Abstract
C1–2 polyaxial screw-rod fixation is a relatively new technique. While recognizing the potential for inadvertent vertebral artery injury, there have been few reports in the literature outlining all the possible complications. Aim of this study is to review all cases of C1 lateral mass screws insertion with emphasis on the evaluation of potential structures at risk during the procedure. We retrospectively reviewed all patients in our unit who had C1 lateral mass screw insertion over a 2-year period. The C1 lateral mass screw was inserted as part of an atlantoaxial stabilization or incorporated into a modular occiput/subaxial construct. Outcome measures included clinical and radiological parameters. Clinical indicators included age, gender, neurologic status, surgical indication and the number of levels stabilized. Intraoperative complications including blood loss, vertebral artery injury or dural tears were recorded. Postoperative pain distribution and neurological deficit were recorded. Radiological indicators included postoperative plain radiographs to assess sagittal alignment and to check for screw malposition or construct failure. A total of 18 lateral mass screws were implanted in 9 patients. There were three male and six female patients who had C1 lateral mass screw insertion in this unit. Two patients had atlantoaxial stabilization for C2 fracture. There were four patients with rheumatoid arthritis whose C1 lateral mass screws were inserted as part of an occipitocervical or subaxial cervical stabilization. There was no vertebral artery injury, no cerebrospinal fluid leak and minimal blood loss in all patients. Three patients developed postoperative occipital neuralgia. This neuralgia was transient, in one of the patients having settled at 6-week follow-up. In the other two patients the neuralgia was unresolved at time of latest follow-up but was adequately controlled with appropriate pain management. Postoperatively no patient had radiographic evidence of construct failure and all demonstrated excellent sagittal alignment. It has been reported that the absence of threads on the upper portion of the long shank screw may protect against neural irritation. However, insertion of the C1 lateral mass screw necessitates careful caudal retraction of the C2 dorsal root ganglion. The insertion point for the C1 lateral mass screw is at the junction of the C1 posterior arch and the midpoint of the posterior inferior part of the C1 lateral mass. Two patients in our series suffered occipital neuralgia post-insertion of C1 lateral mass screws. This highlights the potential for damage to the C2 nerve root during C1 lateral mass screw placement.
Keywords: C1 lateral mass screw, Posterior atlantoaxial stabilization, Occipital neuralgia, C2 nerve root, C2 dorsal root ganglion
Introduction
C1 lateral mass screw fixation was first described in 1994 by Goel and Laheri [3] and popularized by Harms and Melcher in 2001 [6]. The advantages of this technique over the Magerl transarticular screw technique include the intraoperative ability to reduce C1/2 subluxation and a theoretical reduction in the risk of vertebral artery injury [1, 2]. While occipital neuralgia has been recognized as a possible complication of C1 lateral mass fixation, there have been few documented reports to date.
Potential causes of postoperative occipital neuralgia include irritation of the nerve root by the C1 lateral mass screw or as a result of traction on the dorsal root ganglion during screw insertion.
The design of C1 lateral mass screws includes an 8 mm smooth portion that remains above the posterior surface of the C1 lateral mass. This is specifically aimed at reducing C2 root irritation (Fig. 1).
Fig. 1.

C1 lateral mass screw with 8-mm section without threads to reduce chance of irritation to C2 nerve root
Harms and Melcher [6] reported no cases of occipital neuralgia in a series of 37 consecutive cases.
Goel et al. [3, 4] published results of 160 patients, none of whom experienced occipital neuralgia. In his description of the original technique, he described the importance and relevance of sectioning of the C2 ganglion for wide exposure of the region.
However, Gunnarsson et al. reported on three cases of occipital neuralgia in a series of 25 patients and Rhee et al. reported a case report of occipital neuralgia after C1 lateral mass screws [6, 10]. There have been increasing reports in recent literature of this devastating complication and from our unit we report two patients who developed unilateral occipital neuralgia after placement of C1 lateral mass screws.
Methods
We report retrospectively on nine consecutive cases of C1 lateral mass screw fixation over a 2-year period 2004–2006. Indications for surgery included: odontoid fracture non-union (2 patients), rheumatoid arthritis (4 patients) and tumor (3 patients). The C1 lateral mass screw was inserted as part of an atlantoaxial stabilization (2 patients) or incorporated into a longer construct (7 patients).
All patients had routine preoperative X-ray, CT and MRI. Two of the rheumatoid patients were myelopathic preoperatively; there were no neurological deficits in the other seven patients.
All patients were anaesthesised and placed prone on a Mayfield headrest. Surgical technique was identical to that described by Harms and Melcher [6]. All drilling and screw placement of C1 and C2 was performed under image intensification. Caudal retraction of the C2 nerve root dorsal ganglion was necessary in all cases to facilitate drilling, tapping and C1 screw insertion. Haemostasis in the region of the C2 root was achieved using a combination of bipolar electrocautery, gelfoam with thrombin and cotton pledgets.
All patients were immobilized in a soft cervical collar postoperatively. Intraoperative complications including blood loss, vertebral artery injury or dural tears were also assessed. Note was made of any postoperative wound or pain issues or an altered neurological state. Postoperative and follow-up radiographs were assessed for sagittal alignment, screw position, and construct failure (Fig. 2).
Fig. 2.
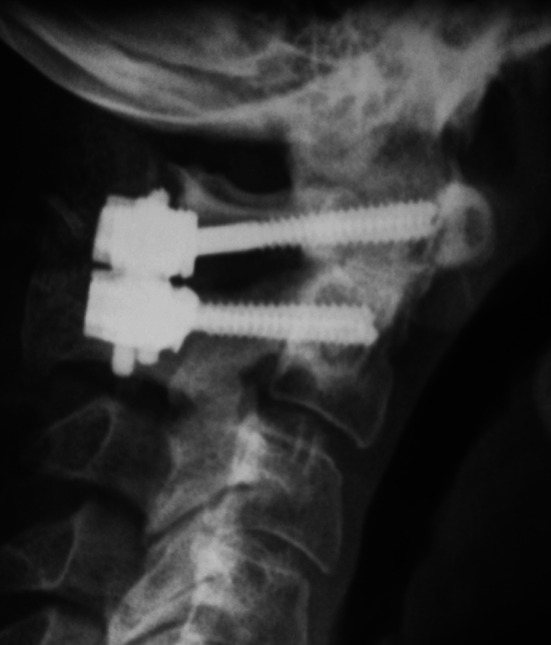
Postoperative cervical spine lateral radiograph of C1 lateral mass screw
Results
A total of 18 C1 lateral mass screws were implanted in 9 patients. There were three male and six female patients included in the study. Patient age ranged from 23 to 78. All patients had a minimum follow-up of 2 years.
There were no intraoperative complications and no alteration in neurological status of any patient.
Three patients complained of postoperative occipital neuralgia. This was transient in one patient having settled at 6-week follow-up. The other two patients with persistent neuralgia had odontoid fracture non-unions. Both patients experienced pain that was constant in nature. Neither case occurred early in the series and solid C1/2 fusion was achieved in both cases. Both patients had CT performed to confirm solid fusion. There was no evidence radiographically that there was loosening of the constructs, aseptic or infected. White cell counts, erythrocyte sedimentation rates and C reactive proteins were recorded in patients to rule out low-grade infection. One patient had removal of instrumentation at 9 months postoperatively but his pain persisted. Cultures taken at time of construct removal were negative. At 2-year follow-up both patients’ occipital neuralgia remained, necessitating referral to the Clinical Pain Service.
At 2-year follow-up sagittal alignment was satisfactory in all cases, there were no cases of pseudoarthrosis or construct failure.
Discussion
A variety of techniques have been described to achieve fixation of the upper cervical spine in the presence of atlantoaxial instability. These have evolved from posterior wiring techniques of Brooks, Gallie and Sonntag to screw fixation techniques. The Magerl transarticular technique provides significant fixation advantages over wiring techniques and up to a 100% fusion rate [5, 7–9, 11]. However, anatomical reduction of C1 on C2 prior to screw insertion is required and there is potential for inadvertent vertebral artery injury [12]. Various anatomical factors such as an increased thoracic kyphosis may interfere with transarticular screw insertion.
Independent screw fixation of C1 (lateral mass) and C2 (pedicle) substantially reduces the risk of vertebral artery injury and facilitates reduction of C1 on C2 following screw insertion. The technique can also be used in cases of fixed C1/2 subluxation and avoids the need to place instrumentation under the posterior arch of C1 when stabilizing the atlantoaxial complex [6].
The dimensions of the C1 lateral mass are sufficient to accommodate an appropriately placed 3.5-mm screw with minimal risk to neurovascular structures [1]. His technique requires caudal retraction of the C2 dorsal root ganglion to expose the C1 lateral mass screw entry point. Excessive caudal retraction may contribute to postoperative occipital neuralgia. Reduction of C1 onto C2 may also be a contributing factor to the development of the occipital neuralgia.
It has been assumed that C2 root irritation could be avoided by the absence of threads on the initial 8 mm of screw [6]. However, Goel et al. [3, 4] used fully threaded screws in 160 patients and reported no cases of occipital neuralgia.
Conclusion
Occipital neuralgia may occur following the insertion of C1 lateral mass screws. It most likely results for excessive retraction of the C2 root during screw insertion and every attempt should be made to avoid this.
In this series, two patients had persistent pain at 2-year follow-up and it did not respond to removal of instrumentation. The occurrence of occipital neuralgia after C1 lateral mass screw insertion is a debilitating complication with increasing numbers of cases being reported in the literature
We therefore recommend specific reference to this complication when obtaining informed patient consent.
References
- 1.Currier BL, Yaszemski ML. The use of C1 lateral mass fixation in the cervical spine. Curr Opin Orthop. 2004;15:184–191. doi: 10.1097/01.bco.0000127817.76306.61. [DOI] [Google Scholar]
- 2.Fiore AJ, Haid RW, Rodts GE, Subach BR, Mummaneni PV, Riedel CJ, Birch BD. Atlantal lateral mass screws for posterior spinal reconstruction: technical note and case series. Neurosurg Focus. 2002;12(1):E5. doi: 10.3171/foc.2002.12.1.6. [DOI] [PubMed] [Google Scholar]
- 3.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 4.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002;51:1351–1357. doi: 10.1097/00006123-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Grob D, Jeanneret B, Aebi M, Markwalder TM. Atlanto-axial fusion with transarticular screw fixation. J Bone Jt Surg Br. 1991;73:972–976. doi: 10.1302/0301-620X.73B6.1955447. [DOI] [PubMed] [Google Scholar]
- 6.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 7.Henriques T, Cunningham BW, Olerud C, et al. Biomechanical comparison of five different atlantoaxial posterior fixation techniques. Spine. 2002;25:2877–2883. doi: 10.1097/00007632-200011150-00007. [DOI] [PubMed] [Google Scholar]
- 8.Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 9.Melcher RP, Puttlitz CM, Kleinstueck FS, et al. Biomechanical testing of posterior atlantoaxial fixation techniques. Spine. 2002;27:2435–2440. doi: 10.1097/00007632-200211150-00004. [DOI] [PubMed] [Google Scholar]
- 10.Rhee WT, You SH, Kim SK, Lee SY. Troublesome occipital neuralgia developed by c1–c2 harms construct. J Korean Neurosurg Soc. 2008;43(2):111–113. doi: 10.3340/jkns.2008.43.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith MD, Kotzar G, Yoo J, et al. A biomechanical analysis of atlantoaxial stabilization methods using a bovine model: C1/2 fixation analysis. Clin Orthop Relat Res. 1993;290:285–295. [PubMed] [Google Scholar]
- 12.Stokes JK, Villavicencio AT, Liu PC, et al. Posterior atlantoaxial stabilization: new alternative to C1–2 transarticular screws. Neurosurg Focus. 2002;12(1):E6. doi: 10.3171/foc.2002.12.1.7. [DOI] [PubMed] [Google Scholar]


