Abstract
Ossification of the posterior longitudinal ligament (OPLL) is a common spinal disorder that presents with or without cervical myelopathy. Furthermore, there is evidence suggesting that OPLL often coexists with cervical disc hernia (CDH), and that the latter is the more important compression factor. To raise the awareness of CDH in OPLL for spinal surgeons, we performed a retrospective study on 142 patients with radiologically proven OPLL who had received surgery between January 2004 and January 2008 in our hospital. Plain radiograph, three-dimensional computed tomography construction (3D CT), and magnetic resonance imaging (MRI) of the cervical spine were all performed. Twenty-six patients with obvious CDH (15 of segmental-type, nine of mixed-type, two of continuous-type) were selected via clinical and radiographic features, and intraoperative findings. By MRI, the most commonly involved level was C5/6, followed by C3/4, C4/5, and C6/7. The areas of greatest spinal cord compression were at the disc levels because of herniated cervical discs. Eight patients were decompressed via anterior cervical discectomy and fusion (ACDF), 13 patients via anterior cervical corpectomy and fusion (ACCF), and five patients via ACDF combined with posterior laminectomy and fusion. The outcomes were all favorable. In conclusion, surgeons should consider the potential for CDH when performing spinal cord decompression and deciding the surgical approach in patients presenting with OPLL.
Keywords: Posterior longitudinal ligament ossification, Cervical, Disc hernia, Magnetic resonance imaging, Cerebrospinal fluid leakage
Introduction
Ossification of the posterior longitudinal ligament (OPLL), characterized by the heterotopic bone formation in the posterior ligament, is a common spinal disorder in Japan and other Asian countries [1, 2]. It is known that the presence of prominent OPLL does not always indicate the presence of cervical myelopathy [3]. Furthermore, OPLL often coexists with other spinal disorders including cervical disc hernia (CDH); for example, 30 of 54 cases (55.6%) of OPLL were reported to be accompanied by disc hernia [4]. The clinical symptoms in patients presenting with OPLL appear or aggravate due to CDH, and as such, a herniated cervical disc is considered an important compression factor. However, the clinical and radiographic features, and surgical management of OPLL in combination with CDH have not been well described.
In the present study, we reviewed the neurological state, type of OPLL, magnetic resonance imaging (MRI) findings, and choice of surgical approach in patients presenting with OPLL associated with CDH in our hospital.
Materials and methods
Patient population
Between January 2004 and January 2008, a total of 142 patients presenting with OPLL underwent surgery in our Orthopedic Department. We examined the patient’s case histories, clinical manifestations, radiographic data, intraoperative findings, and the outcomes in detail. Twenty-six patients with disc hernia as the major compression factor according to MRI and intraoperative findings were selected for our study.
Radiological evaluation
All patients had a preoperative plain radiograph, three-dimensional computed tomography construction (3D CT), and MRI of the cervical spine. The diameter of the spinal canal was measured from the middle of the posterior surface of the vertebral body to the nearest point on the corresponding spinolaminar line. The mean value of the measures at C2–C7 represented the spinal canal diameter for that patient. The occupying rate was defined as the greatest thickness of OPLL divided by the anteroposterior diameter of the bony spinal canal on the axial CT image. On the sagittal image, OPLL was classified into three types: segmental, continuous, or mixed according to a previous classification [5]. We also examined the extent of OPLL. The grade of spinal cord compression from OPLL was classified into three ranks by MRI: I, no dural compression; II, dural compression but with no compression of the cord; or III, indentation of the cord. The level of disc hernia was examined in sagittal and axial MRI scans, and the greatest compression level was recorded.
Surgical management
All 26 patients received anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion (ACCF), or ACDF combined with posterior laminectomy and fusion. We performed ACDF in patients with disc hernia as the major compression factor and with Grade II spinal cord compression resulting from OPLL. In patients with Grade III compression from ossified ligament, an occupying rate less than 50%, and with no more than three ossified segments, ACCF was chosen to remove the herniated disc and the ossified ligament simultaneously. ACDF combined with posterior laminectomy and fusion was performed in patients with Grade III compression, an occupying rate more than 50%, or more than three ossified segments.
Surgical technique
Under general anesthesia, patients were placed in the supine position with the neck slightly extended. The cervical spine was exposed through a standard right-side anterior approach. The appropriate surgical level was confirmed by intraoperative radiography. During the whole decompression procedure the removal of the cervical disc was the most important step. The herniated portion of the disc, particularly in the posterior of longitudinal ligament, should be removed first using pituitary forceps, thus protecting the spinal cord from the follow-up decompression procedure. In ACDF, the osteophyte and ossified ligament were removed by diamond drill until they were thin enough, and then were cut with 1–2-mm Kerrison rongeur and curettes. This procedure facilitated the use of Kerrison rongeur and curettes because of the interruption of OPLL at the disc level and the hole in the unossified ligament due to CDH. In ACCF, after the discectomy procedure described above, the vertebral bodies were partially removed using an appropriate rongeur. The residual vertebral bodies and OPLL were removed by diamond drill until the OPLL was cut paper thin. The OPLL was then separated from the dural matter using a specialized microdissector. The head of this dissector was a hook with a narrow slot that was inserted under the OPLL from the unossified ligament at disc level, then rotated and slightly lifted. The ligament was cut off by scalpel along the slot. The OPLL was then meticulously separated using the microdissector and removed using 1–2-mm Kerrison rongeur and microcurettes. The width of the trough should extend 20 mm or nearly the width of the spinal canal to obtain a complete resection of the ossified mass. The posterior vertebral marginal was slightly cut to avoid secondary compression after expansion of the dural sac. After decompression, the titanium mesh cage filled with autologous bone fragments or iliac crest strut, together with the anterior cervical plate, were used to restore the stability of the involved segments. The process of posterior laminectomy and fusion was performed as typical.
Clinical assessment
The Japanese Orthopedic Association (JOA) scoring system was used to evaluate the neurological status before and after the operation. An improvement rate (IR) was calculated as IR = (postoperative JOA score – preoperative JOA score)/(17 – preoperative JOA score) × 100%. Surgical outcome was defined by the IR as follows: excellent (IR ≥ 75%), good (75% > IR ≥ 50%), fair (50% > IR ≥ 25%), and poor (IR < 25%).
Statistical analysis
The student t test was used for comparison of paired data. Differences between patients with and without CDH were assessed by the Chi-squared test. P value less than 0.05 was considered statistically significant. Results are presented as mean ± standard deviation (SD).
Results
Clinical features
Of our 142 OPLL patients, 26 (18.3%) presented with obvious cervical disc hernia. There were 17 men and nine women, with an age range of 45–68 years (mean 54.3 ± 6.6 years). Past history showed no clinical symptom in three patients (11.5%), minor numbness in 19 patients (73.1%), weakness in six patients (23.1%), and gait disturbance in two patients (7.7%), while no patients presented with sphincter dysfunction. A remote cause in these 26 patients was relatively common, and included a fall to level ground in five patients (19.2%), traffic accidents in two patients (7.7%), and violent massage manipulation in one patient (3.9%). There was no remote cause in the other 18 patients (69.2%). The duration of symptoms ranged from 1 to 12 months (mean 9.8 ± 2.2 months) (Table 1). The most common presenting clinical symptoms after aggravation were numbness in 23 patients (88.5%), weakness in 17 patients (65.4%), gait disturbance in seven patients (26.9%), upper extremity radicular symptoms in three patients (11.5%), and bladder dysfunction in one patient (3.8%). The preoperative Japanese Orthopaedic Association (JOA) score ranged from 5 to 12 points (mean 9.3 ± 1.8).
Table 1.
Difference in patients with OPLL between CDH present and CDH absent
| CDH present (26) | CDH absent (116) | P value | |
|---|---|---|---|
| Mean age (years) | 54.3 ± 6.6 | 56.1 ± 5.9 | >0.05 |
| Gender | |||
| Male | 17 (65.4) | 82 (70.7) | >0.05 |
| Female | 9 (34.6) | 34 (29.3) | |
| Duration of symptoms (months) | 9.8 ± 2.2 | 12 ± 3.1 | <0.01 |
| Remote cause | |||
| Yes | 8 (30.8) | 19 (16.4) | >0.05 |
| No | 18 (69.2) | 97 (83.6) | |
| Mean spinal canal diameter (mm) | 14.7 ± 1.2 | 14.2 ± 1.1 | >0.05 |
| Mean occupying rate (%) | 38.8 ± 9.3 | 49.7 ± 8.2 | <0.01 |
| Type of OPLL | |||
| Segmental (%) | 15 (57.7) | 45 (38.8) | >0.05 |
| Mixed (%) | 9 (34.6) | 38 (32.8) | >0.05 |
| Continuous (%) | 2 (7.7) | 33 (28.4) | <0.05 |
| Mean extent of OPLL | 3.3 ± 0.9 | 3.0 ± 0.2 | >0.05 |
Radiological findings
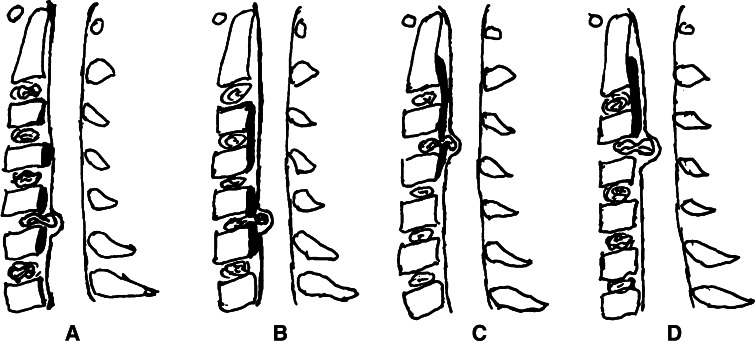
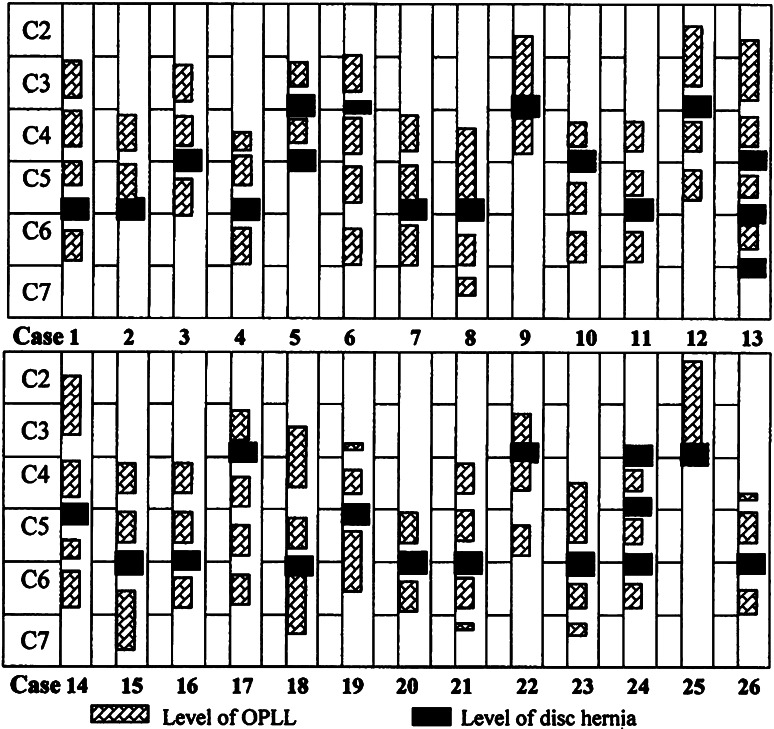
The mean diameter of the spinal canal on preoperative plain radiographs was 14.7 ± 1.2 mm (range 12–16 mm). Sagittal 3D CT scans of the cervical spine showed segmental-type OPLL in 15 patients (57.7%), mixed-type OPLL in nine patients (34.6%), and continuous-type OPLL in two patients (7.7%) (Fig. 1). Preoperative CT scans showed that the mean occupying rate reached 38.8 ± 9.3% (range 21–78%). On the sagittal images, OPLL extended from two to five vertebrae (mean 3.3 ± 0.9). No patient presented with Grade I spinal cord compression from OPLL, while Grade II was observed in eight patients and Grade III in 18 patients. Due to the large herniated discs, the greatest compression was observed at the disc levels and in Grade III. The herniated portions of the cervical discs were easily observed in axial scanograms and in sagittal T1-weighted MR images. A CDH protrusion at C5–C6 occurred in 15 patients (48.4%), at C3–C4 in eight patients (25.8%), at C4–C5 in seven patients (22.6%), and at C6/7 in one patient (3.2%) (Fig. 2).
Fig. 1.
Classification of OPLL associated with CDH. a segmental-type OPLL with CDH. b mixed-type OPLL with CDH. c, d continuous-type OPLL with CDH
Fig. 2.
Illustrations showing the levels of OPLL in the cervical spine and the levels of disc hernias in 26 patients. Patients 9 and 25 were continuous-type OPLL. Segmental ossification less than 1/2 vertebra was not calculated, such as for patients 19, 21, 23, and 26
Surgical approach and outcomes
Eight patients underwent ACDF to remove the herniated discs and the ossified ligaments at the disc level, 13 patients underwent ACCF to remove the discs and the ossified ligaments, and five patients underwent ACDF to remove the disc hernias combined with one- or two-stage posterior laminectomy and fusion. All these cases were followed-up for a mean period of 18 months (range 12–36 months). In general, the neurological status was significantly improved. The mean JOA score increased from 9.3 ± 1.8 (range 5–12) prior to surgery to 14.2 ± 1.3 (range 11–16) points at the last follow-up (P < 0.01). The improvement rate (IR) of neurological function ranged from 22.2–87.5% (mean 63.2 ± 15.2%). The surgical outcome was excellent in ten patients (38.5%), good in 14 patients (53.9%), fair in one patient (3.8%), and poor in one patient (3.8%).
Complications
In our case series, complications included cerebrospinal fluid (CSF) leakage in one case and epidural hematoma in one case. CSF leakage occurred after a dural tear during the operation due to tight adhesion with the dura; however, there was no significant dural defect. If CSF leakage occurred after operation, the drainage tube was pulled out 12 h after operation and continuous pressure was applied to the wound. In our experience, CSF leakage usually stopped after 3–5 days conservative treatment of local pressure. The patient who experienced epidural hematoma recovered neurological function after an emergency operation. There was no neurological deficit due to the prompt evacuation of hematoma.
Case reports
Case 18
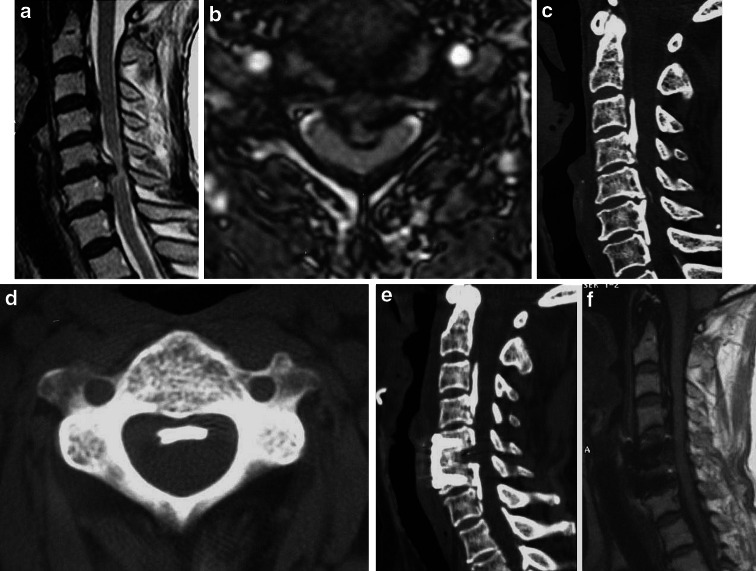
A 67-year-old woman complained of hand numbness and spastic weakness of the upper limb and hand for 2 months after a fall to the ground. There was only minor finger numbness prior to the fall. MRI showed a Grade II spinal cord compression attributable to OPLL, and the greatest compression was at C5/6 due to the disc hernia. Sagittal 3D CT showed a mixed-type OPLL from C3 to C7. The greatest occupying rate caused by OPLL was 26%. Anterior discectomy and fusion was performed and a normal spinal cord appearance was visible after surgery. The patient recovered from surgery without complications, and her symptoms improved dramatically. Her preoperative JOA score was 7, postoperative JOA score was 15, and IR was 80.0% (Fig. 3).
Fig. 3.
A 67-year-old patient with spinal cord compression mainly from C5/6 disc hernia but not from OPLL. a, b Sagittal and axial MRI scanograms of the cervical spine showing Grade II compression from OPLL, and the maximum compression at C5/6 disc level. c Sagittal 3D CT showing mixed-type OPLL from C3 to C7. d Axial scanogram showing a flat ossified ligament. e Sagittal 3D CT after ACDF and instrumentation showing an adequate decompression. f Sagittal MRI showing good spinal cord appearance after ACDF
Case 24
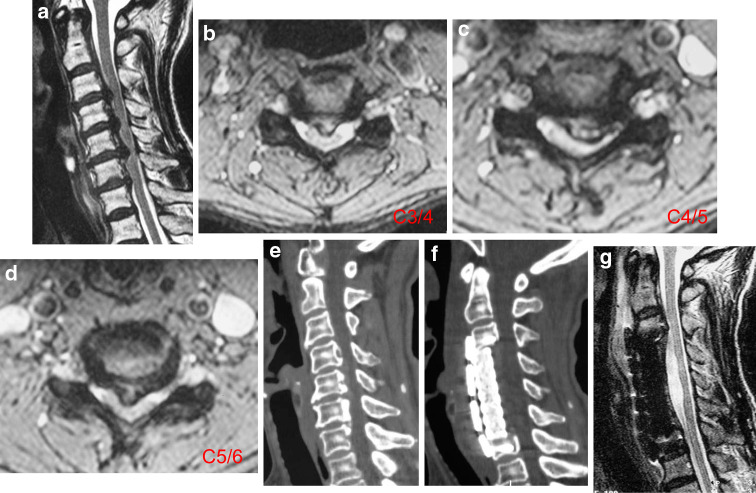
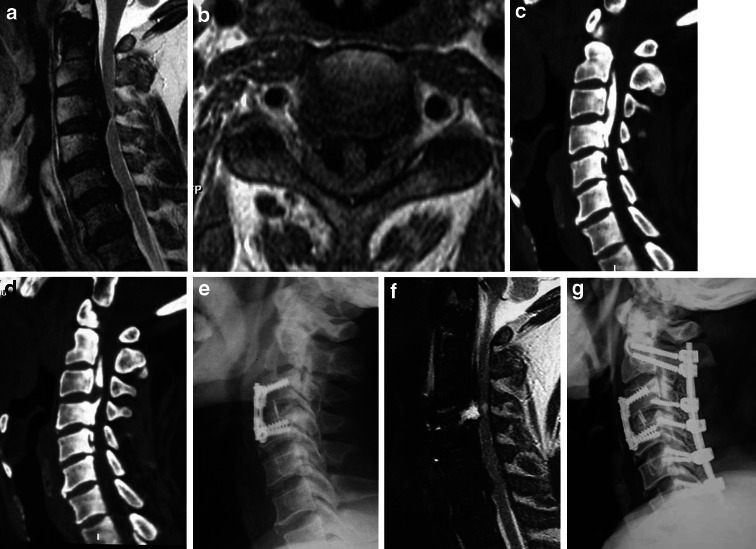
A 57-year-old woman complained of slight numbness and weakness in the limbs for 4 months. The symptoms had evidently aggravated in the last 2 months, and coincided with gait disturbance. There was no remote cause. Questioning revealed that she worked as a cleaner and often swept the floor for long hours. MRI of the cervical spine showed Grade III compression caused by OPLL. However, C3/4, C4/5, and C5/6 disc hernias were also visible, and compressed the spinal cord much more severely. Axial scanograms showed soft disc hernias compressing the cord at C3/4, C4/5, and C5/6. Sagittal 3D CT showed segmental-type OPLL from C4 to C6. The greatest occupying rate caused by OPLL was 31%. Anterior corpectomy with fusion was performed to remove the disc hernias and the ossified ligaments. Postoperative MRI showed a good spinal cord appearance. After the operation the patient showed marked recovery from the myelopathy with no complications. Her preoperative JOA score was 6, postoperative JOA score was 14, and IR reached 72.7% (Fig. 4).
Fig. 4.
A 57-year-old patient with spinal cord compression from disc hernia, and OPLL with no more than three segments and a 50% occupying rate. a Sagittal MRI of the cervical spine showing Grade III compression due to OPLL and the maximum compression at disc level. b–d Axial scanograms showing C3/4, C4/5, and C5/6 disc hernias. e Sagittal 3D CT showing segmental-type OPLL from C4 to C6. f, g Anterior corpectomy with fusion was performed and a good cord appearance was visible
Case 9
A 58-year-old man complained of numbness in his limbs associated with slight gait disturbance for 5 months. The limb weakness and gait disturbance were evidently aggravated, and bladder dysfunction appeared, after a violent neck massage in the last month. MRI showed maximum compression at C3/4 resulting from a disc hernia. Grade III compression from OPLL at C3–C4 was also observed. The occupying rate reached 78%. One-stage anterior discectomy was performed and the symptoms improved, although there was some residual numbness and gait disturbance. MRI showed satisfactory decompression at C3/4, while compression at C3 and C4 remained. We then performed a two-stage posterior laminectomy that resulted in further patient recovery. His preoperative JOA score was 6, two-stage postoperative JOA score was 11, and IR was 45.5% (Fig. 5).
Fig. 5.
Spinal cord compression from anterior CDH and OPLL with occupying rate more than 50%. a, b Sagittal and axial MRI scanogram showing compression from OPLL, particularly at the C3/4 disc level. c, d Sagittal 3D CT showing continuous-type OPLL from C2 to C4, but an unossified area in the middle part of the longitudinal ligament at C3/4. e One-stage ACDF was performed. f Compression from OPLL at C3 and C4 remained. g Two-stage posterior laminectomy was performed
Discussion
Coexistence of OPLL and CDH
It is well established that ossification of the posterior longitudinal ligament often coexists with cervical disc herniation. However, there only a few reports on the co-incidence of disc hernia and OPLL. In one study, approximately 32% of cases were accompanied by disc hernia for segmental-type OPLL, 6% for mixed-type OPLL, and 5% for continuous-type OPLL [6]. In another study, 79% of cases presented with cervical disc hernias in segmental-type OPLL, 33% of cases in mixed-type, and 17% of cases in continuous-type [4], while disc hernias were reported to be more frequent in segmental OPLL (81%) [7]. Kim et al. [8] also reported that 72 of 163 OPLL patients presented with cervical disc hernias (44.2%). Of note, those studies only assessed disc hernia using radiology, and only rarely combined with clinical features and intraoperative findings, which likely accounts for their high incidence rates. In contrast, a study by Ichimura et al. [9] reported only two cases of disc hernia in 107 OPLL patients. In the present study, we only counted patients with obvious cervical disc hernia as a major compression factor, resulting in our relatively low incidence rates.
It was previously reported that OPLL was observed less in patients with CDH, while CDH was common in patients presenting with OPLL [4, 10]. There is little difference in the incidence of CDH between Asian and non-Asian races, although OPLL occurs predominantly in Asian countries [1, 2]. These two phenomena imply that CDH may not be the causative factor for OPLL, although OPLL may initiate CDH. The predominant hypothesis is that pathologic changes such as hypertrophy, ossification, and laceration of the posterior longitudinal ligament invade the annulus fibrosus, which is firmly attached to the posterior longitudinal ligament, thus increasing the potential for disc hernia. In patients presenting OPLL, several cervical vertebral bodies were ‘fixed’ and moved as one vertebral body. However, the interruption of the ossified longitudinal ligament at the disc level and the fragility of the annulus fibrosus increase the risk of disc hernia, particularly in patients with a remote cause [11, 12].
Significance of MRI findings
Changes in cervical soft disc hernia cannot be detected by plain X-ray films, while normal CT scans do not reflect the exact degree of spinal cord compression or the location of the disc hernia. MRI is the preferred imaging modality due to its favorable soft tissue contrast. The sagittal T2-weighted MRI only poorly differentiated OPLL from disc hernias due to similarities in signal intensity, while disc hernias were clear on the axial scanograms. The quality of sagittal T1-weighted MRI was superior to that of T2-weighted imaging in the differentiation of these components. On T1-weighted MRI, disc hernia was revealed as an isointense or slightly high-intense lesion, whereas OPLL was observed as a hypointense lesion. An equivalent or slightly high-intense signal with the intervertebral disc on the dorsal side of ossification of the posterior longitudinal ligament can be seen on sagittal T1-weighted MR imaging and on axial scanogram [7, 13]. An obvious intraoperative herniated portion of cervical disc, which usually extended to the posterior of the longitudinal ligament, was observed in all cases exhibiting the aforementioned radiographic features.
Choice of surgical procedure
The three surgical procedures for patients of OPLL are anterior, posterior, and anterior combined with posterior. Anterior corpectomy and resection of OPLL is a radical surgical option due to direct decompression, and provides satisfactory results. It is a good indication for patients with less than 50% occupying rate and three ossified segments. Patients with an extensive OPLL affecting more than three levels or severe OPLL with an occupying rate more than 50% should be treated via a posterior laminectomy or laminoplasty, or potentially via an anterior combined with a posterior approach [14, 15]. In our case series, a herniated cervical disc was the most important compression factor. Furthermore, in some cases, the ossified ligament did not compress the spinal cord or initiate the patient’s clinical symptoms. The treatment for this kind of ossified ligament remains controversial. We decided that the herniated disc, not the ossified ligament, was the first and most important problem to address. In some patients, even ACDF only was performed, such as for case 18. The outcomes were favorable in all patients. In patients with CDH in combination with OPLL, the choice of surgical procedure for treatment of disc hernia is sometimes even more important than that for OPLL itself. Only the posterior approach is a relative contraindication in these patients because of the anterior herniated cervical disc, especially in patients with cervical kyphosis [14].
The progression of OPLL after posterior decompression and setting aside of the ossified ligament is a major concern in spinal surgery, although symptomatic recurrence of OPLL is rare [16], with the frequency of symptomatic progression of OPLL reported as less than 1%, while circumferential decompression, fixation, and fusion for OPLL may delay its progression [17–19].
CSF
There is currently no objective basis for discriminating preoperative adhesion between ligament and dura mater, whether by CT, MRI, or other modalities, and it remains difficult to identify cases with a potential risk for dural leakage. However, in our experience, the more severe the ossification the greater the risk of adhesion. An absolute adhesion usually exists in the most ossified site but at not all the ossified area. Thus, a large extent and a satisfactory separation between the OPLL and the dura mater is able to be performed with care. In another case series of 23 patients presenting with severe OPLL, an occupying rate greater than 50%, and who had received ACCF, there was absolute adhesion at the most ossified site in 15 patients (65.2%) and CSF in 14 patients (61.0%). In that study, a significant dural defect was not observed due to the careful separation and localized absolute adhesion.
In the cases where it was difficult to separate at the most ossified site, one of two possible surgical tactics was chosen. One was the floating method in which the OPLL was only separated from the vertebral wall, but remained attached to the dura mater. The entire ossified mass could be gradually floated anteriorly to eventually relieve spinal cord compression. However, the decompressive effect achieved using the floating method was limited, or occurred very slowly. Thus, in our patients the entire ossified mass including OPLL and the attached dura mater were removed completely if they could not be separated. This technique required operation with the aid of a microscope, and the arachnoid membrane was hoped to be preserved to avoid a large area of membrane defect and resulting uncontrolled CSF leakage. However, if arachnoid membrane damage occurred, it was difficult to patch or sew up due to the narrow surgical field and the limited area of membrane defect. Furthermore, although a cerebrospinal fluid pseudocyst was possible, in our experience the dural tear healed, and the pseudocyst gradually disappeared after 2 months of repeated aspiration, and CSF leakage can be cured using just conservative treatment [20–22].
Conclusion
Cervical disc hernia may be a relatively more important compression factor in patients presenting ossification of the posterior longitudinal ligament. Surgical procedure selection should be made by detailed study of clinical and radiological features, especially using 3D CT and MRI. Only the posterior approach is not advised in such patients, and follow-up should be performed for a longer period of time.
Contributor Information
Hai-song Yang, Email: yanghs.spine@yahoo.com.cn.
De-yu Chen, Phone: +86-21-81886806, FAX: +86-21-63520020, Email: chendyspine@yahoo.com.cn.
References
- 1.Lee T, Chacha PB, Khoo J. Ossification of posterior longitudinal ligament of the cervical spine in non-Japanese Asians. Surg Neurol. 1991;35:40–44. doi: 10.1016/0090-3019(91)90200-S. [DOI] [PubMed] [Google Scholar]
- 2.Kim T, Bae K, Uhm W, et al. Prevalence of ossification of the posterior longitudinal ligament of the cervical spine. Joint Bone Spine. 2007;75:47–474. doi: 10.1016/j.jbspin.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 3.Nakanishi T, Mannen T, Toyokura Y, et al. Symptomatic ossification of the posterior longitudinal ligament of the cervical spine: clinical findings. Neurology. 1974;24:1139–1143. doi: 10.1212/wnl.24.12.1139. [DOI] [PubMed] [Google Scholar]
- 4.Hanakita J, Suwa H, Namura S, et al. The significance of the cervical soft disc herniation in the ossification of the posterior longitudinal ligament. Spine. 1994;15:412–418. doi: 10.1097/00007632-199402001-00006. [DOI] [PubMed] [Google Scholar]
- 5.Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine. 1981;6:354–364. doi: 10.1097/00007632-198107000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Kokubu S, Sakurai M, Yawata J, et al. Results of anterior vs. posterior decompression for cervical myelopathy due to OPLL. Rinsho-Seikeigeka. 1988;23:543–553. [Google Scholar]
- 7.Koyanagi I, Iwasaki Y, Hida K, Imamura H, Abe H. Magnetic resonance imaging findings in ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg. 1998;88:247–254. doi: 10.3171/jns.1998.88.2.0247. [DOI] [PubMed] [Google Scholar]
- 8.Kim K, Isu T, Sugawara A, Matsumoto R, Isobe M. Anterior decompression via a wide transvertebral approach and a ceramic insert in a patient with cervical degenerative disease. Surg Neurol. 2007;67:127–134. doi: 10.1016/j.surneu.2006.06.059. [DOI] [PubMed] [Google Scholar]
- 9.Ichimura S, Hirabayashi K, Satomi K, et al. Results of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Rinsho-Seikeigeka. 1988;23:555–562. [Google Scholar]
- 10.Hanakita J, Suwa H, Namura S, et al. Cervical soft disc. Clinical analysis of 35 cases. Neurol Med Chir. 1988;28:1175–1180. doi: 10.2176/nmc.28.1175. [DOI] [PubMed] [Google Scholar]
- 11.Palacios E, Brackett CE, Leary D. Ossification of the posterior longitudinal ligament associated with a herniated intervertebral disc. Radiology. 1971;100:313–314. doi: 10.1148/100.2.313. [DOI] [PubMed] [Google Scholar]
- 12.Koyanagi I, Iwasaki Y, Hida K, et al. Acute cervical cord injury associated with ossification of the posterior longitudinal ligament. Neurosurgery. 2003;53:887–892. doi: 10.1227/01.NEU.0000083590.84053.CC. [DOI] [PubMed] [Google Scholar]
- 13.Kondo S, Onari K, Watanabe K, Hasegawa T, Toguchi A, Mihara H. Hypertrophy of the posterior longitudinal ligament is a prodromal condition to ossification: a cervical myelopathy case report. Spine. 2001;26:110–114. doi: 10.1097/00007632-200101010-00019. [DOI] [PubMed] [Google Scholar]
- 14.Mizuno J, Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6:282–288. doi: 10.1016/j.spinee.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: clinical results and limitations of laminoplasty. Spine. 2007;32:647–653. doi: 10.1097/01.brs.0000257560.91147.86. [DOI] [PubMed] [Google Scholar]
- 16.Tokuhashi Y, Ajiro Y, Umezawa N. A patient with two re-surgeries for delayed myelopathy due to progression of ossification of the posterior longitudinal ligaments after cervical laminoplasty. Spine. 2009;34:101–105. doi: 10.1097/BRS.0b013e31818a3135. [DOI] [PubMed] [Google Scholar]
- 17.Kato Y, Iwasaki M, Yonenobu K (1995) Long-term results of posterior decompressive surgery for cervical myelopathy due to OPLL. In: Terayama K (ed) Investigation committee report of 1995 on the ossification of the spinal ligaments. Japanese Ministry of Public Health and Welfare, Tokyo, pp 209–213 (in Japanese)
- 18.Onari K, Akiyama N, Kondo S, et al. Long-term follow-up results of anterior interbody fusion applied for cervical myelopathy due to ossification of the posterior longitudinal ligament. Spine. 2001;26:448–493. doi: 10.1097/00007632-200102150-00024. [DOI] [PubMed] [Google Scholar]
- 19.Choi S, Lee SH, Lee JY, et al. Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients. J Spinal Disord Tech. 2005;18:309–314. doi: 10.1097/01.bsd.0000161236.94894.fc. [DOI] [PubMed] [Google Scholar]
- 20.Chen Y, Guo Y, Chen D et al (2009) Diagnosis and surgery of ossification of posterior longitudinal ligament associated with dural ossification in the cervical spine. Eur Spine J 18(10):1541–1547 [DOI] [PMC free article] [PubMed]
- 21.Smith MD, Bolesta MJ, Leventhal M, et al. Postoperative cerebrospinal fluid fistula associated with erosion of the dura. Findings after anterior resection of ossification of the posterior longitudinal ligament in the cervical spine. J Bone Joint Surg. 1992;74:270–277. [PubMed] [Google Scholar]
- 22.Epstein NE, Hollingsworth R. Anterior cervical microdural repair of cerebrospinal fluid fistula after surgery for ossification of the posterior longitudinal ligament. Surg Neurol. 1999;52:511–514. doi: 10.1016/S0090-3019(99)00135-4. [DOI] [PubMed] [Google Scholar]