Abstract
Prevalent vertebral compression fracture(s) have been reported as having a negative impact on pain, disability, and quality of life. But no study has evaluated the effect of previous fracture on the course of acute compression fractures. The aim of the present study was to compare the natural course of the acute compression fracture in patients with (n = 51) and without (n = 56) previous vertebral compression fracture(s). The study is a retrospective analysis of a prospective cohort followed with postal questionnaires during a 12-month period after an acute fracture event. Eligible patients were those over 40 years of age, who were admitted to the emergency unit because of back pain and had an X-ray confirmed acute vertebral body fracture. A total of 107 patients were included in the study. The pain, disability (von Korff pain and disability scores), ADL (Hannover ADL score), and quality of life (QoL) (EQ-5D) were measured after 3 weeks, and 3, 6, and 12 months. The X-rays from the first visit to the emergency unit were evaluated. The difference of the scores between the groups with and without previous fracture was statistically significant (P < 0.05) at 3 weeks, 6 and 12 months for von Korff disability score, at all occasions for EQ-5D and at 3–12 months for Hannover ADL score, but only at 12 months for the von Korff pain intensity score. In both the groups all scores had improved in a statistically significant way at 3 months. The number of previous fractures was related to all the outcome scores in a statistically significant way (P < 0.05) except von Korff pain intensity score at 3 weeks and 3 months and von Korff disability score at 3 months. In conclusion, disability, ADL, and QoL scores, but not pain intensity score, were significantly worse in the patients with previous fracture from the fracture episode through the first 12 months. However, the improvements during the follow-up year seen in both groups were of a similar magnitude. The presence or absence of a previous fracture in an acutely fractured patient will influence the prognosis and thus possibly also the indications for treatments.
Keywords: Vertebral body fracture, Osteoporosis, Prevalent fracture, Quality of life, Disability, Treatment
Introduction
The vertebral compression fracture is one of the most common osteoporotic fractures [6]. Approximately 30–50% of women and 20–30% of men suffer at least one vertebral fracture during their lifetime and half of them will experience multiple fractures [39]. The impact of the fracture on pain, daily activities, and quality of life (QoL) has been poorly evaluated. In a recent study, the natural course of the acute vertebral compression fracture was followed during 1 year and it was shown that this fracture, with few exceptions, resulted in a severely painful condition that lasted at least for 1 year, deteriorating both back function and quality of life [48]. In spite of high prevalence of this type of fracture, little is known about the extent of the negative impact on the patient following the acute fracture.
Retrospective studies have reported that the type of fracture has no impact on the pain [25], whereas the location and grade of fracture deformity influence the QoL or severity of pain [7, 43, 47]. However, in a recent prospective study, it was found that the degree of the acute fracture deformation was an important factor in deciding the prognosis of pain as well as disability and QoL [49].
The prevalent fracture is defined as vertebral compression fracture(s) diagnosed from a single time point X-ray using morphological method not differentiating acute and previous fracture. Many prevalent fracture studies have reported that the number, level, and severity of a prevalent fracture had a negative impact on pain, disability, and QoL [5, 15, 27, 34, 35, 41]. The odds of impaired function, for example, were reported as 1.4 times higher in the presence of a single previous vertebral compression, and 3.1 times higher with two or more deformities [27]. Prevalent vertebral fractures have been found to be a strong predictor for the occurrence of a subsequent fracture [4, 10, 29, 32, 42]. It has been found that 19.2% of women with an acute fracture will experience a second one within 1 year and the relative risk of an incident fracture for the patients with one prevalent deformity was 3.2, 9.8 for 2, and 23.3 for 3 or more which could eventually contribute to the poor prognosis [7, 32, 37]. These findings make it reasonable to assume that the existence of a previous fracture might explain some of the differences in prognosis of pain, disability, and QoL seen in patients with an acute vertebral fracture. The aim of the present study was to compare the course of an acute vertebral compression fracture in aspects of pain, disability, QoL, and ADL in patients with and without previous vertebral compression fractures.
Materials and methods
All patients over 40 years of age who were admitted to the emergency unit at Sahlgrenska University Hospital, Gothenburg, Sweden because of back pain and had a radiologically confirmed acute vertebral fracture, which resulted from a low-energy trauma, were eligible for the study. Detailed methods have previously been described by Suzuki et al. [48]. In brief, eligible patients who suffered an acute vertebral compression fracture answered four different questionnaires (von Korff pain intensity and disability questionnaires, Hannover ADL score, and EQ-5D) at 3 weeks, and 3, 6, and 12 months after the acute fracture. The von Korff pain intensity score and disability score range between 0 and 100, where 0 refers to “no pain” and “no interference with activities”, while a score of 100 refers to “severe pain” and “unable to carry on any activities”, respectively [52, 53]. The Hannover ADL score, which focuses on musculoskeletal disorders, ranges from 0 (worst back function) to 100 (best back function) [30]. EQ-5D, which is a generic health-related quality of life measure, ranges between a negative value which indicates “worse than death” (death 0) and 1, which indicates “full health” [12, 13]. The X-ray taken at the initial visit was evaluated by a radiologist and later separately re-evaluated by two spine surgeons. The fracture acuteness was determined based on: (1) the existence of a fracture deformation compared with the normal neighboring vertebrae, (2) pain at or near the fracture deformation, (3) an evident sharp edge in the deformed region, and (4) no callus formation at the fractured vertebra [2]. In questionable cases, the previous or subsequent examinations were used, if available. Three osteoporotic fracture types, i.e. wedge, crush, and concave, have been described [37]. The grade of fracture deformation was evaluated by the semi-quantitative method presented by Genant [18–20].
Statistical analysis
All the data was entered and analyzed using the SPSS v. 14 the statistical analysis program. Both parametric (independent t test) and non-parametric (Mann–Whitney U test) tests were used for comparison of the scores derived from the questionnaires. For the analysis of overall differences between the groups during 1 year, repeated ANOVA was used. Nominal variables were tested using the Chi-square test. Pair-wise associations were tested using Pearson’s correlation coefficient test, when the data were on a continuous scale. For ordinal data, Spearman’s correlation coefficient test was used. All tests were two-sided. The results were considered to be significant at P < 0.05.
Results
Patient characteristics
The characteristics of the acute fracture patients with and without previous fracture(s) are shown in Table 1. Fifty-one (48%) patients had at least one previous compression fracture, while 56 (52%) patients had no previous fracture. No statistically significant differences were found between the two groups. However, it was a tendency of more severely deformed acute fractures among the patients having a previous fracture and likewise the percentage of patients with no recollection of trauma tended to be more frequent among the patients with previous fracture.
Table 1.
Baseline characteristics of the acute fractures patients with and without previous fracture. No statistically significant differences were found between the two groups
| Patient characteristics | No previous fracture | With previous fracture |
|---|---|---|
| Population | 56 | 51 |
| Age, mean ± SD (range) | 73.5 ± 11.9 (42–96) | 77.7 ± 11.6 (51–96) |
| Gender, female (%) | 37 (66) | 35 (69) |
| Acute fracture location | ||
| Thoracic spine | 28 (50%) | 30 (59%) |
| Lumbar spine | 28 (50%) | 21 (41%) |
| Type of fracture | ||
| Wedge | 40 (71%) | 34 (67%) |
| Concave | 10 (18%) | 10 (20%) |
| Crush | 6 (11%) | 7 (14%) |
| Grade of fracture deformation | ||
| Mild | 15 (27%) | 7 (14%) |
| Moderate | 26 (46%) | 24 (47%) |
| Severe | 15 (27%) | 20 (39%) |
| Kyphosis mean ± SD (degrees) | 42.7 (n = 21) | 44.2 (n = 26) |
| Lordosis mean ± SD (degrees) | 31.7 (n = 50) | 29.2 (n = 44) |
| Cause of trauma | ||
| A level fall | 36 (64%) | 26 (51%) |
| Lift of a heavy object | 1 (2%) | 1 (2%) |
| Some unidentified trauma | 0 (0%) | 2 (4%) |
| Traffic accident | 4 (7%) | 0 (0%) |
| No recollection of trauma | 15 (27%) | 22 (43%) |
| Time elapse before visit | ||
| Within first week | 36 (64%) | 36 (71%) |
| Within 1 month | 7 (13%) | 9 (17%) |
| Unidentified | 13 (23%) | 6 (12%) |
| Hospitalization or not | ||
| Immediate return home | 46 (82%) | 36 (71%) |
| Hospitalized | 10 (18%) | 13 (25%) |
| Nursing home | 0 (0%) | 2 (4%) |
| Hospital stay, days mean ± SD (range) | 16.7 ± 5.9 | 16.6 ± 9.7 |
Previous fracture characteristics and influence on the acute fracture
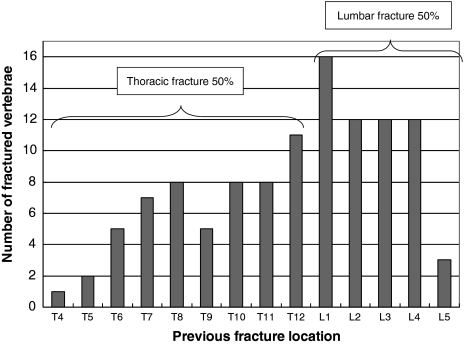
The characteristics of the previous fracture can be seen in Table 2 and their location can be seen in Fig. 1. No statistically significant relations between the existence of a previous fracture(s) and the acute fracture level, grade or type of acute fracture could be detected (P > 0.05). In patients with previous fracture(s) the acute fracture in 71% appeared as an adjacent fracture within two vertebrae from the previous one.
Table 2.
The characteristics of previous fracture
| Number of previous fracture (%) | |
| One | 27 (25) |
| Two | 9 (8) |
| Three | 3 (3) |
| Four | 6 (6) |
| Five | 5 (5) |
| Six | 1 (1) |
| Previous fracture location (% among the patients who had previous fracture) | |
| At least one previous fracture in thoracic spine | 34 (67) |
| At least one previous fracture in lumbar spine | 29 (57) |
| Thoracic spine only | 22 (43) |
| Lumbar spine only | 17 (33) |
| Both thoracic and lumbar spine | 12 (24) |
| The acute fracture as adjacent fracture (% among the patients who have previous fracture) | |
| Within one level | 23 (45) |
| Within two levels | 36 (71) |
Fig. 1.
Location of the previous fractures for the study population (total number of previous fractures 110)
Vertebral levels included in the X-ray examination
The X-ray examination did not include all levels of the thoracic and lumbar spines for all of the patients. The vertebral levels included in the examination can be seen in Table 3.
Table 3.
Vertebral levels included in the acute X-ray examination
| X-rayed level | Number of patients | Percent |
|---|---|---|
| L5–T1 | 37 | 34.6 |
| L5–T4 | 2 | 1.9 |
| L5–T5 | 2 | 1.9 |
| L5–T6 | 3 | 2.8 |
| L5–T7 | 15 | 14.0 |
| L5–T8 | 16 | 15.0 |
| L5–T9 | 19 | 17.8 |
| L5–T10 | 4 | 3.7 |
| L4–T1 | 4 | 3.7 |
| L3–T1 | 2 | 1.9 |
| L1–T1 | 2 | 1.9 |
| T12–T1 | 1 | 0.9 |
| Total | 107 | 100.0 |
Outcome differences between the patients with and without previous fracture
All the outcome measures, i.e. pain, disability, ADL, and QoL, improved between the 3 weeks and the 3 months follow-ups, both in the patients with and without any previous fracture(s). In patients with previous fracture(s), all scores were worse than the scores in the patients without previous fracture(s) (Table 4). The differences between the groups’ scores were significantly different at almost all follow-up occasions. The von Korff pain intensity score was nearly a complete exception in this respect. The initial scores in comparison with the scores after 12 months were worse among the patients having a previous fracture (P < 0.005). The von Korff pain intensity score was also an exception here with no difference between the initial and 12 months values (P > 0.05). When EQ-5D’s five dimensions (i.e. mobility, self-care, usual activity, pain/discomfort, and anxiety/depression) were analyzed separately and expressed as the percentage of the patients who had “no or light” problems versus “moderate or severe” problems, the proportion of the “moderate or severe” group was especially elevated (bad) for the mobility dimension (P < 0.01) among the patients with previous fractures at all the follow-up times (Table 5). For the pain/discomfort dimension, the proportion of “moderate or severe” problems was significantly different only at the 3- and 12-month follow-ups (P < 0.05).
Table 4.
Scores from the four questionnaires in patients with an acute fracture, with or without a previous fracture(s)
| Follow-up | No previous fracture (n = 56) (n = 54)a | Previous fracture (n = 51) (n = 47)a | Difference between previous and no previous fracture | |||
|---|---|---|---|---|---|---|
| Mean | Median | Mean | Median | P(para) | P(non-para) | |
| von Korff pain score | ||||||
| 3 weeks | 68.9 | 68.5 | 73.0 | 76.7 | NS | NS |
| 3 months | 59.3 | 63.3 | 63.8 | 70.0 | NS | NS |
| 6 months | 57.0 | 57.0 | 64.8 | 70.0 | NS | NS |
| 12 months | 56.5 | 60.0 | 64.9 | 70.0 | NS | 0.020 |
| von Korff disability score* | ||||||
| 3 weeks | 64.5 | 63.3 | 74.0 | 80.0 | 0.045 | 0.023 |
| 3 months | 53.5 | 51.5 | 59.7 | 63.0 | NS | NS |
| 6 months | 45.0 | 48.5 | 58.0 | 66.7 | 0.017 | 0.008 |
| 12 months | 48.4 | 48.5 | 60.3 | 67.0 | 0.030 | 0.009 |
| EQ-5D* | ||||||
| 3 weeks | 0.47 | 0.64 | 0.26 | 0.09 | 0.003 | 0.002 |
| 3 months | 0.57 | 0.69 | 0.47 | 0.62 | NS | 0.020 |
| 6 months | 0.63 | 0.69 | 0.45 | 0.62 | 0.006 | 0.003 |
| 12 months | 0.57 | 0.71 | 0.46 | 0.62 | NS | 0.008 |
| Hannover ADL score* | ||||||
| 3 weeks | 41.0 | 37.5 | 34.1 | 25.0 | NS | NS |
| 3 months | 53.9 | 52.0 | 41.5 | 41.7 | 0.009 | 0.013 |
| 6 months | 51.9 | 52.0 | 39.0 | 33.0 | 0.010 | 0.014 |
| 12 months | 53.9 | 54.0 | 40.6 | 33.3 | 0.008 | 0.019 |
NS not significant
aThe number of patients in the von Korff disability score analysis
* Significant over all difference between patients with and without previous fracture over 12 months (P < 0.05) by repeated ANOVA
P(para) indicates P value by parametric test (independent t test)
P(non-para) indicates P value by non-parametric test (Mann–Whitney test)
Table 5.
Percent of patients reporting moderate or severe problems in the five dimensions of EQ-5D at the four follow-up times
| EQ-5D dimensions | Follow-up time | Percent of patients who had moderate or severe problems | ||
|---|---|---|---|---|
| No previous fracture (n = 56) | Previous fracture (n = 51) | Difference* | ||
| Mobility | 3 weeks | 46.4 | 76.5 | 0.001 |
| 3 months | 37.5 | 70.6 | 0.001 | |
| 6 months | 35.7 | 64.7 | 0.003 | |
| 12 months | 35.7 | 74.5 | 0.001 | |
| Self-care | 3 weeks | 21.4 | 23.5 | NS |
| 3 months | 16.1 | 13.7 | NS | |
| 6 months | 16.1 | 11.8 | NS | |
| 12 months | 14.3 | 9.8 | NS | |
| Usual activities | 3 weeks | 78.6 | 86.3 | NS |
| 3 months | 60.7 | 78.4 | 0.047 | |
| 6 months | 66.1 | 72.5 | NS | |
| 12 months | 60.7 | 76.5 | NS | |
| Pain/discomfort | 3 weeks | 96.4 | 98.0 | NS |
| 3 months | 80.4 | 98.0 | 0.004 | |
| 6 months | 82.1 | 92.2 | NS | |
| 12 months | 82.1 | 96.1 | 0.023 | |
| Anxiety/depression | 3 weeks | 66.1 | 80.4 | NS |
| 3 months | 48.2 | 66.7 | NS | |
| 6 months | 44.6 | 60.8 | NS | |
| 12 months | 46.4 | 64.7 | NS | |
* Chi-square test
Subgroup analysis which might have influence on the questionnaire outcomes
Adjacent and non-adjacent acute fracture
Among the patients who had previous fracture(s) (51 patients), the acute fracture occurred within one vertebra from the previous fracture in 23 patients. In 36 patients (71%) the acute fracture occurred within two adjacent vertebrae from a previous fracture that was more frequent (P < 0.05) than the occurrence of an “non-adjacent” acute fracture (P < 0.05). There were, however, no differences in outcome when these two groups were compared.
Number of previous fractures and the outcome measures
With the exceptions of the von Korff pain intensity score at 3 weeks and 3 months and the von Korff disability score at 3 months, all the other scores were correlated to the number of previous fractures (Table 6).
Table 6.
Correlation between the number of previous fractures and the outcome measures
| Number of previous fracture(s) | Correlation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number (n = 56) (n = 54)a | One (n = 27) (n = 54)a | Two (n = 9) (n = 9)a | Three or more (n = 15) (n = 13)a | Outcomes and number of previous fracture | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | rbs | P | |
| von Korff pain intensity score | ||||||||||
| 3 weeks | 68.9 | 18.9 | 71.9 | 24.2 | 70.7 | 13.8 | 76.4 | 13.4 | 0.14 | NS |
| 3 months | 59.3 | 22.6 | 61.0 | 22.8 | 66.7 | 14.9 | 67.1 | 16.8 | 0.11 | NS |
| 6 months | 57.0 | 22.7 | 62.2 | 22.0 | 67.4 | 14.2 | 67.8 | 18.6 | 0.20 | 0.04 |
| 12 months | 56.5 | 23.4 | 65.4 | 21.5 | 67.9 | 16.7 | 62.0 | 26.0 | 0.21 | 0.03 |
| von Korff disability score | ||||||||||
| 3 weeks | 64.5 | 23.2 | 72.6 | 27.4 | 71.4 | 16.0 | 78.5 | 19.6 | 0.23 | 0.02 |
| 3 months | 53.5 | 26.6 | 55.2 | 25.1 | 62.6 | 18.0 | 66.2 | 25.1 | 0.16 | NS |
| 6 months | 45.0 | 29.0 | 53.5 | 24.8 | 63.8 | 18.8 | 62.8 | 26.0 | 0.28 | 0.01 |
| 12 months | 48.4 | 28.2 | 56.8 | 26.1 | 65.1 | 19.2 | 63.8 | 31.0 | 0.25 | 0.01 |
| EQ-5D | ||||||||||
| 3 weeks | 0.47 | 0.34 | 0.22 | 0.36 | 0.36 | 0.33 | 0.29 | 0.39 | −0.26 | 0.01 |
| 3 months | 0.57 | 0.38 | 0.53 | 0.28 | 0.41 | 0.32 | 0.39 | 0.36 | −0.24 | 0.01 |
| 6 months | 0.63 | 0.34 | 0.46 | 0.34 | 0.39 | 0.36 | 0.45 | 0.40 | −0.27 | 0.00 |
| 12 months | 0.57 | 0.39 | 0.48 | 0.35 | 0.31 | 0.29 | 0.51 | 0.43 | −0.22 | 0.02 |
| Hannover ADL score | ||||||||||
| 3 weeks | 41.0 | 21.8 | 36.7 | 24.1 | 34.7 | 15.3 | 29.0 | 21.6 | −0.22 | 0.03 |
| 3 months | 53.9 | 25.8 | 41.7 | 25.0 | 49.1 | 18.6 | 36.5 | 20.1 | −0.25 | 0.01 |
| 6 months | 51.9 | 29.0 | 39.6 | 24.1 | 39.3 | 20.6 | 37.8 | 17.8 | −0.23 | 0.01 |
| 12 months | 53.9 | 28.1 | 39.8 | 23.8 | 37.6 | 20.1 | 43.7 | 23.2 | −0.20 | 0.04 |
aNumber of patients for von Korff disability score analysis
brs Spearman correlation coefficient
Influence of spinal curvature on the outcome measures
A positive correlation (r = 0.54, P = 0.001) was found between the size of the thoracic kyphosis and the lumbar lordosis in the study population, but no correlations were noted between the size of thoracic kyphosis or the lumbar lordosis and any of the outcome measures.
Discussion
This study showed that the presence of one or more previous vertebral compression fractures added to the negative effect a subsequent acute fracture had on disability, QoL, and ADL, but not on the pain. The greater the number of previous fractures, the worse was the effect. As reported earlier, part of this finding can be explained by the fact that prevalent vertebral compression fractures worsen back pain [15, 17, 33, 40, 41, 43, 44] and QoL [23, 35, 46, 47, 51]. The number and severity of the prevalent fracture were especially related to the outcomes [15, 35, 43, 47, 51]. The most likely explanation for the worsening negative effect of a previous fracture is that the patients in this study who had a previous fracture(s) already were more disabled and had a lower QoL at the time when the subsequent acute fracture occurred. A less likely but possible explanation could be that the previous fracture(s) itself worsen the course of the acute fracture without lowering the scores before the time of the acute fracture event. The fact that the previous fracture’s effect on pain was less pronounced could coincide with the findings that the influence of an incident fracture on QoL and disability can last at least 5 years [22, 23, 27], while pain has been found to last somewhat shorter, i.e. 2–4 years [1, 24]. It is probable that, in this study, some of the previous fractures were so old that pain had started to decrease.
Incident fracture is defined as the fracture(s) diagnosed from series of radiographs taken at certain intervals and detecting vertebral shape changes using morphometrical methods. Cockerill and co-workers [8] reported that an incident fracture that happened as a new fracture during a mean period of 3.8 years, lowered QoL more than among the controls, irrespective of the presence or absence of a prevalent fracture. If, however, the incident fracture, in that study occurred as a first fracture episode, no differences were noted between the cases and controls, the last group including subjects both with and without a prevalent fracture(s) [8]. This suggests that it was the second fracture which resulted in the long lasting (>3 years) deterioration of QoL. Furthermore, several earlier studies have shown that the number of previous fractures, especially “moderately” and “severely deformed” previous fractures were related to impaired QoL [35, 36] as well as pain and disability [15, 24, 39]. These results are consistent with the findings in the present study, where relationships were found between the number of previous fractures and impaired QoL, disability, and ADL only.
In the present study, it was evident that the 1 year course of QoL, disability, and ADL was very similar, although on different levels of disturbance for those with and without a previous fracture(s). This suggests that the effect of the acute fracture per se was equally bad in both the patients with and without previous fracture. An extended follow-up period, longer than 1 year after the acute fracture in patients with and without a previous fracture(s), is needed in order to better understand the confounding effect of a previous fracture. This could reveal, for example, the possible finding of an earlier recovery among those patients without a previous fracture(s).
Influence of fracture location
The acute fracture occurring within two vertebral levels from previous fracture(s) was significantly frequent in this study, however, an observation made also in an earlier study [32]. On the contrary, Davis et al. [10] found that a prevalent fracture deformity increased the risk of a subsequent deformity at vertebrae distant from the initial deformity. A reason for the discrepancy could be that the fractures in that study were categorized into three distinct regions of the spine, not as in the current study as adjacent or not adjacent.
In patients with a previous fracture, the influence of an adjacent acute fracture on pain, disability, and QoL has not been settled. A negative influence of an adjacent fracture has been noted in one study [7], but not in the others [35, 47]. The present study could not detect any negative effects of an adjacent fracture within one or two vertebrae.
The analysis of the influence of the location of the previous fracture(s) indicated more negative effect when the previous fracture(s) were located in the thoracic, rather than in the lumbar spine in this study. This finding is contradictory to the results from previous studies [7, 35, 47]. However, this finding must be cautiously interpreted because some of the most proximal thoracic levels were not included in the radiographic examination in the present study (see Table 3).
Influence of kyphosis and lordosis
The relation between kyphosis and back pain or disability is controversial. Some authors have shown a correlation between the size of the kyphosis and pain or disability [17, 31, 43, 45]. This study and also others could not detect any such correlation [3, 16]. It has been shown earlier that the size of the kyphosis is multi-factorial [9, 11, 14, 16, 28, 38, 50]. The present findings suggested that even severe or multiple fracture deformities in at least a few vertebrae had limited effects on the kyphosis.
The finding of a relation between kyphosis and lordosis indicated a compensatory mechanism to maintain sagital spinal imbalance [26].
Reasons for the negative effect of the previous fracture
The reason for the previous fracture’s negative influence on the subsequent acute fracture is not clear. Several possible explanations have been suggested. It is not unlikely that during the subsequent year, perhaps even sub-clinical, new compression fractures could occur. Rao and co-workers [37] have indicated such a possibility. They reported that 19.2% of the women with a confirmed incidental fracture had a second fracture within 1 year [37]. It has also been shown that the relative risk of an incident vertebral fracture increases depending on the number, the level (greatest at T5–T7 and L1–L3), and the severity of the previous fracture [32]. In the present study, the finding that the mobility dimension of the EQ-5D, in particular, had a high inclusion of patients with “moderate or severe” problems when moving (Table 5), could be one explanation for an increased fracture risk. Hindered motion and physical activity due to severe pain is likely to accelerate bone mineral losses and thus add to the already manifested bone fragility. Another explanation might be fear, i.e. fear of falling and sustaining a new fracture. It has been found that fear of falling or depression is adversely affected by a pre-existing vertebral fracture(s) [21]. This could correspond to the tendency of an elevated anxiety/depression dimension of EQ-5D to some extent among the patients with a previous fracture in the present study (Table 5).
Conclusion
Patients with an acute vertebral compression fracture, who also had a history of a previous fracture(s), had poorer outcomes in terms of disability, QoL and ADL, but not pain, than the patients without a previous fracture(s), despite the fact that the natural course of healing on these outcomes was similar in both groups. The previous fracture(s) worsened the outcomes from the beginning and continued up to at least 1 year. Therefore, for the prognosis and indication of treatments such as kyphoplasty or vertebroplasty, the influences of a previous fracture(s) should be considered.
Acknowledgments
The study was supported by grants from The Swedish Council for Working Life and Social Research, AFA Insurance, Sahlgrenska academy at Gothenburg University. The study was made possible through the cooperation with the Department of Orthopaedic Surgery, Nagoya City University, Nagoya Japan and its chairman professor Takanobu Otsuka.
References
- 1.Begerow B, Pfeifer M, Pospeschill M, Scholz M, Schlotthauer T, Lazarescu A, Pollaehne W, Minne HW. Time since vertebral fracture: an important variable concerning quality of life in patients with postmenopausal osteoporosis. Osteoporos Int. 1999;10:26–33. doi: 10.1007/s001980050190. [DOI] [PubMed] [Google Scholar]
- 2.Bengner U, Johnell O, Redlund-Johnell I. Changes in incidence and prevalence of vertebral fractures during 30 years. Calcif Tissue Int. 1988;42:293–296. doi: 10.1007/BF02556362. [DOI] [PubMed] [Google Scholar]
- 3.Bergenudd H, Nilsson B, Uden A, Willner S. Bone mineral content, gender, body posture, and build in relation to back pain in middle age. Spine. 1989;14:577–579. doi: 10.1097/00007632-198906000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of osteoporotic fractures research group. J Bone Miner Res. 1999;14:821–828. doi: 10.1359/jbmr.1999.14.5.821. [DOI] [PubMed] [Google Scholar]
- 5.Burger H, Daele PL, Grashuis K, Hofman A, Grobbee DE, Schutte HE, Birkenhager JC, Pols HA. Vertebral deformities and functional impairment in men and women. J Bone Miner Res. 1997;12:152–157. doi: 10.1359/jbmr.1997.12.1.152. [DOI] [PubMed] [Google Scholar]
- 6.Chrischilles EA, Butler CD, Davis CS, Wallace RB. A model of lifetime osteoporosis impact. Arch Intern Med. 1991;151:2026–2032. doi: 10.1001/archinte.151.10.2026. [DOI] [PubMed] [Google Scholar]
- 7.Cockerill W, Ismail AA, Cooper C, Matthis C, Raspe H, Silman AJ, O’Neill TW. Does location of vertebral deformity within the spine influence back pain and disability? European vertebral osteoporosis study (EVOS) group. Ann Rheum Dis. 2000;59:368–371. doi: 10.1136/ard.59.5.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cockerill W, Lunt M, Silman AJ, Cooper C, Lips P, Bhalla AK, Cannata JB, Eastell R, Felsenberg D, Gennari C, Johnell O, Kanis JA, Kiss C, Masaryk P, Naves M, Poor G, Raspe H, Reid DM, Reeve J, Stepan J, Todd C, Woolf AD, O’Neill TW. Health-related quality of life and radiographic vertebral fracture. Osteoporos Int. 2004;15:113–119. doi: 10.1007/s00198-003-1547-4. [DOI] [PubMed] [Google Scholar]
- 9.Cortet B, Roches E, Logier R, Houvenagel E, Gaydier-Souquieres G, Puisieux F, Delcambre B. Evaluation of spinal curvatures after a recent osteoporotic vertebral fracture. Joint Bone Spine. 2002;69:201–208. doi: 10.1016/S1297-319X(02)00381-0. [DOI] [PubMed] [Google Scholar]
- 10.Davis JW, Grove JS, Wasnich RD, Ross PD. Spatial relationships between prevalent and incident spine fractures. Bone. 1999;24:261–264. doi: 10.1016/S8756-3282(98)00176-8. [DOI] [PubMed] [Google Scholar]
- 11.Smet AA, Robinson RG, Johnson BE, Lukert BP. Spinal compression fractures in osteoporotic women: patterns and relationship to hyperkyphosis. Radiology. 1988;166:497–500. doi: 10.1148/radiology.166.2.3336728. [DOI] [PubMed] [Google Scholar]
- 12.Dolan P, Gudex C, Kind P, Williams A. The time trade-off method: results from a general population study. Health Econ. 1996;5:141–154. doi: 10.1002/(SICI)1099-1050(199603)5:2<141::AID-HEC189>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 13.Dolan P, Gudex C, Kind P, Williams A. Valuing health states: a comparison of methods. J Health Econ. 1996;15:209–231. doi: 10.1016/0167-6296(95)00038-0. [DOI] [PubMed] [Google Scholar]
- 14.Ensrud KE, Black DM, Harris F, Ettinger B, Cummings SR. Correlates of kyphosis in older women. The fracture intervention trial research group. J Am Geriatr Soc. 1997;45:682–687. doi: 10.1111/j.1532-5415.1997.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 15.Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK. Contribution of vertebral deformities to chronic back pain and disability. The study of osteoporotic fractures research group. J Bone Miner Res. 1992;7:449–456. doi: 10.1002/jbmr.5650070413. [DOI] [PubMed] [Google Scholar]
- 16.Ettinger B, Black DM, Palermo L, Nevitt MC, Melnikoff S, Cummings SR. Kyphosis in older women and its relation to back pain, disability and osteopenia: the study of osteoporotic fractures. Osteoporos Int. 1994;4:55–60. doi: 10.1007/BF02352262. [DOI] [PubMed] [Google Scholar]
- 17.Finsen V. Osteoporosis and back pain among the elderly. Acta Med Scand. 1988;223:443–449. doi: 10.1111/j.0954-6820.1988.tb15896.x. [DOI] [PubMed] [Google Scholar]
- 18.Genant HK, Jergas M. Assessment of prevalent and incident vertebral fractures in osteoporosis research. Osteoporos Int. 2003;14(Suppl 3):S43–S55. doi: 10.1007/s00198-002-1348-1. [DOI] [PubMed] [Google Scholar]
- 19.Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR. Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The study of osteoporotic fractures research group. J Bone Miner Res. 1996;11:984–996. doi: 10.1002/jbmr.5650110716. [DOI] [PubMed] [Google Scholar]
- 20.Genant HK, Wu CY, Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 21.Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone. 1996;18:185S–189S. doi: 10.1016/8756-3282(95)00500-5. [DOI] [PubMed] [Google Scholar]
- 22.Greendale GA, Barrett-Connor E, Ingles S, Haile R. Late physical and functional effects of osteoporotic fracture in women: the Rancho Bernardo study. J Am Geriatr Soc. 1995;43:955–961. doi: 10.1111/j.1532-5415.1995.tb05557.x. [DOI] [PubMed] [Google Scholar]
- 23.Hall SE, Criddle RA, Comito TL, Prince RL. A case–control study of quality of life and functional impairment in women with long-standing vertebral osteoporotic fracture. Osteoporos Int. 1999;9:508–515. doi: 10.1007/s001980050178. [DOI] [PubMed] [Google Scholar]
- 24.Huang C, Ross PD, Wasnich RD. Vertebral fractures and other predictors of back pain among older women. J Bone Miner Res. 1996;11:1026–1032. doi: 10.1002/jbmr.5650110721. [DOI] [PubMed] [Google Scholar]
- 25.Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, O’Neill TW. Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European vertebral osteoporosis study group. Osteoporos Int. 1999;9:206–213. doi: 10.1007/s001980050138. [DOI] [PubMed] [Google Scholar]
- 26.Itoi E. Roentgenographic analysis of posture in spinal osteoporotics. Spine. 1991;16:750–756. doi: 10.1097/00007632-199107000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Jinbayashi H, Aoyagi K, Ross PD, Ito M, Shindo H, Takemoto T. Prevalence of vertebral deformity and its associations with physical impairment among Japanese women: the Hizen–Oshima study. Osteoporos Int. 2002;13:723–730. doi: 10.1007/s001980200099. [DOI] [PubMed] [Google Scholar]
- 28.Kalliomaki JL, Siltavuori L, Virtama P. Stature and aging. J Am Geriatr Soc. 1973;21:504–506. doi: 10.1111/j.1532-5415.1973.tb01651.x. [DOI] [PubMed] [Google Scholar]
- 29.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 30.Kohlmann T, Raspe H. Hannover functional questionnaire in ambulatory diagnosis of functional disability caused by backache. Rehabilitation (Stuttg) 1996;35:I–VIII. [PubMed] [Google Scholar]
- 31.Leidig G, Minne HW, Sauer P, Wuster C, Wuster J, Lojen M, Raue F, Ziegler R. A study of complaints and their relation to vertebral destruction in patients with osteoporosis. Bone Miner. 1990;8:217–229. doi: 10.1016/0169-6009(90)90107-Q. [DOI] [PubMed] [Google Scholar]
- 32.Lunt M, O’Neill TW, Felsenberg D, Reeve J, Kanis JA, Cooper C, Silman AJ. Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: results from the European Prospective Osteoporosis Study (EPOS) Bone. 2003;33:505–513. doi: 10.1016/S8756-3282(03)00248-5. [DOI] [PubMed] [Google Scholar]
- 33.Lyles KW, Gold DT, Shipp KM, Pieper CF, Martinez S, Mulhausen PL. Association of osteoporotic vertebral compression fractures with impaired functional status. Am J Med. 1993;94:595–601. doi: 10.1016/0002-9343(93)90210-G. [DOI] [PubMed] [Google Scholar]
- 34.Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, Segal M, Genant HK, Cummings SR. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 35.Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15:1384–1392. doi: 10.1359/jbmr.2000.15.7.1384. [DOI] [PubMed] [Google Scholar]
- 36.Randell AG, Bhalerao N, Nguyen TV, Sambrook PN, Eisman JA, Silverman SL. Quality of life in osteoporosis: reliability, consistency, and validity of the osteoporosis assessment questionnaire. J Rheumatol. 1998;25:1171–1179. [PubMed] [Google Scholar]
- 37.Rao RD, Singrakhia MD. Painful osteoporotic vertebral fracture. Pathogenesis, evaluation, and roles of vertebroplasty and kyphoplasty in its management. J Bone Joint Surg Am. 2003;85-A:2010–2022. [PubMed] [Google Scholar]
- 38.Resnick D. Degenerative diseases of the vertebral column. Radiology. 1985;156:3–14. doi: 10.1148/radiology.156.1.3923556. [DOI] [PubMed] [Google Scholar]
- 39.Ross PD. Clinical consequences of vertebral fractures. Am J Med. 1997;103:30S–42S. doi: 10.1016/S0002-9343(97)90025-5. [DOI] [PubMed] [Google Scholar]
- 40.Ross PD, Davis JW, Epstein RS, Wasnich RD. Pain and disability associated with new vertebral fractures and other spinal conditions. J Clin Epidemiol. 1994;47:231–239. doi: 10.1016/0895-4356(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 41.Ross PD, Ettinger B, Davis JW, Melton LJ, 3rd, Wasnich RD. Evaluation of adverse health outcomes associated with vertebral fractures. Osteoporos Int. 1991;1:134–140. doi: 10.1007/BF01625442. [DOI] [PubMed] [Google Scholar]
- 42.Ross PD, Genant HK, Davis JW, Miller PD, Wasnich RD. Predicting vertebral fracture incidence from prevalent fractures and bone density among non-black, osteoporotic women. Osteoporos Int. 1993;3:120–126. doi: 10.1007/BF01623272. [DOI] [PubMed] [Google Scholar]
- 43.Ryan PJ, Blake G, Herd R, Fogelman I. A clinical profile of back pain and disability in patients with spinal osteoporosis. Bone. 1994;15:27–30. doi: 10.1016/8756-3282(94)90887-7. [DOI] [PubMed] [Google Scholar]
- 44.Ryan PJ, Evans P, Gibson T, Fogelman I. Osteoporosis and chronic back pain: a study with single-photon emission computed tomography bone scintigraphy. J Bone Miner Res. 1992;7:1455–1460. doi: 10.1002/jbmr.5650071213. [DOI] [PubMed] [Google Scholar]
- 45.Ryan SD, Fried LP. The impact of kyphosis on daily functioning. J Am Geriatr Soc. 1997;45:1479–1486. doi: 10.1111/j.1532-5415.1997.tb03199.x. [DOI] [PubMed] [Google Scholar]
- 46.Salaffi F, Cimmino MA, Malavolta N, Carotti M, Di Matteo L, Scendoni P, Grassi W. The burden of prevalent fractures on health-related quality of life in postmenopausal women with osteoporosis: the IMOF study. J Rheumatol. 2007;34:1551–1560. [PubMed] [Google Scholar]
- 47.Silverman SL, Minshall ME, Shen W, Harper KD, Xie S. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the multiple outcomes of raloxifene evaluation study. Arthritis Rheum. 2001;44:2611–2619. doi: 10.1002/1529-0131(200111)44:11<2611::AID-ART441>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 48.Suzuki N, Ogikubo O, Hansson T. The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months. Eur Spine J. 2008;17:1380–1390. doi: 10.1007/s00586-008-0753-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suzuki N, Ogikubo O, Hansson T. The prognosis for pain, disability, activities of daily living and quality of life after an acute osteoporotic vertebral body fracture: its relation to fracture level, type of fracture and grade of fracture deformation. Eur Spine J. 2009;18:77–88. doi: 10.1007/s00586-008-0847-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Twomey L, Taylor J. Age changes in lumbar intervertebral discs. Acta Orthop Scand. 1985;56:496–499. doi: 10.3109/17453678508993043. [DOI] [PubMed] [Google Scholar]
- 51.Schoor NM, Ewing SK, O’Neill TW, Lunt M, Smit JH, Lips P. Impact of prevalent and incident vertebral fractures on utility: results from a patient-based and a population-based sample. Qual Life Res. 2008;17:159–167. doi: 10.1007/s11136-007-9287-0. [DOI] [PubMed] [Google Scholar]
- 52.Korff M, Deyo RA, Cherkin D, Barlow W. Back pain in primary care. Outcomes at 1 year. Spine. 1993;18:855–862. doi: 10.1097/00007632-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 53.Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–149. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]