Abstract
Lateral whole-spine radiography is a useful tool in the management of spinal deformity, but the most appropriate arm position during radiography has yet to be determined. In this prospective study, we evaluated 26 adult volunteers and 22 patients with lumbar spinal canal stenosis. Lateral whole-spine radiographs were acquired in the most stable and relaxed position while the subjects were standing with their arms extended and their hand gently clasped in front of the trunk (clasped position). The following parameters were measured: sagittal vertical axis (SVA), lumbar lordotic angle (LLA), pelvic angle (PA), pelvic lordosis angle (PRS1), pelvic tilt (PT), and pelvic incidence (PI). The reliability of measurements was assessed by interclass correlation coefficients. The SVA was slightly positive in volunteers. LLA, PA, PRS1, PT, and PI were compatible with standard normal values. The results showed “almost perfect agreement” with regard to intra- and interobserver reliability. The clasped position can be used effectively and reliably for measurement of sagittal spinal alignment for the lumbar region in adults.
Keywords: Sagittal spinal alignment, Arm position, Sagittal vertical axis, Clasped position
Introduction
Sagittal spinal alignment is an important aspect for the clinician to consider in the evaluation and treatment of spinal deformities. Global sagittal spinal alignment is described by a plumb line dropped from the center of the C7 vertebral body [8]. Studies in normal adult subjects indicate that the typical sagittal vertical axis (SVA) is neutral or slightly positive [9, 15]. Aging is associated with a decrease in spinal mobility and lumbar lordosis, as well as pelvic backtilt and forward bending trunk [4, 5, 18]. Optimally, the standing position during radiographic acquisition is functionally representative of relaxed standing posture. Though relaxed standing is a functional and easily assumed position, the presence of the arms on the sides prohibits adequate radiographic visualization of the spinal landmarks. Standing with the arms forward flexed to allow radiographic visualization of the spine results in negative shift of SVA [3, 6, 15, 21]. There is no general agreement on the most appropriate arm position when taking a lateral whole-spine radiograph.
The aim of the present study was to evaluate the reliability of our technique, clasped position, in the measurement of spinal sagittal alignment, and in addition, to determine if the position represents a functional stance for accurate sagittal balance evaluation.
Materials and methods
This prospective study included 26 adult volunteers (15 males and 11 females) and 22 consecutive patients with lumbar spinal canal stenosis (LSCS) (12 males and 10 females). The average age of volunteers was 32.7 years (range 22–51) and for patients was 62.0 years (range 25–82). All human subjects had lateral long cassette radiographs of the whole-spine performed in the most stable and relaxed position while the subjects were standing with their arms extended and their hand gently clasped in front of the trunk (clasped position) (Fig. 1). To evaluate radiographic parameters in the most natural upright posture of each subject, the position of the lower limbs was not standardized. Two radiographs were taken 1–4 weeks apart. The radiographs were measured twice by the first observer (HS, experienced spine surgeon), then independently measured at other days by a second observer (JM, resident, orthopedic surgery).
Fig. 1.
Clinical picture (a) and lateral whole-spine radiograph (b) in clasped position
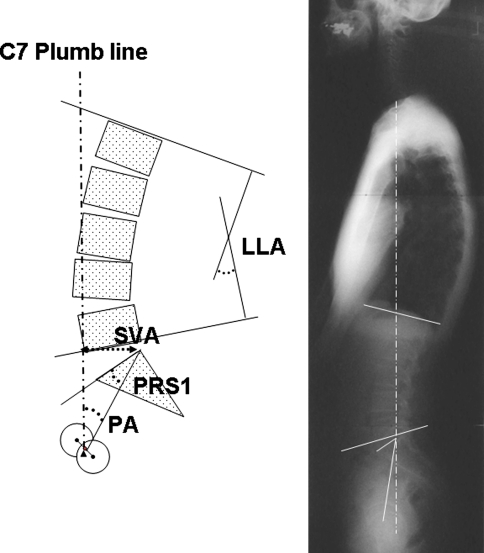
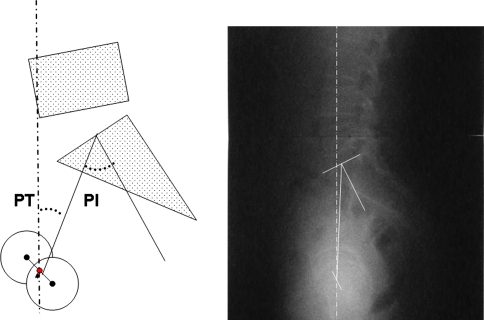
On unmarked X-rays, the following radiographic parameters were measured manually as described previously [7, 11, 14, 22]: SVA (defined as the distance between the C7 plumb line and the posterior superior corner on the superior margin of S1), lumbar lordotic angle (LLA, the angle from the upper endplate of L1 to the lower end plate of L5), pelvic angle (PA, the angle between the line connecting the posterior superior corner of S1 to the bicoxofemoral axis and the vertical plane), pelvic lordosis angle (PRS1, the angle between the line connecting the posterior superior corner of the S1 to the bicoxofemoral axis and the upper endplate of S1), pelvic tilt (PT, the angle between the line connecting the midpoint of the sacral plate to the axis of the femoral heads, and the vertical), and pelvic incidence (PI, the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting the point to the middle axis of the femoral heads) (Figs. 2, 3).
Fig. 2.
Measurements of spinal and pelvic sagittal balance. SVA sagittal vertical axis, LLA lumbar lordotic angle, PA pelvic angle, PRS1 pelvic morphologic angle
Fig. 3.
Measurements of spinal and pelvic sagittal balance. PT pelvic tilt, PI pelvic incidence
Values were expressed as mean ± SD. The measurements were tabulated and analyzed using Excel (Microsoft, Redmond, WA). The reliability of measurement was analyzed by using intraclass correlation coefficients (ICC) and 95% confidence interval (95% CI) [19]. The ICC values were interpreted according to the Landis-defined categories for the interpretation of the kappa [13]; values from 0 to 0.2 represent slight agreement, 0.2 to 0.4 are fair agreement, 0.4 to 0.6 indicate moderate agreement, 0.6 to 0.8 show substantial agreement, and 0.8 to 1.0 represent almost perfect agreement.
The study protocol was approved by the Human Ethics Review Committee of Tokyo Medical University and a signed consent form was obtained from each subject.
Results
The SVA was slightly positive in normal adult subjects (2.3 ± 18.6 mm), which was similar to the reported age-matched normal values [1, 16, 17]. The LLA, PA, PRS1, PT, and PI of the normal subjects were also similar to the standard values matched by age for Japanese (Table 1). Patients with LSCS had larger SVA, smaller LLA, larger PA, and similar PRS1, compared with the respective values of the adult volunteers (Table 1), and these results were comparable with our previous report [20].
Table 1.
Sagittal parameters for adult volunteers and patients with lumbar spinal canal stenosis (LSCS)
| Adult volunteers | Age-adjusted standard values to adult volunteers | Patients with LSCS | |
|---|---|---|---|
| n | 26 | 22 | |
| Age (years) | 32.7 ± 8.3 | 62.0 ± 15.4 | |
| SVA (mm) | 2.3 ± 18.6 | 6.1 ± 24.1a | 32.8 ± 41.5 |
| 14 ± 19b | |||
| LLA (°) | 46.8 ± 11.5 | 44.3 ± 12.5a | 26.2 ± 10.9 |
| PA (°) | 17.9 ± 5.8 | 19.4°c | 26.3 ± 9.8 |
| PRS1 (°) | 37.1 ± 9.9 | 35.5°c | 34.6 ± 8.9 |
| PT (°) | 11.3 ± 9.4 | 10.8 ± 5.5d | 21.0 ± 9.8 |
| PI (°) | 46.3 ± 11.1 | 46.7 ± 8.7d | 49.7 ± 10.4 |
The ICC value of SVA, LLA, PA, PRS1, PT, and PI were as follows: intrarater reliability of normal subjects 0.84 (95% CI 0.68–0.92), 0.92 (95% CI 0.84–0.96), 0.89 (95% CI 0.77–0.95), 0.92 (95% CI 0.83–0.96), 0.97 (95% CI 0.94–0.99), and 0.97 (95% CI 0.93–0.99), intrarater reliability of patients 0.86 (95% CI 0.64–0.97), 0.91 (95% CI 0.80–0.96), 0.86 (95% CI 0.78–0.90), 0.90 (95% CI 0.77–0.96), 0.93 (95% CI 0.85–0.97), and 0.94 (95% CI 0.86–0.98), interrater reliability of volunteers 0.95 (95% CI 0.90–0.98), 0.97 (95% CI 0.94–0.99), 0.93 (95% CI 0.85–0.97), 0.98 (95% CI 0.96–0.99), 0.97 (95% CI 0.88–0.97), and 0.96 (95% CI 0.92–0.98), respectively (Tables 2, 3). The intra- and interobserver agreement rates with measurements in clasped position were high, i.e., all results showed ‘almost perfect agreement’.
Table 2.
Intrarater reliability of measurements
| Adult volunteers | Patients with LSCS | |||
|---|---|---|---|---|
| ICCa | 95% CIb | ICCa | 95% CIb | |
| SVA | 0.84 | 0.68–0.92 | 0.86 | 0.64–0.97 |
| LLA | 0.92 | 0.84–0.96 | 0.91 | 0.80–0.96 |
| PA | 0.94 | 0.87–0.97 | 0.86 | 0.78–0.90 |
| PRS1 | 0.92 | 0.83–0.96 | 0.90 | 0.77–0.96 |
| PT | 0.97 | 0.94–0.99 | 0.93 | 0.85–0.97 |
| PI | 0.97 | 0.93–0.99 | 0.94 | 0.86–0.98 |
aICC: intraclass correlation coefficients
b95% CI: 95% confidence interval
Table 3.
Interrater reliability of measurements
| Adult volunteers | ||
|---|---|---|
| ICCa | 95% CIb | |
| SVA | 0.95 | 0.90–0.98 |
| LLA | 0.97 | 0.94–0.99 |
| PA | 0.93 | 0.85–0.97 |
| PRS1 | 0.98 | 0.96–0.99 |
| PT | 0.97 | 0.88–0.97 |
| PI | 0.96 | 0.92–0.98 |
aICC: intraclass correlation coefficient
b95% CI: 95% confidence interval
Discussion
In the present study, the SVA values of adult volunteers were not negative in clasped position, and the spinopelvic parameters were similar to the normal values for age-matched Japanese [1, 12, 16, 17], with high reliability comparable to the findings of other studies [1, 7, 11] (Table 4). Data of patients with LSCS also showed high agreement (Table 2).
Table 4.
Reliability of sagittal parameters in the clasped position and other positions
| Clasped position | 90° of shoulder flexion | 45° of shoulder flexion | ||||
|---|---|---|---|---|---|---|
| Intrarater | Interrater | Intrarater | Interrater | Intrarater | Interrater | |
| SVA | 0.84 | 0.86 | 0.52–0.96a | 0.78–0.94a | N/A | N/A |
| LLA | 0.92 | 0.91 | 0.95–0.98a | 0.97a | 0.88c | 0.97c |
| PA | 0.94 | 0.86 | 0.96–0.99a | 0.98–0.99a | N/A | N/A |
| PRS1 | 0.92 | 0.90 | 0.95b | 0.88b | N/A | N/A |
| PT | 0.97 | 0.93 | N/A | N/A | 0.99c | 0.99c |
| PI | 0.97 | 0.94 | 0.98b | 0.90b | 0.99c | 0.98c |
When taking a lateral whole-spine radiograph, the best body position is close to the relaxed standing position with good reliability and good visualization of the spine. Several studies have examined the effects of arm position on radiographic measurements of sagittal spinal alignment [3, 6, 15, 21]. Vedantam et al. [21] observed differences in SVA at 30° and 90° of shoulder flexion, and they recommended the position of 30° shoulder flexion because of a less negative shift in SVA. The negative shift in SVA was a consistent finding when a subject stood with 45° shoulder flexion relative to relaxed standing [15]. When subjects have a designated standing base to position the feet and an arm support to standardize their arm flexion angle, the positioning does not standardize the distribution of weight or center of mass, which may affect sagittal parameters [3]. While Faro et al. [3] proposed fists on clavicles position, which offered less negative SVA than 45° of shoulder flexion, Aota et al. [1] reported a negative shift of SVA even in fists on clavicles position compared to relaxed standing with arms-at-side. Raising arms with shoulder flexion could theoretically result in a posterior shift of the trunk to counterbalance the lever arm [21]. Elbow flexion with placement of both fists on the ipsilateral clavicles could be accompanied by some shoulder flexion, which causes a negative shift of SVA. In the present study, the clasped position offered slightly positive value for SVA, which is compatible with the value in relaxed standing with arms-at-side [1]. The spinopelvic parameters measured at the clasped position were similar to the normal values for age-matched Japanese subjects [1, 12, 13].
The reliability of the SVA measurement was questioned by Jackson et al. [10] because of poor visualization of the C7 vertebra on lateral whole-spine radiographs with 90° of shoulder flexion. On the other hand, Horton et al. [6] reported that the 90° position was inferior to the fists on clavicles position for visualizing the vertebral landmarks. Although we are under the impression that the visualization of key vertebral landmarks with the clasped position is comparable to other arm positions, further studies are needed. However, the reliability for SVA is generally high, suggesting that the variability lies in the actual sagittal balance rather than measurement of the SVA [4, 6, 21].
In conclusion, for evaluation of sagittal spinal alignment for the lumbar region in adults, the clasped position is comparable to relaxed standing position and can be easily achieved without added equipment, with high reliability.
Acknowledgments
The authors thank Dr. F.G. Issa (http://www.word-medex.com.au) for careful reading and editing of the manuscript. No funds were received to conduct this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Aota Y, Saito T, Uesugi M, et al. Does fists-on-clavicles position represent a functional standing position? Spine. 2009;34:808–812. doi: 10.1097/BRS.0b013e31819e2191. [DOI] [PubMed] [Google Scholar]
- 2.Dimar JR, II, Carreon LY, Labelle H, et al. Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur Spine J. 2008;17:1373–1379. doi: 10.1007/s00586-008-0755-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faro FD, Marks MC, Pawelek J, et al. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine. 2004;29:2284–2289. doi: 10.1097/01.brs.0000142224.46796.a7. [DOI] [PubMed] [Google Scholar]
- 4.Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]
- 5.Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech. 2003;16:44–50. doi: 10.1097/00024720-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Horton WC, Brown CW, Bridwell KH, et al. Is there an optimal patient stance for obtaining a lateral 36″ radiograph? A critical comparison of three techniques. Spine. 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 7.Jackson RP, Hales C. Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers. Spine. 2000;25:2808–2815. doi: 10.1097/00007632-200011010-00014. [DOI] [PubMed] [Google Scholar]
- 8.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 9.Jackson RP, Peterson MD, McManus AC, et al. Compensatory spinopelvic balance over the “hip axis” and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine. 1998;23:1750–1767. doi: 10.1097/00007632-199808150-00008. [DOI] [PubMed] [Google Scholar]
- 10.Jackson RP, Kanemura T, Kawakami N, et al. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Jackson RP, Phipps T, Hales C, et al. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28:151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Kanemura T, Imagama S, et al. Spino-pelvic alignment in an asymptomatic Japanese population—mean and variance of upright thoracolumbar spino-pelvic alignment in Japanese. J Joint Surg. 2009;28:558–567. [Google Scholar]
- 13.Landis JR, Koch CG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 14.Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marks MC, Stanford CF, Mahar AT, et al. Standing lateral radiographic positioning does not represent customary standing balance. Spine. 2003;28:1176–1182. doi: 10.1097/00007632-200306010-00018. [DOI] [PubMed] [Google Scholar]
- 16.Matsuoka H, Komagata M, Nishiyama M, et al. Radiographic assessment of sagittal spinal alignment to correlate standards classified by age and low back pain. J Tokyo Med Univ. 2004;62:64–71. [Google Scholar]
- 17.Ochiai J, Kanzaki K, Saito G, et al. The study of sagittal alignment for Japanese. J Jpn Soc Spine Surg Relat Res. 2006;17:274. [Google Scholar]
- 18.Schwab F, Lafage V, Boyce R, et al. Gravity line analysis in adult volunteers. Age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine. 2006;31:E959–E967. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 19.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki H, Endo K, Kobayashi H, et al. Correlation of sagittal spinal alignment with clinical symptoms in lumbar canal stenosis. J Lumbar Spine Disord. 2008;14:23–27. doi: 10.3753/yotsu.14.23. [DOI] [Google Scholar]
- 21.Vedantam R, Lenke LG, Bridwell KH, et al. The effect of variation in arm position on sagittal spinal alignment. Spine. 2000;25:2204–2209. doi: 10.1097/00007632-200009010-00011. [DOI] [PubMed] [Google Scholar]
- 22.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg (Am) 1983;65:768–772. [PubMed] [Google Scholar]