Abstract
Evaluation of the kyphosis angle in thoracic and lumbar burst fractures is often used to indicate surgical procedures. The kyphosis angle could be measured as vertebral, segmental and local kyphosis according to the method of Cobb. The vertebral, segmental and local kyphosis according to the method of Cobb were measured at 120 lateral X-rays and sagittal computed tomographies of 60 thoracic and 60 lumbar burst fractures by 3 independent observers on 2 separate occasions. Osteoporotic fractures were excluded. The intra- and interobserver reliability of these angles in X-ray and computed tomogram, using the intra class correlation coefficient (ICC) were evaluated. Highest reproducibility showed the segmental kyphosis followed by the vertebral kyphosis. For thoracic fractures segmental kyphosis shows in X-ray “excellent” inter- and intraobserver reliabilities (ICC 0.826, 0.802) and for lumbar fractures “good” to “excellent” inter- and intraobserver reliabilities (ICC = 0.790, 0.803). In computed tomography, the segmental kyphosis showed “excellent” inter- and intraobserver reliabilities (ICC = 0.824, 0.801) for thoracic and “excellent” inter- and intraobserver reliabilities (ICC = 0.874, 0.835) for the lumbar fractures. Regarding both diagnostic work ups (X-ray and computed tomography), significant differences were evaluated in interobserver reliabilities for vertebral kyphosis measured in lumbar fracture X-rays (p = 0.035) and interobserver reliabilities for local kyphosis, measured in thoracic fracture X-rays (p = 0.010). Regarding both fracture localizations (thoracic and lumbar fractures), significant differences could only be evaluated in interobserver reliabilities for the local kyphosis measured in computed tomographies (p = 0.045) and in intraobserver reliabilities for the vertebral kyphosis measured in X-rays (p = 0.024). “Good” to “excellent” inter- and intraobserver reliabilities for vertebral, segmental and local kyphosis in X-ray make these angles to a helpful tool, indicating surgical procedures. For the practical use in lateral X-ray, we emphasize the determination of the segmental kyphosis, because of the highest reproducibility of this angle. “Good” to “excellent” inter- and intraobserver reliabilities for these three angles could also be evaluated in computed tomographies. Therefore, also in computed tomography, the use of these three angles seems to be generally possible. For a direct correlation of the results in lateral X-ray and in computed tomography, further studies should be needed.
Keywords: Spine, Fracture, Kyphosis, Cobb angle, Intra- and interobserver reliability
Introduction
The kyphosis is the most common malposition of the fractured thoracic or lumbar spine. Most fractures develop at the anterior part of the spinal column. The thoracolumbar junction is the preferred part for spinal fractures. At this spinal level about two-third of the load is carried to the anterior spinal column. Without treatment, these fractures lead in most cases to a kyphotic deformity. The progression of kyphosis seems to be influenced mostly by the initial vertebral deformation in the sagittal plane measurable with the Cobb angle [2, 10, 14, 34]. The degree of the vertebral kyphosis shows a direct correlation with the destruction of the bone substance of the fractured vertebra. Following Böhler and Trojan [2, 34] static problems can be developed, if the kyphosis shows an angulation of ≥15° in the sagittal plane [2, 14, 34]. If the kyphosis exceeds this degree, the destruction of bone stock is so gravely, that “bone healing” can only start, when the pretraumatic conditions of vertebral height and profile are reconstructed and stabilized [10, 14, 34]; otherwise, the fracture could be filled on with fibrous tissue, which could endanger the structural integrity of the vertebral body [10]. Therefore, instabilities of the anterior column should be restored and stabilized due to fracture healing has been occurred [9].
Other arguments for a surgical treatment were given by Koller et al. [18]. The authors evaluated the radiological and clinical long-term outcome in thoracolumbar and lumbar burst fractures without neurological deficits. A special focus was centred on the impact of the regional posttraumatic kyphosis, adjacent-level compensatory mechanisms and the global spine balance on the clinical outcome. Spinal adaptability to compensate posttraumatic kyphotic deformity varied in the ranges dictated by pelvic geometry and in particular the pelvic incidence. Therefore, surgical reconstruction and maintenance of a physiologically shaped spinal curve might be the appropriate treatment in more severely crushed thoracolumbar and lumbar burst fractures.
General advantages of the surgical treatment are optimized decompression, fusion of movement segments and mobilization without orthesis, but the main goal remains to avoid the development of a postoperative kyphosis. Böhler and Trojan [2, 34] described that a posttraumatic kyphosis of ≥15° produces always disorders in the long-term follow-up and McLain et al. [24] reported symptoms or functional deficits of the spine for posttraumatic kyphosis ≥10°. Gebhard et al. [11] emphasize a surgical treatment at the fractured spine, if the initial fracture kyphosis is measured to be >20°. This grad of kyphosis is also in our department, an indication for a surgical procedure. If non-operative treatment is indicated, patients are serially followed up for progression of the kyphosis by X-ray. Significant progression is often considered as a nonoperative treatment failure. Reliable and reproducible measurements as well as accurate communication are paramount to clinical decision-making.
Generally, radiographic measurements often play a central role in orthopedic and trauma surgeon decisions, not only in case of spinal fracture. Therefore, it is important to understand the limitations of all radiographic measurement methods [7]. At the thoracic and lumbar spine, using composite measurements of combined frontal and sagittal plane deformities, it should be considered that there are remarkably wide and irregular disperses evaluating, for example, the reciprocal angulation of vertebral bodies in relation to the others in the sagittal plane performed at healthy, asymptomatic individuals [30] and a wide range of the normal sagittal alignment [1]. On the other hand, most asymptomatic individuals are able to maintain their sagittal alignment, despite advancing life. The loss of distal lumbar lordosis is most responsible for sagittal imbalance in those individuals who do not maintain sagittal alignment. This anticipated loss of lordosis, which occurs with the age, should be taken into consideration, indicating spinal surgery [12].
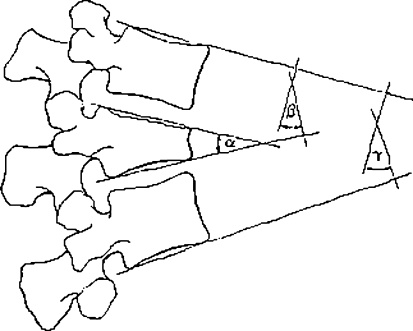
Multiple different methods have been described for measuring fractured vertebras in the operative and nonoperative treatment [5, 6, 23]. The Cobb method [6] remains the most commonly used techniques for radiographic measurement of traumatic or idiopathic kyphosis (see Fig. 1) [19, 32] and is recognized as gold standard [16]. Although, the intra- and interobserver variability of the Cobb method for coronal plane deformity [4, 19, 25, 32] and for the lumbar lordosis [27] have been well studied, the same cannot be said for the measurement of fracture kyphosis, especially using the vertebral, segmental and local kyphosis according to the method of Cobb [6].
Fig. 1.
Vertebral (α), segmental (β) and local (γ) kyphosis according to Cobb (3)
Three goals should be evaluated by the following study: (1) determination of inter- and intraobserver reliability of the vertebral, segmental and local kyphosis measurement according to the method of Cobb [6] in lateral X-rays using a large collective of 120 patients with lumbar and thoracic burst fractures. (2) Determination of inter- and intraobserver reliability of the vertebral, segmental and local kyphosis measurement according to the method of Cobb [6] measured in sagittal computed tomographies. (3) Statistical comparison of the mean inter- and intraobserver reliabilities in both diagnostic work ups (lateral X-ray vs. sagittal computed tomography) and in both fracture localizations (thoracic vs. lumbar spine fractures).
Patients and methods
To evaluate the necessary sample size and the required number of observers, a literature research [8, 13, 15, 22, 29, 33, 35] was performed. Several recent publications evaluating inter- and intraobserver reliabilities of spinal pathologies could be located, most of them using 60 or less X-rays or CT scans [8, 13, 29] and a minimum of 3 observers [22, 29, 33, 35]. Therefore, 120 consecutive patients––60 with thoracic and 60 with lumbar burst fractures––were retrospectively selected from the surgically treated patient collective of our trauma centre. We used for our evaluation the lateral X-rays and sagittal computed tomograms of each patient. Inclusion criteria for selection were legible films in computed tomogram and X-ray in good conditions and the possibility to measure the vertebral, segmental and local kyphosis in both film sets of each patient. Included were only patients with traumatic vertebral burst fractures. In default of a bone mineral density scan in emergency patients, patients with osteoporotic vertebral fractures were excluded by anamnesis of the injury and by age definition of less than 50 years at the time of accident. This age was used, according to the guidelines of the German speaking science communities for osteology (DVO), which attribute no clinical relevance for a fracture-promoting primary osteoporosis for women before menopause and for men younger than 60 years [26]. If X-rays or computed tomographies aroused any suspicion of reduced bone mass, these pictures were also excluded from the study.
Measurement procedure
All films were numbered by an independent observer who did not perform any measurements. Three independent observers, one medical student (A), one orthopedic-trauma surgeon (B) and one orthopedic-trauma surgeon in the third year of education (C) were identified. The three measurement techniques included: (1) the vertebral kyphosis, (2) the segmental kyphosis and (3) the local kyphosis according to the method of Cobb [6]. The evaluated angles are shown in Fig. 1. Prior to the study measurement, a training session was done for the three observers, using ten lateral X-rays and ten sagittal computed tomograms not from the study collective. In this session, the observers were made also confirm with the literature and conditions to attempt the vertebral, segmental and local kyphosis according to the method of Cobb [6]. Blinded to the history, diagnosis, and the patient identity, they each independently performed their two measurements on each X-ray and computed tomography at two different times using a radiographic marking pencil and a geometric protractor. Radiographic lines were completely erased with alcoholic pad before measurement by another observer. After the three observers had measured each X-ray and each sagittal computed tomography, the films were renumbered and redistributed 2 months after the first measurement for a new measure session. The interobserver reliability was attempted to the first measurement. The intraobserver measurement was attempted to the mean results of the first and second measurement.
Statistical analysis
For data evaluations, the program Excel® 2007 (Microsoft Corporation, Microsoft-Campus, Redmond, USA) was used. Complex calculations and the statistic evaluations were done using the statistic program SPSS® V11.0 (SPSS Inc, S. Wacker Drive, Chicago, USA). Owing to evaluation of constant parameters, the intraclass correlation coefficient (ICC) was attempted. The results between >0.8 were defined as excellent, between 0.6 and 0.8 as good, between 0.4 and 0.6 as moderate and <0.4 as bad correlation between two values. For each ICC, the 95% confidence interval was calculated. Differences between single ICCs were considered significant, if the lower and upper boundary of the 95% confidence intervals showed no overlapping. Differences (p values) between mean ICC values were calculated, using the paired Student’s t test. A p < 0.05 was defined as statistically significant.
Results
Thoracic burst fractures
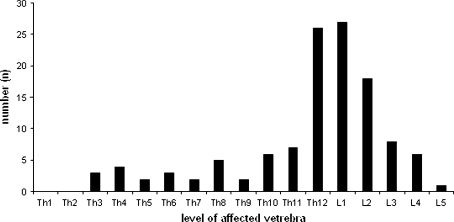
Sixty patients with thoracic burst fractures, 49 (81.7%) with male and 11 (18.3%) female gender, were evaluated. The mean age in this group was 33.4 ± 8.7 years (range 16.9–47.9 years, median 34.8 years). Most fractures were localized at the thoracolumbar junction. Details are shown in Fig. 2.
Fig. 2.
Number and level of the affected lumbar and thoracic vertebras
Interobserver reliability of the observers in thoracic burst fractures
The mean interobserver reliability was “excellent” in the segmental kyphosis in lateral X-ray (ICC = 0.826) and sagittal computed tomography (ICC = 0.824). For the vertebral kyphosis and local kyphosis, a “good” interobserver reliability could be measured in the X-rays (ICC = 0.779, 0.753) and an “excellent” interobserver reliability in the computed tomography (ICC = 0.802, 0.835). There were no significant differences between the three observers. Details are shown in Table 1.
Table 1.
Interobserver reliabilities of thoracic X-rays and computed tomography scans: intraclass correlation coefficient (ICC) and 95% confidence intervals
| A/B | A/C | C/B | |
|---|---|---|---|
| Interobserver reliabilities of X-rays in thoracic fractures | |||
| Vertebral kyphosis | 0.756 | 0.792 | 0.790 |
| Segmental kyphosis | 0.828 | 0.808 | 0.843 |
| Local kyphosis | 0.794 | 0.710 | 0.756 |
| Interobserver reliabilities of computed tomographies in thoracic fractures | |||
| Vertebral kyphosis | 0.878 | 0.709 | 0.818 |
| Segmental kyphosis | 0.849 | 0.801 | 0.823 |
| Local kyphosis | 0.864 | 0.808 | 0.834 |
Intraobserver reliability of the observers in thoracic burst fractures
The mean intraobserver reliability showed “excellent” results for the segmental kyphosis in X-rays and computed tomography (ICC = 0.802, 0.801). The mean intraobserver reliabilities for the vertebral and local kyphosis in the X-rays and computed tomography were “good” (ICC = 0.772, 0.776, 0.730, 0.760). There were no significant differences between the measurements of the three observers. Details are shown in Table 2.
Table 2.
Intraobserver reliabilities of thoracic X-rays and computed tomography scans: intraclass correlation coefficient (ICC) and 95% confidence intervals
| A | B | C | |
|---|---|---|---|
| Intraobserver reliabilities of X-rays in thoracic fractures | |||
| Vertebral kyphosis | 0.729 | 0.762 | 0.825 |
| Segmental kyphosis | 0.759 | 0.805 | 0.842 |
| Local kyphosis | 0.684 | 0.744 | 0.761 |
| Intraobserver reliabilities of computed tomographies in thoracic fractures | |||
| Vertebral kyphosis | 0.809 | 0.719 | 0.801 |
| Segmental kyphosis | 0.781 | 0.803 | 0.819 |
| Local kyphosis | 0.735 | 0.743 | 0.802 |
Differences regarding inter- and intraobserver reliability between X-rays and computed tomography scans in thoracic burst fractures
Statistical analysis showed a significantly higher interobserver reliability for the local kyphosis when measured on the basis of computed tomography scans than when measured solely with plain X-rays (p = 0.01). When measuring the vertebral and segmental kyphosis, the additional use of CT scans did not significantly improve interobserver reliability. Likewise, intraobserver reliability for the vertebral, segmental and local kyphosis was not improved when measured on the basis of CT scans Table 3.
Table 3.
Mean intra class correlation coefficients (ICC) for inter- and intraobserver reliabilities of X-rays and computed tomography scans of thoracic fractures and p values for differences between X-rays and CT scans
| X-rays of the thoracic fractures | Computed tomographies of the thoracic fractures | p value | |
|---|---|---|---|
| Mean inter-observer reliabilities | |||
| Vertebral kyphosis | 0.779 | 0.802 | 0.742 |
| Segmental kyphosis | 0.826 | 0.824 | 0.884 |
| Local kyphosis | 0.753 | 0.835 | 0.010 |
| Mean intraobserver reliabilities | |||
| Vertebral kyphosis | 0.772 | 0.776 | 0.920 |
| Segmental kyphosis | 0.802 | 0.801 | 0.946 |
| Local kyphosis | 0.730 | 0.760 | 0.197 |
Lumbar burst fractures
Sixty patients with lumbar burst fractures, 31 with male (51.7%) and 29 (48.3%) female gender, were evaluated. The mean age in this group was 27.6 ± 7.5 years (range 14.6–39.3 years, median 27.9 years). Most fractures were also located at the thoracolumbar junction. Details are shown in Fig. 2.
Interobserver reliability of the lumbar burst fractures
For the segmental kyphosis results showed “good” interobserver reliability in the X-rays (ICC = 0.790) and “excellent” interobserver reliability in the computed tomography (ICC = 0.874). For the vertebral and local kyphosis, “good” inter- and intraobserver reliabilities were seen in both film sets (ICC = 0.607, 0.704, 0.762, 0.763). There were no significant differences between the measurements of the three observers. Details are shown in Table 4.
Table 4.
Interobserver reliabilities of lumbar X-rays and computed tomographies: intraclass correlation coefficient (ICC) and 95% confidence intervals
| A/B | A/C | C/B | |
|---|---|---|---|
| Interobserver reliabilities of the X-rays in lumbar fractures | |||
| Vertebral kyphosis | 0.694 | 0.624 | 0.691 |
| Segmental kyphosis | 0.849 | 0.759 | 0.762 |
| Local kyphosis | 0.768 | 0.747 | 0.771 |
| Interobserver reliabilities of the computed tomographies in lumbar fractures | |||
| Vertebral kyphosis | 0.717 | 0.670 | 0.725 |
| Segmental kyphosis | 0.859 | 0.877 | 0.885 |
| Local kyphosis | 0.762 | 0.760 | 0.767 |
Intraobserver reliability of the observers in lumbar burst fractures
For the segmental kyphosis, the intraobserver reliability was also “excellent” in X-ray and computed tomography (ICC = 0.803, 0.835). The vertebral and local kyphosis showed “good” intraobserver reliability in both film sets (ICC = 0.685, 0.727, 0.751, 0.780). There were no significant differences between the measurements of the three observers (see Table 5).
Table 5.
Intraobserver reliabilities of the lumbar X-rays and computed tomographies: intraclass correlation coefficient (ICC) and 95% confidence intervals
| A | B | C | |
|---|---|---|---|
| Intraobserver reliabilities of the X-rays in lumbar fractures | |||
| Vertebrale kyphose | 0.656 | 0.688 | 0.710 |
| Segmentale kyphose | 0.826 | 0.787 | 0.795 |
| Lokale kyphose | 0.723 | 0.752 | 0.777 |
| Intraobserver reliabilities of the computed tomographies in lumbar fractures | |||
| Vertebral kyphosis | 0.685 | 0.765 | 0.731 |
| Segmental kyphosis | 0.828 | 0.809 | 0.869 |
| Local kyphosis | 0.789 | 0.771 | 0.781 |
Differences regarding inter- and intraobserver reliability between X-rays and computed tomography scans in lumbar burst fractures
Statistical analysis showed a significantly higher interobserver reliability for the vertebral kyphosis when measured on the basis of computed tomography scans than when measured solely with plain X-rays (p = 0.035). When measuring the local and segmental kyphosis, the additional use of CT scans did not significantly improve interobserver reliability. Intraobserver reliability for the vertebral, segmental and local kyphosis was not improved when classified on the basis of CT scans when compared with when classified with plain X-rays (see Table 6).
Table 6.
Mean intra class correlation coefficients (ICC) for inter- and intraobserver reliabilities of X-rays and computed tomography scans of lumbar fractures and p values for differences between X-rays and CT scans
| X-rays of the lumbar fractures | Computed tomographies of the lumbar fractures | p value | |
|---|---|---|---|
| Mean interobserver reliabilities | |||
| Vertebral kyphosis | 0.670 | 0.704 | 0.035 |
| Segmental kyphosis | 0.790 | 0.874 | 0.151 |
| Local kyphosis | 0.762 | 0.763 | 0.883 |
| Mean intraobserver reliabilities | |||
| Vertebral kyphosis | 0.685 | 0.727 | 0.137 |
| Segmental kyphosis | 0.803 | 0.835 | 0.267 |
| Local kyphosis | 0.751 | 0.780 | 0.253 |
Differences of inter- and intraobserver reliabilities between thoracic and lumbar fractures in conventional X-rays and computed tomographies
Statistical analysis showed significantly higher interobserver reliability for the local kyphosis in thoracic fractures compared with lumbar fractures when assessed on the basis of CT scans (p = 0.045). Furthermore, a significantly higher intraobserver reliability was found for the vertebral kyphosis in thoracic fractures compared with lumbar fractures when assessed on the basis of plain X-rays (p = 0.024). In contrast, no statistically significant differences were found between the interobserver reliabilities of thoracic and lumbar fractures for vertebral (p = 0.072), segmental (p = 0.351), and local (p = 0.685) kyphosis when assessed with plain X-rays and for vertebral (p = 0.11) and segmental (p = 0.133) kyphosis with CT scans. Likewise, statistical analysis showed no statistically significant differences regarding intraobserver reliabilities of thoracic and lumbar fractures for segmental (p = 0.986) and local (p = 0.152) kyphosis when assessed with plain X-rays and for vertebral (p = 0.429), segmental (p = 0.137), and local (p = 0.453) kyphosis when assessed on the basis of CT scans.
Discussion
The treatment of thoracic and lumbar fractures is also based on the posttraumatic degree of resultant kyphosis and vertebral height loss. Therefore, radiographs need to provide adequate information regarding the deformity to understand progression in kyphosis or scoliosis and to make adequate therapeutic decisions [4, 20, 32]. Various methods of measuring fracture kyphosis on lateral spine radiographs have been described [5, 17, 19, 23, 28]. The majority have been derived from the method of Cobb [6]. Generally, the Cobb angle [6] is the most widely used parameter for quantifying the severity of deformity curvatures [21, 28] and especially in measurement of thoracic kyphosis [4, 16]. The Cobb method was originally drawn down on anterior–posterior (ap) radiographs for evaluating scoliosis. The use of endplate lines [6] to construct the angles such as the kyphosis angle on lateral radiographs are often referred to as the “modified Cobb method”.
Critical comments about the method of Cobb [6] using in the evaluation of kyphosis are not new. However, various studies have reported a high variance and measurement error associated with the Cobb angle in obtaining kyphosis or lumbar lordosis measurements [4, 25, 27, 32]. This could be attributed to difficulty in identifying the margins of the endplate due to radiographic obstruction attributed to the ribs, the shoulder girdle, and/or inherent endplate irregularities associated with spinal deformity. Especially in measurement of osteoporotic compression fractures, the difficulties in identifying the endplates as a baseline for measurement could be a problem [16, 21]. The Cobb angle predominantly reflects endplate tilt of vertebrae between selected limits of the curve, and therefore may not reveal changes regionally within the curve, nor true intervertebral curvature relative to vertical. This limitation may become more problematic for patients with osteoporosis and especially for patients with a multisegmental fractured vertebral column, where vertebral deformities are common [3].
All studies about osteoporotic [3, 21], idiopathic [20, 32] or traumatic kyphosis [5, 17, 19, 23, 28, 31] dealing with the kyphosis angles according to the technique of Cobb [6], measure the angle in the conventional lateral X-ray.
Because computed tomography is performed on a lying patient, measurement of the kyphosis angles is probably not usual. However, in modern emergency management the whole body computed tomography is more and more common and conventional X-rays are not available in all cases before surgical procedures starts. Therefore, surgical indication in these cases will strongly be influenced only by computed tomography of the injured patient and its spine. Our study verified in computed tomography for thoracic and lumbar burst fractures “excellent” to “good” inter- and intraobserver reliabilities. Regarding both fracture localizations (thoracic and lumbar fractures) and both diagnostic work ups (X-rays and computed tomographies), the segmental kyphosis showed the best inter- and intraobserver reliabilities. Regarding both diagnostic work ups (X-rays and computed tomographies), significant differences could be evaluated for interobserver reliabilities of vertebral kyphosis measured in X-rays of lumbar fractures (p = 0.035) and interobserver reliabilities for local kyphosis, measured in X-rays of thoracic fractures (p = 0.010). Regarding both fracture localizations (thoracic and lumbar fractures), significant differences could alone be evaluated in interobserver reliabilities for the local kyphosis measured in computed tomographies (p = 0.045) and in intraobserver reliabilities for the vertebral kyphosis measured in X-rays (p = 0.024). All other measurements showed no statistical significant differences.
Findings in conventional X-rays
In conventional lateral X-ray, the measurement of vertebral, local and segmental kyphosis showed “good” to “excellent” inter- and intraobserver reliabilities. Therefore, in conventional lateral X-ray, these angles could be a helpful tool indicating surgical procedures.
Regarding our radiological findings, Seel et al. [28] and Kuklo et al. [19] showed comparable results: Kuklo et al. [19] evaluated five different measurement methods in conventional lateral X-rays for their reliability and reproducibility in thoracic and lumbar burst fractures, building the ICC coefficient. Therefore, 3 observers evaluated 50 lateral X-rays at two separate occasions. Method 1 (=local kyphosis) showed “excellent” results for the intraobserver (ICC = 0.83–0.94) and interobserver reliability (ICC = 0.81). Method 2 (=segmental kyphosis) showed “good” intraobserver reliabilities (ICC = 0.67–0.7) and “moderate” interobserver reliability (ICC = 0.59). Method 5 (=vertebral kyphosis) showed “good” and “excellent” intraobserver reliabilities (ICC = 0.73–0.85) and “good” interobserver reliability (0.71). Kuklo’s et al. [19] study was limited to lateral X-rays. The vertebral, segmental and local kyphosis were not evaluated in sagittal computed tomographies. Regarding this main difference to our study, further different study results are probably explained due to the smaller and different patient collective of Kuklo et al. [19]: he evaluated only 50 lateral X-rays and the collective included fractured vertebras from Th8 to L4. We observed 120 patients, in our study, with fracture levels from Th3 to L5.
Seel et al. [28] evaluated the inter- and intraobserver reliability of 3 different methods in 24 lateral X-rays of thoracic and lumbar fractures. Therefore, four observers measured with a special tool (Oxford-Cobbometer) the vertebral kyphosis (method 1), the angle between the inferior endplate of the vertebra above the index vertebra and the superior endplate of the vertebra below the index vertebra (method 2) and the kyphosis ratio at two different times. The vertebral kyphosis showed intraobserver reliabilities with “good” to “excellent” (ICC = 0.747–0.925) results and an “excellent” mean interobserver reliability (ICC = 0.939). However, method 2 showed better inter- and intraobserver reliability. Differences in our results may be explained using the Oxford-Cobbometer and the smaller patient collective. More details, which explains further result discrepancies, especially about fracture levels are not given by the author.
Studies of osteoporotic compression fractures with kyphosis of the vertebras show similar results to the cited results of traumatic kyphosis. Lee et al. [21] for example measured the vertebral kyphosis in 15 lateral X-rays of patients with osteoporotic fracture kyphosis. The correlation coefficient of the inter- and intraobserver reliability for the vertebral kyphosis was 0.71 (0.65–0.76).
Findings in computed tomographies
A direct comparison of our results in computed tomographies is only possible to one study, recently published by Street et al. [31]. The authors assessed the measurement reliability of plain X-rays, computed tomographies (CT) and magnetic resonance imaging (MRI) and their inter-modality agreement. Inter- and intraobserver reliability of the Cobb angle (=vertebral kyphosis), the Gardner segmental deformity angle (=segmental kyphosis) and the anterior body compression percentage in fractured vertebras of the thoracic–lumbar junction of ten patients were retrospectively evaluated by ten independent spine surgery fellowship-trained observers. The following results were found:
Inter- and intraobserver reliability of local kyphosis showed in computed tomography ICCs of 0.94739 and 0.98904 and in plane X-rays of 0.98234 and 0.99609. Inter- and intraobserver reliabilities of the segmental kyphosis revealed ICCs of 0.9499 and 0.98831 in computed tomography and ICCs of 0.97831 and 0.99548 in conventional X-rays. Therefore, all measurements in both diagnostic work ups showed “excellent” inter- and intraobserver reliabilities. Regardless of the imaging modality or the parameter being measured, the intraobserver reliability was statistically always better than the interobserver reliability. Plain X-rays had better overall inter- and intraobserver reliability followed by computed tomography and MRI. Reliability was very high in general with the highest reliability for intraobserver reliability of the linear measures on plain radiographs. The inter-modality agreement was highest for plain X-rays and computed tomography.
Differences between our results and the measurements of Street et al. [31] could be explained by the different study procedures: Street et al. [31] compared the results of 10 patients evaluated by 10 observers in contrast to our study protocol, which included 120 patients and 3 observers. Street et al. [31] evaluated fractures of the thoracolumbar junction. In our study, all thoracic and lumbar vertebras were included for measurement. The main difference between our actual study and the results published by Street et al. [31] is probably the use of digital images and digital measurement software. This software allows the examiner to provisionally mark only anatomical landmarks (e.g., corners of vertebral bodies) and end plates of the superior and inferior vertebrae of the kyphotic deformity. A magnification tool is used to ensure maximum accuracy of placement of the anatomical landmarks. After these lines are drawn, the software automatically generates and displays the lengths and angles formed bay these lines. In contrast to this digital measurement procedure in our study “handmade” measurements directly on the hard-copy films of computed tomographies and plain X-rays were done using only pencil and geometric protractor.
However, we agree with Street et al. [31], that also in sagittal computed tomography the use of the Cobb angle (measured as vertebral, segmental and local kyphosis in our study) seems to be generally possible in clinical practice and the inter-modality agreement suggests that measures by CT and plain X-ray my be clinically interchangeable. However, the exact correlation between the different diagnostic work ups should be evaluated in further studies.
Conclusion
“Good” to “excellent” inter- and intraobserver reliabilities for vertebral, segmental and local kyphosis in X-ray were evaluated. Therefore in lateral X-ray, the use of these angles could be a helpful tool, indicating surgical procedures. Regarding both fracture localizations (thoracic and lumbar fractures) and both diagnostic work ups (X-ray and computed tomography), the segmental kyphosis showed the best inter- and intraobserver reliabilities. Therefore, in practical use, we emphasize the determination of the segmental kyphosis, because of the highest reproducibility of this angle. “Good” to “excellent” inter- and intraobserver reliabilities for vertebral, segmental and local kyphosis could also be evaluated in computed tomographies. Therefore, also in computed tomographies, the use of these three angles seems to be generally possible. For a direct correlation of results in lateral X-ray and in computed tomography further studies should be done.
References
- 1.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and the thoracolumbar junction. Spine. 1989;14(7):717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Böhler J. Conservative treatment of thoracic and lumbar spinal fractures. Z Unfallmed Berufserkr. 1972;108:100–104. [PubMed] [Google Scholar]
- 3.Briggs AM, Wrigley TV, Tully EA, Adams PE, Greig AM, Bennell KL. Radiographic measures of thoracic kyphosis in osteoporosis: Cobb and vertebral centroid angles. Skeletal Radiol. 2007;36:761–767. doi: 10.1007/s00256-007-0284-8. [DOI] [PubMed] [Google Scholar]
- 4.Carman DL, Browne RH, Birch JG. Measurement of scoliosis and kyphosis radiographs. J Bone Joint Surg. 1990;72-A:328–333. [PubMed] [Google Scholar]
- 5.Chan DP, Seng NK, Kaan KT. Nonoperative treatment in burst fractures of the lumbar spine (L2–L5) without neurologic deficits. Spine. 1993;18:320–325. doi: 10.1097/00007632-199310000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Cobb JR. Outline for the study of scoliosis. American Academy of Orthopaedic Surgeons Instructional Course Lectures No. 5. Ann Arbor: JW Edwards; 1948. pp. 261–275. [Google Scholar]
- 7.Cowell HR. Radiographic measurements and clinical decisions. J Bone Joint Surg. 1990;72-A:319. [PubMed] [Google Scholar]
- 8.Dimar JR, 2nd, Carreon LY, Labelle H, Djurasovic M, Weidenbaum M, Brown C, Roussouly P. Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur Spine J. 2008;17(10):1373–1379. doi: 10.1007/s00586-008-0755-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eysel P, Hopf C, Füderer S. Kyphotic deformities in fractures of the thoracolumbar spine. Orthopäde. 2001;30:955–964. doi: 10.1007/s001320170009. [DOI] [PubMed] [Google Scholar]
- 10.Farcy JPC, Weidenbaum M, Glassman SD. Sagittal index in management of thoracolumbar burst fractures. Spine. 1990;15(9):958–965. doi: 10.1097/00007632-199009000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Gebhard F, Schultheiss M. Surgical treatment of fractures of the lumbar spine. In: Käfer W, Cakir B, Mattes T, Reichel H, editors. Orthopedic spine surgery. An instructional course book, chap 14. Darmstadt: Steinkopf; 2008. pp. 129–136. [Google Scholar]
- 12.Gelb DE, Lawrence GL, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asyptomatic middle and older aged volunteers. Spine. 1995;20(12):1351–1358. [PubMed] [Google Scholar]
- 13.Glayas P, Mac-Thiong JM, Parent S, Guise JA, Labelle H. Assessment of lumbosacral kyphosis in spondylolisthesis: a computer-assisted reliability study of six measurement techniques. Eur Spine J. 2009;18(2):212–217. doi: 10.1007/s00586-008-0818-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goultallier D, Louis R. Therapeutic indications in unstable fractures of the spine. Rev Chir Orthop Reparatrice Appar Mot. 1977;63(5):475–481. [PubMed] [Google Scholar]
- 15.Gstoettner M, Sekyra K, Walochnik N, Winter P, Wachter R, Bach CM. Inter- and intraobserver reliability assessment of the Cobb angle: manual versus digital measurement tools. Eur Spine J. 2007;16(10):1587–1592. doi: 10.1007/s00586-007-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrison DE, Harrison DD, Cailliet R, Janik TJ, Holland B. Radiographic analysis of lumbar lordosis. Centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine. 2006;26(11):E235–E242. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 17.Kaneda K, Abumi K, Fujiya M. Burst fractures with neurologic deficits of the thoracolumbar–lumbar spine. Spine. 1984;9:788–795. doi: 10.1097/00007632-198411000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Koller H, Acosta F, Hempfing A, Rohrmüller D, Tauber M, Lederer S, Resch H, Zenner J, Klampfer H, Schwiger R, Bogner R, Hitzl W. Long-term investigation of nonsurgical treatment for thoracolumbar and lumbar burst fractures: an outcome analysis in sight of spinopelvic balance. Eur Spine J. 2008;17:1073–1095. doi: 10.1007/s00586-008-0700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuklo TR, Polly DW, Owens BD, Zeidman SM, Chang AS, Klemme WR. Measurement of thoracic and lumbar burst fracture kyphosis. Spine. 2001;26(1):61–66. doi: 10.1097/00007632-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 20.Kuklo TR, Potter BK, O’Brien MF, Schroeder TM, Lenke LG, Polly DW., Jr Spinal Deformity Study Group. Reliability analysis for digital adolescent idiopathic scoliosis measurements. J Spinal Discord Tech. 2005;18(2):152–159. doi: 10.1097/01.bsd.0000148094.75219.b0. [DOI] [PubMed] [Google Scholar]
- 21.Lee SW, Hong JT, Son BC, Sung JH, Kim IS, Park CK. Analysis of accuracy of kyphotic angle measurement for vertebral osteoporotic compression fractures. J Clin Neurol. 2007;14:961–965. doi: 10.1016/j.jocn.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Mac-Thiong JM, Pinel-Giroux FM, Guise JA, Labelle H. Comparison between constrained and non-constrained Cobb techniques for the assessment of thoracic kyphosis and lumbar lordosis. Eur Spine J. 2007;16(9):1325–1331. doi: 10.1007/s00586-007-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McAffee PC, Yuan HA, Ladda NA. The unstable burst fracture. Spine. 1982;7:365–373. doi: 10.1097/00007632-198207000-00007. [DOI] [PubMed] [Google Scholar]
- 24.McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoraco-lumbar fractures. J Bone Joint Surg Am. 1993;75:162–169. doi: 10.2106/00004623-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Morrissy RT, Goldsmith GS, Hall EC, Kehl D, Cowie GH. Measurement of the Cobb angle on radiographs of patients who have scoliosis. Evaluation of intrinsic error. J Bone Joint Surg. 1990;72-A:320–327. [PubMed] [Google Scholar]
- 26.Pfeilschifter J et al (eds) (2006) Evidence based consensus guidelines for osteoporosis. Prophylaxis, diagnostic work-up and therapy for women at the menopause and men older than 60 years. Long version 2006. Insurance association of the German speaking sience communities of osteology (DVO). Schattauer, Stuttgart, pp 1–343
- 27.Polly DW, Kilkelly FX, McHale KA, Asplund LM, Mulligan M, Chang AS. Measurement of lumbar lordosis. Evaluation of intraobserver, interobserver, and technique variability. Spine. 1996;21(13):1530–1536. doi: 10.1097/00007632-199607010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Seel EH, Verrill CL, Metha RL, Davies EM. Measurement of fracture kyphosis with the Oxford Cobbometer. Intra- and interobserver reliabilities and comparison with other techniques. Spine. 2005;30(8):964–968. doi: 10.1097/01.brs.0000158952.43914.fb. [DOI] [PubMed] [Google Scholar]
- 29.Silber JS, Lipetz JS, Hayes VM, Lonner BS. Measurement variability in the assessment of sagittal alignment of the cervical spine: a comparison of the gore and the Cobb methods. J Spinal Discord Tech. 2004;17(4):301–305. doi: 10.1097/01.bsd.0000095824.98982.53. [DOI] [PubMed] [Google Scholar]
- 30.Stagnara P, Mauroy CD, Gonon GP, Costanzo G, Dimmet J, Pasquet A. Reciprocal Angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7(4):335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Street J, Lenehan B, Albietz J, Bishop P, Dvorak M, Fisher C. Intraobserver and interobserver reliability of measures of kyphosis in thoracolumbar fractures. Spine. 2009;9:464–469. doi: 10.1016/j.spinee.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 32.Stotts AK, Smith JT, Santora SD, Roach JW, Roach JW, D`Astous JL. Measurement of the spinal kyphosis: implications for the management of Scheuermann’s kyphosis. Spine. 2002;27(19):2143–2146. doi: 10.1097/00007632-200210010-00013. [DOI] [PubMed] [Google Scholar]
- 33.Tallroth K, Ylikoski M, Landtman M, Santavirta S. Reliability of radiological measurements of spondylolisthesis and extension-flexion radiographs of the lumbar spine. Eur J Radiol. 1994;18(3):227–231. doi: 10.1016/0720-048X(94)90341-7. [DOI] [PubMed] [Google Scholar]
- 34.Trojan E. Langfristige Ergebnisse von 200 Wirbelbrüchen der Brust/Lendenwirbelsäule ohne Lähmung. Z Unfallmed Berufserkr. 1972;2:122–134. [PubMed] [Google Scholar]
- 35.Zhang J, Lou E, Le LH, Hill D, Raso J, Wang Y. Computer-assisted Cobb angle measurement on posterior radiographs. Stud Health Technol Inform. 2008;140:151–156. [PubMed] [Google Scholar]