Abstract
The aim of this study was to analyze the correlation ratios between the sagittal back contour (flèche cervicale and lombaire, trunk inclination) and selected parameters of craniofacial morphology in children. The patient sample consisted of 66 healthy children with a mean age of 11.2 years (SD 1.6 years), of which 34 were male (mean age 11.5 years, SD 1.3 years) and 32 were females (mean age 10.9 years, SD 1.9 years). The children were recruited during the preparation of the initial orthodontic treatment records. Craniofacial morphology was analyzed by six angular measurements: facial axis, mandibular plane angle, inner gonial angle, lower facial height, facial depth and maxilla position. Rasterstereography was used for reconstruction of the spinal back sagittal profile. From the profile flèche cervicale, flèche lombaire and trunk inclination were determined and the correlations with the craniofacial morphology were calculated (Pearson and Mann–Whitney U test). Significant correlations were found with respect to the inner gonial angle and the flèche cervicale, the mandibular plane angle and the flèche lombaire, the inner gonial angle and the flèche lombaire, and the angular lower facial height and the flèche lombaire, as well as the inner gonial angle and the trunk inclination. The craniofacial vertical growth pattern, presented by mandibular plane angle, inner gonial angle and the angular lower facial height, and the correlation to flèche cervicale and lombaire as well as trunk inclination reveal correlations between growth pattern and sagittal back contour.
Keywords: Body posture, Rasterstereography, Craniofacial morphology, Cephalometry
Introduction
Orthodontic literature contains descriptions of correlations between the craniofacial morphology and the body posture [1–3]. In our own recent studies, we used lateral cephalometric radiographs to analyze the craniofacial morphology and the jaw position in relation to the skeletal growth pattern in adults and found correlations to selected body posture parameters analyzed by means of video rasterstereography [4]. Patients with a higher degree of vertical craniofacial morphology and mandibular retrognathism showed higher kyphotic and lordotic angles compared to patients with a smaller degree of vertical craniofacial morphology and mandibular prognatism. On the basis of the documented correlations, we concluded that the mandibula is more closely correlated to the muskuloskeletal anatomy of the cervical spine than the maxilla [4]. Similar findings were reported by Segatto et al. [5, 6] in studies carried out on children with different spinal deformities. Michelotti et al. [3] also reported correlations between the upper spine sections and mandibular position. They did not find evidence of correlations between the jaw position and further caudally located spinal sections. Festa et al. [2] analyzed the correlations between the sagittal jaw position and cervical lordosis using lateral skull radiographs on 70 Caucasian adult women (mean age 27.4 years) and observed significant correlations between an increased cervical lordosis and mandibular retrognathism. Similarly, D’Atillo et al. [7] established correlations between the cervical lordosis and craniofacial parameters such as the overjet and the mandibular position, length and divergence. In another study, D’Atillo et al. [8] observed significant associations between the cervical spinal lordosis and the sagittal craniofacial morphology by analyzing lateral skull radiographs of 120 children (average age 9.5 years). The study showed decreased cervical lordosis angles in children revealing skeletal class III and an extension of the head in children with class II morphology. The authors concluded that the “posture of the neck seems to be strongly associated with the sagittal as well as the vertical structure of the face”.
Assessment of spinal shape is generally done by lateral X-rays [9]. However, to avoid radiation hazard, estimation of spinal shape from back surface measurements is an alternative. By developing objective methods for the analysis of the back shape, it is possible to assess the sagittal contour of the back and to determine shape parameters such as kyphotic and lordotic angle. These angles have been shown to provide a reliable description of the back shape and, intraindividually, to be highly correlated with the pertinent radiological parameters, with subjects standing in their typical relaxed standing posture [10, 11]. Besides angle measures, also horizontal distance measures, such as flèche cervicale and flèche lombaire, may be used to characterize sagittal back shape [12]. Therefore, using back surface measurements and the assessment of back shape parameters, it seems to be possible to assess the correlations between the craniofacial morphology and the sagittal contour in the cervical, thoracic, lumbar lordotic and pelvic regions in children without using spinal radiography [4, 13]. Although these optical methods provide highly accurate objective results without resorting to ionizing radiation, they are rarely used in orthodontic research [10, 14].
We conducted a prospective study to substantiate the observations in literature. Our working hypothesis was that there was an interrelation in preadolescents between the craniofacial morphology and the body posture. Here, we report in our study, correlations between cephalometric parameters and the flèche cervicale and flèche lombaire, virtually being parameters that quantify the sagittal deviation of the back contour, as well as the trunk inclination, which represents the sagittal inclination of the back surface measured from the real vertical line.
Materials and methods
Subjects
The sample consisted of 66 children with a mean age of 11.2 years (SD 1.6 years; minimum 8.0 years, maximum 15.8 years), of which 34 were male (mean age 11.5 years, SD 1.3 years; minimum 9.3 years, maximum 14.2 years) and 32 were female (mean age 10.9 years, SD 1.9 years; minimum 8.0 years, maximum 15.8 years).
The children were recruited during their first visit to the Department of Orthodontics, University of Münster when the initial orthodontic treatment records were prepared. Anamnestically, none of the examined children exhibited motor or neurological problems, internal diseases, orthopedic trauma or impairments. There was no history of spinal disorders or spinal surgery and all parents of the patients gave their informed consent to the study design according to the local ethics committee and the Helsinki criteria.
Cephalometric examination
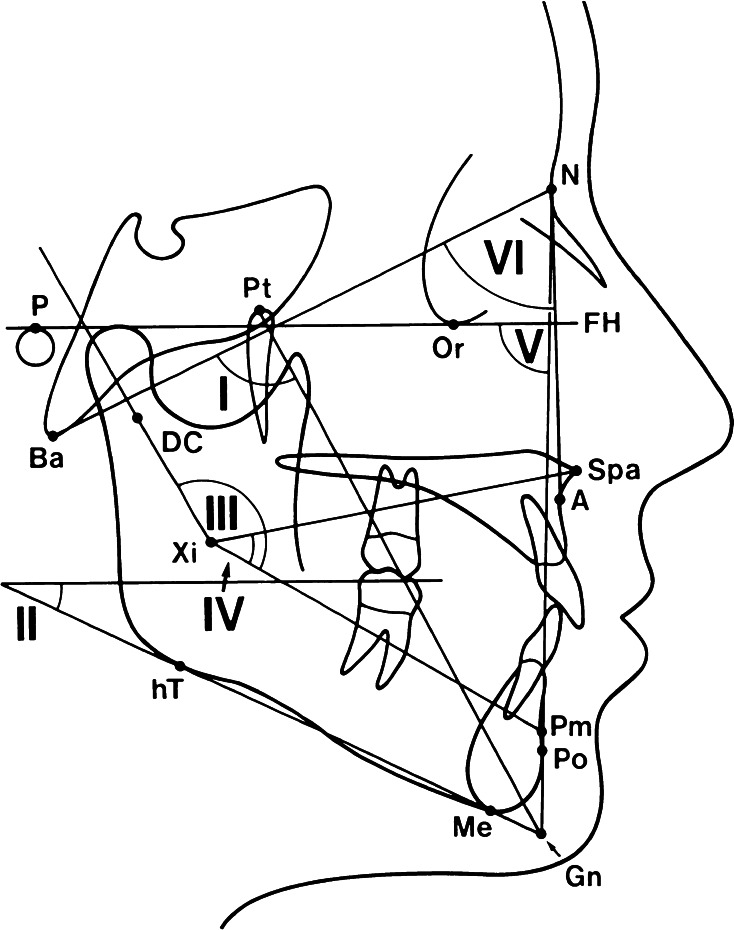
A standardized lateral skull radiograph (24 × 30 cm films, Planex Regular, Kodak, Germany) was taken (film–focus distance 3.2 m; final enlargement 1%; exposure data 15–25 mAs, 72–81 kV) of each patient. The radiographs were digitized (Scanner: Power Look III, Umax Systems, Willich, Germany; resolution 300 dpi) and a cephalometric tracing was performed by means of a cephalometric analysis software (Onyx Ceph Version 2.7.8, Image Instruments, Chemnitz, Germany) (Fig. 1).
Fig. 1.
Lateral cephalometric reference points, lines and angles determined in this study (1–6)
Six angular skeletal parameters were considered to be the most relevant for this study (facial axis, inner gonial angle, mandibular plane angle, lower facial height, facial depth and maxilla position) and were determined according to Fig. 1 and Table 1 [4, 15].
Table 1.
Cephalometric reference points: lines and measurement values (1–6)
| 1 | Ba-N–Pt-Gn | Facial axis |
| 2 | P-Or–Me-hT | Mandibular plane angle |
| 3 | Xi-DC–Xi-Pm | Inner gonial angle |
| 4 | Xi-Spa–Xi-Pm | Lower facial height |
| 5 | P-Or–N-Po | Facial depth |
| 6 | Ba-N–N-A | Maxillary position |
Rasterstereography
To measure spinal shape in the sagittal plane, the optical, contact-free method of rasterstereography was selected. To avoid radiation hazards, this method has been favoured to radiography, although it does not provide intrinsic radiological measures to be correlated with radiological craniofacial measurements. However, optical back shape measurement and analysis have been shown to be in good correlation with radiological findings [10, 11].
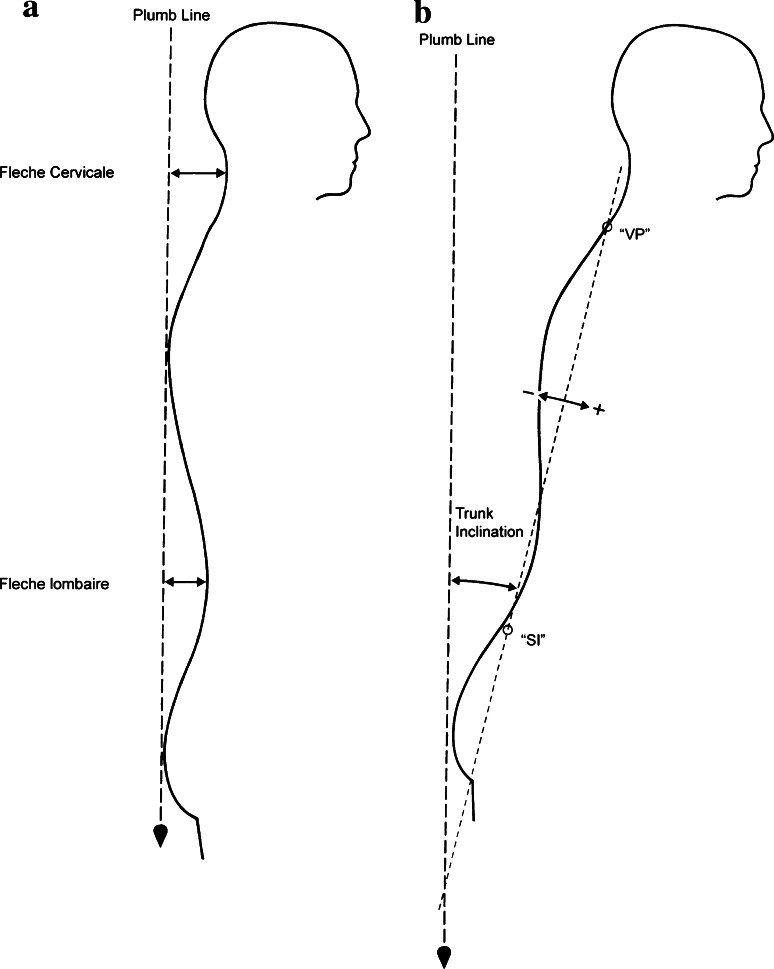
Rasterstereography (Formetric 2, Diers International GmbH, Schlangenbad, Germany) is a photogrammetric method to measure 3D back shape in a single shot of only 0.04 s [16, 17]. Following the recommendations of the supplier, the record is taken with the patient standing free without any trunk fixation. Motion artifacts due to postural sway therefore must be considered. During measurement, a bundle of light sections is projected on the patient’s back and is recorded from a different direction. Thus, image data allow accurate reconstruction of the back providing a digital model of the back ready for geometrical analysis (Fig. 2) [14]. Additionally, orientation data giving reference to the measurement lab, particularly to the vertical direction, are provided.
Fig. 2.
Rasterstereography is a three-dimensional analysis method for the back shape profile. A multitude of light sections is projected on the patient’s back from a different direction than that of the optical measurement unit, thereby compiling shape information along the section line
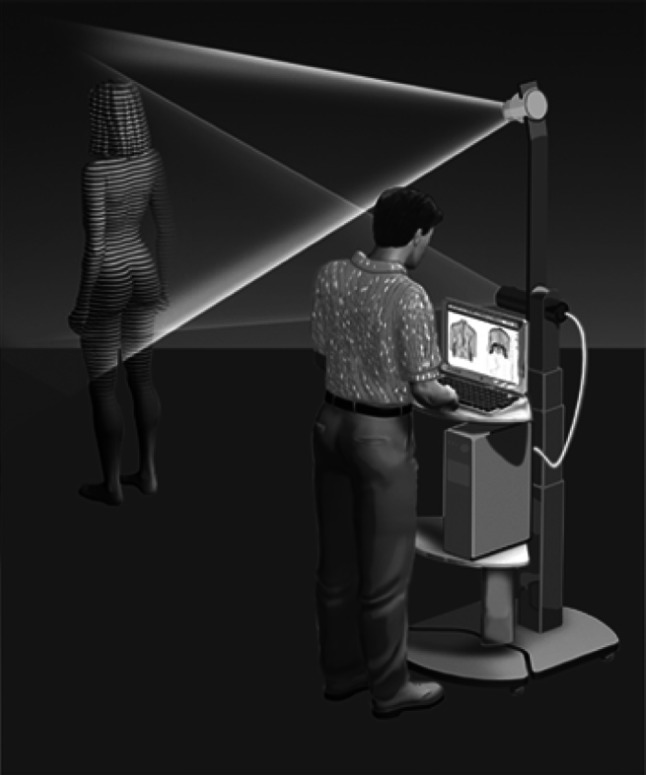
Sophisticated geometric analysis of the digital back model comprises automatic localization of three different anatomical landmarks and reconstruction of the sagittal back contour. The anatomical landmarks are the vertebra prominens (“VP”) and the left and right spina iliaca in the pelvic region. A further landmark is calculated as the geometric midpoint between the spinae (“SI”). Together with the VP landmark, it defines the localization of the sagittal profile on the back surface.
Geometric analysis of the sagittal profile is performed automatically and provides a set of different parameters to characterize body posture and the shape of the profile [18, 19]. To characterize the kyphotic and lordotic curves, the parameters of “flèche cervicale” and “flèche lombaire” are selected. These parameters measure the horizontal distance from a virtual plumb line to the apex of cervical and lumbar lordosis, respectively, instead of a real plumb line as described by Stagnara [20, 21]. For calculation, this plumb line is positioned to run along the kyphotic apex (Fig. 3a). To characterize body posture, the parameter of “trunk inclination” is calculated. It provides the angle spanned by the vertical direction and the connecting line between VP and SI (Fig. 3b). If the vertebra prominens is just above the midpoint between the spinae, this angle will be zero. It is positive in the case of leaning forward and negative in the case of leaning backward.
Fig. 3.
a Flèche cervicale and flèche lombaire presenting the sagittal alignment of the patient’s back. Both variables are measured as the sagittal distance between the lowest point of the cervical and lumbar spine, respectively, toward the plumb line. b Trunk inclination is measured as an angle between the line connecting the vertebral point (VP) and the midline of the right (DR) and left (DL) dimple points representing the spina iliaca (SI) of the upright standing patient toward the plumb line
Statistics
The patient’s data were blinded before the cephalometric analysis was carried out. The method error in determining the cephalometric measurements was assessed using Dahlberg’s formula (mean square error (SE2) = d2/2n (d = difference between repeated measurements; n = number of recorded radiographs) [22]. For the lateral cephalometric analysis, the method error was determined by repeating the measurements for six variables on randomly chosen radiographs at 2-week intervals by the same operator.
Data analysis was performed with the software SPSS 14.0 (Lead Tech., Chicago, IL, USA). A descriptive analysis was used to determine mean values, standard deviations (SD) and range. Further analysis was done by calculating Pearson’s correlation coefficient. For differentiation into different craniofacial types, the following threshold values for the cephalometric parameters were defined: facial axis, 90°; inner gonial angle, 150°; mandibular plane angle 23°; lower facial height, 45°; facial depth, 90°; and maxillary position 64°. Horizontal growth pattern was determined for facial axis values greater than 90°, inner gonial angle values less than 150°, mandibular plane angle less than 23° and lower facial height angles less than 45°. Vertical growth pattern was determined when the facial axis value was less than 90°, inner gonial angle greater than 150°, mandibular plane angles greater than 23° and lower facial height angles greater than 45°. To assess the direction and the strength of the interdependency between the detected cephalometric and body posture correlations, the R 2 values were calculated in the range diagram. The Mann–Whitney U test was applied to test for significant differences between the craniofacial types in terms of the parameters of back shape and posture. P < 0.05 was set as the level of significance in all tests. For the angular and distance measurements, the error of method was calculated according to Dahlberg [22]. The error levels were set at 0.5° and 0.5 mm according to Trpkova et al. [23].
Results
In the case of the cephalometric measurements, the standard errors of the mean values were less than 0.5° and 0.5 mm, respectively.
The cephalometric analysis of the lateral cephalometric radiographs revealed the following values:
for the facial axis, a mean value of 90.6° (SD 4.3°; minimum 82.1°, maximum 100.2°);
for the mandibular plane angle, 20.2° (SD 4.7°; minimum 12.3°, maximum 32.5°);
for the inner gonial angle, 149.5° (SD 6.0°; minimum 135.2°, maximum 165.2°);
for the angular lower facial height, 44.3° (SD 4.2°; minimum 36.1°, maximum 54.6°);
for the face depth, 89.8° (SD 3.4°; minimum 83.8°, maximum 96.1°);
for the maxilla position, 62.2° (SD 3.5°; minimum 54.8°, maximum 69.4°).
The analysis of the rasterstereographic parameters characterizing back shape and posture revealed:
for the flèche cervicale, a mean value of 23.7 mm (SD 8.5 mm; minimum 8.5 mm, maximum 40.3 mm);
for the flèche lombaire, 30.7 mm (SD 10.8 mm; minimum 10.4 mm, maximum 58.1 mm);
for the trunk inclination, 1.2° (SD 2.9°; minimum −4.4°, maximum 7.3°).
Correlation coefficients between cephalometric and rasterstereographic parameters are given in Table 2. Statistically significant correlations were found between the inner gonial angle and the flèche cervicale, the mandibular plane angle and the flèche lombaire, the inner gonial angle and the flèche lombaire, and the angular lower facial height and the flèche lombaire, as well as the inner gonial angle and the trunk inclination.
Table 2.
Statistics: cephalometric measurement values (mean, SD, minimum and maximum) in relation to the orthopedic variables (P value, r 2)
| Statistics | Flèche Cervicale | Flèche Lombaire | Trunk Inclination | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Minimum | Maximum | P value | r 2 | P value | r 2 | P value | r 2 | |
| Facial axis | 90.6° | 4.3° | 82.1° | 100.2° | 0.97 | 0.014 | 0.579 | 0.005 | 0.254 | 0.02 |
| Mandibular plane angle | 20.2° | 4.7° | 12.3° | 32.5° | 0.330 | 0.0001 | 0.028* | 0.073 | 0.173 | 0.029 |
| Inner gonial angle | 149.5° | 6.0° | 135.2° | 165.2° | 0.025* | 0.0001 | 0.002** | 0.146 | 0.003** | 0.127 |
| Lower facial height | 44.3° | 4.2° | 36.1° | 54.6° | 0.233 | 0.006 | 0.008** | 0.106 | 0.426 | 0.01 |
| Facial depth | 89.8° | 3.4° | 83.8° | 96.1° | 0.591 | 0.003 | 0.929 | 0.001 | 0.961 | 0.001 |
| Maxilla position | 62.2° | 3.5° | 54.8° | 69.4° | 0.101 | 0.03 | 0.354 | 0.013 | 0.870 | 0.001 |
* Significant, **highly significant
The r 2 values were as follows:
- For the relationship of the parameter flèche cervicale,
- with respect to the inner gonial angle, r 2 = 0.0001.
- For the flèche lombaire,
- with respect to the mandibular plane angle, r 2 = 0.073;
- with respect to the inner gonial angle, r 2 = 0.146;
- angular lower facial height, r 2 = 0.106.
- For the trunk inclination:
- with respect to the inner gonial angle, r 2 = 0.127.
Craniofacial morphology and body posture (Table 3)
Table 3.
Differences between the basal mesial or distal and the vertical or horizontal group of the flèche cervicale, -lombaire and the trunk inclination (P was set at <0.05) determined by Mann–Whitney U test
| Statistics | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cephalometric measurement | Facial axis | Mandibular plane | Inner gonial angle | Lower facial height | Facial depth | Maxilla position | ||||||||||||
| Skeletal Pattern | Vertical (n = 26) | Horizontal (n = 40) | P value | Vertical (n = 20) | Horizontal (n = 46) | P value | Vertical (n = 28) | Horizontal (n = 38) | P value | Vertical (n = 30) | Horizontal (n = 36) | P value | Mesial (n = 36) | Distal (n = 30) | P value | Mesial (n = 26) | Distal (n = 40) | P value |
| Flèche cervicale, mm (23.68 mm, ± 8.55 mm) | 23.84 ± 7.53 | 23.58 ± 9.24 | 0.958 | 26.28 ± 7.10 | 22.55 ± 8.94 | 0.074 | 26.19 ± 7.31 | 21.83 ± 9.01 | 0.04 | 23.29 ± 8.3 | 24.01 ± 8.82 | 0.643 | 22.56 ± 8.91 | 25.03 ± 8.03 | 0.198 | 25.54 ± 7.37 | 22.47 ± 9.12 | 0.093 |
| Flèche lombaire, mm (30.67 mm, ± 10.84 mm) | 29.63 ± 7.94 | 31.35 ± 12.42 | 0.462 | 35.52 ± 4.64 | 28.56 ± 12.06 | 0.007** | 36.63 ± 8.35 | 26.28 ± 10.48 | 0.001** | 36.61 ± 6.47 | 32.43 ± 7.312 | 0.017* | 30.44 ± 13.21 | 30.97 ± 7.24 | 0.959 | 32.08 ± 10.62 | 29.75 ± 11.01 | 0.248 |
| Trunk inclination, ° (1.21°, ± 2.90°) | 1.79 ± 2.81 | 0.83 ± 2.94 | 0.115 | 0.44 ± 2.41 | 1.55 ± 3.06 | 0.199 | −0.06 ± 2.59 | 2.15 ± 2.79 | 0.004** | 1.11 ± 2.92 | 1.29 ± 2.93 | 0.877 | 1.24 ± 3.18 | 1.18 ± 2.59 | 0.877 | 0.89 ± 2.72 | 1.43 ± 3.03 | 0.294 |
* Significant ** highly significant
Regarding the cephalometric parameter facial axis, the patients in the horizontal (n = 40) and vertical group (n = 26) revealed no significant differences in the body posture.
The mandibular plane angle concerning the flèche lombaire showed differences between the patients in the horizontal and vertical groups (P = 0.007). Patients with a horizontal growth pattern had smaller mean values (28.6 mm; n = 46) compared to the vertical ones (35.5 mm; n = 20).
The group differences regarding the inner gonial angle were significant with respect to the flèche cervicale (P = 0.04); the horizontal group of patients revealed significantly lower (21.8 mm; n = 38) values than those in the vertical group (26.2 mm; n = 28). Likewise, the flèche lombaire was significantly lower (P = 0.001) in the case of the horizontal group (26.3 mm; n = 38) compared to the vertical group of patients (36.6 mm; n = 28). Similarly, the two groups differed significantly (P = 0.004) in the trunk inclination angle, indicating that patients from the horizontal group lean slightly forward by 2.2° in contrast to the vertical group, where perfect vertical alignment (−0.1°) is observed.
The flèche lombaire was different (P = 0.017) in the case of the lower facial height, indicating that horizontal patients reveal smaller (32.4 mm; n = 36), and vertical patients greater, values (36.6 mm; n = 30).
Sagittal jaw position and body posture
No significant differences were detected regarding the sagittal position of the upper or lower jaw and flèche cervicale, flèche lombaire or the trunk inclination, respectively.
Discussion
The patient sample in this study consisted of a specific orthodontic patient group. There was no control group because of ethical reasons: avoiding X-ray exposure of the patients when producing lateral cephalometric radiographs. This resulted in a wide range of cephalometric measurement values in the vertical and sagittal craniofacial morphology. The variance in cephalometric variables was the same as the variance seen in previous studies [24]. The cephalometric analysis of the patient’s lateral X-rays revealed different groups of craniofacial morphology:
mandibular prognatism or retrognathism;
maxillary prognatism or retrognathism;
vertical growth pattern;
horizontal growth pattern.
As described in literature, the authors are not aware of an objective and reproducible examination method for the documentation of body posture [1, 3]. Lateral thoracic and pelvic X-rays could have been used for the analysis of posture, but would have involved radiation exposure for the patients. Therefore, rasterstereography was applied due to its accuracy and easy integration into a scientific protocol [10, 14]. The implementation of rasterstereography in orthodontic and orthopedic studies has been described in former studies [4, 13, 25]. The sagittal curvature reliability of rasterstereography was demonstrated by Hackenberg et al., when compared with X-rays [26, 27].
The present study reveals correlations between the angular cephalometric parameters describing the vertical or horizontal growth pattern of the mandibula related to the cranium (angular lower facial height), as well as the vertical type of the mandibula itself (mandibular plane angle and inner gonial angle), the back shape parameters, flèche cervicale and lombaire, and trunk inclination.
We conclude that our working hypothesis about an existing correlation between different craniofacial morphological types and sagittal spinal posture with respect to flèche cervicale/lombaire and trunk inclination is valid within the limitations of the methods of this study. Furthermore, by a sophisticated analysis of the correlations, we were able to separate two different groups of patients exhibiting correlated spinal and craniofacial morphology. Patients with a vertical growth pattern in the mandibula exhibit a more pronounced sagittal curvature manifested by larger values for the flèche cervicale as well as for the flèche lombaire parameters. In contrast, children with a more horizontal growth pattern reveal a flattened sagittal curvature with smaller values of the flèche parameters.
However, the analysis of neurologically or muscularly balanced interactions is beyond the scope of this study, which is limited to the statistical description of morphological correlations between craniofacial growth patterns in preadolescents. Motion artifacts due to postural sway may affect the parameters of trunk inclination and of spinal curvature. Generally, the effect is stronger on postural parameters, such as trunk inclination, than on sagittal shape parameters such as kyphotic and lordotic angle or flèche parameters [19, 28]. In addition, postural sway results in a broadening of the statistical distribution, thus weakening the acuity of the statistical decision. Using pads to align the patients might have resolved this problem, however, at the expense of reflectory artifacts.
Further investigations on the interaction and the individual spinal development in association with craniofacial growth seem to be necessary to understand these correlations. No significant correlations were determined between sagittal position of the mandibula or maxilla with respect to the cranium and the examined orthopedic parameters. The trunk inclination showed relevant connections only to the inner gonial angle. Possible explanations can be found in studies by Solow et al. and Huggare et al. It can be summarized as the “soft tissue stretching hypothesis”, indicating that an increased force level produced by bending the head backward results in an increased stretching of the soft tissues of the head and the neck layers, influencing the craniofacial growth and leading to a more vertical growth pattern [24, 29, 30]. This would explain the increased flèche cervicale values in our vertical patient group. Possibly, the increased flèche cervicale leading to a more curved cervical lordosis resulted in an increased thoracic and lumbar curvature. This sagittal alignment would therefore be developmentally connected to the craniofacial complex. Possible interactions by changing the craniofacial growth pattern, as it is possible to a certain extent by the functional appliance treatment in orthodontics, should be analyzed in further randomized clinical trials.
Our results agree with Nobili et al., who showed correlations between the sagittal jaw position and the body posture in the thoracic and cervical region [31]. The results of our study are at variance with Michelotti et al. [3] who stated that there were no statistically significant correlations between craniofacial morphology and trunk posture with the exception of a positive correlation between cervical curvature and craniofacial morphology.
Conclusions
Contrary to the craniofacial sagittal growth pattern, the vertical growth pattern determined by the mandibular plane angle, the inner gonial angle and the angular lower facial height is in close correlation with the sagittal body posture described by the flèche cervicale, flèche lombaire and trunk inclination.
In the case of the three craniofacial parameters showing this close correlation, the groups established on the basis of the different growth patterns were differentiated by the sagittal back contour indicators of the lower spine sections.
The rasterstereography used to determine the sagittal body posture at several levels proved to be an appropriate (radiation free) examination method for observation of similar correlations.
Conflict of interest statement
None.
Contributor Information
Carsten Lippold, Email: lippold@uni-muenster.de.
Emil Segatto, Phone: +36-30-9969800, FAX: +36-1-4731447, Email: dr.segatto@chello.hu.
András Végh, Email: aveghdr@chello.hu.
Burkhard Drerup, Email: drerup@uni-muenster.de.
Tatjana Moiseenko, Email: tdm@uni-muenster.de.
Gholamreza Danesh, Email: siamak@uni-muenster.de.
References
- 1.Korbmacher H, Eggers-Stroeder G, Koch L, Kahl-Nieke B. Correlations between anomalies of the dentition and pathologies of the locomotor system- a literature review. J Orofac Orthop. 2004;65:190–203. doi: 10.1007/s00056-004-0305-3. [DOI] [PubMed] [Google Scholar]
- 2.Festa F, Tecco S, Dolci M, Ciufolo F, Di Meo S, Filippi MR, Ferritto AL, D′Attillio M. Relationship between cervical lordosis and facial morphology in Caucasian women with skeletal class II malocclusion: a cross-sectional study. Cranio. 2003;21:121–129. doi: 10.1080/08869634.2003.11746240. [DOI] [PubMed] [Google Scholar]
- 3.Michelotti A, Manzo P, Farella M, Martina R. Occlusion and posture: is there evidence of correlation? Minerva Stomatol. 1999;48:525–534. [PubMed] [Google Scholar]
- 4.Lippold C, Danesh G, Schilgen M, Drerup B, Hackenberg L. Relationship between Thoracic, Lordotic, and Pelvic Inclination and Craniofacial Morphology in Adults. Angle Orthod. 2006;76:779–785. doi: 10.1043/0003-3219(2006)076[0779:RBTLAP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Segatto E, Jianu R, Marschalko P, Vegh A. Dentofacial features of children diagnosed with scoliosis and Scheuermann’s disease. TMJ. 2006;56:259–264. [Google Scholar]
- 6.Segatto E, Lippold C, Vegh A. Craniofacial features of children with spinal deformities. BMC Musculoskelet Disord. 2008;9:169. doi: 10.1186/1471-2474-9-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Attilio M, Epifania E, Ciuffolo F, Salini V, Filippi MR, Dolci M, Festa F, Tecco S. Cervical lordosis angle measured on lateral cephalograms; findings in skeletal class II female subjects with and without TMD: a cross-sectional study. Cranio. 2004;22:27–44. doi: 10.1179/crn.2004.005. [DOI] [PubMed] [Google Scholar]
- 8.D’Attilio M, Caputi S, Epifania E, Festa F, Tecco S. Evaluation of cervical posture of children in skeletal class I, II, and III. Cranio. 2005;23:219–228. doi: 10.1179/crn.2005.031. [DOI] [PubMed] [Google Scholar]
- 9.Stagnara P, De Mauroy JC, Dran G, Gonon GP, Constanzo G, Dimnet J, Pasquet A. Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7:335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Drerup B. The measurement of the kyphotic angle by contact-free registration of back shape. Z Orthop Ihre Grenzgeb. 1982;120:64–70. doi: 10.1055/s-2008-1051577. [DOI] [PubMed] [Google Scholar]
- 11.Crawford RJ, Price RI, Singer KP. The effect of interspinous implant surgery on back surface shape and radiographic lumbar curvature. Clin Biomech. 2009;24:467–472. doi: 10.1016/j.clinbiomech.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Neugebauer H. Back measuring device for mass examination. Z Orthop Ihre Grenzgeb. 1970;108:395–406. [PubMed] [Google Scholar]
- 13.Sinko K, Grohs JG, Millesi-Schobel G, Watzinger F, Turhani D, Undt G, Baumann A. Dysgnathia, orthognathic surgery and spinal posture. Int J Oral Maxillofac Surg. 2006;35:312–317. doi: 10.1016/j.ijom.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Hierholzer E, Drerup B, et al. High-resolution rasterstereography. In: D’Amico M, et al., editors. Three-dimensional analysis of spinal deformities. Amsterdam: IOS Press; 1995. pp. 435–439. [Google Scholar]
- 15.Proffit WR. Contemporary orthodontics. 3. St Louis: Mosby; 2000. [Google Scholar]
- 16.Frobin W, Hierholzer E. Rasterstereography: a photogrammetric method for measurement of body surfaces. Photogramm Eng Remote Sens. 1981;47:1717–1724. [PubMed] [Google Scholar]
- 17.Drerup B, Hierholzer E. Back shape measurement using video rasterstereography and three-dimensional reconstruction of spinal shape. Clin Biomech. 1994;9:28–36. doi: 10.1016/0268-0033(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 18.Drerup B, Hierholzer E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J Biomech. 1987;20:961–970. doi: 10.1016/0021-9290(87)90325-3. [DOI] [PubMed] [Google Scholar]
- 19.Drerup B, Hierholzer E, Ellger B, et al. Shape analysis of the lateral and frontal projection of spine curves assessed from rasterstereographs. In: Sevastik JA, et al., editors. Research into spinal deformities. 1. Amsterdam: IOS Press; 1997. pp. 271–275. [Google Scholar]
- 20.Stagnara P. Ambulante orthopädische Behandlung der Scheuermannschen Krankheit im floriden Stadium. Schweiz med Wschr. 1965;95:674. [Google Scholar]
- 21.Stagnara P, du Peloux J, Fauchet R. Traitement orthopaedique ambulatoire de la maladie de Scheuermann en periode devolution. Rev Chir Orthop. 1966;52:585–600. [Google Scholar]
- 22.Dahlberg B. Statistical methods for medical and biological students. New York: Interscience Publications; 1940. [Google Scholar]
- 23.Trpkova B, Major P, Prasad N, Nebbe B. Cephalometric landmarks identification and reproducibility: a meta-analysis. Am J Orthod Dentofac Orthop. 1997;112:165–170. doi: 10.1016/S0889-5406(97)70242-7. [DOI] [PubMed] [Google Scholar]
- 24.Solow B, Sandham A. Cranio-cervical posture: a factor in the development and function of the dentofacial structures. Eur J Orthod. 2002;24:447–456. doi: 10.1093/ejo/24.5.447. [DOI] [PubMed] [Google Scholar]
- 25.Lippold C, Danesh G, Hoppe G, Drerup B, Hackenberg L. Trunk inclination, pelvic tilt and pelvic rotation in relation to the craniofacial morphology in adults. Angle Orthod. 2007;77:29–35. doi: 10.2319/121205-434R.1. [DOI] [PubMed] [Google Scholar]
- 26.Hackenberg L, Hierholzer E, Potzl W, Götze C, Liljenqvist U. Rasterstereographic back shape analysis in idiopathic scoliosis after posterior correction and fusion. Clin Biomech. 2003;18:883–889. doi: 10.1016/S0268-0033(03)00169-4. [DOI] [PubMed] [Google Scholar]
- 27.Hackenberg L, Hierholzer E, Pötzl W, Götze C, Liljenqvist U. Rasterstereographic back shape analysis in idiopathic soliosis after anterior correction and fusion. Clin Biomech. 2003;18:1–8. doi: 10.1016/S0268-0033(02)00165-1. [DOI] [PubMed] [Google Scholar]
- 28.Hierholzer E, Drerup B. Rasterstereographic functional examinations: precision measurement of kyphosis and lordosis. In: Stokes IAF, editor. Research into spinal deformities. 2. Amsterdam: IOS Press; 1999. pp. 101–104. [Google Scholar]
- 29.Huggare JAV, Cooke MS. Head posture and cervicovertebral anatomy as mandibular growth predictors. Eur J Orthod. 1994;16:175–180. doi: 10.1093/ejo/16.3.175. [DOI] [PubMed] [Google Scholar]
- 30.Huggare JAV. The first cervical vertebra as an indicator of mandibular growth. Eur J Orthod. 1989;11:10–16. doi: 10.1093/oxfordjournals.ejo.a035959. [DOI] [PubMed] [Google Scholar]
- 31.Nobili A, Adversi R. Relationship between posture and occlusion: a clinical and experimental investigation. Cranio. 1996;14:274–285. doi: 10.1080/08869634.1996.11745978. [DOI] [PubMed] [Google Scholar]