Abstract
Introduction:
Malignant gliomas are a heterogeneous group of primary central nervous system neoplasms that represent less than 2% of all cancers yet carry a significant burden to society. They are frequently associated with considerable and progressive neurological disability and are ultimately intractable to all forms of treatment. Temozolomide (TMZ) is a new second generation DNA alkylating agent that has become part of malignant astrocytoma management paradigms because of its proven efficacy, ease of administration, and favorable toxicity profile.
Aims:
To review the role of TMZ in the management of malignant astrocytomas (World Health Organization grades III and IV) including newly diagnosed (n) and recurrent (r) anaplastic astrocytomas (AA) and glioblastomas.
Evidence review:
A series of pivotal clinical trials have established a role for TMZ in the treatment of malignant astrocytomas. A large phase II trial examining the role of TMZ in rAA showed a response rate of 35%, and a 6-month progression-free survival of 46%. This led to the accelerated approval of TMZ by the FDA and the EU for the treatment of rAA. Evidence for a role of TMZ in nAA is currently limited but research is ongoing in this area. The role of TMZ in the management of glioblastoma at the time of recurrence (rGBM) is less impressive but evidence for its activity was demonstrated in two large phase II trials that led to the approval of TMZ for this indication in Europe and Canada but not in the US. A recent large prospective randomized phase III trial showed that the addition of TMZ during and after radiation therapy (RT) in newly diagnosed (nGBM) patients prolonged median overall survival by 2.5 months; perhaps more importantly, the 2-year survival rate for patients receiving TMZ and RT was 26% compared with 10% for those receiving RT alone. Concurrent TMZ with RT followed by adjuvant TMZ has become the standard of care for nGBM patients. Based on the evidence presented in this trial, TMZ received approval from the FDA and the EU for patients with nGBM in 2005.
Place in therapy:
There is evidence to support the use of TMZ for the following diseases in the order of most to least convincing: nGBM, rAA, rGBM, and nAA. This order may quickly change as more trials are being designed and implemented, particularly with novel TMZ dosing schedules.
Keywords: temozolomide, evidence, malignant astrocytoma, glioma, anaplastic astrocytoma, glioblastoma
Scope, aims, and objectives
In the US, temozolomide (TMZ; Temodar®, Temodal®, Schering-Plough Corporation) is indicated for recurrent anaplastic astrocytoma (rAA) and newly diagnosed glioblastoma (nGBM), and in Europe for nGBM, recurrent glioglastoma (rGBM), and rAA. This review summarizes the disease background, current therapy options, and unmet medical needs for patients with malignant gliomas, and outlines the current evidence for the role of TMZ in the management of malignant gliomas. Outcomes evaluated included objective radiographic response, progression-free survival at 6 months (PFS6m), median overall survival (mOS), 2-year survival, health-related quality of life (HRQoL), and the safety/tolerability profile of TMZ when used for the above indications.
Core evidence place in therapy summary for temozolomide (TMZ) in malignant astrocytomas
| Outcome measure | Evidence | Implications |
|---|---|---|
| Patient-oriented evidence | ||
| The addition of TMZ to standard RT followed by adjuvant TMZ increases the percentage of patients with PFS at 6 months (53.9% for TMZ/RT + TMZ vs 36.4% for RT alone, a 17.2% increase) | Clear | TMZ increases the percentage of progression-free nGBM patients |
| Concurrent TMZ/RT followed by adjuvant TMZ increases mOS by 2.5 months compared with RT alone in nGBM patients | Clear | TMZ results in improved survival among nGBM patients |
| Concurrent TMZ/RT followed by adjuvant TMZ increases 2-year survival from 10% to 24% for nGBM patients treated with RT alone | Clear | TMZ increases the odds of nGBM patients surviving to the 2-year time point |
| Concurrent TMZ/RT followed by adjuvant TMZ results in a 37% reduction in the risk of death for nGBM patients compared with RT alone | Clear | TMZ reduces the risk of death among nGBM patients |
| The HRQoL scores among nGBM patients treated with concurrent TMZ/RT followed by adjuvant TMZ were not inferior to the HRQoL scores derived from patients treated with RT alone | Clear | TMZ does not reduce the quality of life among nGBM patients |
| The PFS6m for rGBM patients treated with TMZ was 21% compared with a PFS6m of only 8% for patients treated with PCB, a 13% increase | Clear | TMZ improves the percentage of progression-free rGBM patients at 6 months compared with PCB |
| TMZ does not seem to improve survival among rGBM or rAA patients | Limited | TMZ does not improve survival when used for recurrent disease |
| TMZ treatment results in improved HRQoL scores when used for both rGBM and rAA patients | Clear | TMZ improves patient quality of life when used for recurrent disease |
| Disease-oriented evidence | ||
| nGBM patients treated with neoadjuvant TMZ achieve an ORR of 20% | Moderate | TMZ given prior to RT for nGBM patients results in radiographic improvement that usually correlates with clinical improvement |
| rGBM patients treated with TMZ did not achieve an improved ORR compared with other agents | Limited | TMZ given to rGBM patients does not result in a better radiographic response compared to other agents |
| TMZ possibly results in a higher ORR for rAA patients (35%) compared with only a 14% ORR for patients treated with other chemotherapeutic agents. Because of the differences in baseline patient characteristics for those two trials, no definitive conclusions can be drawn | Limited | TMZ may result in a more significant radiographic improvement when given to rAA patients compared with other agents |
| Economic evidence | ||
| TMZ is an expensive new agent but the added costs may be justified by the improved survival among nGBM patients | Limited | Despite the lack of conclusive cost-effectiveness data, TMZ should be considered especially from nGBM patients |
| The cost effectiveness of TMZ in recurrent disease is not clear at this point | Limited | One study concludes that TMZ may not be cost effective in recurrent disease compared with lomustine |
Abbreviations: HRQoL, health-related quality of life; mOS, median overall survival; nGBM, newly diagnose survival; glioblastoma; ORR, objective radiographic response; PCB, procarbazine; PFS, progression-free survival; PFS6m, progression-free survival at 6 months; rAA, recurrent anaplastic astrocytoma; rGBM, recurrent glioblastoma; rGBM, recurrent glioblastoma; RT, radiotherapy.
Methods
The English language medical literature was searched in the following databases.
Medline
EMBase
Cochrane reviews
The search terms used were temozolomide, glioblastoma, and anaplastic astrocytoma, and the records were limited to clinical trials, meta analyses, practice guidelines, and randomized controlled trials. The cutoff dates were from beginning through to March 25, 2008 (Table 1).
Table 1.
Evidence base included in the reviewa
| Category |
Number of records |
|---|---|
| Full papers | |
| Initial search | 96 |
| Records included | 58 |
| Records excluded | 38 |
| Search update | |
| Hand search of cross-references | 29 |
| Preclinical evidence | 9 |
| Level 1 evidence (systematic review, meta analysis) | 2 |
| Level 2 clinical evidence (RCT) | 9 |
| Level ≥ 3 clinical evidence | 45 |
| Trials other than RCT | 42 |
| Case reports | 5 |
| Economic evidence | 10 |
Notes:
Some references fall under multiple categories.
For definition of levels of evidence, see the Core Evidence website (http://www.dovepress.com/core-evidence-journal).
Abbrevation: RCT, randomized controlled trial.
Disease overview
Epidemiology
According to the Central Brain Tumor Registry of the US (CBTRUS) database, the number of reported cases of glioblastoma (GBM) between 1998–2002 was 12 943.1 The age-adjusted incidence of GBM was 3.05 [confidence interval (CI): 3.00, 3.10] and the median age at diagnosis was 64 years (CBTRUS 2006). The number of reported anaplastic astrocytoma (AA) cases during the same period was 2029 and the age-adjusted incidence was 0.47 (CI: 0.45, 0.49), with a median age at diagnosis for AA of 51 years.1
In the registry, GBM was the most common subtype of glioma and represented 20.3% of all malignant and nonmalignant brain tumors, and 50.7% of all glioma subtypes. In contrast, AA represented only 3.2% of all malignant and nonmalignant brain tumors, and 7.9% of all gliomas. The age-adjusted incidence rates for both GBM and AA were higher among males compared with females (3.86 per 100 000 person years in males versus 2.39 per 100 000 person years in females for GBM, and 0.56 per 100 000 person years among males versus 0.38 per 100 000 person years among females for AA). The incidence of both AA and GBM among white people was almost double the rate among black people.1
Risk factors and etiology
Familial, environmental, and genetic factors have been implicated in the development of astrocytomas. Most reported studies lack statistical power to identify unequivocally any single risk factor for the development of malignant gliomas.
Familial factors
Malignant astrocytomas are occasionally found at a higher frequency in families where several other malignancies are prevalent. Such familial cancer syndromes are due to germline mutations and include Li-Fraumeni syndrome, neurofibromatosis, Turcot syndrome, and multiple enchondromatosis.2 Interestingly, neurofibromatosis type-1 is due to a mutation on chromosome 17, which also harbors the p53 gene implicated in the genesis of many malignant gliomas.3
Environmental factors
Environmental factors that contribute to the development of malignant gliomas are notoriously difficult to ascertain with confidence. Because of the relatively low incidence of malignant gliomas, studies are able to establish a possible but inconclusive relationship between environmental exposures and the development of malignant gliomas. Ionizing radiation, however, has unequivocally been implicated in the genesis of secondary brain malignancies including AA and GBM after a minimallatency period of approximately 10 years.4,5 For instance, the routine use of prophylactic irradiation for leukemia has resulted in an increased risk of secondary gliomas in this patient population.6
On the other hand, there has been considerable debate as to whether high-energy electromagnetic radiation generated by the use of cellular phones contributes to the genesis of malignant gliomas. Results are conflicting but several studies have concluded that cellular telephones do not seem to be related causally to the development of malignant gliomas.8 Long-term follow up studies may still be needed however to settle this debate.
Genetic mutations
Gliomas are believed to arise as a result of a series of genetic aberrations that slowly accumulate over time.9 Theoretically, asthenumber of geneticmutationsincreases, tumors may progress from low-grade to higher grade phenotypes and genotypes. Molecular profiling has allowed the characterization of genetic mutations within brain tumor samples. GBMs can arise as a result of progression from low-grade astrocytomas, also known as secondary GBM, or de novo, also known as primary GBM. Primary (de novo) GBM represents approximately 80% of all GBMs. The genetic mutations within each of those entities may differ markedly. For example, mutation of the proapoptotic p53 gene located on chromosome 17 is believed to be the primary event involved in the genesis of a low-grade astrocytoma and is found with a higher incidence among secondary GBM tumor samples.3 Consequently, the mutated p53 gene is found with increasing frequency (>65%) in diffuse [World Health Organization (WHO) grade II] astrocytomas.10 This molecular derangement typically results in defective apoptosis and allows for uncontrolled cellular proliferation.11 In addition, overexpression of the platelet-derived growth factor receptor is found in over 60% of low-grade astrocytomas.11 The further sequential accumulation of genetic mutations in the form of loss of heterozygosity for chromosome 10q (LOH 10q), as well as mutation of the tumor suppressor retinoblastoma gene, has been observed in the progression of low-grade diffuse astrocytomas (WHO grade II) to AA (WHO grade III).12 Several genetic mutations are found in both GBM and AA or GBM arising from AA, but with variable frequency. For example, p53 mutation is far less frequent in primary GBM (∼25%) when compared with AA (∼50%) and secondary GBM (∼65%).13 Additionally, LOH 10q is found in only ∼8% of GBM that have evolved from AA, compared with ∼50% of primary GBM.14 The amplification of the epidermal growth factor receptor seems more important in primary GBM (∼36%) than in GBM that arises from an underlying AA (∼8%).11 These differences may aid in the diagnosis and prognosis of AA and GBM, and potentially identify targeted therapies to specific tumor subtypes based on genetic features.
Histologic subtypes
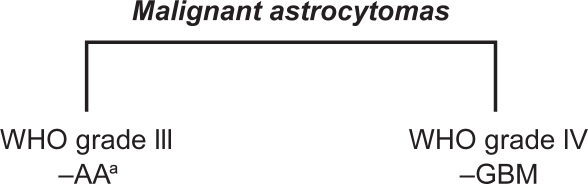
Astrocytomas are classified in ascending order of aggressiveness into WHO grades I–IV.15 Malignant astrocytomas fall under the more aggressive WHO grades III and IV and include AA (WHO grade III) and the most aggressive astrocytic neoplasm, GBM, which is classified as a grade IV tumor in the WHO grading scheme (Figure 1). GBM is also the most frequently encountered primary brain malignancy in the adult population.11,16
Figure 1.
WHO classification scheme for malignant astrocytomas.
Notes: aSome AAs containing oligodendroglial components are classified as anaplastic oligoastrocytomas (AOA).
Abbreviations: AA, anaplastic astrocytoma; GBM, glioblastoma multiforme; WHO, World Health Organization.
Goals of therapy
The goals of surgery for nGBM and nAA differ from those for recurrent disease. The goals of surgery for nGBM and nAA include providing tissue for an accurate pathologic diagnosis as well as tumor cytoreducation that can alleviate symptoms and reduce neurological deficits. For recurrent disease, the goal is usually tumor debulking alone. Whenever surgical resection is possible, the goal is maximal feasible tumor reduction provided that this can be achieved safely. Postoperative radiotherapy (RT) and chemotherapy are given to treat any residual disease and achieve a durable remission.
Despite multimodality treatment, patients with malignant gliomas invariably relapse, and at this time treatment goals are palliative in nature to the extent that therapeutic efforts are focused on delaying further tumor progression and preserving quality of life.
Evaluating response to therapy
In the earlier phase I and II trials evaluating the safety and efficacy of TMZ, an objective radiographic response was often used as a primary endpoint.17,18 Recently, PFS6m has been utilized as a new primary outcome measure in neurooncology because objective radiographic responses are uncommon in trials of new agents for recurrent malignant glioma, and because disease stabilization (radiographic or clinical) has been perceived as a valuable and treatment-specific outcome. The use of mOS and HRQoL have also been implemented as useful and informative secondary outcomes. To this extent, quality-adjusted life-year (QALY) is an emerging indicator incorporating both quantity and quality of life as a single parameter.19,20 In economic analyses, the cost of QALYs gained by administering a drug is an important measure of the cost effectiveness of the drug and may play an important role in drug reimbursement decisions. QALY is calculated by the duration spent in a health state (in years) weighted by the preference to that state (utility).
The following discussion defines the parameters employed as endpoints in the trials evaluating TMZ activity in malignant astrocytomas.
Objective radiographic response
One of the most widely adopted measures of tumor response is the objective radiographic response (ORR) according to the criteria proposed by MacDonald et al.21 Imaging modalities include contrasted computerized tomography (CT) scans of the brain or gadolinium-enhanced magnetic resonance (MR) scans, and these scans are obtained at various time points following treatment. In this scale, the two largest perpendicular diameters of the enhancing mass are multiplied and the product is then used as a baseline measure of the “tumor size.” Four response categories are identified on contrast-enhanced CT or MR scans.
Partial response (PR): a 50% decrease in tumor size compared to a prior scan at least 1 month apart, on a stable (>2 weeks) dose of steroids, and neurologically stable or improving.
Complete response (CR): the complete disappearance of the contrast-enhancing mass.
Progressive disease: an increase in tumor size >25% compared to a prior scan at least 1 month apart, on a stable (>2 weeks) dose of steroids, and neurologic worsening.
Stable disease: all other response categories.
Some of the drawbacks associated with this technique include a relatively wide interobserver variability of the measurements (hence the importance of a central radiology review of all scans assessed in a clinical trial), the occasional presence of multifocal disease that can be difficult to measure, variations associated with scanning techniques (such as dose of contrast medium), and variations in the timing of contrast injections relative to image acquisition. Furthermore, since tumors are three-dimensional masses, a bidimensional quantitative measure often fails to reflect the true size and dimensions of the tumor. In addition, some gliomas enhance heterogeneously and may contain nonenhancing areas that may not be included in the measurements, while conversely some contrast-enhancing areas may not represent tumor, but rather postsurgical changes or radiation effect. Despite these limitations, the ORR is a commonly employed endpoint used to assess efficacy of chemotherapeutic agents for the treatment of malignant astrocytomas.
Progression-free survival
PFS6m
PFS6m is defined as the percentage of patients who are alive and progression-free clinically and radiographically 6 months after the start of an intervention.
Median PFS
The median PFS is the median survival for a group of patients who remain progression-free after the initiation of an intervention.
Overall survival
mOS
The mOS is defined as the median time from start of treatment to death among a group of trial patients.
2-year survival
The 2-year survival is defined as the percentage of patients alive 2 years after the beginning of an intervention.
HRQoL
HRQoL is assessed using validated quality of life instruments such as the European Organisation for the Research and Treatment of Cancer (EORTC) quality of life questionnaires Core-30 and the EORTC brain cancer module (BN-20).22,23 The seven domains commonly utilized for the assessment of quality of life changes in trials involving brain tumor patients include global HRQoL and physical role, cognitive, emotional, and social functioning. A >10 point change on a 0–100 point scale is considered significant in the determination of changes in HRQoL status.24,25 Commonly, quality of life improvements correlate with radiographic response, and deterioration in quality of life correlates with radiographic progression. A drug that is capable of delaying time to tumor progression may therefore favorably impact quality of life in a clinically meaningful way, even if it fails to prolong overall survival.26
Current treatment options
nGBM and nAA
Patients with nGBM are treated with the three common modalities available for the treatment of all gliomas: surgery, RT, and chemotherapy. The first step in the management of gliomas is to obtain a pathologic diagnosis either through a stereotactic biopsy or open resection. Ideally, the surgeon attempts to perform a gross total resection of the tumor with the exception of deep-seated, inaccessible tumors, and tumors located in eloquent brain regions where resection may result in significant neurologic compromise. Postoperatively, involved field radiation is given to the enhancing region plus a 2–3 cm margin. RT is typically given in fractions of 2 Gy each for 6 weeks (60 Gy total).27 Postoperative RT and chemotherapy are given to treat residual disease that is invariably present following surgery.28
For patients with nAA, the current standard treatment options include maximal feasible surgical resection followed by involved field, conformal RT similar to the dose schedule prescribed for nGBM (60 Gy in 30 fractions of 2 Gy each). Although there is scant evidence to support a role for adjuvant chemotherapy in the management of AA, many neurooncologists frequently prescribe adjuvant chemotherapy for patients with this disease.
rGBM and rAA
Patients with GBM invariably exhibit disease recurrence, even among those with a complete response following successful treatment. At the time of disease recurrence, patients are commonly prescribed second-line chemotherapy agents, most often a nitrosourea.29 Other chemotherapeutic agents utilized in the salvage setting include nitrosoureas, etoposide, cyclophosphamide, and platinum compounds.30–32
A second craniotomy with tumor resection is typically reserved for reasonably well patients with tumors that have caused worsening neurologic deficits or a rise in intracranial pressure.33 Repeat irradiation is also a treatment option at the time of relapse but this is seldom prescribed because of the markedly increased risk of radionecrosis and leukoencephalopathy associated with repeat irradiation.34,35 Some of the newer RT techniques such as intensity-modulated radiation therapy and radiosurgery may minimize such risks but these remain experimental approaches for recurrent gliomas.36
Unmet needs
Malignant astrocytomas have long been considered amongst the most resistant cancers to therapeutic intervention. Despite advances in surgical and RT techniques over the last few decades, these therapies have had minimal impact on survival statistics. Attempts to improve survival with the addition of adjuvant chemotherapy have generally been disappointing, and numerous large phase III trials examining this matter have failed to show a survival advantage for chemotherapy-treated patients.37–40 Despite these generally negative results, a systematic meta analysis of 12 randomized trials demonstrated a small, but statistically significant, survival advantage for patients treated with adjuvant chemotherapy (a 5% increase in 2-year survival from 15% to 20%).41
Clinical evidence with TMZ
TMZ is an orally active alkylating agent that has shown activity in the treatment of malignant gliomas. Unlike many other chemotherapeutic agents, it readily crosses the blood-brain barrier and has a well tolerated safety profile. Until recently, the nitrosoureas were the first-line agents used for the treatment of malignant gliomas despite their minimal efficacy and significant toxicity. TMZ on the other hand has now become the first-line agent particularly for the treatment of GBM because of its proven benefit and good safety profile.
TMZ pharmacology
TMZ is a second generation imidazotetrazinone derivative. It undergoes a series of spontaneous reactions under physiologic conditions beginning with its hydrolysis into its active metabolite 5-(3-methyl-1-triazen-1-yl) imidazole-4-carboxamide, which further undergoes degradation into a methyldiazonium ion. This ion is the active compound that transfers a methyl group to DNA and thus affects the cytotoxic activity of TMZ. Although the final degradation product, 4-amino-5-imidazole-carboxamide is eliminated through the kidney, no TMZ dose adjustments are usually required for patients with impaired renal function.42
TMZ exerts its cytotoxic action via DNA methylation at the N-7 and O-6 positions of guanine, and the O-3 position of adenine. Although methylation of the O-6 position of guanine represents only a small fraction of the total DNA lesions induced by TMZ, it remains the major effector of its cytotoxic action. Methylation of guanine at the O-6 position results in “mismatch” incorporation of thymidine instead of cytosine.
This error is recognized by the mismatch repair (MMR) enzyme system that attempts to excise thymidine. Since guanine methylation persists, a series of futile replication and repair cycles ensue, ultimately resulting in apoptotic cell death. In the presence of the DNA repair enzyme O-6-methlguanine-DNA methyltransferase (MGMT, a DNA repair enzyme that removes methyl adducts at the O-6 position of guanine added by TMZ),43 the methylation of guanine can be repaired thereby allowing the cells to escape TMZ-induced cell death. Therefore, for TMZ to exert its cytotoxic action, a cell needs an intact MMR system and deficient or low MGMT enzyme levels. Conversely, a deficient MMR system coupled with high MGMT expression levels may mediate TMZ resistance.44,45
TMZ toxicity profile
Drug-related toxicities are typically graded according to the National Cancer Institute Common Toxicity Criteria (NCI-CTC) version 3.0.46 The most common toxic side effects associated with TMZ are nausea, vomiting, fatigue, and hematologic toxicity. According to the NCI-CTC, toxic side effects are graded on a scale of 1–5. Tables 2 and 3 summarize the various grades of severity of some of the more common side effects associated with TMZ.
Table 2.
Nonhematologic toxicities associated with TMZ
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | |
|---|---|---|---|---|---|
| Nausea | Loss of appetite without alteration in eating habits | Decreased oral intake without weight loss, dehydration or malnutrition; IV fluids indicated<24 hrs | Inadequate oral fluids or caloric intake: IV fluids, tube feeds or TPN required >24 hrs | Life-threatening consequences | Death |
| Vomiting | 1 episode in 24 hrs | 2–5 episodes in 24 hrs, IV fluids required <24 hrs | >6 episodes in 24 hrs, IV fluids or TPN required >24 hrs | Life-threatening complications | Death |
| Fatigue | Mild fatigue over baseline | Moderate fatigue causing difficulty with performing ADL | Severe fatigue interfering with ADL | Disabling fatigue |
Abbreviations: ADL, activities of daily living; IV, intravenous; TPN, total parenteral nutrition.
Table 3.
Hematologic toxicities associated with TMZ
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | |
|---|---|---|---|---|---|
| Leucocyte count (109/L) | <LLN-3 | <3.0–2.0 | <2.0–1.0 | <1.0 | Death |
| Lymphocyte count (109/L) | <LLN-0.8 | <0.8–0.5 | <0.5–0.2 | <0.2 | Death |
| Neutrophils(109/L) | <LLN-1.5 | <1.5–1.0 | <1.0–0.5 | <0.5 | Death |
| Hemoglobin (g/dL) | <LLN-10 | <10–8 | <8–6.5 | <6.5 | Death |
| Platelets (109/L) | <LLN-75 | <75–50 | <50–25 | <25 | Death |
Notes: <LLN, less than lower limit of normal.
There are single case reports describing instances of severe toxic side effects associated with TMZ treatment. One report describes the development of listeria, brain abscess, pneumocystis pneumonia, and Kaposi’s sarcoma in a GBM patient treated with TMZ.47 Another report describes the development of organizing pneumonitis associated with temozolomide.48
Objective radiographic response
nGBM and nAA
TMZ has been assessed in several clinical trials for the treatment of nGBM as a single agent. Response rates varied depending on the dosing schedule utilized in these trials.
A phase II multicenter study examined the role of neoadjuvant TMZ (prior to RT) for the treatment of nGBM and nAA patients. In this trial, a total of 187 patients received two cycles of TMZ at 200 mg/m2/day for 5 consecutive days every 28 days, and the objective response rate was determined using the bidimensional criteria on pre and postchemotherapy enhanced scans. A total of 162 patients were evaluable for response, and the ORR was 20% (95% CI 14, 26).49
A nonrandomized open-label phase II study evaluated the role of TMZ in combination with the antiangiogenic agent thalidomide for the treatment of nGBM. A total of 44 patients were treated with surgery followed by RT, and subsequently 19 patients (43%) received thalidomide alone and 25 (57%) received thalidomide with TMZ. Only two patients (8%) in the combined thalidomide/ TMZ group achieved an ORR.50
A phase I trial assessed the safety and efficacy of combining TMZ with procarbazine (PCB) for the treatment of glioma patients. This trial enrolled 16 nGBM, seven nAA, and five low-grade glioma patients. Although this trial was designed to evaluate the safety of the TMZ/PCB combination, a 36% ORR was observed.51
Neoadjuvant TMZ in combination with carmustine was evaluated for the treatment of analplastic gliomas in a phase II trial. A total of 41 patients received four cycles of neoadjuvant TMZ and carmustine prior to RT. Histology included nAA (81%), newly diagnosed anaplastic oligodendroglioma (12%), and mixed tumors (7%). The ORR was 29%, with a 2% CR and a 27% PR.52 Despite a reasonable response rate, this combination chemotherapy regimen was associated with considerable myelosuppression.
rGBM and rAA
Two pivotal trials have evaluated the response of patients with rGBM to TMZ treatment26,53 and one trial has evaluated rAA.54 The ORR to TMZ in rGBM in the two trials was 5% and 8%, respectively,26,53 which was similar to an ORR of 6% among rGBM patients treated with a variety of chemotherapeutic agents including nitrosoureas.55 The ORR with TMZ among rAA patients, however, was 35%,54 an outcome that compared favorably with a 14% ORR for patients treated with other chemotherapeutic agents.55 This trial served as the foundation for the approval of TMZ in 1999 in Europe and the US for the treatment of rAA. Although objective response rates in rGBM patients treated with TMZ were less impressive than data derived from rAA patients, a study by Yung and colleagues comparing efficacy of TMZ with PCB noted that the overall response (PR + stable disease) was higher among patients treated with TMZ [51/112 patients (45.6%) versus 37/113 (32.7%), P =0.049].26 The ORR (PR + CR) however was no different between the two groups, with six PR with both TMZ and PCB, and no CR with either agent.26
Progression-free survival
nGBM and nAA
TMZ has been shown to increase the percentage of progression-free patients with malignant gliomas at the 6-month time point following initiation of treatment. Several trials have evaluated the effect of TMZ on PFS6m either alone or in combination with other drugs for the treatment of nGBM and nAA,28,56 including a phase II trial that investigated the role of TMZ in combination with lomustine for the treatment of nGBM. Lomustine was administered at a dose of 110 mg/m2 (day 1) with TMZ 100 mg/m2/day (days 2–6) plus involved field RT to 31 patients with nGBM. The PFS6m for this group was 61.3%.56 The role of neoadjuvant TMZ was investigated in another phase II trial where TMZ was given after a biopsy was performed and prior to RT. The ORR to TMZ was therefore assessed without the confounding effects of surgery or radiotherapy.49
Several in-vitro studies suggested that TMZ may act as a radiosensitizer when administered concurrently with RT.57,58 In order to investigate whether TMZ administered during and after RT provides a clinical benefit compared with RT alone, a pilot phase II trial was conducted by Stupp et al.59 A total of 64 patients with nGBM from two institutions were randomized to receive TMZ 75 mg/m2/day for 42 consecutive days during RT (60 Gy in 30 fractions), followed by adjuvant TMZ 150–200 mg/m2/day for 5 consecutive days every 28 days. Patients received up to six cycles of adjuvant TMZ following concurrent treatment. Although this trial did not report PFS6m or median progression-free survival (mPFS), a mOS of 16 months, a 1-year survival of 58%, and a 2-year survival of 31 % were reported.59
A similar phase II trial examined the efficacy of TMZ in combination with RT followed by adjuvant TMZ.60 In this trial 130 patients (110 assessable) were randomly assigned to receive either TMZ 75 mg/m2/day with concurrent RT (60 Gy in 30 fractions; n =57) followed by six cycles of adjuvant TMZ 150 mg/m2/day on days 1–5 and days 15–19 every 28 days, or RT alone (60 Gy in 30 fractions; n =53). The administration of TMZ on days 15–19 of each adjuvant cycle represented a 50% increase in TMZ dose compared to the conventional regimen. The PFS6m observed in this trial was 67.1 % in the TMZ/RT group compared with 44.9% in the RT only group. The 1-year survival for patients treated with TMZ and RT was 56.3% (95% CI 44.12, 71.60), an outcome that was comparable to that observed in the trial conducted by Stupp et al.59
The encouraging phase II results using concurrent and adjuvant TMZ for the treatment of nGBM led to a definitive phase III trial conducted by EORTC and the National Cancer Institute of Canada Clinical Trials Group (NCIC CTG).28 In this large randomized international trial, 286 patients were assigned to receive RT alone and 287 patients were assigned to receive RT plus TMZ followed by adjuvant TMZ for a maximum of six cycles. RT consisted of 60 Gy administered in 30 fractions, and chemotherapy consisted of TMZ administered concurrently during RT at a dose of 75 mg/m2/day. The adjuvant TMZ regimen was 150 mg/m2/day for 5 days on cycle 1 and if tolerated, increased to 200 mg/m2/day for 5 days every 28 days on cycles 2 and thereafter. Patients receiving concurrent and adjuvant TMZ had a significantly better PFS6m (53.9%, CI 48.1, 59.6), compared with those receiving RT alone (36.4%, CI 30.8, 41.9).28
rGBM and rAA
Three pivotal phase II trials have established a role for TMZ in the treatment of patients with rGBM and rAA.26,53,54 These trials were the first to adopt PFS6m as a primary endpoint. Earlier trials utilizing the ORR as an endpoint may have underestimated clinical efficacy because clinical and quality of life benefits may be derived without radiographic evidence of tumor regression.17,18 The first two trials evaluated the efficacy of TMZ in rGBM and showed a PFS6m of 18%53 and 21% (versus 8% for PCB)26 respectively, and a corresponding ORR of only 8%53 and 5%.26 Since a PFS6m of >10% was deemed indicative of adequate drug activity,61,62 these trials demonstrated a positive role for TMZ in rGBM. TMZ was subsequently approved in Europe for the treatment of rGBM.
A third trial evaluating TMZ in rAA enrolled 162 patients and demonstrated an impressive PFS6m of 46%.54 The ORR among this group of rAA patients was 35%, results that compared favorably with an MD Anderson Cancer Center database of rAA patients who received various chemotherapeutic agents and had a PFS6m of only 31%.55 This led to the accelerated approval of TMZ in 1999 by the FDA and the European Medicines Agency (EMEA) for the treatment of rAA.
TMZ has also been investigated in combination with other chemotherapeutic and targeted agents in an attempt to improve its efficacy against malignant gliomas. A recent North American Brain Tumor Consortium phase II trial combined TMZ with the antiangiogenic agent thalidomide for rGBM patients.63 This trial enrolled 44 rGBM patients (43 patients were evaluable) for clinical efficacy and safety of TMZ. Eligible patients had rGBM after standard surgical resection and RT, and 82% of patients were chemotherapy-naïve at the time of relapse. TMZ was given in the standard 5-day cycle (150–200 mg/m2/day on days 1–5 every 28 days) and thalidomide 400 mg was given orally on days 1–28, and escalated to 1200 mg if tolerated. This trial demonstrated a PFS6m of 24%, suggesting that the combination was not superior to single agent TMZ when used for the treatment of rGBM.63
MGMT has been implicated as one of the mechanisms of tumor resistance to alkalytator and methylator chemotherapies.44,45 Depletion of MGMT has been demonstrated in vitro by cisplatin and continuous TMZ administration.64 TMZ in combination with cisplatin was therefore evaluated for the treatment of rGBM patients.65 In this phase II study, 50 patients with rGBM (49 patients were assessable) were given TMZ 130 mg/m2 bolus on day 1, followed by 70 mg/m2 every 12 hours on days 2–5, repeated every 4 weeks. Cisplatin was given in a dose of 75 mg/m2 on day 1 only of each 4-week cycle. The dose of TMZ was escalated to a cumulative maximum of 1000 mg/m2 over 5 days in the absence of hematologic toxicity. This regimen resulted in a PFS6m of 34% (95% CI 23, 50) and a median PFS of 18.4 weeks, and was associated with an acceptable toxicity profile.65
Another phase II trial evaluated a TMZ and cisplatin combination regimen in rGBM and rAA patients.66 Thirty-three patients (20 rGBM and 13 rAA patients) were treated with cisplatin 40 mg/m2 intravenously on days 1 and 2 plus TMZ 200 mg/m2/day on days 2–6 (24 hours after first cisplatin dose), and cycles were repeated every 4 weeks. This regimen resulted in a 52% PFS6m and a mPFS of 33 weeks (29.3 weeks for GBM and 39.5 weeks for AA). However, the higher PFS6m and mPFS demonstrated in this trial is likely due to the proportion of rAA patients included.66
Liposomal doxorubicin has demonstrable activity in a variety of malignancies,67 and its combination with TMZ was recently explored for the treatment of rGBM.68 In this phase II trial, 22 patients with rGBM were given liposomal doxorubicin 40 mg/m2 on day 1 with TMZ 200 mg/m2/day on days 1–5 administered in 4-week cycles. This regimen produced a PFS6m of 32% and an mPFS of 3.2 months.68
The matrix metalloproteinase inhibitor marimastat has also been investigated in combination with TMZ for the treatment of rGBM. Evidence derived from in-vitro data indicated that marimastat can inhibit glioma cell invasion, and for this reason its combination with TMZ is theoretically appealing.69 A total of 44 patients with rGBM received TMZ (200 mg/m2/day, days 1–5) and marimastat (50 mg/day, days 8–28) in a 28-day cycle for two cycles. The PFS6m in this group of patients was 39% and mPFS was 17 weeks. This study was complicated by a 47% incidence of joint and tendon pain that resulted in the removal of 11 % of patients from the study. The authors concluded that while the activity of this regimen appeared promising, further refinements were needed to minimize the toxic side effects.70
TMZ maintains activity in rGBM even at second recurrence. A small Italian study demonstrated a PFS6m of 24% when TMZ (standard 5-day regimen) was given to a group of 42 patients with rGBM at the time of second relapse.71 Although these patients were heavily pretreated with various chemotherapeutic agents, TMZ remained a viable therapeutic option for this group of patients.
Continuous daily dosing or “dose-dense” TMZ represents an attractive treatment approach based on in-vitro data demonstrating rapid MGMT enzyme depletion with continuous exposure to TMZ.72 A small Memorial Sloan-Kettering Cancer Center phase II trial evaluated continuous TMZ in recurrent malignant gliomas. This trial enrolled 35 patients (28 with rGBM, three with rAA, two with recurring anaplastic oligodendroglioma, and two with recurring anaplastic oligoastrocytomas) to receive TMZ 75 mg/m2/day for 42 days, in 70-day cycles. The PFS6m for the entire group was 27%, while PFS6m for the subgroup of GBM patients was 19%.73 Despite the acceptable PFS6m, the data failed to show superiority of this approach over the standard 5-day TMZ regimen.
Overall survival
nGBM and nAA
The definitive EORTC/NCIC phase III trial has demonstrated conclusively that TMZ can prolong mOS in nGBM patients by 2.5 months.28 These results confirm earlier phase II trials that demonstrated a survival advantage for TMZ in newly diagnosed malignant astrocytomas.56,60 TMZ given immediately in the postoperative setting and prior to neoadjuvant RT for nGBM and nAA patients resulted in a mOS of 10 months (16 months for responding patients versus only 3 months for nonresponders).49 Assessing TMZ efficacy in the neoadjuvant setting provides an advantage in that the benefit derived is not confounded by an RT effect or the effect of other chemotherapeutic agents.
The promising results obtained with neoadjuvant TMZ treatment led to further refinements of TMZ dosing schedules for the treatment of nGBM. A pilot phase II trial conducted by Stupp and colleagues59 assessed the novel approach of concurrent TMZ/RT followed by adjuvant TMZ given to 69 nGBM patients.59 The mOS reported in this study was 16 months. Another phase II trial compared TMZ + RT followed by adjuvant TMZ (150 mg/m2/day on days 1–5 and 15–19) with RT alone. The mOS reported for the TMZ/RT group was 13.4 versus 7.7 months for the RT group (P = 0.001).59 The phase II data reported by Stupp et al59 led to a definitive phase III trial conducted by the EORTC/NCIC in order to confirm the benefit of this novel regimen for the treatment of nGBM patients.28 As noted earlier, this trial enrolled 573 patients (286 patients in the RT arm and 287 patients in the TMZ/RT arm) most of whom were pathologically-proven GBM patients (93% in the RT arm and 92% in the TMZ/RT arm). At a median follow up of 28 months, 84% of the enrolled patients had died. For the patients who received concurrent and adjuvant TMZ, their unadjusted hazard ratio for death was 0.63 (95% CI 0.52, 0.75; P < 0.007 by the log-rank test), which translates into a 37% reduction in the risk of death for nGBM patients receiving concurrent and adjuvant TMZ, compared with those receiving RT alone. The mOS reported for the TMZ/RT group was 14.6 (95% CI 13.2, 16.8) versus 12.1 months (95% CI 11.2, 13.0) for RT alone, which translates into a 2.5-month increase in mOS for the TMZ/RT group compared with the RT only group. This was the first phase III trial to demonstrate a statistically significant and clinically meaningful survival advantage with the addition of chemotherapy to standard RT for nGBM patients.
Several other studies have used TMZ with other agents in an attempt to further improve the survival statistics. A phase II study enrolling 45 patients (38 with GBM and seven with AA) combined TMZ (150 mg/m2/day on days 1–5) with irinotecan (150 mg/m2/day on days 6 and 17) given every 4 weeks for a maximum of six cycles.74 Patients with GBM had a mOS of 12.8 months but this regimen was associated with a high rate of toxicity and failed to improve the survival statistics over TMZ alone for the treatment of nGBM and nAA patients.
Another phase II trial treated 31 patients with a combination of involved field RT (60 Gy in 30 fractions), lomustine (100 mg/m2 on day 1), and TMZ (100 mg/m2/day on days 2–6) every 4 weeks for up to six cycles. The reported mOS was 22.6 months and the regimen was associated with acceptable toxicity, indicating that further investigation of this approach may be warranted.56
rGBM and rAA
TMZ has established activity in the treatment of rGBM and rAA patients. Three pivotal phase II studies demonstrated radiographic response to TMZ in rGBM and rAA patients but failed to prolong mOS compared with historic databases of patients treated with other chemotherapeutic agents.26,53–55
The first study enrolled 138 rGBM patients and reported an mOS of 5.4 months.53 Patients treated with a variety of chemotherapeutic agents in a study conducted by Wong and colleagues55 had a similar mOS of 5.8 months. Another trial enrolled 225 rGBM patients randomized to PCB or TMZ. Patients receiving TMZ treatment had a mOS of 7.3 months compared with 5.8 months in those treated with PCB. This 1.5-month increase in mOS for TMZ-treated patients failed to reach statistical significance.26 A further trial examining the role of TMZ in rAA enrolled 162 patients and reported a mOS of 13.6 months.54 Data derived from the trial conducted by Wong and colleagues of patients receiving a variety of chemotherapeutic agents reported a mOS of 11 months among rAA patients.55 Despite the failure of TMZ to improve survival outcome, these trials nevertheless demonstrated improvements in the novel endpoint PFS6m as well as HRQoL, leading to the approval of TMZ for the treatment of rGBM and rAA patients.
Combining TMZ with other agents has also been investigated for the treatment of rGBM and rAA patients. For example, a small trial in 22 patients with rGBM reported a mOS of 8.2 months for the combination of doxorubicin with TMZ.68 Another study combining marimastat with TMZ reported a mOS of 45 weeks.70
To date, combining TMZ with other agents does not appear to confer an additional survival advantage over TMZ alone for the treatment of recurrent malignant astrocytomas. Table 4 summarizes the effect of TMZ on various trial endpoints when used for the treatment of malignant astrocytomas.
Table 4.
Evidence for TXZ efficacy in malignant astrocytomas
| nGBM/nAA | rGBM/rAA | Reference | |
|---|---|---|---|
| ORR | Neoadjuvant TMZ: 20% TMZ + TLD: 8% TMZ (GBM, AA and LGG): 36% |
Single agent TMZ for rGBM: 5% Single agent TMZ for rGBM: 8% Single agent TMZ for rAA: 35% rGBM: 6% rAA: 14% |
Brada et al;49 Yung et al26 Baumann et al;53 Brada et al50 Newlands et al;51 Yung et al54 Wong et al55 |
| PFS6m | TMZ/RT + adjuvant TMZ: 67.1 % RT alone: 44.9% TMZ/RT + adjuvant TMZ: 53.9% RT alone: 36.4% |
rGBM: 18% rGBM: 21 % vs 8% for PCB rAA: 46% rGBM: 15% rAA: 31 % |
Athanassiou et al60 Brada et al54 Yung et al26,54 Stupp et al28 Wong et al55 |
| mOS | nGBM/nAA (neoadjuvant TMZ): 10 mo nGBM (TMZ/RT + TMZ): 16 mo nGBM (TMZ/RT + TMZ): 13.4 mo RT alone: 7.7 mo |
rGBM: 5.4 mo rGBM: 7.3 mo vs 5.8 mo for PCB rAA: 13.6 mo |
Brada et al;49,50 Stupp et al58 2002; Yung et al;26 Athanasiou, et al;54 Yung et al108 Stupp et al28 |
| nGBM (TMZ/RT + TMZ): 14.6 mo RT alone: 12.1 mo |
rGBM: 5.8 mob rAA: 11 mob All patients: 7.0 mob |
Wong et al55 |
Notes:
Historic database of patients treated with multiple chemotherapeutic agents in a trial conducted by Wong and colleagues55 is used for comparison.
Data converted from weeks to months for ease of comparison using the formula (weeks × 7)/30 = months.
Abbreviations: Car, carmustine; Cis, cisplatin; GBM, glioblastoma; LGG, low grade glioma; mo, months; mOS, median overall survival; nAA, newly diagnosed anaplastic astrocytoma; nGBM, newly diagnosed GBM; ORR, objective radiographic response; PCB, procarbazine; PFS6m, progression-free survival at 6 mo; rGBM, recurrent GBM; rAA, recurrent anaplastic astrocytoma; RT, radiotherapy; TLD, thalidomide; TMZ, temozolomide.
HRQoL
The addition of TMZ to the standard treatment approaches of surgery and RT has been shown to impact positively on HRQoL among recurrent glioma patients. Two studies by Osoba and colleagues75,76 examined the effect of TMZ on HRQoL in patients with rAA and rGBM.
The first study calculated changes from baseline scores of seven HRQoL domains (role and social functioning, global quality of life, visual disorder, motor disorder, communication deficit, and drowsiness) in rAA patients treated with TMZ.76 These HRQoL domains were assessed every 4 weeks at each TMZ treatment cycle, and changes were compared to pretreatment (baseline) scores. This study demonstrated a significant improvement (defined as an increase ≥10 points from baseline scores) in all HRQoL domains following TMZ treatment. These improvements correlated with freedom from disease progression, and dropped sharply at the time of disease progression.76 Since TMZ is known to delay the time to tumor progression among recurrent glioma patients, this may in part explain the improvements in HRQoL scores seen with TMZ treatment.
A large phase II trial comparing the efficacy of TMZ with PCB in rGBM also included assessments of HRQoL scores. In this trial, 225 patients were randomly assigned to receive either TMZ (n =112) or PCB (n =113) at the time of first relapse.26 Patients receiving TMZ scored consistently higher on seven HRQoL domains, and this improvement was maintained until disease progression. Since TMZ was given on every 5 of 28 days while PCB was given daily for 28 days, the authors commented that the improvement in HRQoL may have been related to toxicity associated with daily PCB administration rather than to TMZ benefit. However, the study also demonstrated that TMZ delayed time to tumor progression compared with PCB, a parameter that closely correlates with maintenance or improvement in HRQoL.26 Whether or not TMZ directly impacts HRQoL parameters, its favorable toxicity profile compared with other chemotherapeutic agents likely plays a role in maintaining quality of life in a population that has to endure many potential adverse drug events.
Patients enrolled in a recent EORTC/NCIC phase III trial examining the role of concurrent TMZ/RT followed by adjuvant TMZ among nGBM patients were also assessed for changes in the predefined HRQoL measures at baseline and every 3 months following treatment until disease progression. Changes in HRQoL were calculated among patients receiving concurrent TMZ/RT followed by adjuvant TMZ and those receiving RT alone. HRQoL was a secondary endpoint for this study and was calculated based on the EORTC quality of life questionnaire Core-30 and the EORTC BN-20. The parameters used to measure HRQoL were fatigue, overall health, social function, emotional function, future uncertainty, insomnia, and communication deficit. Improvement in HRQoL was defined as an increase of ≥10 points compared with baseline. Overall, the study concluded that the addition of TMZ to RT did not impair the HRQoL measures compared with RT alone.77
Safety and tolerability
TMZ therapy has been consistently shown to be relatively safe and reasonably well tolerated in multiple trials for the treatment of malignant gliomas. The most commonly tested dosing schedule is a standard 5-day regimen of 150–200 mg/m2/day, which was developed in the early 1990s by Newlands and coworkers.78 In an early phase I trial, TMZ given as asingle bolus of 50 mg/m2, and subsequently escalated to 1200 mg/m2, resulted in no antitumor activity but was associated with myelosuppression as a major dose-limiting toxicity.51 The 5-day regimen was subsequently developed and given as a starting dose of 150 mg/m2/day for 5 days, in 28-day cycles and escalated to 200 mg/m2/day for 5 days on subsequent cycles if tolerated. This regimen was associated with clinical activity as opposed to the single TMZ dose and furthermore, 17% (two CR and two PR) of 23 patients demonstrated an ORR.51 The side effects associated with this regimen included nausea and vomiting that were controlled with 5HT3-antagonists. There was also little cumulative toxicity with this regimen and patients tolerated repeated cycles for up to 3 years.51
The first trial to examine the safety and tolerability of TMZ given concurrently and adjuvantly with RT was conducted by Stupp and colleagues in 2002. During the concomitant phase of treatment, grade lll or lV neutropenia or thrombocytopenia was observed in four patients (6%) each. Grade lll or lV lymphocytopenia was a very common side effect observed with this regimen, with 79% of patients suffering from this toxicity during the concurrent TMZ/RT phase of treatment. Three patients developed infections: two had Pneumocystis carinii pneumonia (PCP), and one developed osteomyelitis. Both patients with PCP had grade lll or lV neutropenia and lymphocytopenia at the time of the infection.58 Following the development of PCP in these two patients, pentamidine prophylaxis was introduced in the trial to be given to patients receiving concurrent treatment and no further PCP episodes were observed. During the adjuvant phase of treatment grade lll or lV neutropenia occurred in 2% of patients, while grade lll or lV thrombocytopenia occurred in 6% of patients. Only 2% of patients developed grade lll or lV anemia during adjuvant TMZ administration.
Nonhematologic toxicities during both phases of treatment were well tolerated and included nausea and vomiting (managed by standard antiemetics), moderate to severe fatigue, and rash resulting in discontinuation of treatment. One patient developed intracranial hypertension, refractory seizures, and loss of vision, all of which were considered delayed radiation-induced adverse events rather than side effects related to TMZ.
The EORTC/NCIC phase III trial enrolled the largest number of patients to date treated with TMZ.28 It therefore provided a large sample size for assessing safety and tolerability of TMZ in combination with RT and as a single agent in the adjuvant setting. There were no grade lll or lV hematologic toxic effects noted among those treated with RT alone. During the concurrent RT/TMZ treatment, 12 patients (4%) experienced grade lll or lV neutropenia while grade lll or lV thrombocytopenia occurred in nine patients (3%). Grade lll or lV hematologic toxicities were reported in 19 patients (7%) (Table 5).28
Table 5.
Grade 3 or 4 hematologic toxic effects [% (n)] in patients treated with temozolomide (adapted from Stupp et al28)
| Concomitant TMZ/RT (n = 284) | Adjuvant TMZ (n = 223) | Entire study perioda(n = 284) | |
|---|---|---|---|
| Leukopenia | 7 (2) | 11 (5) | 20 (7) |
| Neutropenia | 12 (4) | 9 (4) | 21 (7) |
| Thrombocytopenia | 9 (3) | 24 (11) | 33 (12) |
| Anemia | 1 (<1) | 2 (1) | 4 (1) |
| Any | 19 (7) | 32 (14) | 46 (16) |
Notes:
The entire study period is defined as the period from study entry to 7 days after disease progression.
Abbreviations: RT, radiotherapy; TMZ, temozolomide.
Overall, TMZ given concurrently with RT or as a single agent is well tolerated, with noncumulative myelotoxicity as the main dose-limiting side effect. Nonhematologic toxicities are usually well tolerated and include mild-to-moderate fatigue, constipation, nausea, and vomiting.
Prognostic factors
Prognostic determinants of survival for patients with malignant astrocytomas include tumor grade and histology (ie, GBM or AA), age, Karnofsky performance status (KPS), and MGMT promoter methylation status.79,80 The most important prognosticfactor and the one that most closely predicts mOS is tumor grade. Patients with GBM (WHO grade IV) fare worse than those with the lower grade AA (WHO grade III).1 Although GBM occurs on average among patients 10 years older than those with AA, age is likely to be an independent negative prognostic factor1 Among elderly patients (>75 years) with GBM, the 2-year survival is only 1.4% compared with 29.8% for patients aged between 20 and 44 years old.1 Patients with a lower performance status fare worse than those who are fully functional, and have a better KPS.
Several trials have evaluated the role of the extent of surgical resection in prolonging survival among malignant astrocytoma patients.81,82 Although some trials have shown that patients who have undergone gross total resection have better outcomes compared with those undergoing subtotal resection or biopsy only, these trials are fraught with confounding variables.83,84 For example, patients who underwent biopsy only were typically of older age and with worse KPS scores. In such instances, multivariate analysis revealed that the extent of surgery did not correlate with improved survival.85
Curran and colleagues86 have developed a recursive partitioning analysis (RPA) model of treatment and pretreatment-related prognostic variables for patients with malignant gliomas86,87(Table 6).
Table 6.
Original and adapted RTOG/EORTC RPA class III–V (adapted from Mirimanoff et al87)
| RPA class | RTOG (original) | EORTC |
|---|---|---|
| III age, years tumor type mental status performance status | <50 Anaplastic astrocytomas Abnormal | <50 Glioblastoma multiforme WHO PS 0 |
| Or age, years tumor type performance status | <50 Glioblastoma multiforme KPS 90–100 | |
| IV age, years tumor type performance status | <50 Glioblastoma multiforme KPS < 90 | <50 Glioblastoma multiforme WHO PS 1–2 |
| Or age, years tumor type performance status treatment mental status | ≥50 Anaplastic astrocytomas KPS 70–100 < 3 from time of first symptom to start of treatment | >50 Glioblastoma multiforme Complete/partial surgery MMSE ≥ 27 |
| Or age, years tumor type mental state treatment status | ≥50 Glioblastoma multiforme Good neurologic function Surgical resection | |
| V age, years tumor type performance status mental status treatment status | ≥50 Glioblastoma multiforme KPS 70–100 Neurologic function that inhibits the ability to work Surgical resection or biopsy only followed by at least 54.4 Gy radiotherapy | ≥50 Glioblastoma multiforme MMSE < 27 Biopsy only |
| Or age, years tumor type performance status mental status | ≥50 Glioblastoma multiforme KPS < 70 Normal |
Abbreviations: EORTC, European Organization for Research and Treatment of Cancer; KPS, Karnofsky performance status; MMSE, Mini Mental State Evaluation; RPA, recursive partitioning analysis; RTOG, Radiation Therapy Oncology Group; WHO PS, World Health Organization performance status.
The RPA model was applied to the 64 patients enrolled in the phase II trial comparing RT with RT/TMZ for nGBM patients.87 Median survival among these patients was 24 months for RPA class III, 14 months for RPA class IV, and 9 months for RPA class V, which compared favorably with a Radiation Therapy Oncology Group database.87 This was an incentive for conducting a larger phase III randomized trial that resulted in a new standard of care for the treatment of nGBM.28 The RPA methodology in this study was also used to evaluate the effect of adding TMZ to RT on median survival time. Among patients in the RPA class III receiving RT + TMZ, there was a gain of 7 months in median survival time and of 24% in the 2-year survival time (P =0.006). For this subset of patients, adding TMZ to RT resulted in a 43% probability of survival at 2 years.28 The addition of TMZ to RT still maintained its benefit among RPA class IV patients, more than doubling the 2-year survival rates compared with RT alone (P = 0.0001). The gain among the RPA class V patients was statistically insignificant (P =0.054), indicating that such patients with poor prognostic variables are least likely to benefit from addition of TMZ to RT (Table 7).28 However, this should not be taken as a reason to withhold TMZ treatment from RPA class V patients, since it is not known whether they derive benefits in other variables such as HRQoL.
Table 7.
Overall survival rates by RPA class (adapted from Stupp et al28)
| RPA class |
Median survival |
2-year survival |
||
|---|---|---|---|---|
| Months | 95% CI | % | 95% CI | |
| III | 17 | 15–21 | 32 | 21–2 |
| IV | 15 | 13–16 | 19 | 15–24 |
| V | 10 | 9–12 | 11 | 7–16 |
Abbreviation: RPA, recursive partitioning analysis.
Ongoing clinical development
Several trials are ongoing to evaluate the efficacy of 1 TMZ with various chemotherapeutic as well as targeted agents. For example, a phase I trial evaluating the safety and tolerability of adding everolimus (RAD001), an inhibitor of mammalian target of rapamycin (mTOR), to TMZ in nGBM patients is currently being conducted by the NCIC CTG.88
Continuous daily “dose-dense” TMZ is also currently under investigation for the treatment of recurrent malignant gliomas. Patients with recurrent malignant gliomas who have shown evidence of progression on the 5-day TMZ regimen are candidates for this trial. Patients receive TMZ at 75 mg/m2/day in 28-day cycles, and the cycles are repeated for up to a year if tolerated.89
In order to overcome MGMT-induced TMZ resistance, some trials have assessed the efficacy of combination regimens with TMZ and O-6-benzylguanine (an MGMT inhibitor).90,91 To date, these trials have failed to demonstrate improvements in outcome compared with TMZ alone but further investigations are ongoing.
Economic evidence
Because TMZ is associated with high acquisition costs, it is important to assess whether these additional costs are associated with measurable benefits. A report by Wasserfallen and colleagues92 showed that the addition of TMZ to RT for the treatment of nGBM patients was eight times more expensive than RT alone.92 Several reports therefore assessed the costs of TMZ per life-year and QALY gained, and whether such costs were below the acceptable threshold of $US50 000 per life-year gained as proposed by Prosser and colleagues.92 The decision whether or not to reimburse TMZ treatment by payors may be influenced by such economic analyses of cost-1 ratios, especially in systems with limited healthcare resources.
Data from a phase II trial evaluating the safety and efficacy of concurrent and adjuvant TMZ in nGBM.59 were collected, and associated costs retrospectively computed.92 The phase II trial enrolled 64 patients from two institutions, but only data related to 46 patients at one institution (University Center of Vaud, Lausanne, Switzerland) were analysed. Costs were computed for four separate periods: during concurrent TMZ and RT; during adjuvant TMZ; during the follow-up period and up to disease recurrence; and finally from disease recurrence until death.
This study showed that TMZ treatment had an average cost of €20 952 (eight times more expensive than RT alone). TMZ drug acquisition costs represented 54% of the total costs during the concurrent phase and 75% of the total costs during the adjuvant phase.93 Costs associated with the follow-up period (after completion of adjuvant TMZ) were largely attributable to hospitalizations as well as brain imaging studies, while those associated with disease recurrence were mainly due to palliative care hospitalizations and further chemotherapy treatments. This study also reported that the overall cost of care associated with TMZ use for nGBM patients treated in this trial ranged from €10 893 to €125 275, with a median of €34362, and that TMZ acquisition costs represented 55% of this sum. The median cost per month of survival was €2307 and the cost of TMZ per year of survival was €27 684. Interestingly, tumor MGMT promoter status and extent of surgery significantly affected the costs associated with TMZ treatment. Patients with tumors that had methylated MGMT promoter had a statistically significantly longer follow-up period before disease recurrence compared with patients with tumors that had unmethylated MGMT promoter (19.6 ± 17.7 versus 2.3 ± 1.7 months; P = 0.049). The costs incurred during this longer follow-up period were higher (€4793 ±3848 versus €636 ±633; P = 0.049), but the average monthly costs were similar. Patients who underwent surgical debulking also fared better than those who underwent biopsy only, and had longer adjuvant periods of TMZ treatment (144 ± 50 versus 80 ± 24 days, P = 0.032) and longer survival (10.9 ± 10.7 versus 4.1 ± 4.7 months, P =0.014). Interestingly, the total costs per month of survival for patients undergoing surgical debulking were lower than in those undergoing biopsy only because they required fewer hospitalizations despite the greater costs associated with TMZ use.92 This study was limited, however, by the small sample size and the retrospective nature of the analysis. Moreover, cost-effectiveness or cost-utility measures for TMZ in nGBM patients were not determined. Importantly, this study demonstrated that since concurrent and adjuvant TMZ was associated with a 4-month increase in median survival, the additional costs associated with this regimen would exceed the acceptable threshold of $US50 000 per life-year gained. The authors argued that this should not be a reason to withhold TMZ from a patient population with little or no other effective alternatives.
Another report by Wasserfallen and colleagues94 calculated the cost effectiveness and cost utility of TMZ use in patients with rGBM or rAA. The median cost effectiveness of TMZ in this patient population ranged between €28 817 and €38450. When these cost s were weighted by the individual mean health status (area under the Karnofsky curve), the cost utility ranged from €41167 to €53369 per QALY gained. This figure fell below the accepted $US50 000 threshold.94
A report commissioned by the Health Technology Assessment Programme on behalf of the National Institute for Health and Clinical Excellence (NICE) in England and Wales, reviewed the cost effectiveness of TMZ based on a literature review up to the year 200095 (prior to the completion of the EORTC/NCIC phase III trial). The report concluded that since TMZ resulted in gains in PFS but not in overall survival for patients with rGBM, the cost per QALY gained was approximately €40 000. Furthermore, this report concluded that until appropriate randomized controlled trials comparing TMZ with other alternative therapies were conducted, no firm conclusions about the cost effectiveness of TMZ should be drawn.97
However, the more recent EORTC/NCIC phase III trial clearly demonstrated that the addition of TMZ to RT conferred a survival advantage for newly diagnosed GBM patients versus those receiving RT alone. Based on this trial, concurrent and adjuvant TMZ became the standard of care for the treatment of nGBM despite its added costs. A study by Mabasa and Taylor evaluated mOS and compared the cost effectiveness of TMZ and lomustine in patients with recurrent malignant glioma.96 A retrospective review of medical records from 41 patients was conducted. Patients receiving TMZ (mean 5.1 cycles) incurred a mean cost of $Can10 746, while those receiving lomustine (mean 3.1 cycles) incurred a mean cost of $Can129. Lomustine is a relatively inexpensive chemotherapeutic agent that is given orally once every 6 weeks. TMZ, a newer and more expensive agent, is given in a 5 consecutive day regimen every 28 days. This may explain the higher costs associated with TMZ treatment. In addition, patients with recurrent disease are generally resistant to chemotherapy. Since TMZ has not been shown to provide a survival benefit in recurrent disease versus lomustine, the use of the more expensive TMZ may not be cost effective in this patient population. The incremental cost-effectiveness ratio for each life-year gained with TMZ ranged from $Can32 247 to $Can162186. Since the study found no difference in mOS achieved with the two drugs, the authors concluded that lomustine was more cost effective than TMZ for the treatment of recurrent malignant glioma.96
Another study from Finland evaluated the cost effectiveness of TMZ versus PCV (procarbazine, lomustine, vincristine) treatment for rGBM patients. This study concluded that 1 extra life-month gained with TMZ cost €2367, 1 extra progression-free life-month gained cost €2165, and the cost for each additional QALY gained was €32471 compared with PCV. The study also concluded that TMZ has a “high probability” of being cost effective compared with PCV for rGBM patients from a Finnish healthcare payer perspective.97 Another small Finnish study concluded that the high acquisition costs of TMZ are compensated by prolonged home care and possibly by the ability to retain working capacity during TMZ treatment among patients with recurrent gliomas.98 Despite the additional costs associated with TMZ use, the improved survival and HRQoL in patients with malignant gliomas may justify the added costs to society.
Patient group/population
Certain populations may differentially benefit from TMZ treatment. For example, patients with tumors harboring methylated MGMT promoter were found to have better outcomes compared with those with tumors that had unmethylated MGMT promoters.99 The benefit of TMZ for the elderly (age >70 years) is unknown.28
MGMT methylation status
MGMT effectively reverses the cytotoxic action of TMZ and thus high MGMT expression levels are associated with TMZ resistance. Patients with silenced MGMT gene expression due to hypermethylation of MGMT promoters were shown to respond more favorably to concurrent TMZ/RT compared with those who had unmethylated MGMT promoters and high MGMT gene expression levels.99 In this study, tumor samples obtained from nGBM patients enrolled in the EORTC/NCIC phase III study were analyzed for MGMT promoter methylation status by methylation-specific polymerase chain reaction techniques99 (Table 8).
Table 8.
Effect of MGMT promoter methylation status on PFS and OS among patients receiving concurrent temozolomide/radiotherapy versus radiotherapy alone (adapted from Hegi et al99)
| Clinical endpoint | TMZ + RT (n = 106) | RT (n = 100) |
|---|---|---|
| Methylated MGMT (n) | 46 | 46 |
| PFS6m (%) | 47.8 | 68.9 |
| 2-year OS (%) | 22.7 | 46.0 |
| Unmethylated MGMT (n) | 54 | 60 |
| PFS6m (%) | 35.2 | 40.0 |
| 2-year OS (%) | <2 | 13.8 |
Abbreviations: MGMT, O-6-methylguanine-DNA methyltransferase; OS, overall survival; PFS6m, progression-free survival at 6 months; RT, radiotherapy; TMZ, temozolomide.
Elderly patients
The treatment of elderly patients (≥70 years old) with newly diagnosed malignant gliomas remains controversial. The pivotal EORTC/NCIC phase III trial evaluating concurrent and adjuvant TMZ for nGBM excluded patients of this age.28 One study has compared an abbreviated course of radiation (3 weeks) to the standard 6-week schedule in elderly patients diagnosed with malignant gliomas. The trial concluded that the 3-week schedule was better tolerated and achieved similar results compared with the 6-week regimen.100 Another phase III trial compared RT with standard supportive care in elderly patients with AA and GBM, and concluded that RT was associated with superior outcomes.101 Because of these findings, some neurooncologists advocate an abbreviated 3-week course of RT for elderly patients with nGBM and nAA. It is not clear whether the addition of TMZ concurrently and/or adjuvantly to this shortened RT treatment would provide any additional advantage to this elderly population. A trial sponsored by the NCIC/CTG is currently exploring the benefit of adding TMZ to RT in patients aged >65 years.
Another phase III trial assessed the efficacy of TMZ alone instead of RT in a group of 32 elderly patients. TMZ treatment resulted in a PR rate of 31%, stable disease in a further 41 % of patients, while 28% had evidence of progressive disease. This cohort of patients achieved a mOS of 6.2 months (13.3 months among those achieving a PR), which compares favorably with median survival associated with RT alone.102 In addition, TMZ treatment was associated with a relatively mild and often predictable side effect profile, which makes it an attractive treatment option for this frail patient population.102 A further retrospective study comparing TMZ alone (150 mg/m2 for 5 days every 28 days) with RT alone in 86 elderly patients with newly diagnosed malignant glioma reported a higher median survival among those treated with TMZ alone, but the difference did not reach statistical significance (6.0 versus 4.1 months).103
Dosage, administration, and formulation
TMZ is used for the treatment of newly diagnosed as well as recurrent GBM and AA. Based on the EORTC/NCIC trial, TMZ is given concurrently with RT at 75 mg/m2 followed by a minimum of six cycles of adjuvant TMZ. Adjuvant TMZ is administered at 150 mg/m2 for 5 days on cycle 1 and 200 mg/m2 from cycle 2 onward provided blood counts are adequate. The cycles are repeated every 28 days.
The management approach for patients with rAA is very similar to rGBM.104 Based on a trial by Yung et al54 demonstrating an ORR rate of 35% to TMZ, this agent is frequently employed for the treatment of rAA.54
When treating recurrent disease, TMZ is administered daily for 5 days similar to the adjuvant regimen mentioned above. On the other hand, nAA is typically treated with surgical resection followed by conformal RT with or without concurrent TMZ. The addition of concurrent TMZ is of no proven value in the treatment of nAA because of the lack of a RCT showing superiority of this approach over RT alone.105 An international collaborative trial that will answer this question is underway.
TMZ is available in capsules of 5, 20, 100, and 250 mg. It achieves approximately 100% bioavailability after oral administration. In addition, TMZ achieves excellent blood-brain barrier penetration and the measured cerebrospinal fluid area under the curve (AUC) is typically 20%–40% of the plasma AUC.106
Place in therapy
Based on a number of trials, TMZ is quickly becoming a first-line agent for the treatment of malignant astrocytomas, both because of its proven efficacy as well as its safety profile. Concurrent TMZ and RT followed by adjuvant TMZ is currently the standard of care for nGBM. The role of TMZ for the management of nAA as well as for recurrent disease is less well defined at present but is widely used by neurooncologists for the first-line treatment of these disease entities.
In patients with rGBM, TMZ is associated with an increase of up to 6 months in PFS compared with PCB. Patients with rAA treated with a variety of chemotherapeutic agents achieved a PFS6m of 31%,55 while rAA patients treated with TMZ in a phase II trial achieved a PFS6m of 46%. The figures from these two trials are difficult to compare because of the differences in baseline patient characteristics. The worse outcome recorded in the trial conducted by Wong et al55 may be explained by the high proportion of patients with multiple recurrences and therefore with poorer prognoses.
Patients with rGBM and rAA had better HRQoL scores after treatment with TMZ. HRQoL was also not compromised in nGBM patients treated with concurrent TMZ and RT followed by adjuvant TMZ.
Concurrent TMZ with RT followed by adjuvant TMZ results in a 2.5-month prolongation of median survival among nGBM patients compared with patients receiving RT alone. More importantly, studies show that the probability of surviving to 2 years after diagnosis was only 1 in 10 for nGBM patients treated with RT alone, while patients treated with concurrent and adjuvant TMZ had a 1 in 4 chance of surviving to the 2-year time point.
Newly-diagnosed patients with a methylated MGMT promoter as well as those in RPA class III (age <50 years and PS of 0) seem to benefit the most from the addition of TMZ. Further studies are clearly needed to further refine the dosing schedules as well as identify ideal agents to be used in combination with TMZ in order to improve outcomes for patients with malignant glioma.
Acknowledgments
Drs Omar and Mason have acted as consultants and advisors for, and received honoraria from, Schering-Plough Corporation.
References
- 1.CBTRUS (Central Brain Tumor Registry of the US) 2005–2006. Primary Brain Tumors in the United States Statistical Report, 1998–2002 Years Data Collected. Available at: http://www.cbtrus.org/reports//2005-2006/2006report.pdf
- 2.Louis DN, von Deimling A. Hereditary tumor syndromes of the nervous system: overview and rare syndromes. Brain Pathol. 1995;5:145–151. doi: 10.1111/j.1750-3639.1995.tb00588.x. [DOI] [PubMed] [Google Scholar]
- 3.Konopka G, Bonni A. Signaling pathways regulating gliomagenesis. Curr Mol Med. 2003;3:73–84. doi: 10.2174/1566524033361609. [DOI] [PubMed] [Google Scholar]
- 4.Tamura M, Misumi S, Kurosaki S, Shibasaki T, Ohye C. Anaplastic astrocytoma 14 years after radiotherapy for pituitary adenoma. No Shinkei Geka. Neurological Surgery. 1992;20:493–497. (in Japanese). [PubMed] [Google Scholar]
- 5.Tsang RW, Laperriere NJ, Simpson WJ, et al. Glioma arising after radiation therapy for pituitary adenoma. A report of four patients and estimation of risk. Cancer. 1993;72:2227–2233. doi: 10.1002/1097-0142(19931001)72:7<2227::aid-cncr2820720727>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 6.Neglia JP, Robison LL, Stovall M. New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2006;98:1528–1537. doi: 10.1093/jnci/djj411. [DOI] [PubMed] [Google Scholar]
- 7.Hardell L, Mild KH, Carlberg M. Case-control study on the use of cellular and cordless phones and the risk for malignant brain tumours. Int J of Radiat Biol. 2002;78:931–936. doi: 10.1080/09553000210158038. [DOI] [PubMed] [Google Scholar]
- 8.Muscat JE, Hinsvark M, Malkin M. Mobile telephones and rates of brain cancer. Neuroepidemiology. 2006;27:55–56. doi: 10.1159/000094381. [DOI] [PubMed] [Google Scholar]
- 9.Kim S, Dougherty ER, Shmulevich I, et al. Identification of combination gene sets for glioma classification. Mol Cancer The. 2002;1:1229–1236. [PubMed] [Google Scholar]
- 10.Ohgaki H, Dessen P, Jourde B, et al. Genetic pathways to glioblastoma: a population-based study. Cancer Res. 2004;64:6892–6899. doi: 10.1158/0008-5472.CAN-04-1337. [DOI] [PubMed] [Google Scholar]
- 11.Ohgaki H, Kleihues P. Population-based studies on incidence, survival rates, and genetic alterations in astrocytic and oligodendroglial gliomas. J Neuropathol Exp Neurol. 2005;64:479–489. doi: 10.1093/jnen/64.6.479. [DOI] [PubMed] [Google Scholar]
- 12.Nozaki M, Tada M, Kobayashi H, et al. Roles of the functional loss of p53 and other genes in astrocytoma tumorigenesis and progression. Neuro Oncol. 1999;1:124–137. doi: 10.1093/neuonc/1.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarkar C, Ralte AM, Sharma MC, Mehta VS. Recurrent astrocytic tumours – a study of p53 immunoreactivity and malignant progression. Br J Neurosurg. 2002;16:335–342. doi: 10.1080/02688697021000007588. [DOI] [PubMed] [Google Scholar]
- 14.Wooten EC, Fults D, Duggirala R, et al. A study of loss of heterozygosity at 70 loci in anaplastic astrocytoma and glioblastoma multiforme with implications for tumor evolution. Neuro Oncol. 1999;1:169–176. doi: 10.1093/neuonc/1.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kleihues R, Louis DN, Scheithauer BW, et al. The WHO classification of tumors of the nervous system J Neuropathol Exp Neurol 200261215–225. discussion 226–229. [DOI] [PubMed] [Google Scholar]
- 16.Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Reilly SM, Newlands ES, Glaser MG, et al. Temozolomide: a new oral cytotoxic chemotherapeutic agent with promising activity against primary brain tumours. Eur J Cancer. 1993;29A:940–942. doi: 10.1016/s0959-8049(05)80198-4. [DOI] [PubMed] [Google Scholar]
- 18.Newlands ES, O’Reilly SM, Glaser MG, et al. The Charing Cross Hospital experience with temozolomide in patients with gliomas. Eur J Cancer. 1996;32A:2236–2241. doi: 10.1016/s0959-8049(96)00258-4. [DOI] [PubMed] [Google Scholar]
- 19.Weinstein MC, Stason WB. Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med. 1977;296:716–721. doi: 10.1056/NEJM197703312961304. [DOI] [PubMed] [Google Scholar]
- 20.Weinstein MC. A QALY is a QALY-or is it? J Health Econ. 1988;7:289–290. doi: 10.1016/0167-6296(88)90030-6. [DOI] [PubMed] [Google Scholar]
- 21.Macdonald DR, Cascino TL, Schold SC, Jr, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990;8:1277–1280. doi: 10.1200/JCO.1990.8.7.1277. [DOI] [PubMed] [Google Scholar]
- 22.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Nat Can Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 23.Osoba D, Aaronson NK, Muller M, et al. The development and psychometric validation of a brain cancer quality-of-life questionnaire for use in combination with general cancer-specific questionnaires. Qual Life Res. 1996;5:139–150. doi: 10.1007/BF00435979. [DOI] [PubMed] [Google Scholar]
- 24.King MT. The interpretation of scores from the EORTC quality of life questionnaire QLQ-C30. Qual Life Res. 1996;5:555–567. doi: 10.1007/BF00439229. [DOI] [PubMed] [Google Scholar]
- 25.Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16:139–144. doi: 10.1200/JCO.1998.16.1.139. [DOI] [PubMed] [Google Scholar]
- 26.Yung WK, Albright RE, Olson J, et al. A phase II study of temozolomide vs procarbazine in patients with glioblastoma multiforme at first relapse. Br J Cancer. 2000;83:588–593. doi: 10.1054/bjoc.2000.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stupp R, Hegi ME, van den Bent MJ, et al. Changing paradigms – an update on the multidisciplinary management of malignant glioma. Oncologist. 2006;11:165–180. doi: 10.1634/theoncologist.11-2-165. [DOI] [PubMed] [Google Scholar]
- 28.Stupp R, Mason WP, van den Bent MJ. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 29.Simpson L, Galanis E. Recurrent glioblastoma multiforme: advances in treatment and promising drug candidates. Expert Rev Anticancer Ther. 2006;6:1593–1607. doi: 10.1586/14737140.6.11.1593. [DOI] [PubMed] [Google Scholar]
- 30.Franceschi E, Cavallo G, Scopece L, et al. Phase II trial of carboplatin and etoposide for patients with recurrent high-grade glioma. Br J Cancer. 2004;91:1038–1044. doi: 10.1038/sj.bjc.6602105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rao RD, Krishnan S, Fitch TR, et al. Phase II trial of carmustine, cisplatin, and oral etoposide chemotherapy before radiotherapy for grade 3 astrocytoma (anaplastic astrocytoma): results of North Central Cancer Treatment Group trial 98-72-51. Int J Radiat Oncol Biol Phys. 2005;61:380–386. doi: 10.1016/j.ijrobp.2004.06.258. [DOI] [PubMed] [Google Scholar]
- 32.Chamberlain MC, Tsao-Wei DD, Groshen S. Salvage chemotherapy with cyclophosphamide for recurrent temozolomide-refractory anaplastic astrocytoma. Cancer. 2006;106:172–179. doi: 10.1002/cncr.21582. [DOI] [PubMed] [Google Scholar]
- 33.Guyotat J, Signorelli F, Frappaz D, Madarassy G, Ricci AC, Bret P. Is reoperation for recurrence of glioblastoma justified? Oncol Rep. 2000;7:899–904. doi: 10.3892/or.7.4.899. [DOI] [PubMed] [Google Scholar]
- 34.Bauman GS, Sneed PK, Wara WM, et al. Reirradiation of primary CNS tumors. Int J Radiat Oncol Biol Phys. 1996;36:433–441. doi: 10.1016/s0360-3016(96)00315-x. [DOI] [PubMed] [Google Scholar]
- 35.Veninga T, Langendijk HA, Slotman BJ, et al. Reirradiation of primary brain tumours: survival, clinical response and prognostic factors. Radiother Oncol. 2001;59:127–137. doi: 10.1016/s0167-8140(01)00299-7. [DOI] [PubMed] [Google Scholar]
- 36.Voynov G, Kaufman S, Hong T, Pinkerton A, Simon R, Dowsett R. Treatment of recurrent malignant gliomas with stereotactic intensity modulated radiation therapy. Am J Clin Oncol. 2002;25:606–611. doi: 10.1097/00000421-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 37.Walker MD, Green SB, Byar DP, et al. Randomized comparisons of radiotherapy and nitrosoureas for the treatment of malignant glioma after surgery. N Engl J Med. 1980;303:1323–1329. doi: 10.1056/NEJM198012043032303. [DOI] [PubMed] [Google Scholar]
- 38.Chang CH, Horton J, Schoenfeld D, et al. Comparison of postoperative radiotherapy and combined postoperative radiotherapy and chemotherapy in the multidisciplinary management of malignant gliomas. A joint Radiation Therapy Oncology Group and Eastern Cooperative Oncology Group study. Cancer. 1983;52:997–1007. doi: 10.1002/1097-0142(19830915)52:6<997::aid-cncr2820520612>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 39.Shapiro WR, Green SB, Burger PC, Mahaley MS, Jr, et al. Randomized trial of three chemotherapy regimens and two radiotherapy regimens in postoperative treatment of malignant glioma. Brain Tumor Cooperative Group Trial 8001. J Neurosurg. 1989;71:1–9. doi: 10.3171/jns.1989.71.1.0001. [DOI] [PubMed] [Google Scholar]
- 40.MRCBTWP (Medical Research Council Brain Tumor Working Party) Randomized trial of procarbazine, lomustine, and vincristine in the adjuvant treatment of high-grade astrocytoma: a Medical Research Council trial. J Clin Oncol. 2001;19:509–518. doi: 10.1200/JCO.2001.19.2.509. [DOI] [PubMed] [Google Scholar]
- 41.Stewart LA. Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet. 2002;359:1011–1018. doi: 10.1016/s0140-6736(02)08091-1. [DOI] [PubMed] [Google Scholar]
- 42.Denny BJ, Wheelhouse RT, Stevens MF, Tsang LL, Slack JA. NMR and molecular modeling investigation of the mechanism of activation of the antitumor drug temozolomide and its interaction with DNA. Biochemistry. 1994;33:9045–9051. doi: 10.1021/bi00197a003. [DOI] [PubMed] [Google Scholar]
- 43.Pearl LH, Savva R. DNA repair in three dimensions. Trends Biochem Sci. 1995;20:421–426. doi: 10.1016/s0968-0004(00)89092-1. [DOI] [PubMed] [Google Scholar]
- 44.Hotta T, Saito Y, Fujita H, et al. O6-alkylguanine-DNA alkyltransferase activity of human malignant glioma and its clinical implications. J Neurooncol. 1994;21:135–140. doi: 10.1007/BF01052897. [DOI] [PubMed] [Google Scholar]
- 45.Gerson SL. MGMT: its role in cancer aetiology and cancer therapeutics. Nature Reviews. Cancer. 2004;4:296–307. doi: 10.1038/nrc1319. [DOI] [PubMed] [Google Scholar]
- 46.NCI-CTC (National Cancer Institute Common Toxicity Criteria) Cancer Therapy Evaluation Program, Common Terminology Criteria for Adverse Events, (DCTD, NCI, NIH, DHHS). 2003http://ctep.cancer.gov/forms/CTCAEv3.pdf
- 47.Ganière V, Christen G, Bally F, et al. Listeria brain abscess, Pneumocystis pneumonia and Kaposi’s sarcoma after temozolomide. Nat Clin Pract Oncol. 2006;3:339–343. doi: 10.1038/ncponc0514. [DOI] [PubMed] [Google Scholar]
- 48.Maldonado F, Limper AH, Lim KG, Aubrey MC. Temozolomide-associated organizing pneumonitis. Mayo Clin Proc. 2007;82:771–773. [PubMed] [Google Scholar]
- 49.Brada M, Ashley S, Dowe A, et al. Neoadjuvant phase II multicentre study of new agents in patients with malignant glioma after minimal surgery. Report of a cohort of 187 patients treated with temozolomide. Ann Oncol. 2005;16:942–949. doi: 10.1093/annonc/mdi183. [DOI] [PubMed] [Google Scholar]
- 50.Baumann F, Bjeljac M, Kollias SS, Baumert BG, et al. Combined thalidomide and temozolomide treatment in patients with glioblastoma multiforme. J Neurooncol. 2004;67:191–200. doi: 10.1023/b:neon.0000021803.01170.03. [DOI] [PubMed] [Google Scholar]
- 51.Newlands ES, Foster T, Zaknoen S. Phase I study of temozolamide (TMZ) combined with procarbazine (PCB) in patients with gliomas. Br J Cancer. 2003;89:248–251. doi: 10.1038/sj.bjc.6601043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chang SM, Prados MD, Yung WK, et al. Phase II study of neoadjuvant 1, 3-bis (2-chloroethyl)-1-nitrosourea and temozolomide for newly diagnosed anaplastic glioma: a North American Brain Tumor Consortium Trial. Cancer. 2004;100:1712–1706. doi: 10.1002/cncr.20157. [DOI] [PubMed] [Google Scholar]
- 53.Brada M, Hoang-Xuan K, Rampling R. Multicenter phase II trial of temozolomide in patients with glioblastoma multiforme at first relapse. Ann Oncol. 2001;12:259–266. doi: 10.1023/a:1008382516636. [DOI] [PubMed] [Google Scholar]
- 54.Yung WK, Prados MD, Yaya-Tur R, et al. Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal Brain Tumor Group. J Clin Oncol. 1999;17:2762–2771. doi: 10.1200/JCO.1999.17.9.2762. [DOI] [PubMed] [Google Scholar]
- 55.Wong ET, Hess KR, Gleason MJ, et al. Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol. 1999;17:2572–2578. doi: 10.1200/JCO.1999.17.8.2572. [DOI] [PubMed] [Google Scholar]
- 56.Herrlinger U, Rieger J, Koch D, et al. Phase II trial of lomustine plus temozolomide chemotherapy in addition to radiotherapy in newly diagnosed glioblastoma: UKT-03. J Clin Oncol. 2006;24:4, 412–417. doi: 10.1200/JCO.2006.06.9104. [DOI] [PubMed] [Google Scholar]
- 57.Wedge SR, Porteous JK, Glaser MG, Marcus K, Newlands ES. In vitro evaluation of temozolomide combined with X-irradiation. Anticancer Drugs. 1997;8:92–97. doi: 10.1097/00001813-199701000-00013. [DOI] [PubMed] [Google Scholar]
- 58.van Rijn J, Heimans JJ, van den Berg J, van der Valk R, Slotman BJ. Survival of human glioma cells treated with various combination of temozolomide and X-rays. Int J Radiat Oncol Bio Phys. 2000;47:779–784. doi: 10.1016/s0360-3016(99)00539-8. [DOI] [PubMed] [Google Scholar]
- 59.Stupp R, Dietrich PY, Ostermann Kraljevic S, et al. Promising survival for patients with newly diagnosed glioblastoma multiforme treated with concomitant radiation plus temozolomide followed by adjuvant temozolomide. J Clin Oncol. 2002;20:1375–1382. doi: 10.1200/JCO.2002.20.5.1375. [DOI] [PubMed] [Google Scholar]
- 60.Athanassiou H, Synodinou M, Maragoudakis E, et al. Randomized phase II study of temozolomide and radiotherapy compared with radiotherapy alone in newly diagnosed glioblastoma multiforme. J Clin Oncol. 2005;23:2372–2377. doi: 10.1200/JCO.2005.00.331. [DOI] [PubMed] [Google Scholar]
- 61.Hosli P, Sappino AP, de Tribolet N, Dietrich PY. Malignant glioma: should chemotherapy be overthrown by experimental treatments? Ann Oncol. 1998;9:589–600. doi: 10.1023/a:1008267312782. [DOI] [PubMed] [Google Scholar]
- 62.Pech IV, Peterson K, Cairncross JG. Chemotherapy for brain tumors. Oncology (Williston Park) 1998;12:537–543. [PubMed] [Google Scholar]
- 63.Groves MD, Puduvalli VK, Chang SM, et al. A North American brain tumor consortium (NABTC 99–04) phase II trial of temozolomide plus thalidomide for recurrent glioblastoma multiforme. J Neurooncol. 2007;81:271–277. doi: 10.1007/s11060-006-9225-y. [DOI] [PubMed] [Google Scholar]
- 64.D’Atri S, Graziani G, Lacal PM, et al. Attenuation of O(6)-methylguanine-DNA methyltransferase activity and mRNA levels by cisplatin and temozolomide in jurkat cells. J Pharmacol Exp Ther. 2000;294:664–671. [PubMed] [Google Scholar]
- 65.Brandes AA, Basso U, Reni M, et al. First-line chemotherapy with cisplatin plus fractionated temozolomide in recurrent glioblastoma multiforme: a phase II study of the Gruppo Italiano Cooperativo di Neuro-Oncologia. J Clin Oncol. 2004;22:1598–1604. doi: 10.1200/JCO.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 66.Silvani A, Eoli M, Salmaggi A, et al. Phase II trial of cisplatin plus temozolomide, in recurrent and progressive malignant glioma patients. J Neurooncol. 2004;66:203–208. doi: 10.1023/b:neon.0000013479.64348.69. [DOI] [PubMed] [Google Scholar]
- 67.Awada A, Gil T, Sales F, et al. Prolonged schedule of temozolomide (Temodal) plus liposomal doxorubicin (Caelyx) in advanced solid cancers. Anticancer Drugs. 2004;15:499–502. doi: 10.1097/01.cad.0000127331.29310.8a. [DOI] [PubMed] [Google Scholar]
- 68.Chua SL, Rosenthal MA, Wong SS, et al. Phase 2 study of temozolomide and Caelyx in patients with recurrent glioblastoma multiforme. Neurooncol. 2004;6:38–43. doi: 10.1215/S1152851703000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tonn JC, Kerkau S, Hanke A, et al. Effect of synthetic matrix-metalloproteinase inhibitors on invasive capacity and proliferation of human malignant gliomas in vitro. IntJ Cancer. 1999;80:764–772. doi: 10.1002/(sici)1097-0215(19990301)80:5<764::aid-ijc22>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 70.Groves MD, Puduvalli VK, Hess KR, et al. Phase II trial of temozolomide plus the matrix metalloproteinase inhibitor, marimastat, in recurrent and progressive glioblastoma multiforme. J Clin Oncol. 2002;20:1383–1388. doi: 10.1200/JCO.2002.20.5.1383. [DOI] [PubMed] [Google Scholar]
- 71.Brandes AA, Ermani M, Basso U, et al. Temozolomide in patients with glioblastoma at second relapse after first line nitrosourea-procarbazine failure: a phase II study. Oncology. 2002;63:38–41. doi: 10.1159/000065718. [DOI] [PubMed] [Google Scholar]
- 72.Tolcher AW, Gerson SL, Denis L, et al. Marked inactivation of O6-alkylguanine-DNA alkyltransferase activity with protracted temozolomide schedules. Br J Cancer. 2003;88:1004–2011. doi: 10.1038/sj.bjc.6600827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Khan RB, Raizer JJ, Malkin MG, Bazylewicz KA, Abrey LE. A phase II study of extended low-dose temozolomide in recurrent malignant gliomas. Neurooncology. 2002;4:39–43. doi: 10.1215/15228517-4-1-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fountzilas G, Karkavelas G, Kalogera-Fountzila A, et al. Post-operative combined radiation and chemotherapy with temozolomide and irinotecan in patients with high-grade astrocytic tumors. A phase II study with biomarker evaluation. Anticancer Res. 2006;26:4675–4686. [PubMed] [Google Scholar]
- 75.Osoba D, Brada M, Yung WK, Prados M. Health-related quality of life in patients treated with temozolomide versus procarbazine for recurrent glioblastoma multiforme. J Clin Oncol. 2000a;18:1481–1491. doi: 10.1200/JCO.2000.18.7.1481. [DOI] [PubMed] [Google Scholar]
- 76.Osoba D, Brada M, Yung WK, Prados MD. Health-related quality of life in patients with anaplastic astrocytoma during treatment with temozolomide. Eur J Cancer. 2000b;36:1788–1795. doi: 10.1016/s0959-8049(00)00165-9. [DOI] [PubMed] [Google Scholar]
- 77.Hamilton DA. Adding concomitant and adjuvant temozolomide to radiotherapy does not reduce health-related quality of life in people with glioblastoma. Cancer Treat Rev. 2006;32:483–486. doi: 10.1016/j.ctrv.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 78.Newlands ES, Blackledge GR, Slack JA, et al. Phase I trial of temozolomide (CCRG 81045: M&B 39831: NSC 362856) Br J Cancer. 1992;65:287–291. doi: 10.1038/bjc.1992.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carson KA, Grossman SA, Fisher JD, Shaw EG. Prognostic factors for survival in adult patients with recurrent glioma enrolled onto the new approaches to brain tumor therapy CNS consortium phase I and II clinical trials. J Clin Oncol. 2007;25:2601–2606. doi: 10.1200/JCO.2006.08.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Compostella A, Tosoni A, Blatt V, Franceschi E, Brandes AA. Prognostic factors for anaplastic astrocytomas. J Neurooncol. 2007;81:295–303. doi: 10.1007/s11060-006-9232-z. [DOI] [PubMed] [Google Scholar]
- 81.Devaux BC, O’Fallon JR, Kelly PJ.Resection, biopsy, and survival in malignant glial neoplasms. A retrospective study of clinical parameters, therapy, and outcome J Neurosurg A993;78767–775. [DOI] [PubMed] [Google Scholar]
- 82.Laws ER, Parney IF, Huang W, et al. Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg. 2003;99:467–473. doi: 10.3171/jns.2003.99.3.0467. [DOI] [PubMed] [Google Scholar]
- 83.Lacroix M, Abi-Said D, Fourney DR, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190–198. doi: 10.3171/jns.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 84.Vuorinen V, Hinkka S, Farkkila M, Jaaskelainen J. Debulking or biopsy of malignant glioma in elderly people – a randomised study. Acta Neurochir (Wien) 2003;145:5–10. doi: 10.1007/s00701-002-1030-6. [DOI] [PubMed] [Google Scholar]
- 85.Levivier M, Violon P, Brotchi J, Goldman S, Kowalczuk A. Quantitative imaging study of extent of surgical resection and prognosis of malignant astrocytomas. Neurosurgery. 1998;43:398–399. doi: 10.1097/00006123-199808000-00151. [DOI] [PubMed] [Google Scholar]
- 86.Curran WJ, Jr, Scott CB, Horton J, et al. Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst. 1993;85:704–710. doi: 10.1093/jnci/85.9.704. [DOI] [PubMed] [Google Scholar]
- 87.Mirimanoff RO, Gorlia T, Mason W, et al. Radiotherapy and temozolomide for newly diagnosed glioblastoma: recursive partitioning analysis of the EORTC 26981/22981-NCIC CE3 phase III randomized trial. J Clin Oncol. 2006;24:2563–2569. doi: 10.1200/JCO.2005.04.5963. [DOI] [PubMed] [Google Scholar]
- 88.NCIC (National Cancer Institute of Canda) Temozolomide and Everolimus in Treating Patients With Newly Diagnosed, Recurrent, or Progressive Malignant Glioblastoma Multiforme (Study Sponsor: National Cancer Institute of Canada). 2007. Available at: http://clinicaltrials.gov/ct2/show/NCT00387400
- 89.Schering Canada Inc The Effects of Continuous 28-Day (28/28) Temozolomide Chemotherapy in Subjects With Recurrent Malignant Glioma Who Have Failed the Conventional 5-Day (5/28) Treatment (P04601AM1). 2007. Available at: http://clinicaltrials.gov/ct2/show/NCT00392171
- 90.Quinn JA, Desjardins A, Weingart J, et al. Phase I trial of temozolomide plus O6-benzylguanine for patients with recurrent or progressive malignant glioma. J Clin Oncol. 2005;23:7178–7187. doi: 10.1200/JCO.2005.06.502. [DOI] [PubMed] [Google Scholar]
- 91.Koch D, Hundsberger T, Boor S, Kaina B. Local intracerebral administration of O(6)-benzylguanine combined with systemic chemotherapy with temozolomide of a patient suffering from a recurrent glioblastoma. J Neurooncol. 2007;82:85–89. doi: 10.1007/s11060-006-9244-8. [DOI] [PubMed] [Google Scholar]
- 92.Wasserfallen JB, Ostermann S, Pica A, et al. Can we afford to add chemotherapy to radiotherapy for glioblastoma multiforme? Cost-identification analysis of concomitant and adjuvant treatment with temozolomide until patient death. Cancer. 2004;101:2098–2105. doi: 10.1002/cncr.20619. [DOI] [PubMed] [Google Scholar]
- 93.Prosser LA, Stinnett AA, Goldman PA, et al. Cost-effectiveness of cholesterol-lowering therapies according to selected patient characteristics. Ann Intern Med. 2000;132:769–779. doi: 10.7326/0003-4819-132-10-200005160-00002. [DOI] [PubMed] [Google Scholar]
- 94.Wasserfallen JB, Ostermann S, Leyvraz S, Stupp R. Cost of temozolomide therapy and global care for recurrent malignant gliomas followed until death. Neurooncology. 2005;7:189–195. doi: 10.1215/S1152851704000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dinnes J, Cave C, Huang S, Major K, Milne R. The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review. Health Technol Assess. 2001;5:1–73. doi: 10.3310/hta5130. [DOI] [PubMed] [Google Scholar]
- 96.Mabasa VH, Taylor SC. Re-evaluation of the cost effectiveness of temozolomide for malignant gliomas in British Columbia. J Oncol Pharm Pract. 2006;12:105–111. doi: 10.1177/1078155206069161. [DOI] [PubMed] [Google Scholar]
- 97.Martikainen JA, Kivioja A, Hallinen T, Vihinen P. Economic evaluation of temozolomide in the treatment of recurrent glioblastoma multiforme. Pharmacoeconomics. 2005;23:803–805. doi: 10.2165/00019053-200523080-00006. [DOI] [PubMed] [Google Scholar]
- 98.Maenpaa HO, Aaltonen K, Mantyla R, Minn H. Temozolomide treatment in glioma – experiences in two university hospitals in Finland. Acta Oncol. 2004;43:579–584. doi: 10.1080/02841860410015271. [DOI] [PubMed] [Google Scholar]
- 99.Hegi ME, Diserens AC, Gorlia T. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Eng l J Med. 2005;352:997–1003. doi: 10.1056/NEJMoa043331. [DOI] [PubMed] [Google Scholar]
- 100.Roa W, Brasher PM, Bauman G. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004;22:1583–1588. doi: 10.1200/JCO.2004.06.082. [DOI] [PubMed] [Google Scholar]
- 101.Keime-Guibert F, Chinot O, Taillandier L. Radiotherapy for glioblastoma in the elderly. N Engl J Med. 2007;356:1527–1535. doi: 10.1056/NEJMoa065901. [DOI] [PubMed] [Google Scholar]
- 102.Chinot OL, Barrie M, Frauger E, et al. Phase II study of temozolomide without radiotherapy in newly diagnosed glioblastoma multiforme in an elderly population. Cancer. 2004;100:2208–2214. doi: 10.1002/cncr.20224. [DOI] [PubMed] [Google Scholar]
- 103.Chang S, Theodosopoulos R, Sneed P. Multidisciplinary management of adult anaplastic astrocytomas. Semin Radiat Oncol. 2001;11:163–169. doi: 10.1053/srao.2001.21428. [DOI] [PubMed] [Google Scholar]
- 104.Glantz M, Chamberlain M, Liu Q, Litofsky NS, Recht LD. Temozolomide as an alternative to irradiation for elderly patients with newly diagnosed malignant gliomas. Cancer. 2003;97:2262–2266. doi: 10.1002/cncr.11323. [DOI] [PubMed] [Google Scholar]
- 105.Stupp R, Reni M, Gatta G, Mazza E, Vecht C. Anaplastic astrocytoma in adults. Crit Rev Oncol Hematol. 2007;63:72–80. doi: 10.1016/j.critrevonc.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 106.Ostermann S, Csajka C, Buclin T, et al. Plasma and cerebrospinal fluid population pharmacokinetics of temozolomide in malignant glioma patients. Clin Cancer Res. 2004;10:3728–3736. doi: 10.1158/1078-0432.CCR-03-0807. [DOI] [PubMed] [Google Scholar]
- 107.Athanassiou AE, Potamianou A, Bountouroglou N, et al. Methotrexate, etoposide, ifosamide and cisplantin (MVIP): an effective first-line therapy for IGCCC intermediate/poor prognosis patients with germ-cell tumors. Single institution experience. J BUON. 2002;7:35–41. [PubMed] [Google Scholar]