Abstract
Lateral mass (LM) screws are commonly used in posterior instrumentation of the cervical spine because of their perceived safety over pedicle screws. A possible complication of cervical LM screw placement is vertebral artery injury or impingement. Several screw trajectories have been described to overcome the risks of neurovascular injury; however, each of these techniques relies on the surgeon’s visual estimation of the trajectory angle. As the reliability hereof is poorly investigated, alignment with a constant anatomical reference plane, such as the cervical lamina, may be advantageous. The aim of this investigation was to determine whether alignment of the LM screw trajectory parallel to the ipsilateral cervical lamina reliably avoids vertebral artery violation in the sub-axial cervical spine. 80 digital cervical spine CT were analysed (40 female, 40 male). Exclusion criteria were severe degeneration, malformations, tumour, vertebral body fractures and an age of less than 18 or greater than 80 years. Mean age of all subjects was 39.5 years (range 18–78); 399 subaxial cervical vertebrae (C3–C7) were included in the study. Measurements were performed on the axial CT view of C3–C7. A virtual screw trajectory with parallel alignment to the ipsilateral lamina was placed through the LM. Potential violation of the transverse foramen was assessed and the LM width available for screw purchase measured. There was no virtual violation of the vertebral artery of C3–C7 with lamina-guided LM screw placement. LM width available for screw purchase using this technique ranged from 5.2 to 7.4 mm. The sub-axial cervical lamina is a safe reference plane for LM screw placement. LM screws placed parallel to the ipsilateral lamina find sufficient LM width and are highly unlikely to injure the vertebral artery, even in bi-cortical placement. Placing LM screws parallel to the lamina appears favourable over conventional techniques.
Keywords: Lateral mass screw trajectory, Surgical technique, Subaxial cervical spine, Vertebral artery injury, Cervical spine anatomy
Introduction
Lateral mass (LM) screws are commonly used in the cervical spine as a safer alternative to pedicle screws, despite their lower pull out strength [10–12]. However, they are occasionally associated with nerve root and vertebral artery injury [6, 13, 16, 18]. In a cadaveric study, Seybold et al. [16] report a vertebral artery injury rate of 5.8% in bi-cortical screw placement.
Several LM screw techniques with the aim of minimising vertebral artery injury have been described, whereby the Jeanneret and Magerl and Roy-Camille adaptations are most widely used [1, 2, 9, 15]. Correct screw placement with these techniques involves reliably estimating a screw trajectory of between 10° and 30° from the sagittal plane.
Neurovascular structures are reliably avoided with an angle of at least 30° to the sagittal plane [13]. Intra-operative freehand estimation of the trajectory can, however, be difficult and the reliability hereof is poorly investigated. As the subaxial cervical lamina forms an angle to the sagittal plane of approximately 50° [8], LM screws could be aligned with this trajectory using the lamina as a more reliable anatomical reference plane and achieve greater safety due to the larger degree of lateral angulation.
The questions to be answered by this investigation are
Will LM screws placed parallel to the cervical lamina reliably avoid the vertebral artery?
Is the lateral mass sufficiently wide to accommodate LM screws placed parallel to the cervical lamina?
Materials and methods
Ethics committee approval was sought for this investigation and found not to be applicable.
Digital Computed Tomography (CT) scans of the cervical spine were selected for this investigation from our university hospital database based on the following criteria:
Age range from 18–80 years old.
Exclusion of neoplasia, deformity, severe degeneration, burst or sagittal split fractures of the subaxial spine in the report.
The vast majority of identified eligible scans had been obtained as part of an emergency trauma work-up wherein standardised inline positioning of the patients head and neck is employed and an axial CT spiral is obtained (slice thickness 1.25 mm). The images are routinely reformatted and archived on the PACS system with the axial images in perpendicular alignment to the longitudinal axis of the vertebrae by the radiology team assessing the scan.
Of the eligible scans 40 male and 40 female scans were selected. Average age was 36 years in the male group and 43 in the female group (range 18–78). Vertebrae from C3–C7 were included in the investigation if the lamina and lateral mass could be visualised together. Only one C7 vertebra with insufficient visualisation of the lateral mass and lamina together needed to be excluded, resulting in a total of 399 vertebrae suitable for this investigation. All scans were available digitally on the Impax PACS system (Agfa), allowing a measurement accuracy of 0.1 mm.
A virtual screw trajectory parallel to the ipsilateral lamina was placed bi-cortically through the LM. The trajectory was aligned 2 mm from the lamina to allow for the necessary clearance of the drill guide and head of a standard 3.5 mm LM screw (Fig. 1). Potential violation of the vertebral artery in line with the trajectory was assessed and the LM width available for screw purchase measured (Fig. 2). Both the left and right sides were analysed.
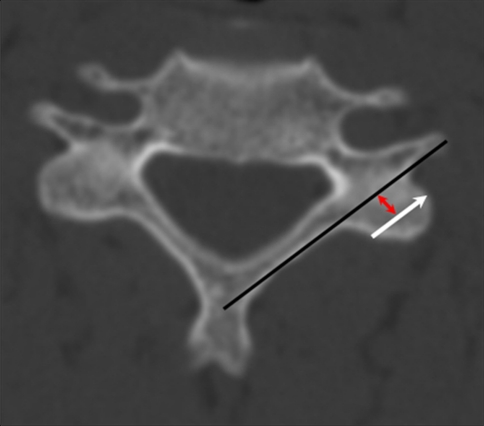
Fig. 1.
Axial CT image showing placement of line parallel to the posterior cortex of the lamina (black line) and virtual LM screw (white arrow). Red arrow represents 2 mm offset to allow for screw head
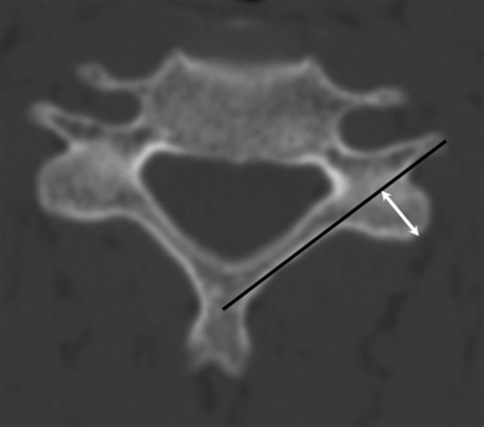
Fig. 2.
Axial image showing measurement of lateral mass width (white arrow)
The measurements were carried out by two investigators, one from the Spinal Surgery Unit, the other from the Radiology Department. Data were collated within a Microsoft Excel spreadsheet. Standard statistics, such as mean and standard deviation, were performed using the Excel spreadsheet, whilst the concordance correlation coefficient and Bland–Altman plot (intra- and inter-observer error) were calculated via the MedCalc statistical software package (http://www.medcalc.be).
Intra-observer error was determined in repeated measurements of LM width on 11 patients (55 vertebrae, 110 LM). The concordance correlation co-efficient was 0.85 (95% C.I.: 0.79–0.89). A Bland–Altman plot showed a mean difference of 0.08 mm between our measurements. These values were judged to be sufficient to enable us to perform the measurements independently and use the obtained values for the intended investigation.
Results
Vertebral artery injury
In the 399 vertebral bodies analysed (bilaterally) from C3–C7, no lamina-guided LM screw would have violated the vertebral artery.
Lateral mass width
LM of females was generally found to be slightly narrower than males (Table 1). In females, the overall average LM width (of all levels C3–C7) available for screw purchase was 6.1 mm. The average width was largest at C5 with 7.1 mm and smallest at C3 with 5.2 mm. In males, the overall average LM width (of all levels C3–C7) available for screw purchase was 6.4 mm. The average width was largest at C6 with 7.4 mm and smallest at C3 with 5.2 mm.
Table 1.
Mean lateral mass width (mm)
| Males | Females | |||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| C3 | ||||
| Mean | 5.4 | 5.2 | 5.4 | 5.2 |
| SD | 1.0 | 1.1 | 0.8 | 1.0 |
| C4 | ||||
| Mean | 6.1 | 6.0 | 5.7 | 5.9 |
| SD | 0.8 | 0.9 | 0.9 | 1.1 |
| C5 | ||||
| Mean | 7.0 | 7.2 | 6.7 | 7.1 |
| SD | 1.0 | 1.2 | 1.1 | 1.2 |
| C6 | ||||
| Mean | 7.4 | 7.4 | 6.8 | 6.8 |
| SD | 1.1 | 1.2 | 1.3 | 1.2 |
| C7 | ||||
| Mean | 6.3 | 6.4 | 5.8 | 5.7 |
| SD | 1.3 | 1.3 | 1.4 | 1.5 |
SD standard deviation
In total, 84% of the investigated vertebrae had a LM width of 5 mm or more which would be able to accommodate a 3.5 mm diameter screw (Table 2). The levels with the lowest percentage of LM with a width >5 mm were C3 and C7 in females with 64 and 66%, respectively. In males, C3 was found to be most restrictive with 73% having a LM width > 5 mm.
Table 2.
Percentage of lateral mass with width >5 mm at each vertebral level
| Males | Females | |
|---|---|---|
| C3 | 73 | 64 |
| C4 | 88 | 86 |
| C5 | 100 | 94 |
| C6 | 98 | 82 |
| C7 | 90 | 66 |
Discussion
Several techniques are described in the literature for placement of LM screws [1], with the two most commonly described in the literature being the Jeanneret & Magerl and Roy-Camille versions [9, 15]. Cadaveric studies have shown that the vertebral artery is at risk with standard LM techniques [1, 13, 16], despite the finding of Ebraheim et al. [5] that the foramen transversarium is in line with the midpoint of the lateral mass. Merola et al. [13] have shown that with modification of the standard techniques of Jeanneret & Magerl [9] and Anderson [2] to 30° lateral angulation, nerve roots and arteries are unlikely to be injured. The same group identified a higher risk of violation of neurovascular structures below C3 with the Roy-Camille technique, suggesting greater safety with the Magerl and Anderson techniques. There is therefore good evidence that a 30° minimum angulation provides a reliable safety margin. The precision of this angle, however, depends on the visual estimation by the surgeon.
We believe that it can be difficult to accurately estimate a 30° angle intra-operatively whilst drilling, and that a reliable anatomical reference plane would be advantageous to the surgeon, especially if less experienced. The study of Seybold et al. [16] supports this notion with the finding that the incidence of injury to neurovascular structures correlates with the level of training.
The purpose of this CT-based study therefore was to determine whether the cervical lamina could be used as a reliable reference plane for the placement of LM screws in the sub-axial cervical spine. Specifically, we sought to determine if the trajectory parallel to the ipsilateral lamina would consistently allow safe passage of the screw lateral to the vertebral artery, while providing sufficient bony purchase in the LM.
The technique we propose is similar to the Jeanneret & Magerl technique [9], the difference being the larger degree of lateral angulation through alignment with the ipsilateral lamina. Hacker et al. [8] have shown the angle of the sub-axial cervical lamina to be 50° from the sagittal plane. Our analysis of the virtual placement of bicortical LM screws aligned with the cervical lamina in 399 vertebrae confirms that vertebral artery injury can almost be excluded in normal anatomy.
The LM widths available for screw purchase (5.2–7.4 mm) measured in our study (Table 1) are smaller than those measured in other articles (8–17.1 mm) [3, 17]. This is related to the large degree of lateral angulation needed to perform our technique, which reduces the amount of bone stock available (based on the assumption that 5 mm of LM bone is needed to incorporate a 3.5 mm screw). As can be seen in Table 2, not all individuals have LM width sufficient for this technique to be performed. This is particularly the case at C3 and C7 in females, where a just over a third of individuals were shown to possess a LM width less than 5 mm. At C7, pedicle screws have been found to be a suitable alternative [1]. The majority of LM would, however, allow our technique to be employed and preoperative assessment of patient’s CT scans would clarify the individual suitability for this technique.
While the presented results suggest that lamina-guided LM placement may be a more reliable method for avoiding vertebral artery injury than conventional techniques, there are several limitations to this study:
The analysed spiral CT scans were all performed in the clinical setting as dictated by clinical requirements and reformatting of the images was performed by several different radiologists. Although performed in a standardised manner, they were not specifically set up for research purposes. However, as one of the largest national university hospitals and the regional trauma centre, we are fortunate in possessing an extensive digital imaging archive from which we were able to select the most suitable scans and only one vertebra needed to be excluded from analysis due to inadequate visualisation of the lamina and LM in the same axial cut.
This study was designed to specifically investigate the hypothesis that the orientation of the lamina can be used to safely and reliably guide LM screws past the vertebral artery. We have not specifically investigated the potential for nerve root injury as the axial image used for analysis was commonly at the level of the pedicle. The intervertebral foramen (and therewith the nerve root) were not visualised. However, given the known anatomical course of the cervical nerve roots and as shown by Pait et al. [14] and Ebraheim et al. [7], the anterolateral border of the LM where our virtual screw exits––regardless of the cranio-caudal angulation––is devoid of relevant neural structures. It is therefore reasonable to assume that the proposed trajectory would also minimise the risk of nerve root injury.
Determination of the actual screw length would require placement in three-dimensional reconstructions of the scans which was not necessary for the purpose of this investigation. Clinically the senior authors have found bicortical screw lengths of 18–22 mm to be applicable.
A disadvantage of this technique is the frequent necessity of removing the tips of the spinous processes in order to align the drill guide with the lamina. Often the lamina will, however, need to be removed in any case for decompressive purposes. The use of spinous processes as a reference for screw trajectory has been suggested by Chin et al. [4], but the authors do describe significant limitations to their suggestion, given that the screw trajectories they produced were highly variable. In view of our findings, we advocate the use of the lamina as a reference plane in preference to the spinous process. The senior authors of this investigation, while not having investigated this scientifically, have not noted an adverse effect of removing the tips of the spinous processes over several years of employing this technique. The obvious limitation to this technique is when performing revision surgery in which laminectomies have previously been performed.
Finally, while the senior authors have successfully performed posterior instrumentation of the sub-axial cervical spine using this technique for several years, formal clinical investigation of this technique is still needed to prove the theoretical advantages suggested by this investigation.
Conclusion
The ipsilateral lamina is a suitable reference plane for the placement of subaxial cervical LM screws. LM screws placed along the trajectory of the cervical lamina are highly unlikely to injure the vertebral artery. The majority of LM possess sufficient width to accommodate screws placed along this trajectory.
References
- 1.An HS, Gordin R, Renner K. Anatomic considerations for plate screw fixation of the cervical spine. Spine. 1991;16(10 Suppl):S548–S551. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 2.Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR. Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine. 1991;16(3 Suppl):S72–S79. doi: 10.1097/00007632-199103001-00012. [DOI] [PubMed] [Google Scholar]
- 3.Barrey C, Mertens P, Jund J, Cotton F, Perrin G. Quantitative anatomic evaluation of cervical lateral mass fixation with a comparison of the Roy-Camille and the Magerl screw techniques. Spine. 2005;30(6):E140–E147. doi: 10.1097/01.brs.0000155416.35234.a3. [DOI] [PubMed] [Google Scholar]
- 4.Chin KR, Eiszner JR, Roh JS, Bohlman HH. Use of spinous processes to determine drill trajectory during placement of lateral mass screws: a cadaveric analysis. J Spinal Disord Tech. 2006;19(1):18–21. doi: 10.1097/01.bsd.0000176976.24318.54. [DOI] [PubMed] [Google Scholar]
- 5.Ebraheim NA, Xu R, Yeasting RA. The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. Spine. 1996;21(11):1291–1295. doi: 10.1097/00007632-199606010-00002. [DOI] [PubMed] [Google Scholar]
- 6.Ebraheim NA, Klausner T, Xu R, Yeasting RA. Safe lateral mass screw lengths in the Roy-Camille and Magerl techniques. An anatomic study. Spine. 1998;23(16):1739–1742. doi: 10.1097/00007632-199808150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim NA, Xu R, Stanescu S, Yeasting RA. Anatomic relationship of the cervical nerves to the lateral masses. Am J Orthop. 1999;28(1):39–42. [PubMed] [Google Scholar]
- 8.Hacker AG, Molloy S, Bernard J. The contralateral lamina: a reliable guide in subaxial, cervical pedicle screw placement. Eur Spine J. 2008;17(11):1457–1461. doi: 10.1007/s00586-008-0756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeanneret B, Magerl F, Ward EH, Ward JC. Posterior stabilization of the cervical spine with hook plates. Spine. 1991;16(3 Suppl):S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 10.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22(9):977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 11.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19(22):2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 12.Kothe R, Ruther W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29(17):1869–1875. doi: 10.1097/01.brs.0000137287.67388.0b. [DOI] [PubMed] [Google Scholar]
- 13.Merola AA, Castro BA, Alongi PR, Mathur S, Brkaric M, Vigna F, Riina JP, Gorup J, Haher TR. Anatomic consideration for standard and modified techniques of cervical lateral mass screw placement. Spine J. 2002;2(6):430–435. doi: 10.1016/S1529-9430(02)00461-8. [DOI] [PubMed] [Google Scholar]
- 14.Pait TG, McAllister PV, Kaufman HH. Quadrant anatomy of the articular pillars (lateral cervical mass) of the cervical spine. J Neurosurg. 1995;82(6):1011–1014. doi: 10.3171/jns.1995.82.6.1011. [DOI] [PubMed] [Google Scholar]
- 15.Roy-Camille R, Saillant G, Laville C, Benazet JP. Treatment of lower cervical spinal injuries––C3 to C7. Spine. 1992;17(10 Suppl):S442–S446. doi: 10.1097/00007632-199210001-00017. [DOI] [PubMed] [Google Scholar]
- 16.Seybold EA, Baker JA, Criscitiello AA, Ordway NR, Park CK, Connolly PJ. Characteristics of unicortical and bicortical lateral mass screws in the cervical spine. Spine. 1999;24(22):2397–2403. doi: 10.1097/00007632-199911150-00018. [DOI] [PubMed] [Google Scholar]
- 17.Stemper BD, Marawar SV, Yoganandan N, Shender BS, Rao RD. Quantitative anatomy of subaxial cervical lateral mass: an analysis of safe screw lengths for Roy-Camille and Magerl techniques. Spine. 2008;33(8):893–897. doi: 10.1097/BRS.0b013e31816b4666. [DOI] [PubMed] [Google Scholar]
- 18.Xu R, Haman SP, Ebraheim NA, Yeasting RA. The anatomic relation of lateral mass screws to the spinal nerves. A comparison of the Magerl, Anderson, and An techniques. Spine. 1999;24(19):2057–2061. doi: 10.1097/00007632-199910010-00016. [DOI] [PubMed] [Google Scholar]