Abstract
The objective of the study was to describe the technique, accuracy of placement and complications of transpedicular C2 screw fixation without spinal navigation. Patients treated by C2 pedicle screw fixations were identified from the surgical log book of the department. Clinical data were extracted retrospectively from the patients’ charts. Pedicle screw placement accuracy was assessed on postoperative CT scans according to Gertzbein and Robbins (GRGr). A total of 27 patients were included in the study. The mean age of the patients was 56 ± 22.0 years; 51.9% of them were female. As much as 17 patients suffered from trauma, 5 of degenerative disease, 3 of inflammations and 2 of metastatic disease. A total of 47 C2 transpedicular screw fixations were performed. The canulated screws were inserted under visual control following the preparation of the superior surface of the isthmus and of the medial surface of the pedicles of the C2. Intraoperative fluoroscopy was additionally used. The postoperative CT findings showed in 55.3% GRGr 1, in 27.7% GRGr 2, in 10.6% GRGr 3, and in 6.3% GRGr 4 pedicle screw insertion accuracy. Screw insertions GRGr 5 were not observed. Screw malpositioning (i.e., GRGr 3 and 4) was significantly associated with thin (<5 mm) pedicle diameters and with surgery for C2 fractures. In the three patients with screw insertions GRGr 4, postoperative angiographies were performed to exclude vertebral artery affections. In one of these three cases, the screw caused a clinically asymptomatic vertebral artery compression. Hardware failures did not occur. In one patient, postoperative pneumonia resulted in the death of the patient. Careful patient selection and surgical technique is necessary to avoid vertebral artery injury in C2 pedicle screw fixation without spinal navigation. A slight opening of the vertebral artery canal (Gertzbein and Robbins grade ≤3) does not seem to put the artery at risk. However, the high rate of misplaced screws when inserted without spinal navigation, despite the fact that no neurovascular injury occurred, supports the use of spinal navigation in C2 pedicle screw insertions.
Keywords: C2 pedicle screw, Placement accuracy, Vertebral artery, Spinal navigation
Introduction
Instability of the upper cervical spine resulting from inflammatory, traumatic, congenital, neoplastic or degenerative disorders may require instrumentation involving the axis [3]. C2 fixation techniques include Gallie [4], Brooks [1] and Sonntag-type interlaminar wiring techniques, the laminar clamp [18], the Magerl C1/2 transarticular screw [17], the C2 pedicle screw technique [6–8, 22, 25] and the C2 intralaminar screw technique [16, 27, 28]. Due to its anatomy and proximity to neural and vascular structures, screw fixations of C2 are generally considered to be demanding.
Biomechanically, transarticular C1/2 screws are superior to wiring and clamp techniques [20]. However, due to the flat trajectory of the screw (as compared to the longitudinal axis of the spine), transarticular C1/2 screw insertion can be a challenging procedure. C1 lateral mass screws rod-connected to C2 pedicle screws have been shown to be biomechanically equivalent [15, 19] or superior [21] to transarticular screws. Thus, transpedicular C2 screw fixation, with its more convenient screw handling, is a valid alternative to C1/C2 transarticular fixation.
Spinal navigation has been shown to improve pedicle screw placement accuracy [12]. However, spinal navigation consumes resources (e.g., it is time consuming) and economical limitations may be a current problem. Due to the good intraoperative anatomical orientation, C2 pedicle screw fixation may be feasible without the use of spinal navigation.
To assess the above-mentioned hypothesis, we describe the technique, accuracy of placement and complications of C2 pedicle screw fixation without the use of spinal navigation in a consecutive series of patients with disorders of the upper cervical spine.
Materials and methods
Patient selection
Patients operated with C2 pedicle screw fixation were identified from the surgical log book of the department. The following data were extracted retrospectively from the patients’ charts: age, gender, type of surgery, duration of surgery, blood loss, blood transfusions performed, complications and their treatment, including hardware failure (defined as screw pull-out with loss or impending loss of stability, clinically symptomatic or not), accuracy of pedicle screw placement and pedicle diameter.
Surgical technique
Prior to surgery, the diameter of the pedicles of the C2, as well as the course of the vertebral artery canal, must be carefully assessed on the C2 computed tomograms with additional sagittal and coronal reconstructions, to ensure that pedicle screws can be placed without bursting a possibly too narrow pedicle or opening the vertebral artery canal.
The patient is placed in a prone position. The head rests in a Mayfield clamp. Lateral fluoroscopy is used to verify alignment and position of the upper cervical spine. The cervical spine is exposed subperiostally according to the segments to be fused.
The dorsal surface of the interarticular part of C2 (isthmus) is prepared from the C1/2 to the C2/3 articular surfaces. Additionally, the medial surfaces of the interarticular part of C2 and of its pedicle, bordering the spinal canal anteriorly to the vertebral body of C2, are prepared.
The entry point for the C2 pedicle screw is the cranial and medial quadrant of the isthmus surface of C2, near the intersection point of the two lines demarking the quadrants.
The pilot hole is drilled with a K-wire directed at a 20°–30° angle in a lateral to medial and cephalad trajectory. The medial as well as cephalad orientations of the K-wire are controlled visually, in line with the dissected medial and superior surfaces of the isthmus and pedicle. The trajectory of the K-wire must be parallel to the flat cranial surface of the isthmus/pedicle and tangential to the curved medial surface of the isthmus/pedicle. In addition, the cephalad orientation is controlled by lateral fluoroscopy.
The integrity of the walls of the pilot hole is verified with a blunt probe. Cannulated screws (Neon, Ulrich Medical, Ulm, Germany) of an appropriate length are inserted monocortically in C2. Contoured longitudinal rods are fastened with a connector to the screw heads and secured in position as required.
In all the patient, early postoperative computed tomographies of the cervical spine for screw placement control are routinely carried out. Follow-up also includes radiographs at an early stage postoperatively, at 3 and 9 month and 2 years postoperatively.
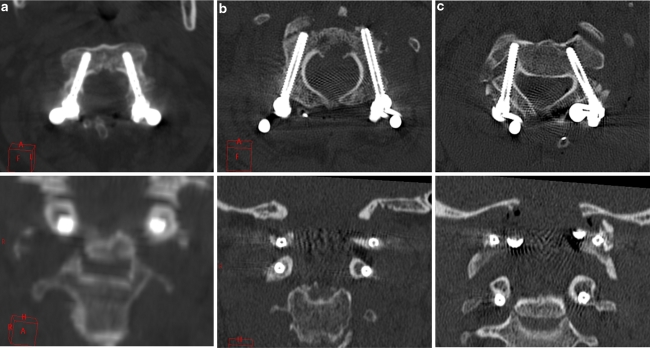
Pedicle screw placement accuracy and involvement of vertebral artery canal
Pedicle screw placement accuracy was assessed on postoperative CT scans according to Gertzbein and Robbins [5] and Kosmopoulos and Schizas [12]. In this classification, screws are rated as follows: perfectly within the pedicle (GRGr 1); perforating the pedicle wall by less than 2 mm (GRGr 2); perforating the pedicle wall by more than 2 mm, but less than 4 mm (GRGr 3); perforating the pedicle wall by more than 4 mm, but less than 6 mm (GRGr 4); and perforating the pedicle wall by more than 6 mm (GRGr 5) (Fig. 1).
Fig. 1.
a Axial and coronal view of C2 pedicle screw placement, on both sides of GRGr 1. b Axial and coronal view of C2 pedicle screw placement, on the right side of GRGr 1, on the left side of GRGr 3. c Axial and coronal view of C2 pedicle screw placement, on the right side of GRGr 4, on the left side of GRGr 2. In the postoperative angiography, there was only vertebral artery affection, but no occlusion
If the screws perforated the pedicle wall, they always did so laterally toward the vertebral artery canal. Thus, the GRGr classification simultaneously described the degree of the pedicle screw effect on the vertebral artery canal, not necessarily on the vertebral artery.
Measurement of the pedicle diameter
The pedicle diameter was defined according to Karaikovic et al. [11] as the narrowest mediolateral diameter of the pedicle of C2. It was measured from the preoperative axial CT scans with scale paper and magnifying lens by two of the authors individually. Measurement differences of ≤1 mm were averaged, while differences of >1 mm resulted in a new measurement.
Statistical analysis
As previously suggested, for statistical analysis, we split the patient population into two groups: Gertzbein and Robins group 1 and 2 (GRGr 1 + 2) versus Gertzbein and Robins group 3 and 4 (GRGr 3–4) [2].
Chi-square test, non-parametric Mann–Whitney test and multiple logistic regression analysis were used for statistical analysis of data. Results were considered significant at the p < 0.05 level. The analyses were performed using the software SPSS 17.
Results
The study comprised 27 successive patients. As much as 17 (62.9%) patients were operated on for trauma, 5 (18.5%) for degenerative diseases, 3 (11.1%) for infectious diseases and 2 (7.4%) for metastatic diseases.
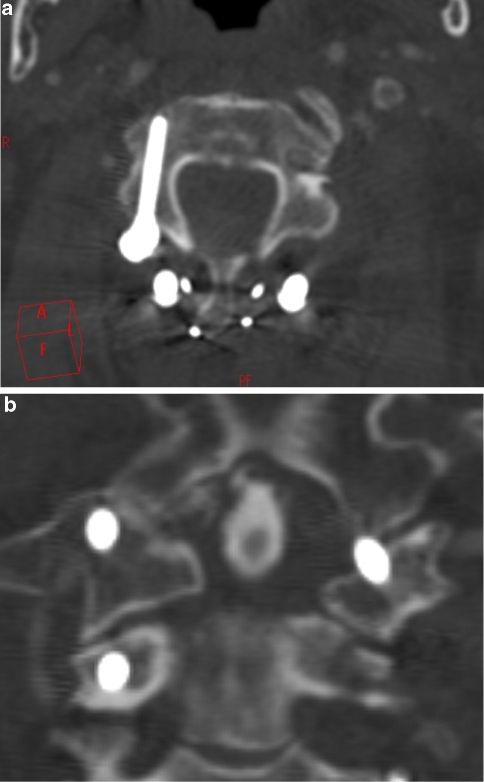
In these 27 patients, 47 C2 transpedicular screw insertions were carried out. In seven patients, a transpedicular screw was inserted only on one side: in five of these cases due to a high-riding vertebral artery (Fig. 2), in one case due to metastasis in one of the pedicles, and in one case due to a too narrow pedicle diameter.
Fig. 2.
A 78-year-old patient with dense and left lateral mass fracture, in the preoperative CTA detection of a traumatic affection involvement of the vertebral artery of the left side. Intraoperatively, high-riding vertebral artery and abandonment of C2 pedicle screw insertion on the left side. a Axial C2 pedicle screw placement in GRGr group 1, b coronal C2 pedicle screw placement in GRGr group 1
A total of 26 (55.3%) screws had a placement accuracy of GRGr 1, 13 (27.7%) screws of GRGr 2, 5 (10.6%) screws of GRGr3 and 3 (6.3%) screws of GRGr 4. No GRGr 5 placement accuracy was observed. The preoperative findings of the patients are shown in Table 1. Preoperative C2 fractures and smaller pedicle diameters were significantly (p = 0.005) more often found in patients with pedicle screws placed with GRGr 3 and 4 accuracy.
Table 1.
Preoperative findings in 27 patients with 47 screws
| Variable | GRGr 1 + 2 (n = 39) | GRGr 3 + 4 (n = 8) | p |
|---|---|---|---|
| Age [median (range)] | 58.00 (7; 89) | 74.00 (29; 89) | 0.308 |
| Gender [(male (%)] | 19 (48.7) | 6 (75) | 0.179 |
| C2# type II [n (%)] | 22 (56.4) | 6 (75) | 0.005 |
| Other pathologies [n (%)] | 17 (43.59) | 2 (25) | – |
| Pedicle diameter in mm (median [range]) | 6.5 [4.50; 8.25] | 4.7 [4; 6.50] | 0.005 |
GRGr Gertzbein and Robbins group
The operative findings are summarized in Table 2. No significant difference in the number of laminectomies performed, duration of surgery, in estimated blood loss or transfusion rates was found between the two patient groups (i.e., GRGr 1 and 2 vs. GRGr 3 and 4).
Table 2.
Intraoperative data in 27 patients with 47 screws
| Variable | GRGr 1 + 2 (n = 39) | GRGr 3 + 4 (n = 8) | p |
|---|---|---|---|
| Number of laminectomies (median [range]) | 1 [1, 2] | 2 [1, 2] | 0.086 |
| Duration of surgery [mean ± SD (min)] | 179.4 ± 51.56 | 182.5 ± 31.39 | 0.842 |
| Blood loss [mean ± SD (ml)] | 747 ± 533.47 | 862.5 ± 542.31 | 0.286 |
| Transfusion rate (%) | 12.8 | 12.5 | 0.980 |
GRGr Gertzbein and Robbins group
The overall complication rate was 10.6%. The complications are summarized in Table 3. No statistically significant difference was found between overall complication rates of the two patients groups. Postoperative meningitis, wound infection and CSF fistula occurred only in patients grouped GRGr 1 and 2. In the three patients grouped GRGr 4, a postoperative angiography was performed to exclude involvement of vertebral artery by the screw. In one of these three cases, the screw caused a clinically asymptomatic vertebral artery compression. In one patient, postoperative pneumonia resulted in the death of the patient. Hardware failures did not occur.
Table 3.
Complications (multiple nominations possible)
| Variable | GRGr 1 + 2 (n = 39) | GRGr 3–4 (n = 8) | p |
|---|---|---|---|
| Overall: 10.6% | 10.25 | 12.5 | 0.853 |
| Surgical complications (%) | 5.1 | 12.5 | 0.442 |
| Vertebral artery compression (%) | 0 | 12.5 | – |
| Meningitis (%) | 2.5 | 0 | – |
| Wound infection | 2.5 | 0 | – |
| CSF fistula (%) | 2.5 | 0 | – |
| Hardware failure (%) | 0 | 0 | – |
| Medical complications (%) | 2.5 | 0 | – |
| Pneumonia (%) | 2.5 | 0 | – |
| Operative mortality (%) | 2.5 | 0 | – |
The influence of preoperative diagnosis, pedicle diameter, duration of surgery and time point of surgery (i.e., at the beginning or at the end of the study period) on the accuracy of screw placement (i.e., GRGr 1 and 2 vs. GRGr 3 and 4) was assessed by logistic regression analysis. Of these variables, thin pedicle diameters were significantly associated with screw malpositioning (i.e., GRGr 3 and 4).
Discussion
Pedicle screw instrumentation is common in the lumbar and thoracic spine, while it remains less common in the cervical spine, including at the C2 level.
The small dimensions of the cervical pedicles and the proximity of vascular and neural structures may explain this reservation. However, pedicle screw instrumentation results in a superior biomechanical stability compared to lateral mass screw fixation [9, 14].
The use of spinal navigation has been shown to improve the accuracy of pedicle screw placement, also in the cervical spine [10, 12, 13, 23, 24]. However, whether this improvement of screw placement accuracy actually translates into a lower incidence of screw placement-associated complications (e.g., need for screw repositioning, incidence of vascular and neurological injury) remains unclear. Also spinal navigation has drawbacks, such as accumulating costs, time consumption, reliability and inherent accuracy limitations; navigation improves intraoperative orientation, while it cannot replace anatomical knowledge and surgical experience. We chose to place C2 pedicle screws without the use of spinal navigation mainly because we found this procedure to be time consuming and laborious, while a clear anatomy of the above-described pedicle screw insertion technique seemed to make it feasible without navigation.
In our present series of C2 pedicle screw placement without use of spinal navigation, 82.9% of the screws were considered to be located accurately (GRGr 1 and 2). In another clinical study, 94.6% of the C2 pedicle screws placed without use of spinal navigation were found to be located accurately [26]. These figures do appear more favorable than ours. The difference may be explained at least in part by the different pedicle screw placement assessment methods: a meta-analysis of pedicle screw placement accuracy over the whole spine disclosed a drop of the quota of accurately placed screws from 91.3 to 86.7%, when looking only at studies specifically stating how pedicle screw placement accuracy was assessed [12]. No further studies addressing the accuracy of C2 pedicle screw placements are available. In their pioneering work, Harms and Melcher [8] and Goel et al. [6], did not state their relevant findings. In a meta-analysis of transpedicular cervical screw insertions (levels not specified), 93.3% of the screws inserted without, and 99.4% of the screws placed with spinal navigation, were found to be placed accurately [12]. In the present study, no screw had to be repositioned due to gross screw misplacement. Screw placement-associated morbidity did not occur. Also in the studies of Goel and Laheri [7], Harms and Melcher [8] and Stulik et al. [26], no screw replacements were considered to be necessary due to gross screw misplacement. Screw-related vascular and neurological complications were not reported. However, in Goel’s series, arterial bleeding occurred in 2.5% of the patients probably due to damage of the vertebral artery [6]. Postoperative angiographies were not performed in these cases.
Thus, it remains unclear whether the higher accuracy of the screw placement reported in literature in spinal navigation-aided instrumentation does in fact lead to a lower incidence of screw replacements and screw placement-associated neurological and vascular morbidity. However, it is probably prudent to assume so, until appropriate studies addressing this issue become available. In the present study, the risk of pedicle screw misplacement (i.e., GRGr 3 and 4) significantly increased in patients with pedicle diameters <5 mm. Thus, in these cases of narrow pedicles, either spinal navigation or an alternative fixation technique might be used. The C2 laminar screw fixation offers a slightly reduced biomechanical rigidity compared to transpedicular fixation, while isthmus (“lateral mass”) screws offer about half of the rigidity of pedicle screws.
Notably, in this study, screws perforating the pedicle wall (i.e., GRGr 2–4), always did so laterally (toward the vertebral artery canal) and not medially (toward the spinal canal). This can be explained by the surgical technique used: the isthmus and the medial surface of the C2 pedicle were always visualized during the drilling of the pilot hole, making disruption of the medial pedicle wall unlikely. Despite the fact that 44.6% of the screws opened the vertebral artery canal (i.e., GRGr 2–4), no tearing/disruption of the vertebral artery occurred. Possibly, this can be explained by the surgical technique used. In screws classified as GRGr 2 and 3, the thin (diameter 2 mm) K-wire that was used probably did not open the lateral pedicle wall. The lateral wall was opened by the cannulated screw (diameter 4 mm) advanced over the K-wire, thus potentially pushing a nearby vertebral artery aside without disrupting it. In screws classified GRGr 4, the K-wire passed through the vertebral artery canal. However, the probability of disrupting the artery with a thin K-wire is lower than with the use of a thick spiral drill. If the K-wire passes through the vertebral artery canal without puncture of the artery, the screw advanced over the K-wire will push the vertebral artery aside and will dislocate or compress rather than disrupt it, as happened in one of our screws classified GRGr 4.
In order to not jeopardize the vertebral artery, in six patients, due to the small diameter of the C2 pedicles disclosed by the preoperative CT scans, preoperatively the decision was taken not to cannulate the pedicles. In a seventh patient, due to the massive destruction of the pedicle by a metastasis, preoperative decision was taken not to incannulate the pedicle, because the screw would not offer any stability.
The main advantage of this study is that it thoroughly analyses the technique and complications of transpedicular C2 screw fixation without use of spinal navigation in a well-documented homogenous series of patients. The main disadvantage of this study is its retrospective character and the relatively low patient numbers.
Conclusions
Careful patient selection and surgical technique are necessary to avoid vertebral artery injury in C2 pedicle screw fixation without spinal navigation. However, a slight opening of the vertebral artery canal (Gertzbein and Robbins grade ≤3) does not seem to put the artery at risk. The high rate of misplaced screws when inserted without spinal navigation, despite the fact that no neurovascular injury occurred, supports the use of spinal navigation in C2 pedicle screw insertions.
References
- 1.Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60:279–284. [PubMed] [Google Scholar]
- 2.Ebraheim N, Rollins JR, Jr, Xu R, Jackson WT. Anatomic consideration of C2 pedicle screw placement. Spine. 1996;21:691–695. doi: 10.1097/00007632-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 3.Fried LC. Atlanto-axial fracture–dislocations. Failure of posterior C1 to C2 fusion. J Bone Joint Surg Br. 1973;55:490–496. [PubMed] [Google Scholar]
- 4.Gallie WE. Skeletal traction in the treatment of fractures and dislocations of the cervical spine. Ann Surg. 1937;106:770–776. doi: 10.1097/00000658-193710000-00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002;51:1351–1356. doi: 10.1097/00006123-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 8.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 9.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 10.Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K. Cervical pedicle screw insertion: assessment of safety and accuracy with computer-assisted image guidance. J Spinal Disord. 2000;13:218–224. doi: 10.1097/00002517-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine. 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 12.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine. 2007;32:E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 13.Kotani Y, Abumi K, Ito M, Minami A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg. 2003;99:257–263. doi: 10.3171/spi.2003.99.3.0257. [DOI] [PubMed] [Google Scholar]
- 14.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kuroki H, Rengachary SS, Goel VK, Holekamp SA, Pitkanen V, Ebraheim NA. Biomechanical comparison of two stabilization techniques of the atlantoaxial joints: transarticular screw fixation versus screw and rod fixation. Neurosurgery. 2005;56:151–159. doi: 10.1227/01.NEU.0000144838.01478.35. [DOI] [PubMed] [Google Scholar]
- 16.Leonard JR, Wright NM. Pediatric atlantoaxial fixation with bilateral, crossing C-2 translaminar screws. Technical note. J Neurosurg. 2006;104:59–63. doi: 10.3171/ped.2006.104.1.59. [DOI] [PubMed] [Google Scholar]
- 17.Magerl F, Seemann P. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine I. New York: Springer; 1986. pp. 322–327. [Google Scholar]
- 18.MCDonnell D, Harrison SJ. Posterior atlantoaxial fusion: Indications and techniques. In: Hitchon PW, Traynelis VC, Rengachary SS, editors. Techniques in spinal fusion and stabilization. New York: Thieme; 1995. pp. 92–106. [Google Scholar]
- 19.Melcher RP, Puttlitz CM, Kleinstueck FS, Lotz JC, Harms J, Bradford DS. Biomechanical testing of posterior atlantoaxial fixation techniques. Spine. 2002;27:2435–2440. doi: 10.1097/00007632-200211150-00004. [DOI] [PubMed] [Google Scholar]
- 20.Naderi S, Crawford NR, Song GS, Sonntag VK, Dickman CA. Biomechanical comparison of C1–C2 posterior fixations, cable, graft, and screw combinations. Spine. 1998;23:1946–1955. doi: 10.1097/00007632-199809150-00005. [DOI] [PubMed] [Google Scholar]
- 21.Oda I, Abumi K, Sell LC, Haggerty CJ, Cunningham BW, McAfee PC. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine. 1999;24:2377–2382. doi: 10.1097/00007632-199911150-00015. [DOI] [PubMed] [Google Scholar]
- 22.Resnick DK, Benzel EC. C1–C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery. 2002;50:426–428. doi: 10.1097/00006123-200202000-00039. [DOI] [PubMed] [Google Scholar]
- 23.Richter M, Amiot LP, Neller S, Kluger P, Puhl W. Computer-assisted surgery in posterior instrumentation of the cervical spine: an in vitro feasibility study. Eur Spine J. 2000;9(Suppl 1):S65–S70. doi: 10.1007/PL00010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richter M, Cakir B, Schmidt R. Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine (Phila Pa 1976) 2005;30:2280–2287. doi: 10.1097/01.brs.0000182275.31425.cd. [DOI] [PubMed] [Google Scholar]
- 25.Stokes JK, Villavicencio AT, Liu PC, Bray RS, Johnson JP. Posterior atlantoaxial stabilization: new alternative to C1–C2 transarticular screws. Neurosurg Focus. 2002;12:E6. doi: 10.3171/foc.2002.12.1.7. [DOI] [PubMed] [Google Scholar]
- 26.Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw–rod system. Eur Spine J. 2007;16:479–484. doi: 10.1007/s00586-006-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004;17:158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Wright NM. Translaminar rigid screw fixation of the axis. Technical note. J Neurosurg Spine. 2005;3:409–414. doi: 10.3171/spi.2005.3.5.0409. [DOI] [PubMed] [Google Scholar]