Abstract
The correction of severe post-tubercular kyphosis (PTK) is complex and has the disadvantage of being multiple staged with a high morbidity. Here, we describe the procedure and results of closing–opening osteotomy for correction of PTK which shortens the posterior column and opens the anterior column appropriately to correct the deformity without altering the length of the spinal cord. Seventeen patients with PTK (10 males; 7 females) with an average age of 18.3 ± 10.6 years (range 4–40 years) formed the study group. There were ten thoracolumbar, one lumbar and six thoracic deformities. The number of vertebrae involved ranged from 2 to 5 (average 2.8). Preoperative kyphosis averaged 69.2° ± 25.1° (range 42°–104°) which included ten patients with deformity greater than 60°. The average vertebral body loss was 2.01 ± 0.79 (range 1.1–4.1). The neurological status was normal in 13 patients, Frankel’s grade D in three patients and grade C in one. Posterior stabilization with pedicle screw instrumentation was followed by a preoperatively calculated wedge resection. Anterior column reconstruction was performed using rib grafts in four, tricortical iliac bone graft in five, cages in six, and bone chips alone and fibular graft in one patient each. Average operating time was 280 min (200–340 min) with an average blood loss of 820 ml (range 500–1,600 ml). The postoperative kyphosis averaged 32.4° ± 19.5° (range 8°–62°). The percentage correction of kyphosis achieved was 56.8 ± 14.6% (range 32–83%). No patient with normal preoperative neurological status showed deterioration in neurology after surgery. The last follow-up was at an average of 43 ± 4 months (range 32–64 months). The average loss of correction at the last follow-up was 5.4° (range 3°–9°). At the last follow-up, the mean preoperative pain visual analogue scale score decreased significantly from 9.2 (range 8–10 points) to 1.5 (range 1–2 points). There was also a significant decrease in mean preoperative Oswestry’s Disability Index from 56.4 (range 46–68) to 10.6 (range 6–15). Complications were superficial wound infections in two, neurological deterioration in one, temporary jaundice in one and implant failure requiring revision in one. Single-stage closing–opening wedge osteotomy is an effective method to correct severe PTK. The procedure has the advantage of being a posterior only, single-stage correction, which allows for significant correction with minimal complications.
Keywords: Tuberculosis, Kyphosis, Closing–opening wedge, Osteotomy
Introduction
The incidence of tuberculosis is on the rise in both the developed and developing world [41, 43]. More than 30 million people worldwide suffer from overt tuberculosis and more than two million have the active, spinal form [31]. The advent of effective antituberculous chemotherapy has largely made uncomplicated spinal tuberculosis a medical disease [20, 22–24]. Although complete disease cure may be achieved with chemotherapy, patients treated conservatively have an average increase of 15° in deformity [21, 25] and 3–5% of the patients end up with a deformity greater than 60° [23, 24, 37].
A severe kyphosis is a major cosmetic and psychological disturbance in a growing child and can result in costopelvic impingement, secondary cardiorespiratory problems and late-onset neurological deficits [37, 38]. Patients with kyphosis who present with persistent pain, neurological deficit, functional disability or cosmetic problems will require surgical correction of the deformity.
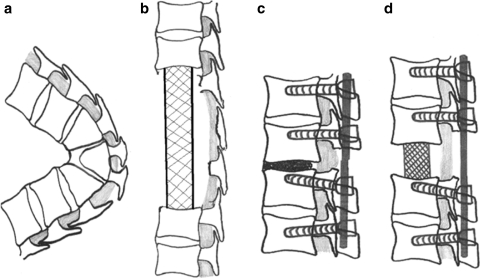
Kyphotic deformities are traditionally corrected by an anterior instrumented fusion [2, 45], a combined anterior–posterior procedure [1, 7, 18, 35] or a posterior procedure only [3, 8, 13, 34], each having its advantages and disadvantages. Anterior procedures are associated with difficulties in approaching the concavity of the angular kyphosis in the deformities greater than 60° [17]. The incidence of coexistent pulmonary tuberculosis is about 15% and anterior approach is complicated by problems of fibrosis and adhesions. In severe childhood disease, 2–3 vertebral bodies are frequently destroyed causing a severe shortening of the anterior column with sparing of the posterior column causing a disparity in column height (Fig. 1a). Correction of this deformity by purely opening up the anterior column can give rise to severe stretching of the spinal cord with risks of neurological deficits (Fig. 1b). Combined anterior and posterior procedures are a major surgical undertaking irrespective of whether it is performed as single or two-staged procedure. Increased treatment cost of an anterior and posterior procedure can also be a significant factor as many of these patients are from the poor socioeconomic status.
Fig. 1.
Surgical options in correction of severe post-tuberculosis kyphotic deformities. a In healed tuberculosis, there is severe shortening of the anterior column with a relatively normal posterior column. The fusion mass is usually slightly retropulsed and causes indentation of the dura. There may be surrounding peridural fibrosis and the exiting nerve roots are crowded at the level of the fusion mass. b Correction of kyphosis by opening up the kyphosis and restoring the anterior column height has the problem of causing stretching of the cord. c Correction by a pure closing wedge osteotomy by posterior column shortening can result in kinking and herniation of the cord through the laminectomy defect. d An osteotomy that shortens the posterior column and opens up the anterior column appropriately can restore the sagittal alignment without either undue elongation or shortening of the cord
Posterior closing osteotomy (which shortens the posterior column) has been used effectively to correct posttraumatic kyphosis, and kyphosis secondary to osteoporosis and ankylosing spondylitis [30, 32, 33, 40]. However, tuberculosis is different from the above conditions in that the loss of the anterior column can be as much as three complete vertebral bodies. A pure closing wedge osteotomy would result in severe kinking of the cord leading to neurological compromise (Fig. 1c). An osteotomy that achieves correction without altering the length of the cord would be the ideal procedure [15] (Fig. 1d). We describe a closing–opening osteotomy for post-tubercular deformity that shortens the posterior column and opens the anterior column appropriately to correct the deformity without compromising the spinal cord.
Patients and methods
Seventeen patients with healed post-tubercular kyphotic deformity formed the study group (Table 1). All patients had a history of childhood spinal tuberculosis and were treated by ambulatory chemotherapy. Patients presented on an average of 5.9 ± 4.2 years (range 1–12 years) after the completion of antituberculous chemotherapy. The indications for surgery were persistent back pain (n = 4), progressive deformity (n = 9) and new onset neurological deficits (n = 4). The neurological status was normal in 12 patients, Frankel D in three patients and Frankel C in two patients [11].
Table 1.
Clinical data of patients and outcome
| Serial no. | Age/sex | Destroyed vertebrae | Vertebral body loss | Number of bodies involved | Deformity (°) | Correction obtained | Neurology (Frankel) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Immediate postoperative | Angle | Percentage | Preoperative | Postoperative | |||||
| 1. | 21/F | T12–L1 | 1.4 | 2 | 46 | 8 | 38 | 83 | E | E |
| 2. | 12/F | T11–T12 | 1.2 | 2 | 43 | 18 | 25 | 58 | E | E |
| 3. | 32/M | T10–T11 | 1.6 | 2 | 42 | 12 | 30 | 71 | E | E |
| 4. | 16/F | T4–T6 | 2.3 | 3 | 100 | 61 | 39 | 39 | C | A |
| 5. | 11/M | T6–T7 | 1.1 | 2 | 47 | 15 | 32 | 68 | E | E |
| 6. | 16/M | T11–L3 | 3.1 | 5 | 93 | 52 | 41 | 44 | D | E |
| 7. | 14/M | T6–T10 | 2.9 | 5 | 74 | 35 | 39 | 53 | C | D |
| 8. | 21/M | T11–T12 | 1.4 | 2 | 45 | 10 | 35 | 77 | E | E |
| 9. | 12/F | T10–T11 | 1.6 | 2 | 47 | 18 | 29 | 62 | E | E |
| 10. | 8/M | T2–T4 | 2.8 | 3 | 104 | 52 | 52 | 50 | E | E |
| 11. | 7/M | T4–T7 | 4.1 | 4 | 96 | 51 | 45 | 47 | E | E |
| 12. | 4/F | T11–T12 | 1.8 | 2 | 48 | 16 | 32 | 66 | E | E |
| 13. | 11/M | T9–T11 | 1.6 | 3 | 80 | 38 | 42 | 52 | C | E |
| 14. | 40/M | T10–T12 | 1.6 | 3 | 102 | 48 | 54 | 53 | E | E |
| 15. | 23/F | T12–L2 | 1.9 | 3 | 64 | 44 | 20 | 32 | E | E |
| 16. | 26/ F | T8 | 1.7 | 2 | 46 | 12 | 34 | 73 | E | E |
| 17. | 38/M | T11–12 | 2.2 | 3 | 100 | 62 | 38 | 38 | C | E |
There were ten males and seven females with an average age of 18.3 ± 10.6 years (range 4–40 years). There were ten thoracolumbar, one lumbar and six thoracic deformities. The number of vertebrae involved in the fusion mass ranged from 2 to 5. The angle of deformity was measured by projecting lines from the upper border of the first healthy vertebra above and the lower border of the first healthy vertebra below the diseased area [28]. Preoperative kyphosis averaged 69.2° ± 25.1° (range 42°–104°) which included ten patients with deformity greater than 60°. The vertebral body loss was calculated on lateral radiograph by measuring the percentage loss in each vertebral body and then adding them up [28]. The average vertebral body loss was 2.01 ± 0.79 (range 1.1–4.1) [28]. Magnetic resonance imaging (MRI) was performed to assess the site of compression and status of the cord. Four patients had restrictive pulmonary disease with poor pulmonary reserve secondary to healed pulmonary tuberculosis and found to be unfit for an anterior procedure by the anaesthetist.
Pain, kyphosis angle and functional and neurological status were the main parameters used for the clinical and radiological assessment. Clinical assessment was performed using the measured Oswestry Disability Index (ODI). All patients were asked to rate preoperative pain measurement using a pain visual analogue scale (VAS) with a score of 0 (no pain) to 10 (unbearable pain). In our series, we could not assess the sagittal balance as at the time of performance of these cases a long radiograph cassette was unavailable in our institution.
Surgical procedure
Positioning
All cases were performed under general anaesthesia. The patient was placed prone over two bolsters with adequate padding of the bony prominences. In patients with severe kyphosis, particular care should be taken to prevent hyperextension of the neck, pressure on the eyes and abdomen. When necessary, the table may be appropriately broken to accommodate the deformity.
Exposure and instrumentation
Through a midline incision extending three or four vertebrae above and below the involved segment(s), the paraspinal muscles are dissected sub-periosteally from the spinous processes and the laminae around the facet joints up to the tips of the transverse processes. The operative field must be wide enough on both sides to allow dissection on the under surface of the transverse processes at the osteotomy site. It was not uncommon to notice dislocation of the facet joints at the level of the apex and spontaneous fusion of the facets at few other levels. Pedicle screws are then inserted under fluoroscopic guidance into normal vertebrae a minimum of two or three above and below the lesion. The proximal and distal level of instrumentation calculated to include all levels of the deformity found to be in fixed kyphosis as seen on the preoperative X-rays. Care must be taken for proper placement of screws, as the pedicle orientation can be grossly altered due to the severe deformity and translation of the vertebral columns at the apex of the deformity. In case of difficulty, it would be prudent to locate the pedicle by a small foraminotomy.
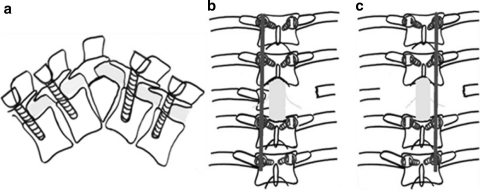
The wedge to be removed is marked using a lateral fluoroscopy view. Bilateral laminectomy is then performed at the marked levels so that the cord is decompressed and fully visualised. A temporary rod (contoured to accommodate the deformity) is applied to maintain spinal stability whilst performing the wedge resection of the anterior column (Fig. 2a, b).
Fig. 2.
a In the surgical procedure, a temporary stabilisation of the spinal column with a pedicle screw construct is first performed before decompression. b A stabilising rod is placed on one side and rib, transverse process and vertebral body resection performed contra laterally. c The stabilising rod is switched to the opposite side and decompression performed contralaterally
The osteotomy and circumferential decompression
The pedicles and exiting nerve roots were then identified. Usually, it is possible to get a sufficient exposure of the fusion mass by gentle retraction of the nerve roots. In patients with more than 60° deformity, there is usually crowding of nerve roots. In the thoracic region, two or three nerve roots can be safely sacrificed by ligating about 3–4 cm away from the intervertebral foramen. The spinal branch of the segmental artery, which runs along with the nerve root, should also be ligated and divided. The ligatures on the sectioned nerve root should be left long and maintained till the end of the procedure as they can be used as landmarks and also to gently lift the dura during the terminal stages of resecting the internal gibbus. Utmost care is taken whilst retracting the nerve roots to avoid traction on the cord.
The ribs at the affected level are transected 3–4 cm lateral to the costotransverse joint, and the pleura are bluntly separated from the ribs (Fig. 2b). The rib heads at the corresponding level, as well as the transverse process, are then carefully excised, remaining extrapleural. The pedicle of the affected level is excised and the nerve roots of the affected level are gently retracted to make room for the operative procedure of anterior decompression or wedge osteotomy. Blunt dissection is followed anteriorly on both sides through the plane between the pleura and the vertebral body. With the proper plane, it is usually possible to bluntly dissect the anterior soft tissue structures away from the anterior margin of the apex. The great vessels are usually separated from the apex by a thick layer of fibrous tissue and can be carefully pushed away from the bone by a peanut or finger tip dissection. The wedge is then marked accurately under fluoroscopic control. The vertebral body (fusion mass) is carefully removed using a curette, rongeur, or high-speed burr in a wedge shape approximating the angular deformity, keeping the posterior vertebral cortex. Its early removal will lead to troublesome bleeding from the epidural veins and also increase the chance of neurological deficits as the cord then continuously descends down into the working area of the burr and other sharp instruments. A second temporary rod is then attached to the screws on the opposite side (Fig. 2c). The initial rod is removed and the decompression procedure repeated on that side. Anteriorly at the apex of the wedge, there is usually a thick fibrocartilaginous tissue that protects against over burring and injury to the great vessels. This needs to be cleared with a curette or sharp dissection so that anterior opening of the apex of the deformity can occur. At the end of the decompression, a circumferential exposure of the dural tube is obtained. Then, the posterior vertebral cortex which has been adequately thinned out with a diamond tip burr is then removed making the osteotomy complete (Fig. 3). A thin Penfield dissector is used to confirm the complete removal of the posterior cortex, so that it does not protrude inside during the closing of the osteotomy. It is not always necessary to remove the posterior longitudinal ligament, which is often adherent to the dura mater.
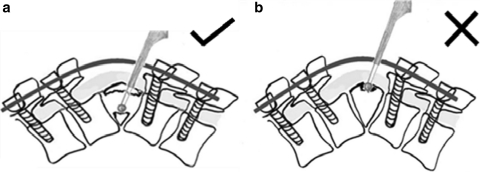
Fig. 3.
a The planned wedge resection of the vertebral body is performed using a high-speed burr and sharp curettes. It is important that a thin shell of posterior cortex of the fusion mass is maintained till the very end so that it forms a natural protection to the cord. b Do not start burring at the apex of the deformity. If decompression is started from the posterior part of the fusion mass, there will be continuous bleeding from the epidural veins and the cord also is prone for injury as it descends down and comes into contact with the working instruments
Deformity correction
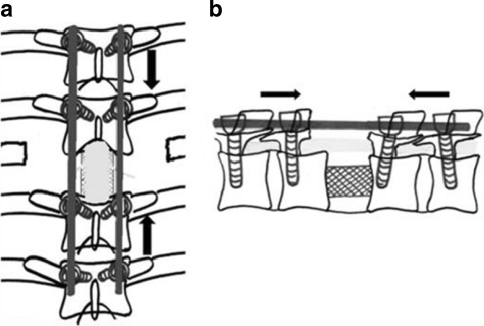
Using contoured rods, shortening is carefully done to produce a concertina collapse of the wedge and correction of the deformity. The entire procedure should be performed slowly and gradually with frequent pauses so that the cord is not shortened suddenly. At the first evidence of kinking of the cord or a concertina type of ballooning of the dura, the shortening is stopped. Further posterior closing is then avoided. The defect in the anterior column is then measured and a vertebral spacer, such as Harms’ titanium mesh cylinder (MossTM titanium surgical mesh, DePuy Motech, Warsaw, IN) with autograft inside or a tricortical iliac crest graft, is carefully inserted into the intervertebral gap. The placement of the graft requires some attention because translation of the vertebral column is frequent and centralisation of the cage may be difficult.
Chip grafts obtained from decompression are used to fill up the remaining gap in the anterior column. The spine is then closed and compressed posteriorly so that the graft is securely compressed (Fig. 4). The tendency for the dura to herniate mildly through the laminectomy defect producing pressure on the cord by the inferior margin of the superior lamina is carefully looked. This can be overcome by extending the laminectomy by another level or by increasing the length of bone graft. A wake-up test is performed to ensure neurological stability. The rods are firmly secured and further packing of the chip grafts is performed. The incision is closed in layers over deep and superficial drains. Patient was allowed to walk with the brace from the fourth or fifth operative day (depending on the neurological status) after the drain removal. None of the patients had evidence of active tuberculosis. However, to prevent the recurrence of the disease, patients were prescribed full course of antituberculous drugs (ATDs) for a minimum period of 9 months. Patients were followed up for 4 weeks, 3 months, 6 months, 1 year and every 6 months thereafter. At each visit, the neurological evaluation was performed and the radiological angle of the deformity, VAS and ODI documented. Patients were braced till the follow-up radiographs showed adequate healing and fusion.
Fig. 4.
a, b After thorough decompression, the posterior rim of the fusion mass is removed. An appropriate sized cage or bone graft is used to open the anterior column so that kinking of the cord is avoided. Posterior compression of the pedicle screws is performed to achieve further correction
Results
All procedures were preformed by the senior author (SR). Average operating time was 280 min (200–340 min) with blood loss of 820 ml (range 500–1,600 ml). The postoperative kyphosis averaged 32.4° ± 19.5° (range 8°–62°). The percentage correction of kyphosis achieved was 56.8 ± 14.6% (range 32–83%). The average deformity correction was 36.7° ± 8.7° (range 25°–52°) following the surgery. Anterior reconstruction was performed using rib grafts in four, tricortical iliac crest graft in five, cages in six and bone chips alone and fibular graft in one patient each. No patient with normal preoperative neurological status showed deterioration in neurology after surgery. Of the patients who had neurological involvement preoperatively, three recovered to Frankel E and one improved to Frankel D and was able to walk with crutches. One patient with preoperative Frankel C deteriorated neurologically to Frankel A in the immediate postoperative period. CT scan done immediately revealed a mal-positioned screw which was revised.
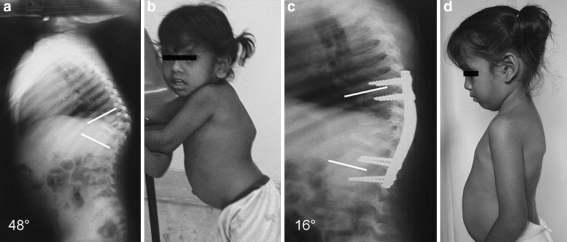
Fourteen patients had spinal stabilisation using pedicle screw rod system. In three children, use of the pedicle screw rod system was prohibited by the high profile of the implants (Fig. 5). These three children had poor posterior musculature making it impossible to obtain a wound closure after pedicle screw fixation. Here, stabilisation had to be achieved by the use of 4.5 narrow dynamic compression plates and screws. Pedicle entry points and trajectories were first confirmed using fluoroscope. Screw tracts were then curetted using the funnel technique and K wires were passed into these pedicles. Contoured DCP was then placed over these K wires and sequentially the K wires were replaced by screws thus correcting the deformity. Although rod in combination with sub-laminar wires is a viable alternative, the risk of neurological injury more so in children made us defer its use. Pedicle screw constructs undoubtedly offer the best opportunity to hold and correct a deformity (Fig. 6).
Fig. 5.
A 48° deformity in a 4-year-old child with completion of ATT treatment 2 years earlier. The deformity has been corrected to 16°. Rib strut grafts have been used to stabilize the anterior column and appropriately moulded dynamic compression plates were used for spinal stabilisation because all the available pedicle screw constructs were too high profile for this child
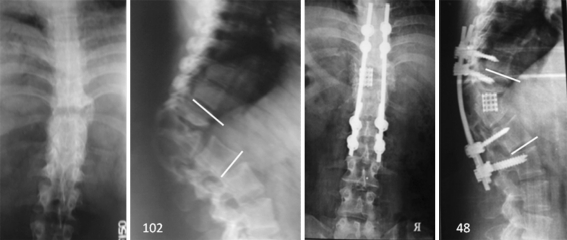
Fig. 6.
Healed tuberculosis of the thoracolumbar spine with a 102° kyphotic deformity in a 40-year-old man. Three vertebral bodies were part of the anterior fusion mass. A closing opening wedge osteotomy was performed and deformity corrected to 48°. A titanium mesh cage filled with bone graft was used to reconstruct the anterior column
Complications were superficial wound infection in two, temporary neurological deterioration in one, temporary jaundice in one and implant failure requiring revision in one. One patient wherein only chip bone grafts were used to reconstruct the anterior column had an implant failure and this was revised by anterior column reconstruction with a cage with no loss of previous correction. No patients complained of neuropathic girdle pain; however, girdle anaesthesia was seen in some of the patients.
The last follow-up was at an average of 43 ± 4 months (range 32–64 months). Radiological fusion was achieved in all patients. There was no outcome difference between rib grafts or iliac crest grafts or cages. The average loss of correction at the last follow-up was 5.4° (range 3°–9°). Distal and proximal junctional kyphosis was not noticed in any of the patients. At the last follow-up, the mean preoperative pain VAS score decreased from 9.2 (range 8–10 points) to 1.5 (range 1–2 points). The decrease in pain was statistically significant. There was also a significant decrease in mean preoperative ODI from 56.4 (range 46–68) to 10.6 (range 6–15).
Discussion
Spinal tuberculosis is the commonest cause of kyphotic deformity in many parts of the world. Spinal tuberculosis involves and destroys the anterior column preferentially in 90% of patients [29, 38] whilst posterior disease is noticed only in 5–10%. Natural healing occurs by collapse of the anterior column till contact is established between healthy vertebrae above and below the lesion. Healing by fusion is the rule, but a gross kyphotic deformity often results before this can occur. Apart from the collapse during the active phase of the disease, deformity can progress in children even after complete cure of the disease. This progress can happen in up to 40% of children due to the inhibitory effect of the increased biomechanical forces of kyphosis on growth plate of the fusion mass and adjacent vertebrae [26, 27]. Post-tuberculous kyphosis in excess of 60° is invariably the result of childhood disease.
Gross kyphotic deformities pose many problems to the patients [29, 38]. In the thoracic and thoracolumbar region, they can result in severe cardiorespiratory embarrassment and also result in late neurological deficit. In the lumbar region, the kyphosis cause severe postural imbalances and can frequently result in severe fore-shortening of the trunk. There can also be increased back pain due to muscle fatigue and friction of the rib cage over the iliac crest. It can also result in problems of self-image and psychological problems in children [26].
Initial attempts of the surgical correction of severe post-tubercular kyphosis (PTK) were difficult and dangerous procedures with a significant complication rate [44]. Thus, Yau et al. advocated a staged procedure with performance of an osteotomy initially, gradual correction in a halo frame and followed by fusion with instrumentation [44]. This protocol was prolonged, multi-staged, and cumbersome to the patient and had a 10% mortality rate and the average amount of correction obtained being only 28%. Advances in spinal surgery with the evolution of better spinal segmental fixation systems have led to the development of other single- or two-stage procedures that achieve good correction with a low complication rate without the need for halo frames or prolonged use of an orthosis. These procedures are broadly classified into anterior-only procedures that involve anterior clearance and reconstruction with anterior fixation systems, the combined anterior and posterior surgical procedures and the presently preferred posterior-only approach.
The choice of correction of a kyphotic deformity by reconstituting the anterior column, shortening the posterior column or a combination of both has important implications to the status of the spinal cord.
Anterior-only procedures have been reported for the correction of post-traumatic deformities and deformity in active spinal tuberculosis [2, 14, 45]. Adequate canal decompression, good correction of the deformity and stabilization of the spine has been reported [2, 14, 45]. However, there are numerous problems in utilising this technique in severe established PTK. Anterior reconstruction and stabilisation using cages and instrumentation have been shown to lengthen the spinal canal [4]. Correction by restoring the anterior column height can severely stretch the spinal cord, especially in spinal tuberculosis as it might have become shortened due to a chronic collapse of the vertebral column. Even minor stretching may be dangerous due to the peridural fibrosis and the transfixion of the dura by the exiting intercostal nerves of the vertebral segments forming the fusion mass.
Anterior-only procedures are not possible in an established kyphotic deformity with sound bony consolidation anteriorly and intact posterior structures. In long standing kyphosis during surgery, many facet joints are found to be fused and this will not allow reconstitution of the sagittal contour by an anterior-only approach.
In severe thoracic kyphotic deformities, it is difficult to approach the concavity of the spine through the anterior transthoracic approach [6, 17]. The anterior approach (thoracotomy/thoracolumbar) in general has the major disadvantage of violation of a normal body cavity and its attendant complications [19]. The presence of compromised lung function, fibrosis and adhesions often seen in these patients adds to the morbidity.
The numerous difficulties and complications associated with the anterior-only approach explain the paucity of studies using this as an isolated surgery. The only study using the anterior approach by Yau et al. [44] concluded that the amount of correction obtained, even when fusion occured, was unrewarding. They emphasised the constant danger of neurological injury as locating the spinal canal was difficult.
A combined anterior and posterior surgery has been shown to reduce the incidence of anterior graft-related problems and ensures better maintenance of the correction [1, 7, 18, 35]. However, the disadvantage of the anterior–posterior procedure is the need for two surgical approaches to treat a pathology resulting in increased blood loss, higher rates of infection and prolonged surgical time; added to this are the difficulties of the anterior approach as explained above. Suk et al. [33] compared the results of the combined anterior–posterior surgery with that of a posterior closed wedge osteotomy in the correction of post-traumatic kyphosis. They concluded that the posterior closed wedge osteotomy procedure gave better surgical results with reduced operating time and less blood loss.
Considering these shortcomings of the anterior approach, either as a stand alone procedure or in combination with a posterior procedure, the correction and stabilisation of the spine through a single-stage posterior approach is a viable option. The advantages of the posterior approach included familiarity of approach, direct access to the apex of the deformity and ability to achieve circumferential decompression of the cord and sound fusion [3, 13, 15, 34].
Posterior-only procedures for the correction of post-infection kyphotic deformities include the posterior vertebral column resection used by Suk et al. [34] and posterior closing wedge osteotomy used by Bezer et al. [3], Kalra et al. [13], Dalvie et al. [8] and Domanic et al. [9], however, these techniques are not universally successful in achieving good correction [3]. In the series by Dalvie et al. [8], a second-stage anterior strut arthrodesis was required in some cases due to unsatisfactory wedge closure and severe residual deformity (>50°), Kalra et al. [13], too, reported a similar complication in their series. Good kyphosis and sagittal balance correction was reported by Domanic et al. [9] in a series which included patients with congenital kyphoscoliosis and post-laminectomy kyphosis. When compared with congenital kyphoscoliosis and post-laminectomy kyphosis, post-infective kyphosis correction is more challenging as the anatomical land marks are usually grossly distorted, the structures anteriorly are tethered (soft tissue and thecal sac) and there are multiple vertebral bodies involved in the post-infective fusion mass.
Posterior shortening procedures have other disadvantages in severe PTK. The anterior column is usually considerably shortened whilst the posterior column is often intact. Closing the wedge will jeopardise the cord by excessive kinking and collapse. (Fig. 1c) The ideal procedure is one in which the posterior column is closed and anterior column appropriately opened such that the length and thus function of the spinal cord is not jeopardised.
Kawahara et al. [15] were the first to describe a closing–opening wedge posterior osteotomy to correct severe kyphotic deformities of non-infectious aetiology. In their seven cases, kyphosis was reduced from an average of 67°–18°. They concluded that although the performance is technically laborious, it offered good correction without jeopardising the integrity of the spinal cord.
This study is the first series using this osteotomy for the correction of severe PTK. The challenges in a PTK as apposed to congenital or post-traumatic deformities are the gross disparity of anterior and posterior column height, multiple vertebral involvement, the presence of significant fibrosis of the anterior prevertebral structures to the spinal column and adhesion of the dura to the spine. We were able to obtain an average correction of 59.23% (range 39–83%). Higher degrees of correction were obtainable in younger patients and in less severe deformities.
The average blood loss in our procedure was 820 ml, with a range of 500–1,600 ml; this was lower compared with that in the procedures advocated by Suk et al. [34] (2,980 ml), Bezer et al. [3] (2,780 ml) and Karla et al. [13] (940 ml). The low blood loss in our series could be attributed mainly to meticulous attention to haemostasis and the use of hypotensive anaesthesia. Hypotensive anaesthesia was used during the stages of dissection, decompression and early stages of the osteotomy, but avoided it in all patients with neurological deficits and during the stages of deformity correction. Another factor could be that many of our patients were children who as a routine only have one-third of the absolute blood loss as adults.
There were only two major complications in our series. One patient developed an implant failure 3 months after surgery. This patient was in the initial stages of this series and failure was due to inadequate reconstruction of the anterior column. During surgery, the anterior column deficit was small and the same was filled with cortico-cancellous bone chips. After closing of the osteotomy, a firm reconstruction was assumed, but there was a failure of the implant that necessitated a revision surgery with the usage of a cage for anterior reconstruction. During the revision, pseudoarthrosis was confirmed. Subsequently, it has been in our protocol to preferentially reconstruct the anterior column using a cage. We have found that packing bone grafts outside the cage is as important, if not more, than packing it inside the cage to achieve better union rates. In the other successful cases, we have not used CT scans, but rather relied on radiological pictures and the absence of clinical symptoms and change in angles.
Only one of the 17 patients deteriorated neurologically. The patient with Frankel C neurological status deteriorated to Frankel A and this was secondary to screw misplacement at the T3 level; immediate revision of the implant was performed. At last follow-up, the patient had no recovery of neurological deficits. Screw placement can be a challenge as the two columns of the spine above and below the level of fusion mass exhibit translation, rotation, and angulations to various degrees. The distortion of anatomy is compounded by the small-sized vertebral bodies in the paediatric age. There is also osteoporosis even after complete healing has been achieved and there may be only one chance for proper placement and purchase of this screw. In patients where difficulty is encountered, we recommend that a lamino-foraminotomy be made to palpate the medial and inferior walls of the pedicle as this serves as a guide to the pedicle position and orientation. None of the patients developed a deep postoperative infection and all went on to have a solid fusion.
The complication rate in our procedure is less compared to that of posterior vertebral column resection as described by Suk et al. [34] who reported complications in 10 of the 25 patients, which included one complete cord injury, two haematomas, two root injuries, one fixation failure, one deep infection, and three haemopneumothorax. Dalvie et al. [8] in their series of nine children had four pneumothoraces and one neurological deterioration with incomplete recovery. Bridwell et al. [5] studied the complications of lumbar pedicle subtraction osteotomy in 33 patients and reported 1 case of lumbar pseudoarthrosis, 6 thoracic pseudoarthrosis and 1 lumbosacral pseudoarthrosis. Fixed angular kyphosis above the instrumentation was seen in two patients and five had transient neurological deficit.
Correction of the deformity is achieved by both closing posteriorly and opening anteriorly. The exact extent that a spinal cord can be safely shortened is not clearly known. Tomita et al. [36] have shown that acute shortening for a level of one vertebral body is not a problem. Gertzbein and Harris [12] cautioned that kinking of the spinal cord and dural buckling are potential problems associated with spinal shortening and advised against attempting corrections more than 40°. Kawahara et al. [15] achieved an average correction of 49° in seven patients who presented with an average preoperative kyphotic angle of 67° using the closing–opening wedge osteotomy technique. During the procedure, the first attempted closing of the wedge posteriorly slowly till the first suggestion of kinking of the cord was evident. At that point, the closing was stopped and the remaining gap in the anterior column was made good by an appropriately sized cage. Further correction was achieved using the cage as a fulcrum. Thus, good correction could be achieved without any neurological compromise. Pressure on the cord by the margins of the lamina must also be avoided and if necessary the laminectomy may be extended by an additional level caudally and cranially to avoid excessive pressure. Spinal cord monitoring was not used in any of our patients, due to non-availability, but would be a valuable addition to this procedure.
Many authors [10, 16, 39, 42] have recommended prophylactic ATDs prior to and following surgeries such as joint replacement operations in healed tuberculosis, as reactivation of tuberculosis is potentially dangerous. Reactivation of disease in healed or quiescent articular tuberculosis after a joint replacement has been reported [10, 42], even in the presence of negative histopathology and culture reports [16]. Although ATD have potential side effects, we chose to prophylactically cover our patients with ATD for a period of 9 months as reactivation of disease following the spinal deformity correction procedure would have serious implications of implant loosening, loss of correction and a complex revision surgery. None of our patients had any complications secondary to ATD.
Conclusion
Severe PTK is associated with problems of poor self-image, back pain, easy fatigability, cardiorespiratory compromise and neurological deficits. Single-stage closing opening wedge osteotomy is a reliable, effective and safe method to correct severe PTK.
References
- 1.Altman GT, Altman DT, Frankovitch KF. Anterior and posterior fusion for children with tuberculosis of the spine. Clin Orthop. 1996;325:225–231. doi: 10.1097/00003086-199604000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Benli IT, Acaroglu E, Akalin S, et al. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J. 2003;12:224–234. doi: 10.1007/s00586-002-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bezer M, Kucukdurmaz F, et al. Transpedicular decancellation osteotomy in the treatment of posttuberculous kyphosis. J Spinal Disord Tech. 2007;20:209–215. doi: 10.1097/01.bsd.0000211271.89485.f1. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, Kuklo T, Lewis SJ, et al. String test measurement to assess the effect of spinal deformity correction on spinal canal length. Spine. 2001;26:2013–2019. doi: 10.1097/00007632-200109150-00015. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH, Lewis SJ, Edwards C, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003;28:2093–2101. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 6.Capner N. The evolution of lateral rachiotomy. J Bone Joint Surg Br. 1954;36B:173–179. doi: 10.1302/0301-620X.36B2.173. [DOI] [PubMed] [Google Scholar]
- 7.Chen WJ, Wu CC, Jung CH, et al. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop. 2002;398:50–59. doi: 10.1097/00003086-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Dalvie SS, Laheri VJ. Closed-wedge spinal osteotomy for the correction of post-tubercular kyphosis in children. J Bone Joint Surg Br. 2000;82-B:283–284. [Google Scholar]
- 9.Domanic U, Talu U, Dikici F, Hamzaoglu A. Surgical correction of kyphosis: posterior total wedge resection osteotomy in 32 patients. Acta Orthop Scand. 2004;75(4):449–455. doi: 10.1080/00016470410001231-1. [DOI] [PubMed] [Google Scholar]
- 10.Eskola A, Santavirta S, Konttinen YT, et al. Cementless total replacement for old tuberculosis of the hip. J Bone Joint Surg Br. 1988;70-B:603–606. doi: 10.1302/0301-620X.70B4.3403606. [DOI] [PubMed] [Google Scholar]
- 11.Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia: I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 12.Gertzbein SD, Harris MB. Wedge osteotomy for the correction of posttraumatic kyphosis. Spine. 1992;17:374–379. doi: 10.1097/00007632-199203000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Kalra KP, Dhar SB, Shetty G, Dhariwal Q. Pedicle subtraction osteotomy for rigid post-tuberculous kyphosis. J Bone Joint Surg Br. 2006;88-B:925–927. doi: 10.1302/0301-620X.88B7.17366. [DOI] [PubMed] [Google Scholar]
- 14.Kaneda K (1991) Anterior approach and Kaneda instrumentation for lesions of the thoracic and lumbar spine. In: Bridwell KH, DeWald RL (eds) The textbook of spinal surgery. JB Lippincott Company, Philadelphia, pp 959–990
- 15.Kawahara N, Tomita K, Hisatoshi B, et al. Closing–opening wedge osteotomy to correct angular kyphotic deformity by a single posterior approach. Spine. 2001;26:391–402. doi: 10.1097/00007632-200102150-00016. [DOI] [PubMed] [Google Scholar]
- 16.Yh Kim, Han DY, Park BM. Total hip arthroplasty for tuberculous coxarthrosis. J Bone Joint Surg Am. 1987;69A:718–727. [PubMed] [Google Scholar]
- 17.Lonstein JE, et al. Cord compression. In: Bradford DS, Lonstein JE, Ogilvie JW, et al., editors. Moe’s textbook of scoliosis and other spinal deformities. 2. Philadelphia: WB Saunders; 1987. pp. 540–547. [Google Scholar]
- 18.Louw JA. Spinal tuberculosis with neurological deficit: treatment with anterior vascularised rib grafts, posterior osteotomies and fusion. J Bone Joint Surg Br. 1990;72:686–693. doi: 10.1302/0301-620X.72B4.2380228. [DOI] [PubMed] [Google Scholar]
- 19.McDonnell MF, Glassman SD, et al. Perioperative complications of anterior procedures on the spine. JBJS. 1996;78-A(6):839–847. doi: 10.2106/00004623-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Medical Research Council A 15-year assessment of controlled trials of the management of tuberculosis of the spine in Korea and Hong Kong: thirteenth report. J Bone Joint Surg Br. 1998;80-B:456–462. doi: 10.1302/0301-620x.80b3.8544. [DOI] [PubMed] [Google Scholar]
- 21.Moon MS, Lee MK. The changes of the kyphosis of the tuberculous spine in children following ambulant treatment. Korean Orthop Assoc. 1971;6:203–208. [Google Scholar]
- 22.Moon MS, Woo YK, Lee KS, et al. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine. 1995;20:1910–1916. doi: 10.1097/00007632-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Moon MS. Tuberculosis of the spine, controversies and a new challenge. Spine. 1997;22:1791–1797. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 24.Moon MS, Kim I, Woo YK, Park YO. Conservative treatment of tuberculosis of the thoracic and lumbar spine in adults and children. Int Orthop. 1987;11:315–322. doi: 10.1007/BF00271307. [DOI] [PubMed] [Google Scholar]
- 25.Parathasarathy R, Sriram K, Satha T, et al. Short course chemotherapy for tuberculosis of the spine: a comparison between ambulant treatment and radical surgery—10 year report. J Bone Joint Surg. 1999;81B:464–471. doi: 10.1302/0301-620X.81B3.9043. [DOI] [PubMed] [Google Scholar]
- 26.Rajasekaran S. The natural history of childhood spinal tuberculosis: a 15-year prospective study. J Bone Joint Surg Br. 2001;83B:954–962. doi: 10.1302/0301-620X.83B7.12170. [DOI] [PubMed] [Google Scholar]
- 27.Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop. 2002;398:85–92. doi: 10.1097/00003086-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Rajasekaran S, Shanmugasundaram TK. Prediction of the angle of gibbus deformity in tuberculosis of the spine. J Bone Joint Surg Am. 1987;69-A(4):503–509. [PubMed] [Google Scholar]
- 29.Rajasekaran S, Shanmugasundaram TK (2002) Spinal tuberculosis. In: Bulstrode C (ed) Oxford textbook of orthopedics and trauma, 1st edn. Oxford University Press, Oxford, pp 1545–1561
- 30.Reyes-Sanchez A, Rosales LM, Miramontes VP, et al. Treatment of thoracolumbar fractures by vertebral shortening. Eur Spine J. 2002;11:8–12. doi: 10.1007/s005860000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Satyasri S (1993) Global epidemiology of tuberculosis. In: Satyasri S (ed) Textbook of pulmonary and extra-pulmonary tuberculosis. Madras, pp 13–18
- 32.Siata K, Hoshini Y, Kikkawa I, et al. Posterior spinal shortening for paraplegia after vertebral collapse caused by osteoporosis. Spine. 2000;25:2832–2835. doi: 10.1097/00007632-200011010-00018. [DOI] [PubMed] [Google Scholar]
- 33.Se-II Suk, Kim JH, Lee SM, et al. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine. 2003;28:2170–2175. doi: 10.1097/01.BRS.0000090889.45158.5A. [DOI] [PubMed] [Google Scholar]
- 34.Se-II Suk, Kim JH, Kim WJ, et al. Posterior vertebra column resection for severe spinal deformities. Spine. 2002;27:2374–2382. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 35.Sundarajan GD, Behera S, Ravi V, et al. The role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg Br. 2003;85:100–106. doi: 10.1302/0301-620X.85B1.13300. [DOI] [PubMed] [Google Scholar]
- 36.Tomita K, Kawahara N, Baba H, et al. Circumspinal decompression for thoracic myelopathy due to combined ossification of the posterior longitudinal ligament and ligamentum flavum. Spine. 1990;15:1114–1120. doi: 10.1097/00007632-199011010-00006. [DOI] [PubMed] [Google Scholar]
- 37.Tuli SM. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop. 1995;19(5):327–331. doi: 10.1007/BF00181121. [DOI] [PubMed] [Google Scholar]
- 38.Tuli SM. Tuberculosis of the skeletal system. 3. New Delhi: Jaypee Brothers; 1991. [Google Scholar]
- 39.Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop. 2002;398:11–19. doi: 10.1097/00003086-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 40.vanRoyen BJ, Slot GH. Closing wedge posterior osteotomy for ankylosing spondylitis: partial corpectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br. 1995;77B:117–121. [PubMed] [Google Scholar]
- 41.Watson JM. Editorial: tuberculosis in Britain today. Br Med J. 1993;306:221–222. doi: 10.1136/bmj.306.6872.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Watts AHG, Lifeso RM. Current concept review: tuberculosis of bone and joints. J Bone Joint Surg Am. 1996;78:288–298. doi: 10.2106/00004623-199602000-00019. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organisation Press Release (1996) WHO/22, March 1996
- 44.Yau ACMC, Hsu LCS, O’Brien JP, Hodgson AR. Tuberculosis kyphosis-correction with spinal osteotomy, halo-pelvic distraction and anterior and posterior fusion. J Bone Joint Surg Am. 1974;56A:1419–1434. [PubMed] [Google Scholar]
- 45.Yilmaz C, Selek HY, Gurkan I, et al. Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Joint Surg Am. 1999;81A:1261–1267. doi: 10.2106/00004623-199909000-00007. [DOI] [PubMed] [Google Scholar]