Abstract
The morbidity of surgical procedures for spine tumors can be expected to be worse than for other conditions. This is particularly true of en bloc resections, the most technically demanding procedures. A retrospective review of prospective data from a large series of en bloc resections may help to identify risk factors, and therefore to reduce the rate of complications and to improve outcome. A retrospective study of 1,035 patients affected by spine tumors—treated from 1990 to 2007 by the same team—identified 134 patients (53.0% males, age 44 ± 18 years) who had undergone en bloc resection for primary tumors (90) and bone metastases (44). All clinical, histological and radiological data were recorded from the beginning of the period in a specifically built database. The study was set up to correlate diagnosis, staging and treatment with the outcome. Oncological and functional results were recorded for all patients at periodic, diagnosis-related controls, until death or the latest follow-up examination (from 0 to 211 months, median 47 months, 25th–75th percentile 22–85 months). Forty-seven on the 134 patients (34.3%) suffered a total of 70 complications (0.86 events per 100 patient-years); 32 patients (68.1%) had one complication, while the rest had 2 or more. There were 41 major and 29 minor complications. Three patients (2.2%) died from complications. Of the 35 patients with a recurrent or contaminated tumor, 16 (45.7%) suffered at least one complication; by contrast, complications arose in 31 (31.3%) of the 99 patients who had had no previous treatment and who underwent the whole of their treatment in the same center (P = 0.125). The risk of major complications was seen to be more than twice as high in contaminated patients than in non-contaminated ones (OR = 2.52, 95%CI 1.01–6.30, P = 0.048). Factors significantly affecting the morbidity are multisegmental resections and operations including double contemporary approaches. A local recurrence was recorded in 21 cases (15.7%). The rate of deep infection was higher in patients who had previously undergone radiation therapy (RT), but the global incidence of complications was lower. Re-operations were mostly due to tumor recurrences, but also to hardware failures, wound dehiscence, hematomas and aortic dissection. En bloc resection is able to improve the prognosis of aggressive benign and low-grade malignant tumors in the spine; however, complications are not rare and possibly fatal. The rate of complication is higher in multisegmental resections and when double combined approach is performed, as it can be expected in more complex procedures. Re-operations display greater morbidity owing to dissection through scar/fibrosis from previous operations and possibly from RT. The treatment of recurrent cases and planned transgression to reduce surgical aggressiveness are associated with a higher rate of local recurrence, which can be considered the most severe complication. In terms of survival and quality of life, late results are worse in recurrent cases than in complicated cases. Careful treatment planning and, in the event of uncertainty, referral to a specialty center must be stressed.
Keywords: Spine, Tumor, En bloc resection, Complication, Morbidity
Introduction
The morbidity of spine surgery as a whole is high and is well reported in the literature [1–7]. En bloc resections [8] are the procedures aimed at surgically removing a tumor in a single, intact piece, fully encased by a continuous shell of healthy tissue, which is defined as the “margin”. These operations can also be performed in the spine [9–15], where anatomical and surgical constraints make them technically demanding. Multiple approaches or a widely enlarged single posterior approach must be planned. The requirement of a margin encasing the tumor can, sometimes, be met by resecting relevant anatomical structures [16] (pleura, dura, muscles, nerve roots, nerves, vessels and so on). Intentional transgression of oncological principles [8, 13] may be considered, the advantage in terms of reduced morbidity and better functional results being weighed against the higher risk of recurrence.
En bloc resection has proved effective in improving the prognosis of primary bone tumors of the spine [9, 17–19] and the quality of life of patients with some isolated metastases, such as those from renal cell carcinoma [20, 21]. When margins are tumor free, local control by means of en bloc resection rises to 92.3% in giant cell tumor (GCT) [22], to 78% in chordoma (CH) [18] and to 82% in chondrosarcoma (CHS) [19]. These are quite remarkable data if compared with the local control achieved in the same studies by intralesional surgery: 72.2% in GCT [20, 22] 22% in CH [18] and 0% in CHS [19].
However, the morbidity of en bloc resection in the spine should always be considered in the decision-making process. Such procedures combine the complications of spine surgery by multiple approaches, tumor surgery and long-duration surgery [23] and can be expected to affect the patient’s quality of life.
Peri-operative adjuvants such as radiation therapy (RT) and chemotherapy improve oncological outcomes in some tumor types, but also exacerbate the risk of local complications [5, 6, 24].
To our knowledge, no report dealing specifically with the complications of en bloc resections in the spine has so far been published. This paper discusses the complications which have occurred in one of the world’s largest single-center series of en bloc resections in the spine.
Complications were divided into major and minor, as described by McDonnell et al. [4], and related to time of occurrence, tumor location, surgical procedures and number of resected segments, previous treatment(s) and RT.
Materials and methods
From January 1990 to December 2007, 1,035 consecutive patients with spine tumors were diagnosed and treated in the same institution. En bloc resections were performed on 134 by the senior author (S.B.) and his team. All cases underwent full clinical radiographic and histological study, and were classified according to the Enneking staging system [8] and the WBB surgical staging system [25]. Surgery was planned accordingly. From the beginning of the period, all available data were inserted into a purpose-built database for use in a prospective study.
The complications were divided into major and minor as described by McDonnell et al. [4]: Any complication that appeared to substantially alter an otherwise full and expected course of recovery was considered to be a “major” complication; others were regarded as “minor”. Complications were further classified as intra-operative, early post-operative and late post-operative. Early complications were those occurring within the first 30 days after surgery, and late complications those occurring after 30 days. Complications were also correlated with the type of resection and the approach adopted: single posterior approach or combined anterior and posterior approaches in the same surgical session. No resection was staged in more than one operation.
Some patients had previously undergone inadequate treatment, such as open biopsy violating the canal, or were referred for recurrent tumor. These were grouped in the category “contaminated cases” (CC) for analysis. Conversely, the cases diagnosed and treated at our institution were classed as “non-contaminated cases” (NCC). Patients were further divided according to whether they had undergone previous RT.
The study group consisted of 72 male and 62 female patients with an average age of 44 ± 18 (range 3–83 years). The median follow-up (FU) was 47 months (last clinical FU examination or until death: range 0–211 months). Follow-up is available for at least 24 months in 97 patients (72.4%); 19 of the remaining 37 died less than 2 years after surgery, 3 from complications and 16 from the tumor. Another 15 patients also died of the disease. Most of the tumors were primary (90 cases: 31 benign and 59 malignant); metastases occurred in 44. The location of the tumor was lumbar in 73 cases, thoracic in 57 and cervical in 4. A single posterior approach was adopted in 47 procedures, while 87 involved anterior and posterior approaches under the same anesthesia. In 101 cases a single level was resected (disk to disk or inferior endplate of the superior vertebra to superior endplate of the inferior vertebra); in 24 cases two levels, in 5 cases three, in 1 case four, in 2 cases five, in 1 case six. No procedure was performed in more than one session.
With regard to the margins described by the pathologist on examination of the final specimen, ‘wide’ was obtained in 88 cases; ‘marginal’ in 27 patients, and ‘intralesional’ in 19 cases.
Statistical analyses
Continuous variables were expressed as mean ± standard deviation, if Gaussian, or as median and 25th–75th percentile, if skewed. Normality of distribution was assessed by means of the Kolmogorov–Smirnov test. Categorical data were shown as absolute and relative frequencies.
A logistic regression analysis was applied to find predictors of complications, considering gender, age, contamination, surgical approach and radiotherapy as covariates. The multivariate model included only covariates with a P < .10 in univariate analysis and was adjusted for location and number of resected levels. Calibration and discrimination of the multivariable model were evaluated by means of the Hosmer–Lemeshow test and the c-statistic, respectively.
Freedom from local recurrences was analyzed by the Kaplan–Meier method, using the log-rank test to compare different curves. A Cox regression was performed to estimate the risk of first local recurrence due to contamination.
A two-sided P-value <.05 was considered to be significant.
For all analyses, SPSS 12.0 statistical software was used (SPSS Inc, Chicago, Illinois).
Terminology for resections [8, 25]:
- Intralesional excision: Defined as piecemeal removal of the tumor. This was subcategorized into:
- Intracapsular, if tumor removal was incomplete, in that gross or histological remnants inside the tumor capsule could be expected.
- Extracapsular, if the whole tumor mass was removed together with the peripheral tissue (3–5 mm or more of healthy peripheral tissue).
- En bloc resection: Complex surgery aimed at removing en bloc the whole tumor mass, including a cuff of healthy tissue encasing the tumor. The pathologist’s evaluation of the thickness of the resected extracapsular tissue enabled en bloc resections to be further sub-classified as:
- Intralesional, if the tumor was violated by planned or unplanned transgression to spare important neuro-vascular structures, thereby causing tumor spillage.
- Marginal, if a very thin shell of normal tissue covered the tumor.
- Wide, if a thick layer of peripheral healthy tissue, a dense fibrous cover (e.g. fascia), or an anatomical barrier not yet infiltrated (e.g. pleura), fully covered the tumor.
Results
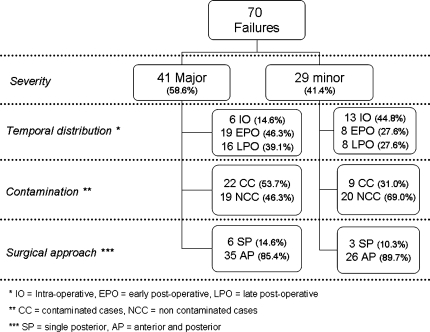
Complications after en bloc excision were observed in 47 out of 134 patients (35.1%). Thirty-two of these patients (68.1%) suffered one complication; 10 (21.3%) had 2 complications; 3 (6.4%) had 3 complications; one (2.1%) had 4 and one (2.1%) had 5 complications (pneumothorax, hematoma, transient paraplegia, late aortic dissection causing complete paraplegia, death). Correlated complications were considered and added separately. The total number of failures was 70; these were analyzed according to severity, temporal distribution, contamination (i.e. previously treated cases) and surgical approach (Fig. 1). The distribution of complications and local recurrences was discontinuous over time; for instance, no complications were recorded in 8 en bloc resections performed in 1990, while 14 complications occurred in 7 patients undergoing en bloc resection in 2005.
Fig. 1.
Distribution of 70 failures according to severity, temporal distribution, contamination, and surgical approach
Severity
Major
According to the McDonnell classification [4], 41 major complications were observed in 26 patients. The most relevant major complications were one intra-operative death due to injury of the vena cava, and two late dissections of the aorta wall, one of which was fatal (Fig. 2). One patient who suffered a massive intra-operative hemorrhage was rescued by means of infusions and drugs. Two myocardial Infarctions occurred in the post-operative course (uneventfully healed). One pulmonary embolism (leading to death) and two transitory renal failures were related to intraoperative hemodynamic imbalance. Six deep infections (5.4%) required surgical debridement and long-term multiple antibiotic treatment. A iatrogenic injury of the left ureter was recognized during surgery and repaired. In one case, temporary post-operative paraplegia was caused by a huge post-operative hematoma; this patient fully recovered, but 8 months later developed paraplegia again due to the above-mentioned fatal aorta wall dissection. Another peculiar major complication was an ex-vacuo fronto-parietal subdural hematoma (Fig. 3) due to depletion of cerebrospinal fluid (an intraoperative lesion of the dura could not be repaired).
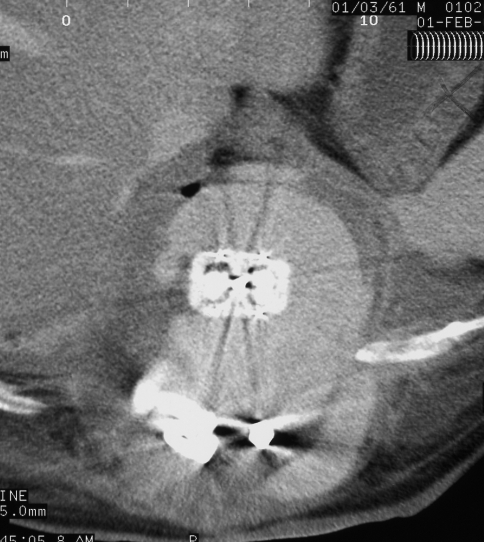
Fig. 2.
Dissection of the aortic wall 8 months after double-approach en bloc resection of a T10 chondrosarcoma previously treated by intralesional excision and cement filling. The patient died on referral to the vascular surgery emergency room
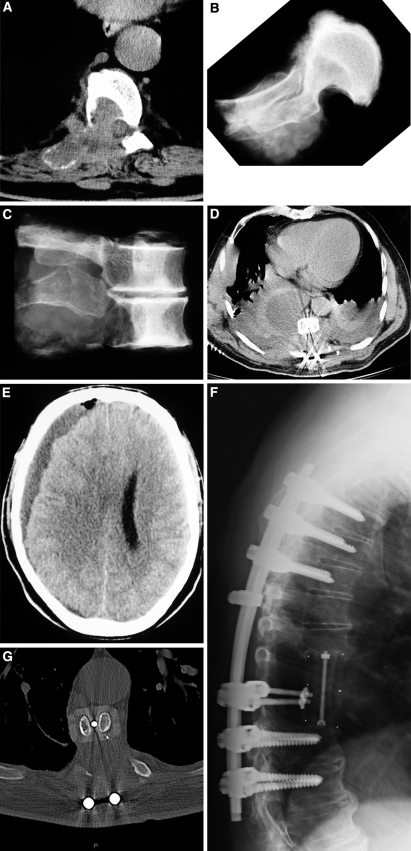
Fig. 3.
a Recurrence of giant cell tumor of T8 and T9 previously treated by partial excision. b, c X-ray of the specimen. En bloc resection, tumor-free margins. d Huge postoperative collection of CSF after non-waterproof suture, during double-approach en bloc resection. The dura injury occurred during the posterior approach (first step) and resulted in a heavy loss of CSF. e Fronto-parietal subdural ex-vacuo hematoma resulting from the CSF depletion. f, g 6-year follow-up examination: no evidence of disease, full function, excellent quality of life
Ten patients (7%) required revision of the posterior instrumentation.
Overall, three patients (2%) died as a result of complications.
Minor
Twenty-nine minor complications were observed in 27 patients. Nine of these suffered dural tears, which were successfully repaired during the same procedure. Injuries to the iliac vein and the vertebral artery in two separate patients were immediately repaired and had no sequelae. In three patients, malposition of the hardware resulted in asymptomatic deformity. One patient complained of retrograde ejaculation. Two cases of acute renal failure were successfully treated by medical therapy.
Temporal distribution
Intra-operative complications
In 18 patients, 6 major and 13 minor intraoperative complications were recorded. Major intraoperative complications were vena cava lesion leading to death, lesion of the aorta, massive hemorrhage from the epidural plexus, and dural tear unrepaired as the lesion was on the opposite side to that of the approach] (2 cases). Minor complications included malposition of the anterior cage, and dural and vascular injuries which were immediately repaired successfully.
Early post-operative complications
Nineteen major complications and eight minor complications were observed in 18 patients. The major complications included a fatal massive pulmonary embolism and a post-operative paraplegia due to both a massive hematoma and hemothorax. Deep vein thrombosis, pneumothorax and tracheal lesions during intubation were reported among the minor complications.
Late post-operative complications
Sixteen major and 8 minor complications were recorded in 19 patients. The most severe cases were two aorta dissections, which occurred 3 and 8 months after surgery; one was fatal (Fig. 2), while the other was successfully treated by open surgery. Other cases were: deep infections (4), hardware failure or loosening (11), deformity (3), laparoceles (2) and retrograde ejaculation (1).
Contamination
Thirty-six patients (26.9%) underwent en bloc resection after unsuccessful previous treatment or open biopsy which had contaminated the epidural space and 98 were treated since the beginning in the AA’s Institution. Five out of 30 patients with primary benign tumors, 21 out of 60 with malignant tumors and 10 out of 44 with metastases were admitted to our department owing to recurrence or progression of the disease. We grouped these in the “contaminated cases” (CC) category for analysis. Conversely, the 98 cases fully diagnosed and treated at the AA’s Institution were included in the “non-contaminated cases” (NCC) category.
Of the 36 patients in the CC group, 17 (47.2%) had at least one complication, seven of these had more than one, and one had 5. The total number of complications was 31 (22 major and 9 minor): 7 intra-operative; 16 early and 8 late postoperative. Two of the three patients who died of complications belonged to this group.
Of the 98 NCC patients, 29 (29.6%) suffered 19 major and 20 minor complications. Eight patients had more than one complication. The complications were intra-operative in 12 cases (one fatal), early postoperative in 11 and late postoperative in 16.
Surgical approach
Combined anterior and posterior approaches were performed during the same operation [10, 12–14] in 87 patients, with two surgeons contemporarily working, while en bloc resection was achieved by means of a single posterior approach [9–11] in 47 cases. The 87 anterior approaches were cervical pre-vascular (1), thoracotomy (20), extrapleural thoraco-abdominal (36), lumbar retroperitoneal (28) and transperitoneal (2).
It is noteworthy that only 5 patients out of 47 (10.6%) who underwent surgery through a single posterior approach had at least one complication (total 9: 6 major, 1 lethal). Conversely, 42 of the 87 patients (48.3%) who underwent a double-approach en bloc resection had at least one complication. The incidence of complications was significantly different when compared on the basis of the surgical approach (P < 0.0001). The morbidity of the anterior approach to the spine is well known [3], in the treatment of tumors it is even worse. A massive hemorrhage due to injury of the vertebral artery occurred during the pre-vascular neck approach. Among the 20 thoracotomy approaches, 4 major complications were recorded. In the 36 extrapleural thoraco-abdominal approaches, 1 major and 2 minor complications arose. During the retroperitoneal approaches, eight major complications (one causing death) and three minor complications occurred.
Radiation therapy
In the series reported, 51 patients underwent RT before or after surgery. Fifteen of these (29.4%) had 21 complications, including 5 deep infections requiring surgical treatment and 1 superficial infection managed with antibiotics. The two cases of late dissection of the aorta occurred after RT (doses 42 and 44 Gy) performed as an adjuvant after an anterior surgical approach. One case of instability due to post-radiation bone necrosis and failure of the posterior hardware requiring revision was also included in this group. Conversely, 35 of the 83 patients (42.2%) who did not undergo RT had at least one complication.
Predictors of complications
Minor complications
The combined surgical approach (OR = 4.92, 95%CI 1.35–17.88, P = 0.016) was a significant. independent predictor of minor complications (Hosmer–Lemeshow test = 0.991, c-statistic = 0.68). Multilevel resection and the tumor location were not significant.
Major complications
The multivariate model used to predict major complications included contamination, combined surgical approach, multilevel resection and tumor location. The combined approach (OR = 3.79, 95%CI 1.09–13.17, P = 0.036) and the number of resected spine segments (OR = 1.95, 95%CI 1.07–3.56, P = 0.030) were independent predictors of major complications. No relationship was found comparing lumbar to cervical and thoracic tumors (Table 1).
Table 1.
Predictivity of complications (major complications)
| Variable | Univariable analysis | Multivariable analysis* | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P-value | OR | 95%CI | P-value | |
| Male gender | 1.54 | 0.64–3.70 | 0.332 | |||
| Age | 1.02 | 0.99–1.04 | 0.169 | |||
| Previous treatment | 3.00 | 1.23–7.34 | 0.016 | 2.06 | 0.77–5.49 | 0.150 |
| Combined approach | 3.64 | 1.17–11.30 | 0.025 | 3.79 | 1.09–13.17 | 0.036 |
| RT therapy | 1.52 | 0.64–3.60 | 0.346 | |||
| Lumbar location | 0.43 | 0.18–1.03 | 0.059 | 0.51 | 0.18–1.49 | 0.217 |
| Malign stage | 1.02 | 0.39–2.66 | 0.963 | |||
| No. of levels resected | 2.45 | 1.41–4.24 | 0.001 | 1.95 | 1.07–3.56 | 0.030 |
* Hosmer–Lemeshow test = 0.947; AUC = 0.74 (95%CI 0.63–0.85, P < 0.0001)
Calibration of the model was very high (Hosmer–Lemeshow test = 0.947) and discrimination was also good (c-statistic = 0.74, 95%CI 0.63–0.85, P < 0.0001). This means that the risk of major complications increases in patients operated with combined approach and is positively correlated to the number of resected levels (Table 1).
Local recurrences
Following the 134 consecutive en bloc resections considered, 21 local recurrences (15.7%) were recorded after a median period of 63 months (4–174 months); 13 (61.9%) of these required further operations.
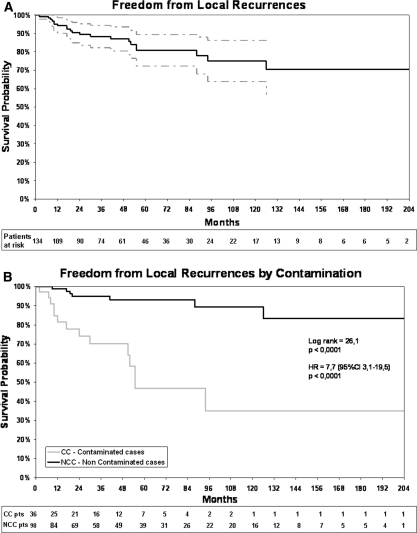
Only 2 patients are still alive without evidence of disease after 50 and 95 months of follow-up; 10 died (2–86 months after local recurrence), and 9 are alive with disease (0–85 months after the local recurrence). Local recurrences were recorded in 14 (38.9%) of the 36 patients in the CC group. Twelve local recurrences were observed in the series of primary malignant tumors. Five of the 14 died of local recurrences and/or diffuse disease after an average of 23 months (range: 10–50 months). Local recurrences were recorded in 7 (7.1%) of the 98 patients in the NCC group.
Freedom from local recurrences after 17 years of follow-up was 70.4 ± 6.9% (CC group = 35.0 ± 13.1%, NCC group = 83.4 ± 7.3%, P < 0.0001) as shown in Fig. 4a and b.
Fig. 4.
Freedom from local recurrences. a Overall (continuous black line; range in dotted gray). b Comparison between contaminated cases (CC, gray line) and non contaminated cases (NCC, black line)
Discussion
In order to identify the risk factors and therefore reduce the rate of complications and improve the outcome, we reviewed a series of 134 en bloc resections, a peculiar and very demanding surgical procedure, treated in the same Institution by the same team, after full staging and oncological planning. This can be considered to represent a homogeneous series of cases It is commonly accepted that the morbidity of surgical procedures for spine tumors is related to both the altered anatomy secondary to the tumor growth, and the fibrosis caused by pre-operative RT or previous surgery. The peculiar surgical techniques required to achieve en bloc resection are expected to increase the rate of complications, as extratumoral resection requires to violate anatomical barriers and manipulate or sacrifice vascular and nervous structures. Bleeding from the tumor mass is not expected, as surgery is extralesional. It may, however, be caused by incidental tumor violation or accidental damage of the epidural plexus and can lead to hemodynamic imbalance if not promptly treated. Manipulation of vascular structures can cause bleeding, which may even be fatal, particularly in revision procedures. After such long-duration surgery, post-operative complications may include early problems related to wound dehiscence or infections. Late complications may include mechanical failures, such as breakage or loosening of the complex circumferential reconstructions; local recurrences may reflect the failure of oncological planning.
Accurate analysis of all the incidences is very difficult as most are multifactorial and may lead to other complications (e.g. hematoma after en bloc resection in the thoracic spine creates hemopneumothorax due to resection of the barrier for oncological purposes, and can cause paraplegia). In this review, we have not considered the sacrifice of important structures performed for oncological purposes to be complications.
Severity
The global rate of complications was quite high after en bloc resection: 47 out of 134 (35.1%) patients had at least one complication in the period considered (0–211 months, median 47 months). En bloc resection in our experience did not present a learning curve with regard to the occurrence of complications. The incidence of complications seemed to be mainly related to the complexity of the procedure, and therefore displayed an unpredictable distribution over time. An important aspect concerns the survival and quality of life of the 27 patients who had at least one major complication. Three died of the complication, eight died of their disease and three are living with their disease. However, 13 (13/27 = 48.1%) are alive and have excellent performance status (like uncomplicated cases) after 25–160 months of follow-up (Fig. 3).
Temporal distribution
Three patients died as a consequence of a complication: one intraoperatively (injury of the cava), one post-operatively (pulmonary embolism) and one 8 months after the operation (aortic wall dissection). All the complications observed were equally distributed over the three time-periods considered (intraoperative, early and late postoperative) Intraoperative complications are related to manipulation of important and vital structures, the risk of injury being higher in patients who have already undergone surgery or previous RT (fibrous scar, tissue fragility). Manipulation of the spinal cord, especially in the thoracic spine, should be very careful. One patient in this series was paraplegic on waking up, but improved significantly (Frankel A to D) after a rehabilitation protocol. Thoracic root transection causes minimal post-operative problems but allows an easier approach to the tumor mass by reducing traction on the cord. Dural tears are more likely when surgery is performed through the scar from a previous operation. Immediate suturing with muscular graft coverage generally leads to prompt and satisfactory healing. When water-proof suturing cannot be performed, CSF depletion may lead to further complications (Fig. 3). Post-operative hematoma always forms whenever a large void is created by the tumor resection, and may cause immediate paraplegia and early deep infections.
Hemodynamic stability is the main intraoperative concern of anesthetists during en bloc resections, as in all long-duration operations. This can also affect the early post-operative course. In our series, myocardial infarction following a rapid decrease in intra-operative hemoglobin rate complicated two procedures, ad an episode of paroxysmal tachycardia was observed; fortunately, all the patients recovered in the following few months. A post-operative pulmonary embolism was fatal in one patient. Renal incompetence also followed incomplete control of hemodynamics. Late complications can also be related to intraoperative work, such as dissections of the aortic walls in patients who have previously undergone surgery or RT (Fig. 2) and in whom detachment of the tumor from the aorta is difficult. In such cases, an aortic bypass should be included in surgical planning to prevent intraoperative injuries and late dissections.
Contamination/referred patients
A higher rate of complications was observed in the group of patients who underwent en bloc resection after open biopsy or previous treatment followed by recurrence. Indeed, 17 on 36 (45.5%) patients in this latter group had at least one complication, compared with 30 on 98 (31%) treated from the beginning in the same center. In particular, a higher risk of major complications was observed: 22 major complications in 17 previously treated patients, compared with 9 major complications in the remaining 30 patients.
Surgical approach
En bloc resection by means of a single posterior approach seems less risky (5 on 47 patients with complications had undergone resection through this approach [11] versus 42 on 87 in whom a double approach [14] had been adopted). Another relevant factor was the surgical complexity, as expressed by the number of resected levels.
These data are related as the double-approach procedure is obviously performed in larger tumors, requiring multisegmental resections, which required more demanding planning for extralesional resection. The morbidity of the anterior approach per se was comparable to that reported by Faciszewski et al. [3].
Radiation therapy
Contrary to what was expected, the rate of complications in the group of patients who underwent adjuvant RT was not higher. Fifteen of the 51 (29%) patients who underwent RT suffered at least one complication, while 32 of the 83 (38.5%) patients whose treatment plan did not involve RT had complications. However, 5 on 6 infections observed in the whole series, and both late dissections of the aortic wall occurred in patients who had had radiation therapy. It may therefore be concluded that radiation-related complications are not more frequent but are more serious and life threatening.
Hardware failures
En bloc resection involves not only resecting bone but also muscle and ligaments, and sacrificing anatomical barriers. The consequent instability is therefore complete and complex circumferential reconstruction is required [14, 26–28]. As this surgical technique is aimed at removing the tumor, long survival is expected; autogenous grafts and/or bone substitutes should be used to achieve spinal fusion. Chemotherapy and RT may affect the possibility of achieving fusion, and timing is critical. The reconstructive technique proposed includes a posterior pedicle screws and rods titanium construct connected with a modular carbon-fiber system filled with autogenous graft or bone substitutes for anterior column reconstruction [28]. This system failed in 10 (7%) of our patients, owing to too short posterior fixation, which was unable to counteract the imbalance due to muscle and ligament sacrifice. These events cannot be connected with RT in this series. No failure of the anterior construct was observed.
Predictors of major complications
Longer operations with extensive exposure of tissue, especially when contemporary open posterior and anterior transthoracic or retroperitoneal approaches are used, seems to increase the risk of major complications, as well as the multilevel resected levels (Table 1). Infections seem to be related to previous RT.
Local recurrences
The main aim of en bloc resection is local and systemic control of the disease, and the achievement of this goal justifies the high level of morbidity. The risk of local recurrence is directly related to the margin of resection [8]. Epidural extension of the tumor increases the risk of local recurrence [11, 13, 16, 17]. Therefore, even major neurological sacrifices must be considered in the decision-making process, given that a local recurrence jeopardizes neurological function and worsens the prognosis. The survival and quality of life of patients with recurrences are very poor. In the series considered, 13 of the 21 patients who suffered recurrences required at least one further operation and only 2 are alive at the final follow-up (one of these had the only benign recurrent tumor). Moreover, comparison between the incidence of local recurrence in CC patients (38.9%) and in NCC patients (7.1%) (Fig. 4b) is illuminating; indeed, it reveals that the prognosis is mainly related to the first treatment and that the infringement of oncological principles may be followed by very serious consequences, as local control is increasingly difficult to achieve through the treatment of further recurrences. Intentionally violating oncological principles to improve the functional outcome means performing intralesional surgery, which reduces the possibility of local control [9–22].
Conclusions
The surgical techniques of en bloc resections are clearly described in the literature. Although there are few reports on large series, these surgical procedures seem to dramatically improve local control in aggressive benign and low-grade malignant bone tumors, also in the spine. Oncologic criteria should guide the decision-making process regarding bone tumors of the spine [8–25]. When en bloc resection is the procedure of choice, surgical planning should take into account not only the functional sacrifices required to meet oncological requirements, but also the intrinsic morbidity of these procedures. This article describes the incidence and type of complications recorded in a large single-center series of en bloc resections, and highlights the predictors of these events. The data support the conclusion that local recurrence is the worst complication, as this negatively affects quality of life and prognosis. By contrast, half of the patients who suffered a major complication are alive and present no evidence of disease after 25–160 months of follow-up.
The results in terms of better prognosis and better local control [9–22] justify performing such highly demanding and risky procedures in aggressive benign and in low-grade malignant bone tumors.
The main risk factors identified on reviewing the series reported were:
manipulation of important and vital structures after previous surgery or radiation;
incomplete intraoperative control of hemodynamics;
double combined approach;
too short posterior fixation and lack of anterior support.
Generally speaking, the incidence of complications and recurrences is significantly higher in revision surgery; the first treatment therefore strongly influences the final outcome from both the oncologic and functional points of view. The whole treatment, from biopsy to resection, should be performed in the same center. Radiation therapy does not increase the rate of complications, but is associated with the most dangerous ones.
En bloc resections should be performed by specifically dedicated teams, including trained oncological surgeons and anesthesiologists.
The decision-making process leading up to en bloc resection should consider not only the high morbidity here reported, but also the positive impact on local control and prognosis in aggressive benign and low-grade malignant tumors. In some isolated metastases from renal cell carcinoma, too, the clinical advantages in terms of quality of life and survival are considerable. Before deciding to reduce morbidity by adopting less aggressive surgery or by intentionally violating oncologically appropriate margins, the higher risk of local recurrence should be considered, and the consequent worsening of the prognosis. The greater morbidity and the higher risk of further recurrence associated with the treatment of a recurrent tumor should also be considered. The surgeon who treats the patient first has a great responsibility, as it is the first treatment that most affects prognosis; in order to prevent a long story of multiple recurrence, complications and painful tumor progression, greater morbidity of the first treatment (as in most of the cases successfully treated) is acceptable.
The high risk of complications should not discourage surgeons from performing en bloc resection when needed, provided that it is technically possible. Most of the patients who sustain complications benefit from the better local control resulting from en bloc resection. Conversely, local recurrences, which mainly result from inappropriate surgery, negatively affect prognosis and are associated with a higher risk of complications during subsequent revision surgery.
Acknowledgments
The authors thank Tiziana De Santo (Medtronic Italy) for her most valuable assistance in statistical analysis, Bernard Patrick for his assistance in translation and Carlo Piovani for imaging and documentation.
References
- 1.Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine. 2008;33:2243–2247. doi: 10.1097/BRS.0b013e31817d1d4e. [DOI] [PubMed] [Google Scholar]
- 2.Weiss HR, Goodall D. Rate of complications in scoliosis surgery—a systematic review of the Pub Med literature. Scoliosis. 2008;3:9. doi: 10.1186/1748-7161-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic, lumbar spine in adults. A review of 1223 procedures. Spine. 1995;20:1592–1599. doi: 10.1097/00007632-199507150-00007. [DOI] [PubMed] [Google Scholar]
- 4.McDonnell MF, Glassman SD, Dimar JR, Puno HMR, Johnson JB. Perioperative complications of anterior procedures of the spine. J Bone Joint Surg Am. 1996;78:839–847. doi: 10.2106/00004623-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 5.McPhee IB, Williams RP, Swanson CE. Factors influencing wound healing after surgery for metastatic disease of the spine. Spine. 1998;23:726–733. doi: 10.1097/00007632-199803150-00015. [DOI] [PubMed] [Google Scholar]
- 6.Pascal-Moussellard H, Broc G, Pointillart V, Simeon F, Vital JM, Senegas J. Complications of vertebral metastasis surgery. Eur Spine J. 1998;7:438–444. doi: 10.1007/s005860050105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wise JJ, Fishgrund JS, Herkowitz HN, Montgomery D, Kurtz LT. Complication, survival rates and risk factors of surgery for metastatic disease of the spine. Spine. 1999;24:1943–1951. doi: 10.1097/00007632-199909150-00014. [DOI] [PubMed] [Google Scholar]
- 8.Enneking WF. Muscoloskeletal tumor surgery. New York: Churchill Livingstone; 1983. pp. 69–122. [Google Scholar]
- 9.Stener B. Complete removal of vertebrae for extirpation of tumors. Clin Orthop Relat Res. 1989;245:72–82. [PubMed] [Google Scholar]
- 10.Roy-Camille R, Mazel Ch, Saillant G, Lapresle Ph. Treatment of malignant tumors of the spine with posterior instrumentation. In: Sundaresan N, Schmidek HH, Schiller AL, Rosenthal DI, editors. Tumors of the spine. Diagnosis and clinical management. Philadelphia: W.B.Saunders; 1990. pp. 473–492. [Google Scholar]
- 11.Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine. 1997;22:324–333. doi: 10.1097/00007632-199702010-00018. [DOI] [PubMed] [Google Scholar]
- 12.Sundaresan N, DiGiacinto GV, Krol G, Hughes JEO. Complete spondylectomy for malignant tumors. In: Sundaresan N, Schmidek HH, Schiller AL, Rosenthal DI, editors. Tumors of the spine. Diagnosis and clinical management. Philadelphia: W.B.Saunders; 1990. pp. 438–445. [Google Scholar]
- 13.Fisher CG, Keynan O, Boyd MC, Dvorak MF. The surgical management of primary tumors of the spine. Spine. 2005;30:1899–1908. doi: 10.1097/01.brs.0000174114.90657.74. [DOI] [PubMed] [Google Scholar]
- 14.Boriani S (2000) Subtotal and total vertebrectomy for tumours. In: Surgical techniques in orthopedics and traumatology 55-070-A. Editions Scientifiques et Medicales Elsevier, Paris
- 15.Boriani S, Biagini R, Iure F, Bertoni F, Malaguti MC, Di Fiore M, Zanoni A. En bloc resection of bone tumors of the thoracolumbar spine. A preliminary report on 29 patients. Spine. 1996;21:1927–1931. doi: 10.1097/00007632-199608150-00020. [DOI] [PubMed] [Google Scholar]
- 16.Biagini R, Casadei R, Boriani S, Erba F, Sturale C, Mascari C, Bortolotti C, Mercuri M. En bloc vertebrectomy and dural resection for chordoma: a case report. Spine. 2003;28:E368–E372. doi: 10.1097/01.BRS.0000084644.84095.10. [DOI] [PubMed] [Google Scholar]
- 17.Hart RA, Boriani S, Biagini R, Currier B, Weinstein JN. A System for surgical staging and management of spine tumors. A clinical outcome study of giant cell tumors of the spine. Spine. 1997;22:1773–1783. doi: 10.1097/00007632-199708010-00018. [DOI] [PubMed] [Google Scholar]
- 18.Boriani S, Bandiera S, Biagini R, Bacchini P, Boriani L, Cappuccio M, Chevalley F, Gasbarrini A, Picci P, Weinstein JN. Chordoma of the mobile spine: fifty years of experience. Spine. 2006;31:493–503. doi: 10.1097/01.brs.0000200038.30869.27. [DOI] [PubMed] [Google Scholar]
- 19.Boriani S, Iure F, Bandiera S, Campanacci L, Biagini R, Di Fiore M, Bandello L, Picci P, Bacchini P. Chondrosarcoma of the mobile spine: report on 22 cases. Spine. 2000;25:804–812. doi: 10.1097/00007632-200004010-00008. [DOI] [PubMed] [Google Scholar]
- 20.Stener B, Henriksson C, Johansson SL, Gunterberg B, Pettersson S. Surgical removal of bone and muscle metastases of renal carcinoma. Acta Orthop Scand. 1984;55:49. doi: 10.3109/17453678408992944. [DOI] [PubMed] [Google Scholar]
- 21.Sakaura H, Hosono N, Mukai Y, Ishii T, Yonenobu K, Yoshikawa H. Outcome of total en bloc spondylectomy for solitary metastasis of the thoracolumbar spine. J Spinal Disord Tech. 2004;17:297–300. doi: 10.1097/01.bsd.0000096269.75373.9b. [DOI] [PubMed] [Google Scholar]
- 22.Boriani S, Bandiera S, Casadei R, Boriani L, Donthineni R, Biagini R (in press) Giant cell tumor of the mobile spine. A review of 49 cases [DOI] [PubMed]
- 23.Di Fiore M, Lari S, Boriani S, Fornaro G, Perin S, Malferrari A, Zanoni A. Major vertebral surgery: intra- and postoperative anaesthesia-related problems. Chir Organi Mov. 1998;83:65–72. [PubMed] [Google Scholar]
- 24.Otsuka NY, Hey L, Hall JE. Postlaminectomy and postirradiation kyphosis in children and adolescents. Clin Orthop. 1998;354:189–194. doi: 10.1097/00003086-199809000-00023. [DOI] [PubMed] [Google Scholar]
- 25.Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine: terminology and surgical staging. Spine. 1997;22:1036–1044. doi: 10.1097/00007632-199705010-00020. [DOI] [PubMed] [Google Scholar]
- 26.Fourney DR, Abi-said D, Lang FF, McCutcheon IE, Gokaslan ZL. Use of pedicle screw fixation in the management of malignant spinal disease: experience in 100 consecutive procedures. J Neurosurg. 2001;94:25–37. doi: 10.3171/spi.2001.94.1.0025. [DOI] [PubMed] [Google Scholar]
- 27.Boriani S, Biagini R, Iure F, Bandiera S, Di Fiore M, Bandello L, Malaguti MC, Picci P, Bacchini P. Reconstruction surgery in the treatment of vertebral tumors. Chir Organi Mov. 1998;83:53–64. [PubMed] [Google Scholar]
- 28.Boriani S, Biagini R, Bandiera S, Gasbarrini A, Iure F. The reconstruction of the anterior column of the thoracic and lumbar spine with the carbon fiber stackable cage system. Orthopedics. 2002;25:37–42. doi: 10.3928/0147-7447-20020101-14. [DOI] [PubMed] [Google Scholar]