ml in the SMA group (P < 0.05). Operative time averaged 284 ± 53 min in the SMA group and 324 ± 41 min in the traditional group (P < 0.05). In the SMA group, the preoperative major curve was 92.6° ± 13.7° with a flexibility of 25.5 ± 7.3% was corrected to 29.4° ± 5.7° demonstrating a 68.4% immediate postoperative correction. In the traditional group, the preoperative major curve was 88.6° ± 14.6° with a flexibility of 29.3 ± 6.6% was corrected to 37.2° ± 7.3° demonstrating a 57.8% immediate postoperative correction. There was a statistic difference between the SMA group and traditional group in correction rate of the major thoracic curve. In the SMA group, one case suffered from deep infection 2 months postoperatively. In the traditional group, 6 of 16 cases suffered pedicle screw pull out or loosening during placement of the standard rod at the apex vertebrae on the concave side. In three cases, the mono-axial pedicle screws near the apex were abandoned and in five cases replaced with poly-axial pedicle screws. This study shows that the temporary use of SMA rod may reduce the operative time, blood loss, while improve the correction of the coronal plane when compared with standard techniques.
Electronic supplementary material
The online version of this article (doi:10.1007/s00586-009-1207-2) contains supplementary material, which is available to authorized users.
Keywords: Scoliosis, Shape memory alloy, Derotation, Translation, Posterior approach
Introduction
Scoliosis is a three-dimensional deformity of the spine for which corrective surgery frequently is required. To improve the correction, techniques in scoliosis surgery were developed from Harrington principles of concave distraction to segmental realignment by rod derotation, cantilever and translation methods [7, 9, 12]. Segmental pedicle screw fixation can further improve the three-dimensional correction by fixating the anterior and posterior columns [20].
However, there can be significant difficulty related to the use of a rigid rod, especially in the apex region of severe scoliosis. These include the placement of the contoured rod in the deformed spine, the concentration of stress during the replacement of pedicle screws one by one, and pull out of pedicle screws. Theoretically, these shortcomings may be avoided by replacing the rigid rod with a relatively malleable rod during the correction.
The Nitinol shape memory alloy (SMA) rod is one option with its considerable flexibility at low temperatures; that is, the material can be shaped as desired at low temperatures. Once the material is heated above its activation temperature, it automatically returns to its original, preselected shape.
These distinct characteristics allow the SMA to be used extensively in cardiovascular stents [2, 10] and in spine surgery [1, 4, 14, 16–18, 25]. We developed the technique where we use the SMA rods as a temporary tool. The SMA rods were replaced by rigid rod at the end of correction. We hypothesized that (1) temporary use of shape memory rods will reduce the operational time, blood loss and (2) achieve better three-dimensional correction compared with using only a standard rigid rod. A retrospective matched cohort study between shape memory rods and rigid rod was conducted to determine which technique of correction provided better clinical and radiographic results.
Materials and methods
From May 2004 to September 2006, patients with matched curve type, ages at surgery, operative methods and fusion levels in our institute were compared. Patients with the major curve of scoliosis located in the main thoracic spine were included. In SMA group, the diagnoses included 10 idiopathic scoliosis, 4 neuromuscular scoliosis and the average age is 15.6 years old (range from 13 to 28). In traditional group, the diagnoses included 11 idiopathic scoliosis, 5 neuromuscular scoliosis and the average age is 14.8 years old (range from 13 to 26). Radiographic analysis included Cobb angle measurements of the major curve preoperatively, immediately postoperatively and at 2-year follow-up (Fig. 1).
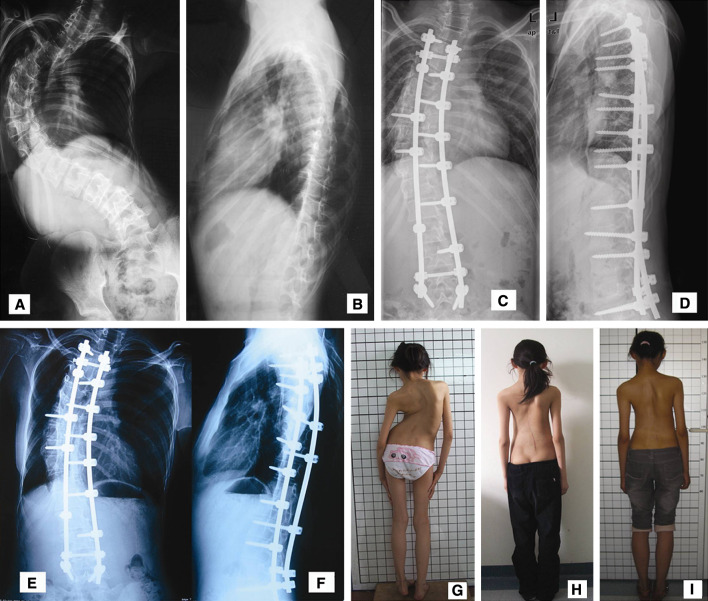
Fig. 1.
A 14-year-old girl with severe scoliosis. a, b Preoperative anteroposterior and lateral radiograph showed 116° main thoracic scoliosis. c, d Anteroposterior and lateral radiograph taken 3 days after the surgery with posterior pedicle screw fixation from T3 to L5 without anterior release. The shape memory alloy rods just served as temporary tool and were replaced by rigid rod at the end of correction intraoperatively. The main thoracic curve was corrected to 38° and the correction rate was 69%. e, f Anteroposterior and lateral radiographs taken 2 years after the surgery, coronal and sagittal alignments were well maintained during the follow-up. g–i Appearance of preoperative, 1 month postoperative and 2 years postoperative
The traditional group was treated with pedicle screw construct using UPSS Instrumentation (Weigao Company, Shandong, China or CDH Medtronic Sofamor-Danek, Memphis, TN). The SMA group was treated with matched pedicle screw systems. The SMA rod just served as a temporary tool and was replaced by a rigid rod at the end of correction. Patients with prior spinal surgery or revision surgery were excluded.
Surgical technique
A standard posterior midline incision was used in both SMA and traditional groups. All patients had a posterior arthrodesis of the spine. All pedicle screws (mono-axial) were inserted with a free hand pedicle screw placement technique, and the intraosseous placement was confirmed via C-arm image intensifier after the insertion. In the traditional group, correction techniques include standard rod derotation and translation. If the concave pedicle near the apex was too rotated to insert a pedicle screw, the screw was abandoned. If it was too difficult to place the rod into pedicle screws secondary to the misalignment, we utilized a poly-axial pedicle screw.
In the SMA group, a shape memory rod (diameter is 6 mm) was cooled in an aseptic ice bath and was contoured according to the configuration of the spinal deformity. Crushed ice was used to control the local temperature during rod insertion into the pedicle screws. With the set screws loose and the sagittal mark line in the proper orientation, the SMA was warmed up with warm water. “Self-correct” was achieved when the shape memory rod resumed to its memory shape (normal sagittal curvature and straight coronal alignment). When the shape of SMA rod does not change with warming it up, a permanent rigid spinal rod was fixed with anchors in the supporting side (convex side). The shape memory rod was then replaced with a permanent rigid rod. Next, distraction on the concave side and compression on the convex side between adjacent level pedicle screws were performed to manage the coronal balance. Facet decortication was performed using a high-speed burr, and facet fusion was performed with allogenic bone graft or autogenous bone graft harvested from spinal process.
Postoperative management
All patients underwent scoliosis correction were extubated after the procedure. Patients were typically allowed to ambulate within 48–72 h without orthosis, when the drain tube was pulled out. Usually, the drain was removed when the blood loss through drain was <50 ml per 24 h. The antibiotic was administrated to prevent infection.
Statistical analysis
All statistical analysis was performed with Stat View Software (SAS Institute, Cary, NC). P < 0.05 was considered statistically significant.
Results
The average blood loss at surgery was 585 ± 188 ml in SMA group and 778 ± 285 ml in traditional group (P < 0.05). Operative time averaged 284 ± 53 min in the SMA group and 324 ± 41 min in the traditional group (P < 0.05) (Table 1).
Table 1.
Operation time, blood loss and complication
| SMA group (n = 14) | Traditional group (n = 16) | P | |
|---|---|---|---|
| Operation time (m) | 284 ± 53 | 324 ± 41 | 0.027* |
| Blood loss (ml) | 585 ± 188 | 778 ± 285 | 0.040* |
| Complication | Deep infection | Screws pulling out, loosen; replace mono-axial screws with multi-axial screws | |
* Statistically significant if P < 0.05
Radiographic results
In the SMA group, the preoperative major curve was 92.6° ± 13.7° with a flexibility of 25.5 ± 7.3% in side-bending film. The deformity was corrected to 29.4° ± 5.7° demonstrating a 68.4% immediate postoperative correction and 32.1° ± 5.6° at the most recent follow-up. There was 2.7° correction loss during the postoperative follow-up. In the traditional group, the preoperative major curve was 88.6° ± 14.6° with a flexibility of 29.3 ± 6.6% in side-bending film. The deformity was corrected to 37.2° ± 7.3° demonstrating a 57.8% immediate postoperative correction and 38.6° ± 6.8° at the most recent follow-up. There was 1.4° correction loss during the postoperative follow-up. There was a statistical difference between the correction rate of the major thoracic curve (Table 2), while no difference was found in the sagittal plane (Table 3).
Table 2.
Comparison of coronal plane change
| SMA group (n = 14) | Traditional group (n = 16) | P | |
|---|---|---|---|
| Global balance (mm) | |||
| Preoperative | 18.2 ± 3.3 | 17.6 ± 4.2 | 0.67 |
| Final FU | 8.5 ± 2.7 | 9.2 ± 2.4 | 0.46 |
| Major curve Cobb angle (°) | |||
| Preoperative | 92.6 ± 13.7 | 88.6 ± 14.6 | 0.45 |
| Flexibility (%) | 25.5 ± 7.3 | 29.3 ± 6.6 | 0.15 |
| IMPO | 29.4 ± 5.7 | 37.2 ± 7.3 | 0.003* |
| Correction rate (%) | 68.4 ± 6.2 | 57.8 ± 9.8 | 0.002* |
| Final FU | 32.1 ± 5.6 | 38.6 ± 6.8 | 0.009* |
| Apical vertebral translation (mm) | |||
| Preoperative | 56.2 ± 16.7 | 52.3 ± 13.4 | 0.48 |
| IMPO | 18.6 ± 12.5 | 22.3 ± 15.6 | 0.45 |
IMPO immediate postoperation, FU follow-up
* Statistically significant if P < 0.05
Table 3.
Comparison of sagittal plane change
| SMA group (n = 14) | Traditional group (n = 16) | P | |
|---|---|---|---|
| Global balance (mm) | |||
| Preoperative | −18.4 ± 33.8 | −17.4 ± 29.6 | 0.87 |
| Final FU | −20.5 ± 34.2 | −19.4 ± 33.8 | 0.90 |
| T5–T12 kyphotic angle (°) | |||
| Preoperative | 25.4 ± 13.8 | 28.6 ± 12.7 | 0.48 |
| IMPO | 17.4 ± 9.7 | 14.3 ± 6.8 | 0.31 |
| Final FU | 18.6 ± 10.4 | 15.2 ± 7.2 | 0.30 |
| T12–S1 lordosis angle (°) | |||
| Preoperative | 55.4 ± 16.8 | 56.8 ± 15.3 | 0.81 |
| IMPO | 50.6 ± 12.3 | 52.4 ± 13.8 | 0.71 |
| Final FU | 54.7 ± 12.9 | 55.8 ± 12.4 | 0.79 |
* Statistically significant if P < 0.05
Complications
There were no neurologic or vascular complications at 2 years of follow-up. One case of deep infection was found 2 months postoperatively in the SMA group. The patient cleared the infection after thorough debridement. In the traditional group, 6 of 16 cases suffered concave pedicle screws pull out or loosening, three cases the pedicle screws near the apex were abandoned and in five cases replaced with poly-axial pedicle screws.
Discussion
In severe scoliosis, the most common treatment is anterior release and a posterior correction and instrumentation [3, 5, 13, 15, 21] while other authors recommended combined anterior and posterior spinal fusion for this curves [6]. With the advent of more sophisticated instrumentation and surgical techniques, greater corrections are being achieved. Some authors report successful posterior-only instrumented fusion for scoliosis with major Cobb angles greater than 90° [8, 11, 19, 24].
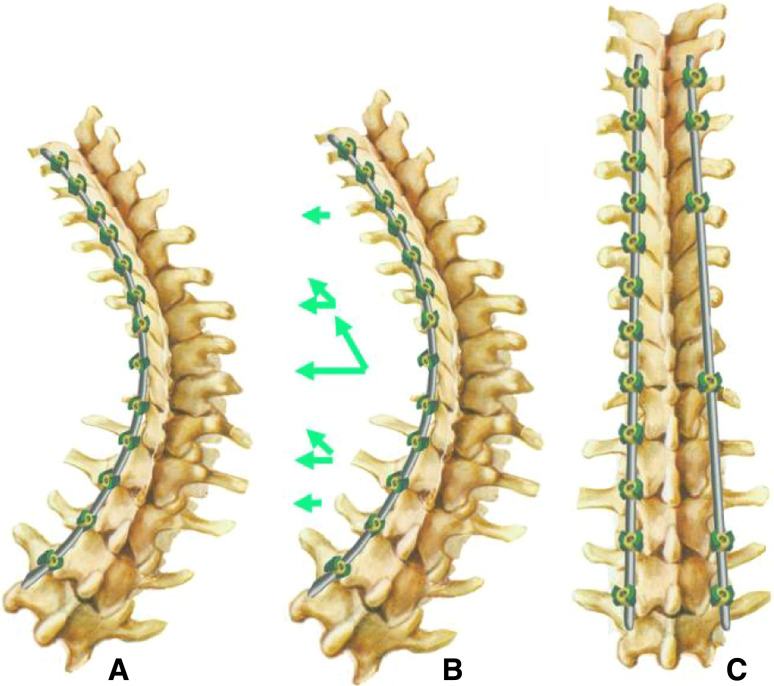
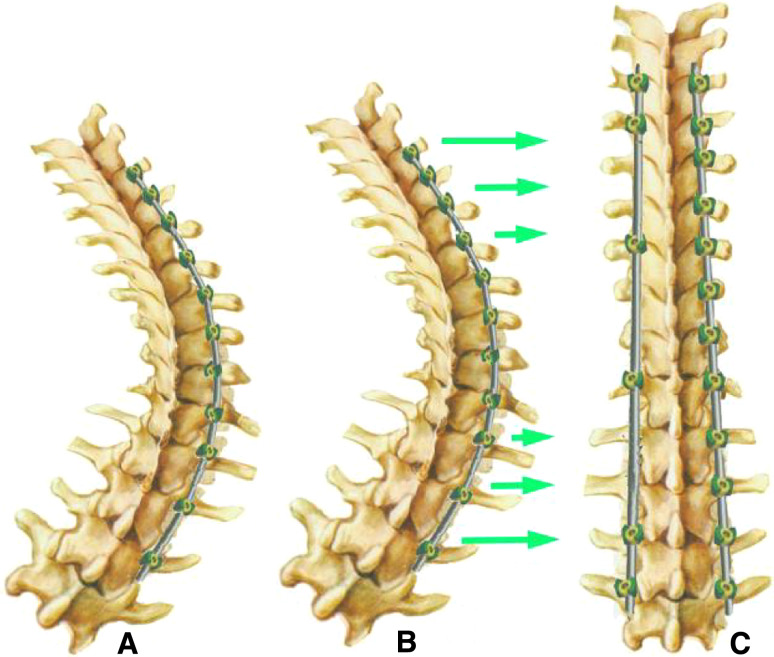
Current correction maneuvers include rod derotation or translation of the pedicle screws to attach the concave rod gradually. These techniques rely on forcing displaced vertebral bodies into alignment, usually by manual force. With SMA rod, the shape recovery forces were used to achieve a gradual three-dimensional scoliosis correction. Forces induce a bending moment to correct the lateral and sagittal curves of the scoliotic spine, and a torque to correct the axial rotation. SMA-based scoliosis correction is an independent form of scoliosis correction, in which a SMA rod functions as the correcting element. However, the mechanism is different between it use on the concave or the convex side. On the concave side, when the bent SMA rod returns to its original shape, both axial torque and pulling forces cause the spine to derogate and translate simultaneously (Fig. 2). On the convex side, the mechanism of correction is to force the misaligned apical vertebrae to a relative normal alignment, which is similar to the technique of cantilever (Fig. 3).
Fig. 2.
When the bent shape memory alloy rod returned to its original shape (physiological curve of spine in sagittal plane and straight in coronal plane) in concave side, both axial torque and pulling forces were performed in concave side of spine, the derotation and translation were achieved simultaneously
Fig. 3.
When the bent shape memory alloy rod returned to its original shape in convex side, the mechanism of correction is to force the malalign apical vertebrae to relative normal alignment, which is similar to the technique of cantilever
In our study, double major curve types were excluded to increase the comparability, because the mechanism of SMA correction in these curves is complicated. The major curve located in the lumbar spine was excluded as well, because the correction is different between the lumbar and thoracic spine secondary to the impact of the chest.
In the traditional group, problems arise when placing the rigid rod into mono-axial pedicle screws at the apex of large curves. This procedure may lead to an increased concentration of stress on the pedicle screw resulting in screw pull out or damage to the screw head. If it is too difficult to place a rigid rod into the top-loading mono-axial pedicle screws one by one in the curve side near the apex region, especially in cases of those with AVT more than 6 or 8 cm, we recommend replacing the mono-axial pedicle screws with poly-axial pedicle screws. In the traditional group, 6 of 16 cases suffered pedicle screw pull out or loosening, three cases pedicle screws near the apex were abandoned and five cases were replaced with poly-axial pedicle screws. Of course, these procedures may potentially increase the operative time, blood loss.
The SMA rod is malleable at low temperatures, which decreases the difficulty in placing the rod on the deformed spine. Our data suggest this reduces both the operative time and blood loss. In addition, SMA-based correction allows the corrective power to be dispersed to a greater number of pedicle screws rather than a single screw. This resulted in decreased complications related to the correction maneuvers. No pedicle screws pulled out and none of the mono-axial screws needed replacement with poly-axial screws in the SMA group.
One insufficient of this technique is that the restoration of thoracic sagittal curve is not obvious in both two groups, although there is a pulling power at the concave side during the SMA-based scoliosis correction. Two main reasons may contribute to the fact that there was no difference in sagittal plane: one is that patients enrolled in this study were severe scoliosis, which means the constructs changes of spine and bony thorax may prevent the correction not only in coronal plane, but also in sagittal plane; the other is that the profile of SMA rod in sagittal plane is a physiological curve of spine, so, the corrective torque may decrease when the deformed spine was corrected near to a normal spine.
Undoubtedly, it is not quite well understood the permanent shape memory effect in vivo from a scientific point of view. In addition, there is a fear of releasing wear debris at the junction between the rod and the anchoring system [22, 23]. These were minimized because we used the shape memory rod as a temporary correction tool. The SMA rod was replaced by rigid rod at the end of correction. Therefore, this procedure takes advantage of the SMA, while minimizes its potential disadvantages.
Conclusion
In summary, all patients in this study had large curves (70°–108°) and were treated by posterior segmental pedicle screw fixation and correction without anterior release. This comparative study of two methods has demonstrated that SMA rod-based scoliosis correction will reduce the operation time, blood loss and achieve better coronal correction rates.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Betz RR, Kim J, D’Andrea LP, et al. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: a feasibility, safety, and utility study. Spine. 2003;28(Suppl):255–265. doi: 10.1097/01.BRS.0000092484.31316.32. [DOI] [PubMed] [Google Scholar]
- 2.Bezzi M, Orsi F, Salvatori FM, et al. Self-expandable nitinol stent for the management of biliary obstruction: long-term clinical results. J Vasc Intervent Radiol. 1994;5:287–293. doi: 10.1016/S1051-0443(94)71485-8. [DOI] [PubMed] [Google Scholar]
- 3.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22:1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 4.Braun JT, Hines JL, Akyuz E, et al. Relative versus absolute modulation of growth in the fusionless treatment of experimental scoliosis. Spine. 2006;15:1776–1782. doi: 10.1097/01.brs.0000227263.43060.50. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH. Surgical treatment of idiopathic adolescent scoliosis. Spine. 1999;24:2607–2616. doi: 10.1097/00007632-199912150-00008. [DOI] [PubMed] [Google Scholar]
- 6.Bullmann V, Halm HFH, Schulte T, et al. Combined anterior and posterior instrumentation in severe and rigid idiopathic scoliosis. Eur Spine J. 2006;15:440–448. doi: 10.1007/s00586-005-1016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 8.Dobbs MB, Lenke LG, Kim YJ, et al. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine. 2006;31:2386–2391. doi: 10.1097/01.brs.0000238965.81013.c5. [DOI] [PubMed] [Google Scholar]
- 9.Harrington PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44:591–610. [PubMed] [Google Scholar]
- 10.Henry M, Amor M, Beyar R, et al. Clinical experience with a new nitinol selfexpanding stent in peripheral arteries. J Endovasc Surg. 1996;3:369–379. doi: 10.1583/1074-6218(1996)003<0369:CEWANN>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Kuklo TR, Lenke LG, O’Brien MF, et al. Accuracy and efficacy of thoracic pedicle screws in curves more than 90°. Spine. 2005;30:222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 12.Labelle H, Dansereau J, Bellefleur C, et al. Comparison between preoperative and postoperative three-dimensional reconstructions of idiopathic scoliosis with the Cotrel–Dubousset procedure. Spine. 1995;20:2487–2492. doi: 10.1097/00007632-199512000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine. 2003;28:S36–S43. doi: 10.1097/00007632-200308011-00007. [DOI] [PubMed] [Google Scholar]
- 14.Lu SB, Wang JF, Guo JF (1986) Treatment of scoliosis with a shape-memory alloy rod. Zhonghua Wai Ke Za Zhi 24: 129–132, 187 [PubMed]
- 15.Niemeyer T, Freeman BJC, Grevitt MP, et al. Anterior thoracoscopic surgery followed by posterior instrumentation and fusion in spinal deformity. Eur Spine J. 2000;9:499–504. doi: 10.1007/s005860000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puttlitz CM, Masaru F, Barkley A, et al. A biomechanical assessment of thoracic spine stapling. Spine. 2007;32:766–771. doi: 10.1097/01.brs.0000259073.16006.ed. [DOI] [PubMed] [Google Scholar]
- 17.Sanders JO, Sanders AE, More R, et al. A preliminary investigation of shape memory alloys in the surgical correction of scoliosis. Spine. 1993;18:1640–1646. doi: 10.1097/00007632-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Schmerling MA, Wilkov MA, Sanders AE, et al. Using the shape recovery of nitinol in the Harrington rod treatment of scoliosis. J Biomed Mater Res. 1976;10:879–892. doi: 10.1002/jbm.820100607. [DOI] [PubMed] [Google Scholar]
- 19.Suk S, Kim JH, Cho KJ, et al. Is anterior release necessary in severe scoliosis treated by posterior segmental pedicle screw fixation. Eur Spine J. 2007;16:1359–1365. doi: 10.1007/s00586-007-0334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suk S, Lee CK, Kim W, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 21.Tokunaga M, Minami S, Kitahara H, et al. Vertebral decancellation for severe scoliosis. Spine. 2000;25:469–474. doi: 10.1097/00007632-200002150-00013. [DOI] [PubMed] [Google Scholar]
- 22.Vieweg U, van Roost D, Wolf HK, et al. Corrosion on an internal spinal fixator system. Spine. 1999;24:946–951. doi: 10.1097/00007632-199905150-00004. [DOI] [PubMed] [Google Scholar]
- 23.Wang JC, Yu WD, Sandhu HS, et al. Metal debris from titanium spinal implants. Spine. 1999;24:899–903. doi: 10.1097/00007632-199905010-00011. [DOI] [PubMed] [Google Scholar]
- 24.Wang Y, Zhang YG, Zhang XS, et al. A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J. 2008;17:361–372. doi: 10.1007/s00586-007-0566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wever DJ, Elstrodt JA, Veldhuizen AG, et al. Scoliosis correction with shape-memory metal: results of an experimental study. Eur Spine J. 2002;11:100–106. doi: 10.1007/s005860100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.