Abstract
This paper reports a morphometric study of the C2 laminae to provide quantitative anatomical data for safe crossing laminar screw placement. A valid trajectory is essential for C2 crossing laminar screw placement. Although several clinical technique notes and modifications to define a safe screw trajectory have been introduced in the recent years, no morphometric analysis has been performed to confirm the accuracy of screw trajectory using this technique. In this study, morphometric analysis was performed on 100 Korean C2 three-dimensional reconstruction CT images. The reconstructive C2 vertebrae from the post-edge of the spinal canal to the spinal process were divided into several zones, 1 mm each. Each zone was chosen as the entry point to imitate a crossing laminar screw (3.5 mm diameter) placement. In each 1-mm zoned trajectory, the screw pass ratio (PR), safe screw angle range (SAR) and maximum screw length (MSL) were measured and compared with the data from the other zoned trajectories. The zone ‘5–6 mm posterior to the post-edge of the spinal canal’ was found to be a more feasible and safer entry point for guiding a crossing laminar screw placement than the other zones because this zone could provide a trajectory with maximal PR (85%), SAR (9.57 ± 4.36º) and a larger MSL (21.74 ± 2.44 mm) than the other areas. The recommended safe screw angle in the axial plane is 49.68 ± 4.94 to 59.19 ± 4.70º. However, the screw angle can vary considerably according to the individual variance. A preoperative evaluation of the screw trajectory is essential for safe screw placement using this technique.
Keywords: Cervical vertebra, Crossing laminar screw, Trajectory analysis, Laminar thickness, Entry point, Safe angle
Introduction
The C2 crossing laminar screw technique reported by Wright [24] in 2004 is a relatively new method for upper cervical fixation. Compared to transarticular screw (Jeanneret and Magerl) [9] and pedicle screw techniques, this method can provide similar stability to the atlantoaxial complex [5, 12, 13], which is considered to be simpler and safer due to the less intraoperative exposure and minimal risk of vertebral artery injury [2, 3, 8, 15, 24]. Subsequent morphological studies reported the applicability of this technique in different populations and showed that this method could be applied safely in most of the specimens they studied [2, 7, 11, 19, 22]. With increasing number of reports of its successful clinical applications, the C2 crossing laminar screw technique is believed to be a safe and effective method for upper cervical surgery [6, 16–18, 20, 21, 23].
Recently, several clinicians recognized the potential complications of this technique: the crossing laminar screw might violate the inner laminar cortex and screw into the spinal canal [1, 23, 24]. Although no acute neurological injuries during surgery have been reported, an intrusion of the screw into the spinal canal can cause a loss of fixation strength and reduce the capacity of the spinal canal, which might result in postoperative cervical instability or long term neurological complications. However, the operators can only check the screw’s deviation on the postoperative CT scans because intra-operative fluoroscopy or X-ray is not helpful for determining screw placement [14]. Minute morphometric analysis on the screw trajectory could be helpful by providing quantitative data to guide safe screw placement using this technique.
Materials and methods
One hundred Korean C2 vertebrae were selected randomly from the Digital Korean Human Model database (Korea Institute of Science and Technology Information, Daejeon, Korea). The demographic information was available for each specimen, including age, gender and height measurements of all cadavers. Fifty specimens were obtained from men, whose average age and height was 50 (21–60) and 165.8 (160–176) cm, respectively. The other 50 specimens were obtained from women, whose average age and height was 54 (27–60) and 156.2 (146–166) cm, respectively. All the measurements were conducted on three-dimensional reconstruction samples on a computer using image-based three-dimensional modeling software (Mimics Ver. 13.0, Materialise, Belgium).
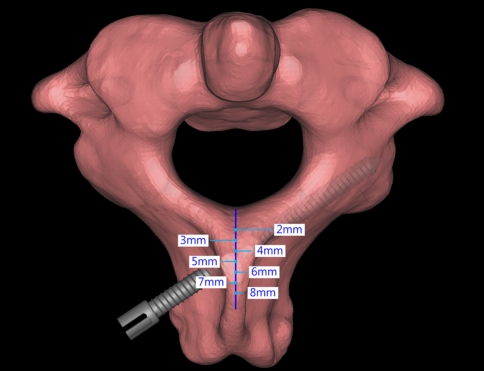
The C2 vertebrae from the post-edge of the spinal canal to the spinal process were divided into several zones, 1 mm each. In each zone, imitations of 3.5 mm diameter screw placement were performed by crossing the bilateral C2 laminae (Fig. 1).
Fig. 1.
Three-dimensional C2 model in Mimics software with a schematic diagram showing the 5–6 mm zoned trajectory for 3.5 mm diameter screw placement by crossing laminar fixation
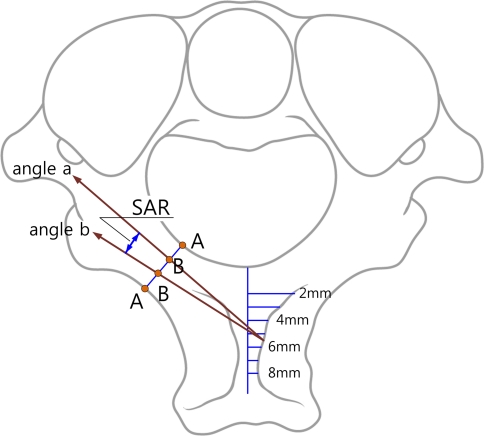
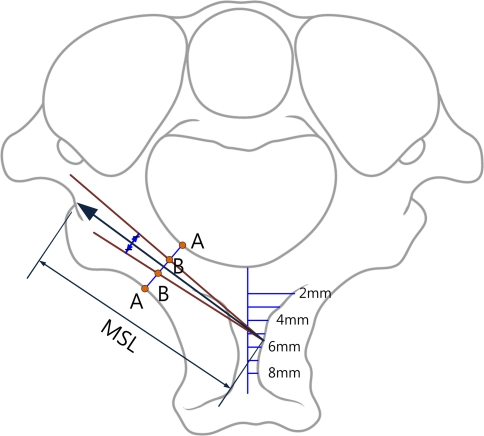
Several zoned trajectories were obtained for each specimen. The screw pass ratio (PR) for the 3.5 mm diameter screw to pass through the mid-lamina (PR), safe screw angle range (SAR) (Fig. 2) and maximum screw length (MSL) (Fig. 3) were measured in every zoned trajectory.
Fig. 2.
Schematic diagram of the safe angle range (SAR) for 3.5 mm diameter screws to cross through the mid-laminae safely without violating the inner laminar cortex in the axial plane. A Mid-point of lamina; AB screw radius (3.5/2 = 1.75 mm) Angle a the minimal safe angle for the inner laminar cortex; Angle b the maximal safe angle for passing the outer mid-lamina cortex
Fig. 3.
Schematic diagram of the maximal screw length (MSL)
Statistical analysis was performed using unpaired Student’s t tests to analyze the PR, SAR and MSL differences in the different zoned trajectories.
Result
Since 18% specimens in this study had spinal processes < 8 mm, morphometric analysis was performed on the first seven zoned trajectories (entry points from 1 to 7 mm posterior to the post-edge of the spinal canal).
The 0–1 mm, 1–2 mm zoned trajectories could not allow 3.5 mm diameter screws to pass through the mid-laminae safely. The 2–3 mm zoned trajectory only had a 54% PR with a minimal SAR of 3.74 ± 1.79º and MSL of 14.73 ± 1.30 mm. The 3–4 mm zoned trajectory had a SR, SAR and MSL of 71%, 4.59 ± 1.71º and 15.28 ± 1.32 mm, respectively. The 4–5 mm zoned trajectory had a SR, SAR and MSL of 77%, 7.62 ± 3.66º and 19.14 ± 2.57 mm, respectively. The 6–7 mm zoned trajectory had a SR, SAR and MSL of 81%, 8.03 ± 4.10º and 21.92 ± 2.37 mm, respectively. The maximum PR (85%) and SAR (9.57 ± 4.36º) were observed at the 5–6 mm zoned trajectory with a larger MSL (21.74 ± 2.44 mm) than the other zoned trajectories except for the 6–7 mm zoned trajectory. Obvious differences were observed in the PR and SAR measurements in the 5–6 mm zoned trajectory compared to the other zoned trajectories (p < 0.01). There were obvious differences in the MSL comparisons between the 5–6 mm zoned trajectory and the other zoned trajectories except for the 6–7 mm zoned trajectory (p < 0.01) (Table 1). The safe screw angle was found to show significant individual variations.
Table 1.
PR, SAR and MSL comparisons in the different zoned trajectories
| Entry point | 0–1 mm | 1–2 mm | 2–3 mm | 3–4 mm | 4–5 mm | 5–6 mm | 6–7 mm |
|---|---|---|---|---|---|---|---|
| PR (%) | – | – | 54 | 71 | 77 | 85 | 81 |
| SA (deg) | – | – | 68.31 ± 2.89 to 72.06 ± 2.37 | 66.36 ± 2.56 to 70.97 ± 1.84 | 55.97 ± 4.36 to 63.61 ± 3.11 | 49.68 ± 4.94 to 59.19 ± 4.70 | 47.05 ± 4.57 to 55.09 ± 4.37 |
| SAR (deg) | – | – | 3.74 ± 1.79 | 4.59 ± 1.71 | 7.62 ± 3.66 | 9.57 ± 4.36 | 8.03 ± 4.10 |
| MSL (mm) | – | – | 14.73 ± 1.30 | 15.28 ± 1.32 | 19.14 ± 2.57 | 21.74 ± 2.44 | 21.92 ± 2.37 |
Values are mean ± SD
PR pass ratio, SAR safe angle range, SA screw angle (in the axial plane), MSL screw length in the middle of safe angle
Discussion
Anatomical studies have examined the applicability of the C2 crossing laminar screw technique by performing morphometric analysis of the C2 laminae. Cassinelli et al. [2] measured the laminar thickness (LT) in the narrowest laminar section in American populations and reported that more than 70% of the specimens they studied had a LT >5 mm. Several other scholars examining the LT in Korean, Chinese and Turkish populations [7, 11, 19] came to similar conclusions: most of the specimens they examined had a LT larger than the diameter of the commonly used cervical screw (3.5 mm). Although the minimum laminar thickness required to allow for safe placement of a screw was not described, there is a common idea that a thickness >5 mm with a precise screw trajectory may be acceptable [2, 22].
Clinicians have concentrated on a screw trajectory study and introduced several technique notes and modified the methods for defining the safe screw trajectory. Wright [24] described in his initial papers, a parallel screw trajectory to the downslope of the dorsal aspect of the contralateral lamina. Cassinelli [2] recommended a slightly more dorsal trajectory that may result in slight penetration into the dorsal cortex. Andrew [1] described a modification by drilling an ‘exit window’ at the facet laminar junctions. Kabir [10] introduced a modified entry point on the ‘removed spinal process basis’ and the application of a three-dimensional navigation system [4]. However, these descriptions were based on clinical experiences. Quantitative data on the accuracy of the screw trajectory using this technique is still lacking.
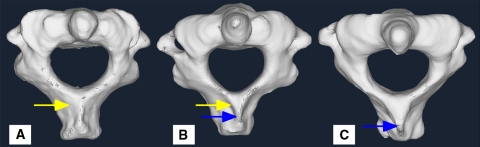
A screw trajectory is composed of two parts: an entry point and a screw angle. Since different entry points can generate different screw angles, the first step for trajectory analysis should be the location of a feasible and precise entry point. The initial entry point suggested by Wright, ‘lamina/spinal process junction, which is close to the rostral margin of the lamina’ [24], is not a constant and precise anatomical location, and there may be difficulties in locating it in some cases (Fig. 4). Kabir’s modified entry point at the ‘removed spinal process basis’ might make the screw graft placement procedure more convenient. However, both entry points lack quantitative data to demonstrate their accuracy for guiding a safe screw trajectory. In this study, every millimeter zone of the posterior part of the C2 vertebrae was tested for 3.5 mm diameter screw placement using the crossing laminar method. Three parameters were used to examine the accuracy of different zoned entry points for guiding a valid screw trajectory:
Fig. 4.
The initial entry point may be difficult to locate in some cases. a ‘Lamina/spinal process junction (yellow arrow), close to the rostral margin (blue arrow) of the lamina’, mentioned by Wright. b In this case, the ‘lamina/spinal process junction’ and ‘rostral margin of the lamina’ were at different levels. c In this case, the entry point was difficult to locate by Wright’s description because there is no an obvious boundary between the lamina and spinal process. The rostral margin is difficult to follow
1. Pass Ratio (PR): Because there is no description regarding the minimal screw length for crossing laminar fixation, it was presumed that the screw should pass through at least half of the laminar length to provide sufficient fixation strength to the atlantoaxial complex. Under this limitation, the screws guided in the 0–1 mm and 1–2 mm zoned trajectories were found have deviated into the spinal canal. The 2–3, 3–4, 4–5 and 6–7 mm zoned screws had a PR of 54, 71, 77 and 81%, respectively. The maximal PR was observed at the 5–6 mm zoned screws (85%). The zone 5–6 mm posterior to the spinal canal had a higher success rate for guiding screw placement with safety than the other zones.
2. Safe Angle Range (SAR) was defined from the minimal safe angle for the inner laminar cortex (margin of the spinal canal) to the maximum safe angle for passing the outer mid-lamina cortex. In this angle range, the screw could pass through at least a 1/2 laminar length without deviating into the spinal canal. The 5–6 mm zoned trajectory had a larger SAR (9.57 ± 4.36º) than the other zoned trajectories (2–3 mm: 3.74 ± 1.79º; 3–4 mm: 4.59 ± 1.71º; 4–5 mm: 7.62 ± 3.66º; 6–7 mm: 8.03 ± 4.10º). The screw trajectory guided in this area could be safer than in other areas due to a larger safe range for adjusting the screw angles.
3. Maximal Screw Length (MSL) is the maximal screw length that can be obtained in the screw trajectory. A trajectory with a larger MSL may provide better fixation strength to the atlantoaxial complex. The MSL in the 5–6 mm zoned trajectory (21.74 ± 2.44 mm) was larger than the MSL in the other anterior zoned trajectories. Although it was slightly smaller than the MSL in the 6–7 mm zoned trajectory (21.92 ± 2.37 mm), the statistical comparison showed no obvious difference between them.
Zone 5–6 mm posterior to the spinal canal was recommended as a more feasible and safer entry point due to the maximum PR, SAR and a larger MSL. The recommended safe screw angle was 49.68 ± 4.94 to 59.19 ± 4.70º in the axial plane. However, the safe angle range can vary considerably according to individual variance. Therefore, preoperative evaluations on MRI and three-dimensional CT images to adjust the screw angles will be essential for safe screw placement using this technique.
In addition, the PR (the screw PR for the 3.5 mm diameter screw to pass through the mid-lamina) was a theoretical datum for evaluating the accuracy of the different trajectories. It may be larger than the actual success ratio of this technique because the latter must consider the laminar tolerance of the screw. In addition, the actual screw insertion should be as deep into the C2 lamina as possible in order to obtain better fixation strength, not only passing through the mid-lamina length.
There were some limitations of this study. All specimens were selected randomly from the Digital Korean Human Model database, and only Koreans were examined. Therefore, trajectory analysis for general population is still unknown. The screw angle measurement was performed only in the axial plane. Although the screw angle in the coronal plane is not as important to the operators as it is in the axial plane, irregularities of the laminar sections in the coronal plane might cause a further decrease in the PR for safe screw fixation.
Conclusion
Quantitative trajectory analysis confirmed zone 5–6 mm posterior to the spinal canal to be a feasible and safer entry point for C2 crossing laminar screw fixation. This might provide useful guidelines for locating a valid entry point for a safe screw placement. The recommended safe screw angle was 49.68 ± 4.94 to 59.19 ± 4.70º in the axial plane. Since the safe screw angle varied considerably according to individual variance, a preoperative evaluation for adjusting the screw angle is recommended for safe screw placement using this technique.
Acknowledgments
This study was supported partially (The author are Dai-Soon Kwak and Seung-Ho Han) by National Research Foundation of Korea (KRF-2008-359-E00001, KRF-2008-314-E00002)
References
- 1.Jea A, Sheth RN, Vanni S, Green BA, Levi AD. Modification of Wright’s technique for placement of bilateral crossing C2 translaminar screws: technical note. Spine J. 2008;8(4):656–660. doi: 10.1016/j.spinee.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Cassinelli EH, Lee M, Skalak A, Ahn NU, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine. 2006;31(24):2767–2771. doi: 10.1097/01.brs.0000245869.85276.f4. [DOI] [PubMed] [Google Scholar]
- 3.Ebraheim N, Rollins JR, Jr, Xu R, Jackson WT. Anatomic consideration of C2 pedicle screw placement. Spine. 1996;21:691–695. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 4.Verlaan JJ. Placement of C2 laminar screws using three-dimensional fluoroscopy-based image guidance by Eric W. Nottmeier and Andrew B. Foy. Eur Spine J. 2008;17(4):616–617. doi: 10.1007/s00586-007-0574-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorek J, Acaroglu E, Berven S, Yousef A, Puttlitz CM. Constructs incorporating intralaminar C2 screws provide rigid stability for atlantoaxial fixation. Spine. 2005;30:1513–1518. doi: 10.1097/01.brs.0000167827.84020.49. [DOI] [PubMed] [Google Scholar]
- 6.Hong JT, Sung JH, Son BC, Lee SW, Park CK. Significance of laminar screw fixation in the subaxial cervical spine. Spine. 2008;33(16):1739–1743. doi: 10.1097/BRS.0b013e31817d2aa2. [DOI] [PubMed] [Google Scholar]
- 7.Hu Y, Xu RM, Ma WH. The feasibility study of posterior laminar screw fixation techniques in axis. Zhongguo Gu Shang. 2008;21(8):581–584. [PubMed] [Google Scholar]
- 8.Igarashi T, Kikuchi S, Sato K, Kayama S, Otani K (2003) Anatomic study of the axis for surgical planning of transarticular screw fixation. Clin Orthop 162–166 [DOI] [PubMed]
- 9.Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Kabir SM, Casey AT. Modification of Wright’s technique for C2 translaminar screw fixation: technical note. Acta Neurochir (Wien) 2009;151(11):1543–1547. doi: 10.1007/s00701-009-0459-2. [DOI] [PubMed] [Google Scholar]
- 11.Kim YJ, Rhee WT, Lee SB, You SH, Lee SY. Computerized tomographic measurements of morphometric parameters of the C2 for the feasibility of laminar screw fixation in Korean population. J Korean Neurosurg Soc. 2008;44(1):15–18. doi: 10.3340/jkns.2008.44.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lapsiwala SB, Anderson PA, Oza A, Resnick DK. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery. 2006;58(3):516–521. doi: 10.1227/01.NEU.0000197222.05299.31. [DOI] [PubMed] [Google Scholar]
- 13.Lehman RA, Jr, Dmitriev AE, Helgeson MD, Sasso RC, Kuklo TR, Riew KD. Salvage of C2 pedicle and pars screws using the intralaminar technique: a biomechanical analysis. Spine. 2008;33(9):960–965. doi: 10.1097/BRS.0b013e31816c915b. [DOI] [PubMed] [Google Scholar]
- 14.Lehman RA, Jr, Sasso RC, Helgeson MD, Dmitriev AE, Gill NW, Rosner MR, Riew KD. Accuracy of intraoperative plain radiographs to detect violations of intralaminar screws placed into the C2 vertebrae: a reliability study. Arch Orthop Trauma Surg. 2009;129(1):25–27. doi: 10.1007/s00402-007-0510-9. [DOI] [PubMed] [Google Scholar]
- 15.Mandel IM, Kambach BJ, Petersilge CA, Johnstone B, Yoo JU. Morphologic considerations of C2 isthmus dimensions for the placement of transarticular screws. Spine. 2000;25:1542–1547. doi: 10.1097/00007632-200006150-00014. [DOI] [PubMed] [Google Scholar]
- 16.Matsubara T, Mizutani J, Fukuoka M, Hatoh T, Kojima H, Otsuka T. Safe atlantoaxial fixation using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery: case report. Spine (Phila Pa 1976) 2007;32(1):E30–E33. doi: 10.1097/01.brs.0000250994.24462.ec. [DOI] [PubMed] [Google Scholar]
- 17.Nakanishi K, Tanaka M, Sugimoto Y, Ozaki T. Posterior cervical spine arthrodesis with laminar screws: a report of two cases. Acta Med Okayama. 2007;61(2):115–119. doi: 10.18926/AMO/32889. [DOI] [PubMed] [Google Scholar]
- 18.Sciubba DM, Noggle JC, Vellimana AK, Conway JE, Kretzer RM, Long DM, Garonzik IM. Laminar screw fixation of the axis. J Neurosurg Spine. 2008;8(4):327–334. doi: 10.3171/SPI/2008/8/4/327. [DOI] [PubMed] [Google Scholar]
- 19.Senoğlu M, Ozbağ D, Gümüşalan Y. C2 intralaminar screw placement: a quantitative anatomical and morphometric evaluation. Turk Neurosurg. 2009;19(3):245–248. [PubMed] [Google Scholar]
- 20.Sugimoto Y, Tanaka M, Nakanishi K, Misawa H, Takigawa T, Ito Y, Ozaki T. Safety of atlantoaxial fusion using laminar and transarticular screws combined with an atlas hook in a patient with unilateral vertebral artery occlusion (case report) Arch Orthop Trauma Surg. 2009;129(1):25–27. doi: 10.1007/s00402-007-0510-9. [DOI] [PubMed] [Google Scholar]
- 21.Tabaraee E, O’Brien JR, Yu WD. Use of C1 lateral mass and C2 intralaminar fixation to stabilize a 30-year-old odontoid fracture that was causing myelopathy. Am J Orthop. 2009;38(4):E78–E81. [PubMed] [Google Scholar]
- 22.Wang MY (2006) C2 crossing laminar screws: Cadaveric morphometric analysis. Neurosurgery 59(1 Suppl 1):59 [DOI] [PubMed]
- 23.Wang MY (2007) Cervical crossing laminar screws: Early clinical results and complications. Neurosurgery 61(5 Suppl 2):311-315 [DOI] [PubMed]
- 24.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004;17:158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]