Abstract
Self reported walking distance is a clinically relevant measure of function. The aim of this study was to define patient accuracy and understand factors that might influence perceived walking distance in an elective spinal outpatients setting. A prospective cohort study. 103 patients were asked to perform one test of distance estimation and 2 tests of functional distance perception using pre-measured landmarks. Standard spine specific outcomes included the patient reported claudication distance, Oswestry disability index (ODI), Low Back Outcome Score (LBOS), visual analogue score (VAS) for leg and back, and other measures. There are over-estimators and under-estimators. Overall, the accuracy to within 9.14 metres (m) (10 yards) was poor at only 5% for distance estimation and 40% for the two tests of functional distance perception. Distance: Actual distance 111 m; mean response 245 m (95% CI 176.3–314.7), Functional test 1 actual distance 29.2 m; mean response 71.7 m (95% CI 53.6–88.9) Functional test 2 actual distance 19.6 m; mean response 47.4 m (95% CI 35.02–59.95). Surprisingly patients over 60 years of age (n = 43) are twice as accurate with each test performed compared to those under 60 (n = 60) (average 70% overestimation compared to 140%; p = 0.06). Patients in social class I (n = 18) were more accurate than those in classes II–V (n = 85): There was a positive correlation between poor accuracy and increasing MZD (Pearson’s correlation coefficient 0.250; p = 0.012). ODI, LBOS and other parameters measured showed no correlation. Subjective distance perception and estimation is poor in this population. Patients over 60 and those with a professional background are more accurate but still poor.
Keywords: Distance perception, Accuracy, Functional tests, Spinal outcome measures
Introduction
Clinical assessments and therapeutic decisions are often based on self-reported estimates of distance. Examples would be the severity of angina, vascular claudication, and chronic respiratory failure. The effect of treatment on these conditions is usually assessed by the distance a patient can walk before the onset of symptoms [7]. In the treatment of spinal disorders shuttle tests or treadmill walking would be considered the ‘gold standard’ and these are the standard clinical tools used in research [6]. Many spinal surgical clinics either lack the resource to measure accurately or have a pragmatic approach to accepting patient self-reported distance as a surrogate for actual walking distance.
The assessment of a patient’s walking ability is important in assigning scores in many functional spine outcome tools such as the Oswestry Disability Index (ODI) and the Low back outcome score. Walking is an important daily functional measure and can predict functional mobility, quality of life and outcome measures [1]. Self reported walking distance is therefore a clinically relevant measure of function.
Lumbar spinal stenosis is defined as any type of narrowing of the lumbar spinal canal, causing compression of the content of the spinal canal, due to a conflict between the available space in the canal and its content [2]. Symptoms are thought to be caused by direct mechanical compression or indirect vascular compression of the nerve roots or the cauda equina [3]. Symptoms are reported to be diverse; patients often complain of pain in the legs and the classic neurogenic claudication that is characterised by pain during walking, numbness, tingling, weakness, and radiating pain down to ankles [3].
There has been an expansion of surgical procedures for the treatment of spinal stenosis with the introduction of interspinous distraction devices and procedures to augment standard operations such as lumbar decompression. Assessment of outcome of interventional procedures is dependant upon understanding the reliability and repeatability of assessment tools. Self reported walking distance is a commonly used practical assessment tool. The documentation of the advantages and disadvantages of reliance on patients self reported disability will assist in the better understanding of which measures of outcome have greatest utility. The aims of this study were to assess the accuracy in distance estimation in patients attending an elective spinal orthopaedic outpatients setting and secondarily to understand factors that might influence perceived walking distance in this population.
Methods
A prospective study was performed at a single institution. Over a 4 month period, all eligible patients who presented to the outpatient setting were invited to participate until a sample size of 100 or more was achieved. They were asked to perform one test of distance estimation and two tests of functional distance perception using pre-measured landmarks. The degree of accuracy was assessed and compared to age and social class. Social class was indicated using the British Registrar General’s scale of social class which consists of five major categories [8]. Social class I is for professionals (doctors, lawyers), Social class II intermediate (nurses, teachers), Social class III is composed of manual and non manual workers (bus driver, cashier), whilst Social class IV is made of partly skilled workers (postman, traffic warden) and Social class V is made up of unskilled workers (labourer, window cleaner) [8]. Patients were excluded if unable to understand through reasons of language, comprehension or immobility.
Standard spine specific outcome measures such as the Oswestry disability index (ODI), Low Back Outcome Score (LBOS), visual analogue score (VAS) for leg and back and modified zung depression index (MZDI) were also collated for each of the above patients. The patient self reported claudication distance was also recorded. Pearson’s coefficient was then used to assess the degree of correlation between accuracy and the spine outcome measures aforementioned. Tests of statistical significance were made with analysis of variance (ANOVA) for differences between social classes and student’s t test for assessment of accuracy compared to age.
Results
103 patients were recruited for this study. The average age was 54 ± 18.4. Overall, the accuracy to within 9.14 m (10 yards) was achieved by only 5% of the subjects in the distance estimation. A greater proportion, 40%, was accurate to within 9.14 m (10 yards) for the two tests of functional distance perception. For the test of distance perception, the actual distance was 111 m and the mean response was 245 m (95% CI 176.3–314.7), range 36.6–1609.3 m. For the first functional test, the actual distance was 29.2 m; the mean response 71.7 m (95% CI 53.6–88.9), range 7.3–402.3 m. The second functional test had an actual distance of 19.6 m and the mean response was 47.4 m (95% CI 35.02–59.9), range 5.48–274.3 m.
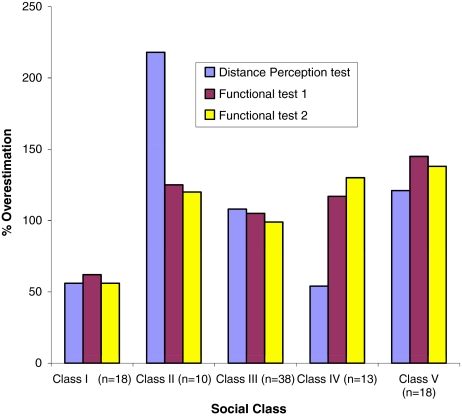
Patients over 60 years of age (n = 43) were twice as accurate with each test performed compared to those under 60 (n = 60) (average 70% overestimation compared to 140%; p = 0.06), Table 1. Patients in social class I (n = 18) were more accurate than those in classes II–V (n = 85): average 59% overestimation compared to 131%; p = 0.13, Fig. 1. Between the social groups, there was no difference in accuracy (ANOVA, p = 0.082). There was a positive correlation between poor accuracy and increasing MZD (Pearson’s correlation coefficient 0.250; p = 0.012). High ODI and other parameters measured showed no correlation with accuracy of distance perception.
Table 1.
Assessment of distance perception in comparison to age
| Estimated distance [metres (m)] | ||
|---|---|---|
| Patients <60 years old (n = 60) | Patients >60 years old (n = 43) | |
| Distance perception (actual distance = 111 m) | ||
| Mean | 256.6 | 188.7 |
| Average difference | 145.6 | 77.6 |
| % overestimation | 131.1 | 69.9 |
| Functional test 1 (actual distance = 29.2 m) | ||
| Mean | 70.1 | 51.6 |
| Average difference | 41.5 | 22.4 |
| % overestimation | 141.8 | 76.6 |
| Functional test 2 (actual distance = 19.6 m) | ||
| Mean | 48.2 | 34.6 |
| Average difference | 28.25 | 14.8 |
| % overestimation | 141.74 | 76.56 |
Fig. 1.
% Overestimation in distance perception in comparison to social class: Class I professionals, Class II intermediate, Class III manual and non-manual workers, Class IV partially skilled workers, Class V unskilled labour
Discussion
There has been a paucity of studies assessing the validity of distance estimation by patients and physicians. In Sharrack’s study [7], both groups were asked to estimate the distance between six well-known landmarks around a hospital setting. The estimates differed by up to 14.6-fold from the measured distances, and the difference between the minimum and maximum estimates was up to 62.5-fold [7]. Watson et al. [11] studied the reliability of distance estimations of claudicants and vascular surgeons, finding that both groups lack accuracy with median overestimates of 52 and 34%, respectively. A more recent study by Giantomaso et al. [4] confirmed the findings of earlier studies but also inferred that patients consistently overestimate their maximal walking distance, whereas physicians tend to underestimate. The study also found that patient’s estimates (though over-estimated) do correlate well with actual walking distance, whereas physician estimates are not at all correlated [4].
This study only looked at patient estimates of distance perception. Across the board, there was significant inaccuracy. Within this, there were under-estimators and over-estimators. Patients over 60 years of age appear to be twice as accurate as those under 60. Possibly the increased sedentary lifestyle that is prevalent in the younger generation may be responsible for this difference. A sedentary lifestyle is almost universal in developed societies, and that this is related to physical, technological and economic environmental conditions [5]. A higher proportion of patients seen with spinal stenosis are over 65 years of age although the incidence of symptomatic lumbar spinal stenosis is unknown [9].
Patients with a professional background, though only making up a small proportion of the study cohort (n = 18), were more accurate than those from other social classes; 59 versus 131%. We believe this difference is clinically significant, although not statistically significant (p = 0.13). This observation is also subject to type 2 error. Recruiting a greater number of professional patients may have led to an observation of statistical significance. We postulate that professionals are more likely to have undergone regimented training in their particular field, be more familiar with tests of ability and therefore are more accurate with distance perception compared to other groups.
All the tests of correlation showed only a positive relationship between overestimation and an increase in the MZDI, an indicator of the amount of distress suffered by a patient. We are unaware of any previous studies that have demonstrated this relationship. As walking distance is considered to be an indicator of function, patients who score high on their MZDI are likely to overestimate the amount they can do which has the potential to impact on their subsequent clinical management.
The patients in this study were only tested on the one occasion, although three different assessments were performed. This study does not take into account other personal factors such as fatigue and time of the day which have been previously noted to be important in walking assessments [4]. Taking the mean from a series of three or more walks on different days may give a more accurate representation of maximum walking distance and would take into account the learning inherent in walking tests [10]. Such an undertaking poses significant logistical difficulty and was not feasible to undertake in this instance.
The short walking tests of 29.2 or 19.6 m had a greater proportion of correct assessments. In a clinical setting doing a short walk of known distance with a patient may help the clinician determine if the patient is an over-estimator or under-estimator. Over estimation is more likely than under estimation. It is important to be aware of this if self reported distance is used as a surrogate for actual walking to claudication distance.
In conclusion, subjective distance perception is poor by patients in this outpatient spinal clinic setting. Patients over 60 and those with a professional background seem to be the most accurate. Increasing distress as assessed by MZD appears to have a negative impact on accuracy of distance perception.
References
- 1.Alexander NB, Guire KE, Thelen DG, et al. Self-reported walking ability predicts functional mobility performance in frail older adults. J Am Geriatr Soc. 2000;48(11):1408–1413. doi: 10.1111/j.1532-5415.2000.tb02630.x. [DOI] [PubMed] [Google Scholar]
- 2.Graaf A, Prak A, Bierma-Zeinstra S, Thomas S, et al. Diagnosis of lumbar spinal stenosis, a systematic review of the accuracy of Diagnostic Tests. Spine. 2006;31(10):1168–1176. doi: 10.1097/01.brs.0000216463.32136.7b. [DOI] [PubMed] [Google Scholar]
- 3.Epstein NE, Maldonado VC, Cusick JF. Symptomatic lumbar spinal stenosis. Surg Neurol. 1998;50:3–10. doi: 10.1016/S0090-3019(98)00022-6. [DOI] [PubMed] [Google Scholar]
- 4.Giantomaso T, Makowsky L, Ashworth NL, et al. The validity of patient and physician estimates of walking distance. Clin Rehabil. 2003;17(4):394–401. doi: 10.1191/0269215503cr626oa. [DOI] [PubMed] [Google Scholar]
- 5.James WP. A public health approach to the problem of obesity. Int J Obes Relat Metab Disord. 1995;19(Suppl 3):S37–S45. [PubMed] [Google Scholar]
- 6.Pratt RK, Fairbank JC, Virr A. The reliability of the shuttle walking test, the Swiss spinal stenosis questionnaire, the Oxford spinal stenosis score, and the Oswestry disability index in the assessment of patients with lumbar spinal stenosis. Spine. 2002;27(1):84–91. doi: 10.1097/00007632-200201010-00020. [DOI] [PubMed] [Google Scholar]
- 7.Sharrack B, Hughes RAC. Reliability of distance estimation by doctors and patients: cross sectional study. BMJ. 1997;315:1652–1654. doi: 10.1136/bmj.315.7123.1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith GD, Hart C, Watt G, et al. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley study. J Epidemiol Community Health. 1998;52(6):399–405. doi: 10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spivak J. Degenerative spinal stenosis. J Bone Joint Surg. 1998;80:1053–1066. doi: 10.2106/00004623-199807000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Steele BG, Holt L, Belza B, et al. Quantitating physical activity in COPD using a triaxial accelerometer. Chest. 2000;117:1359–1367. doi: 10.1378/chest.117.5.1359. [DOI] [PubMed] [Google Scholar]
- 11.Watson CJ, Phillips D, Hands L, et al. Claudication distance is poorly estimated and inappropriately measured. Br J Surg. 1997;84:1107–1109. doi: 10.1002/bjs.1800840819. [DOI] [PubMed] [Google Scholar]