Abstract
The surgical management of cervical spondylodiscitis consists of the resection of the affected disc, the decompression of the cervical spinal cord, followed by the stabilization using an autologous bone graft or a titanium implant combined with a ventral plate fixation. Until now, there were no studies about the practicability and putative safety of PEEK cages in cervical spine infection. Now, we present the history of five patients suffering from neurological deficits and septicemia caused by mono- or bisegmental pyogenic cervical discitis and intraspinal abscess without severe bone destruction. Patients were treated surgically by discectomy, decompression, and ventral spondylodesis. The disc was replaced by a PEEK cage without additional fixation. Progressive bony fusion and complete regression of the inflammatory changes was demonstrated 7–8 months later by a computer assisted tomography and contrast enhanced magnetic resonance imaging, respectively. The vertebral alignment changed minimally; the cages developed only a slight average subsidence. The clinical symptoms improved in all patients significantly. Neck pain or instability was never observed. Nevertheless, prospective investigations of a larger patient series are mandatory. We suppose that the use of PEEK cages represents a potential and safe alternative in the treatment of cervical spondylodiscitis in selected patients.
Keywords: Cervical spondylodiscitis, Targeted antibiotic therapy, Sepsis, PEEK cage, Stabilization, Decompression
Introduction
Cervical spondylodiscitis and cervical epidural abscesses still are a challenge in spine surgery. Possible severely septic and neurological complications make it a life-threatening disease in which urgent treatment is mandatory [1–3]. The surgical management consists of operative debridement of the affected disc, decompression of the spinal cord and ventral stabilization followed by a targeted long-term antibiotic therapy. Autologous bone grafting combined with ventral instrumentation is considered the “gold standard”. Alternatively, intervertebral titanium implants were a possible option during the last decade [4]. However, the use of polyaryl-ether-ether-ketone (PEEK) cages that are very popular in degenerative spine surgery has not yet been investigated in infections. They are still “forbidden” in the treatment of pyogenic cervical discitis.
Biocompatibility studies have demonstrated that the PEEK polymer is non-toxic (ISO 10993-5), and chemical analysis (ISO 10993-18) showed that there is no evidence of any harmful ingredients that could be released in a life-time exposure in mammals. Experimental implantation into rabbits for 1 year according to ISO 10993-6 did not reveal any harmful changes within the surrounding tissue. Virtually no response or even mild fibrosis, like a small fibrous capsule was observed in the animal models. Necrosis, muscle degeneration, or any other significant changes were not observed after sterilization with gamma radiation at more than 73 kGy, following stream sterilization at 121°C (0249°F) and subsequent implantation into the animal model [5].
Here, we present a patient series with cervical spondylodiscitis exclusively treated surgically by the use of PEEK cage insertion and we discuss the results against the background of the recent literature.
Patients and methods
This is a retrospective study of five patients (male:female = 4:1) with an acute mono- (n = 3) or bisegmental (n = 2) pyogenic infection of the cervical spine with the level C5/6 being the most affected one (four of five cases) (Table 1). In one of these patients, the discitis occurred after previous bisegmental fusion. This was performed because of a degenerative spinal stenosis 2 weeks before. The other four patients suffered from a chronic oral (n = 2) or cutaneous infection (n = 2), respectively. All patients suffered from a longterm diabetes mellitus (Tables 1, 2). Our patients’ mean age was 62.4 years. On admission, all patients presented severe neurological deficits (Table 1). The time window from the first manifestation of symptoms to admission in the hospital ranged from 1 to 3 days. C-reactive protein (CRP) was elevated in all cases ranging from 117.1 to 157.0 mg/dl (Table 2). All patients presented with an increased body temperature and an increased leukocyte count as well as an elevated erythrocyte sedimentation rate (ESR) (Table 2).
Table 1.
The survey of five patients with cervical spondylodiscitis shows their main clinical features
| Patient no. | Gender | Age | Comorbidity | Affected levels | Mode of infection | Symptoms on admission | Postoperative symptoms |
|---|---|---|---|---|---|---|---|
| 1 | Female | 68 | Diabetes mellitus | C4/5 and C5/6 | Primary | 1 fever | 1 no fever |
| Mamma carcinoma | 2 neck pain | 2 no neck pain | |||||
| Oral infection | 3 paresis of the right arm | 3 regredient arm paresis | |||||
| 2 | Male | 57 | Diabetes mellitus | C5/6 | Primary | 1 fever | 1 no fever |
| Superficial would infection | 2 neck pain | 2 no neck pain | |||||
| 3 monoparesis of the left arm | 3 bilateral biceps paresis | ||||||
| 3 | Male | 68 | Diabetes mellitus | C3/4 | Primary | 1 fever | 1 no fever |
| Superficial wound infection | 2 neck pain | 2 no neck pain | |||||
| 3 tetraparesis | 3 bilateral deltoideus and biceps paresis | ||||||
| 4 | Male | 56 | Diabetes mellitus | C5/6 & C6/7 | Secondary | 1 neck pain | 1 no fever |
| 2 paresis of the right arm | 2 no neck pain | ||||||
| 3 paresis of the right arm | |||||||
| 5 | Male | 63 | Diabetes mellitus | C5/6 | Primary | 1 fever | 1 no fever |
| 2 neck pain | 2 no neck pain | ||||||
| 2 monoparesis of the left arm | 3 regredient arm paresis |
Table 2.
This survey of the same five patients shows their paraclinical and laboratory data
| Patient no. | Blood glucose on admission (ref. 3.3–5.6 mmol/l) (mmol/l) | Body temperature on admission (ref. aprox. 36.5°C/97.7°F) | Leukocytes on admission (ref. 4.4–11.3 Gpt/l) (Gpt/l) | ESR on admission (ref. 7–12 mm/1st h; <18 mm/2nd h) | CRP on admission (ref. <2 mg/l) (mg/l) | Causing agent | Longterm antibiotic therapy |
|---|---|---|---|---|---|---|---|
| 1 | 7.3 | 39.5°C/103.1°F | 12.2 | 73/105 | 157 | Staphylococcus aureus | Rifampicin 600 mg 1–0–0 |
| Clindamycin 600 mg 1–1–1 | |||||||
| 2 | 15.4 | 38.9°C/102.0°F | 20.8 | 91/96 | 148.8 | Staphylococcus aureus | Clindamycin 600 mg 1–1–1 |
| Metronidazole 400 mg 1–1–1 | |||||||
| 3 | 10.5 | 39.8°C/103.6°F | 18.4 | 69/98 | 117.1 | Staphylococcus aureus | Rifampicin 600 mg 1–0–0 |
| Clindamycin 600 mg 1–1–1 | |||||||
| 4 | 19.5 | 39.9°C/103.8°F | 13.9 | 79/88 | 134.5 | Staphylococcus epidermidis | Rifampicin 600 mg 1–0–0 |
| Clindamycin 600 mg 1–1–1 | |||||||
| 5 | 17.8 | 39.3°C/102.7°F | 11.8 | 86/98 | 152.6 | Staphylococcus aureus | Rifampicin 600 mg 1–0–0 |
| Clindamycin 600 mg 1–1–1 |
The references of the lab values are given in brackets in the headline
The diagnosis was established after cervical magnetic resonance imaging (MRI) with intravenous administration of gadolinium diethylen-triamin-penta acetic acid (gadolinium-DTPA). A putative destruction of the adjacent bony vertebral end plates was excluded by a computer-assisted tomography (CT) examination.
As there were severe and rapidly progressive neurological deficits, the surgical treatment was performed under emergency conditions on the admission day in all five cases. In each operation, we used the typical anterior approach after Cloward [6]. After removal of the disc and debridement of the adjacent bony end plates under mild distraction, the posterior longitudinal ligament was removed and intraspinal pus irrigated using a saline solution via a small Nélaton catheter of 8 Charrière. When there was no liquid pus detectable any more, a PEEK cage (Shell©-Cage/Advanced Medical Technologies AG, Nonnweiler, Germany) was inserted. This was performed, when preoperative imaging with intact bony endplates was confirmed during the surgical procedure.
Because of firm osseous conditions, we did not need to apply an additional ventral plate fixation. The operation was followed by a targeted antibiotic therapy over a minimal period of 12 weeks starting with the intravenous administration of using a threefold combination of antibiotics (gentamycin, vancomycin, and metronidazole). This was immediately adapted according to the specific resistogram after 48 h. After a period of 3 weeks with intravenous antibiotic administration, antibiotics were given orally for the rest of time (Table 2). Patient no. 1 received her antibiotics for full 20 weeks because of her severe infection with septicemia (Table 2). All patients were fully mobilized and a semirigid cervical collar was prescribed for 4 weeks.
A first contrast enhanced MRI and a native CT examination was scheduled during the hospital stay between days 7 and 12 after the operation. The subsequent follow-up examinations were performed between around week 8 (6–10) and around month 6 (29–33 weeks), respectively. Lab controls including the CRP, the ESR, and the white blood cell count were performed. Sinking of the cage and possible kyphotic angulation that was measured by the Cobbs angle, were defined on the last sagittally reconstructed CT scan of the cervical spine. Fusion was assumed when an osseous continuity between the adjacent vertebral bodies was verifiable according to our standard criteria in the surgery of degenerative cervical spine disease.
Results
There were no peri- or postoperative complications. Isolation of the triggering germ from the specimen obtained during the operation revealed staphylococcus species as the causative agent in all patients (Table 2). After a clinical follow-up of 15 months, the neurological deficits improved in all of the five patients (Table 1). Neck pain and signs of instability were not observed during the last follow-up in all patients (Table 1).
At the last radiological follow-up between 29 and 33 weeks after surgery, a bony fusion was achieved in all five patients with a complete regression of the inflammatory changes on MRI (Figs. 1, 2, 3).
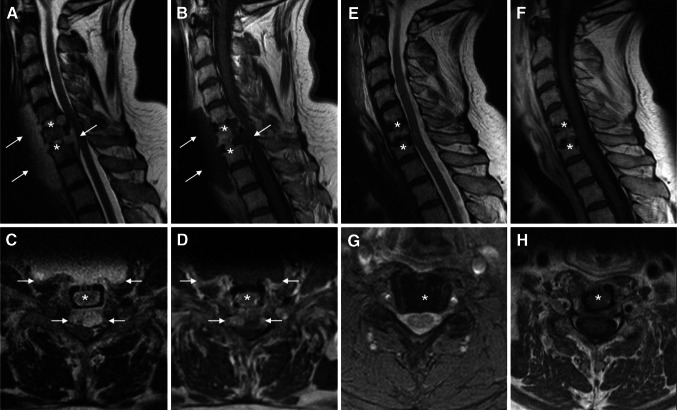
Fig. 1.
Time course of diagnostic imaging during cervical spondylodiscitis with an epidural component (a–d), after surgical decompression and ventral spondylodesis and subsequent targeted antibiotic therapy (e–h). a–d MRI in sagittal (a) and transversal (c) T2 sequence illustrates the mass effect of the acute spondylodiscitis with prevertebral and epidural abscess formation. Gadolinium enhanced T1 sequences in sagittal (b) and transversal (d) orientation demonstrate the contrasted rim and the hypointense, fluid center of the abscesses. The arrows label the margins of the prevertebral and epidural abscesses. The stars mark the former intervertebral disc spaces before cage interposition. e–h The postoperative MRI after 7 months clearly shows the totally decompressed spinal conditions. The sagittal (e) and transversal (g) T2 weighted images make the perimedullary rim of cerebrospinal fluid visible. The sagittal (f) and transversal (h) T1 weighted images after intravenous administration of gadolinium-DTPA illustrate the decreased inflammatory situation without any enhancement of gadolinium. The stars mark the levels of the intervertebral discs. The images belong to patient no. 4 from the Tables 1 and 2
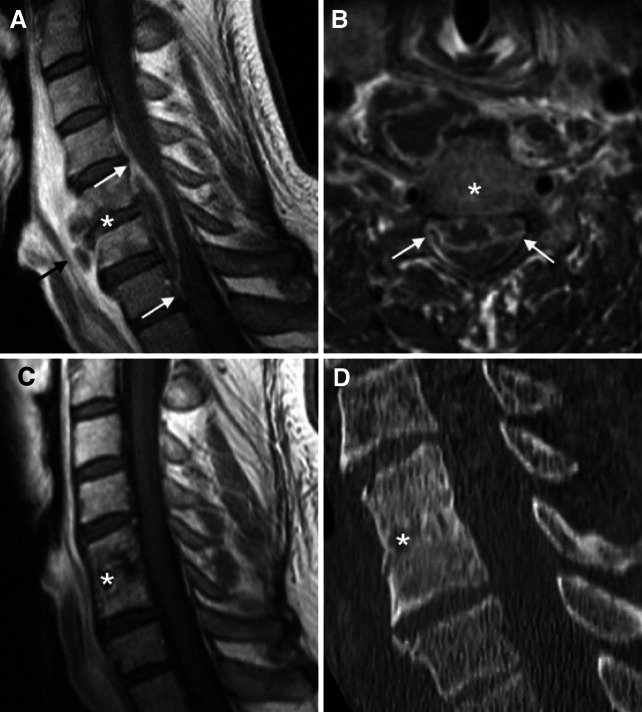
Fig. 2.
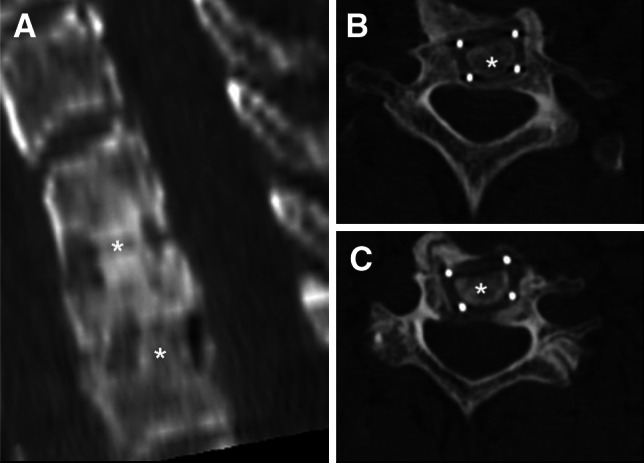
Postoperative CT and MRI imaging after 7 months of the same patient as in Fig. 1. a, b The transversal CT images and their sagittal reconstruction illustrate the total bony fusion between the involved cervical levels. The stars mark the involved levels C5–C7. The patient did not demonstrate any signs of neck pain, micro- or macroinstability. The patient did not demonstrate any signs of neck pain, micro- or macroinstability. The images belong to patient no. 4 from the Tables 1 and 2. Artifacts from metal markers within PEEK cages might be misdiagnosed as lucencies
Fig. 3.
Preoperative imaging of a cervical spondylodiscitis with prevertebral und epidural abscesses, after surgical decompression and 9-months CT-control after monosegmental PEEK-cage spondylodesis. a, b Sagittal and axial gadolinium-enhanced T1-MRI imaging illustrates the spondylodiscitis mainly in segment C5/6 (star) with prevertebral (black arrow) and epidural abscesses (white arrows). c Gadolinium-enhanced T1-MRI imaging after 6 months demonstrates a completely decompressed spinal canal without any sign of a local infection. d Sagital CT images demonstrate the complete bony fusion of the involved level C5/6 1 year after monosegmental PEEK-cage spondylodesis. The stars mark the involved level C5/6. Again, there were no signs of neck pain, micro- or macroinstability in this patient
Concerning the alignment of the vertebral spine, there was one moderate new kyphotic angulation in a patient who had undergone bisegmental fusion measuring 2.7 degrees. In the other four patients, there was a loss of lordosis of 0.6, 0.2, 3.1, and 0.7 degrees. A slight cage subsidence occurred in each of the seven operated segments (Table 1).
Discussion
Nowadays, the surgical management of cervical discitis is based on two general principles. On one side, there has to be sufficient debridement of the infected spinal area with decompression of the neural structures. On the other side, a stable bony fusion of the affected segments is mandatory.
Up to now, an iliac bone graft combined with a ventral plate fixation has been proposed to be the treatment of first choice. Generally, accepted advantages are the stable osseous fusion achieved by an autologous bone graft. The use of exogenous materials inside the infected area is avoided with this technique, but complications from the donor site with disabling persistent pain or even pelvic fracture occur in up to 39% [7]. These complications comprise ongoing problems, even today. During the last years, there has been a new development with some studies showing good results after the use of intervertebral titanium implants combined with ventral or dorsoventral instrumentation [4, 8, 9]. Despite the insertion of exogenous material into the infected area, the fusion rates after titanium device implantation compared to bone grafting were similar.
For uncertain reasons, polyaryl-ether-ether-ketone cages that are widely used in the surgery of the degenerative cervical spine, are still supposed to be unsuitable in pyogenic cervical infections, even though some in vitro and in vivo studies could demonstrate the biocompatibility and the inertness of this material [5, 10]. The first, only recently published clinical study has shown encouraging results concerning the use of a bone graft versus cage implants in patients suffering from lumbar discitis [11]. This study demonstrated the safety and usefulness of the method.
Here, we present five cases of acute pyogenic cervical discitis treated with discectomy, decompression, and ventral spondylosis by PEEK cage insertion and we show bony fusion in subsequent CT scans. Bony fusion occurs 8 months after the surgical intervention with a complete regression of the inflammatory changes on MRI and normalization of the inflammatory lab signs. Against the background of different definitions and study designs, the time window for the cervical fusion as well as the data concerning cage subsidence seems comparable with the data of patients with titanium implants for degenerative disc disease [12–14]. In our patients, there was no relevant destruction of the adjacent vertebral bodies and end plates so that we did not insert an additional internal fixation system. A semirigid cervical collar was sufficient for over a period of 4 weeks. Secondary risks, like screw displacement or material fatigue are avoided by this surgical approach.
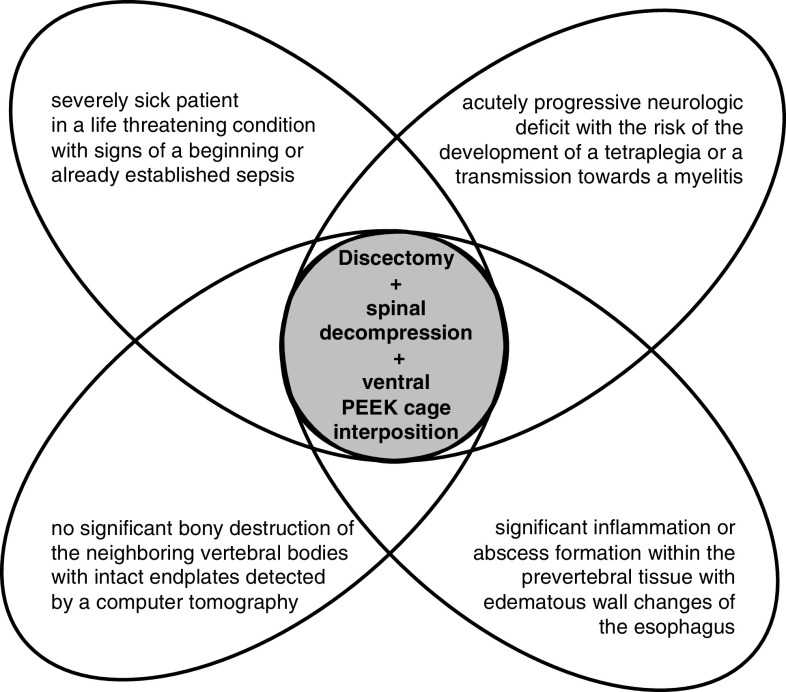
In cases without distinct osseous destruction, PEEK cages seem to be a potential true alternative compared with the standard methods (Fig. 4). The surgical procedure is less complex and saves time, especially when the approach is complicated by inflammatory changes of the surrounding tissue and when the patient suffers from a critically septic condition.
Fig. 4.
Prerequisites for the preoperative evaluation of a ventral spondylodesis by a PEEK cage implantation in cervical spondylodiscitis. Patients who fulfill all criteria listed could be evaluated for insertion of a PEEK cage after microsurgical discectomy and spinal decompression, when their bony endplates of involved vertebrae are intact. Whenever one of the criteria is not given, the standard procedures with a ventral fixation system should be used
Taken together, we suppose the performance of a ventral discectomy, cervical cord decompression, and the simple insertion of a PEEK cage, when the general condition is complicated by a septic situation, e.g., with high fever and disturbances of the systemic circulation, accompanied by a life threatening situation with acutely progressive neurologic deficits caused by a cervical spondylodiscitis with an intraspinal component and when the bony end plate structures are completely intact (Fig. 4).
We think that further prospectively performed clinical and experimental studies are mandatory in order to evaluate the possible use of PEEK cages in the treatment of cervical spondylodiscitis. Our results present this procedure as a noteworthy and potentially new method.
Acknowledgments
This work was supported by the Trust of Neurosurgical Research of the German Society of Neurosurgery to Jan Walter, Susanne A. Kuhn, and Rupert Reichart (2005, 2007, 2008).
Footnotes
J. Walter and S. A. Kuhn contributed equally to this work.
Contributor Information
Susanne Antje Kuhn, Email: Susanne.Kuhn@med.uni-jena.de.
Christian Ewald, Phone: +49-3641-9323001, FAX: +49-3641-9323002, Email: Drewald@hotmail.com.
References
- 1.Heyde CE, Boehm H, El Saghir H, Tschöke SK, Kayser R. Surgical treatment of spondylodiscitis in the cervical spine: a minimum 2-year follow-up. Eur Spine J. 2006;15(9):1380–1387. doi: 10.1007/s00586-006-0191-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P, Kannerup AS, Niedermann B. Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop. 2008;79(5):650–659. doi: 10.1080/17453670810016678. [DOI] [PubMed] [Google Scholar]
- 3.Frangen TM, Kälicke T, Gottwald M, Andereya S, Andress HJ, Russe OJ, Müller EJ, Muhr G, Schinkel C. Surgical management of spondylodiscitis. An analysis of 78 cases. Unfallchirurg. 2006;109(9):743–753. doi: 10.1007/s00113-006-1084-7. [DOI] [PubMed] [Google Scholar]
- 4.Korovessis P, Petsinis G, Koureas G, Iliopoulos P, Zacharatos S. Anterior surgery with insertion of titanium mesh cage and posterior instrumented fusion performed sequentially on the same day under one anesthesia for septic spondylitis of thoracolumbar spine: is the use of titanium mesh cages safe? Spine. 2006;31(9):1014–1019. doi: 10.1097/01.brs.0000215049.08622.9d. [DOI] [PubMed] [Google Scholar]
- 5.Green S, Schlegel J (2001) Polymers for the medical industry. In: Conference Proceedings, Paper 2
- 6.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6):602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 7.Sasso RC, LeHuec JC, Shaffrey C, Spine Interbody Research Group Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech. 2005;18(Suppl):S77–S81. doi: 10.1097/01.bsd.0000112045.36255.83. [DOI] [PubMed] [Google Scholar]
- 8.Kuklo TR, Potter BK, Bell RS, Moquin RR, Rosner MK. Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech. 2006;19(5):376–382. doi: 10.1097/01.bsd.0000203945.03922.f6. [DOI] [PubMed] [Google Scholar]
- 9.Korovessis P, Repantis T, Iliopoulos P, Hadjipavlou A. Beneficial influence of titanium mesh cage on infection healing and spinal reconstruction in hematogenous septic spondylitis: a retrospective analysis of surgical outcome of twenty-five consecutive cases and review of literature. Spine. 2008;33(21):E759–E767. doi: 10.1097/BRS.0b013e318187875e. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28(32):4845–4869. doi: 10.1016/j.biomaterials.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pee YH, Park JD, Choi YG, Lee SH. Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine. 2008;8(5):405–412. doi: 10.3171/SPI/2008/8/5/405. [DOI] [PubMed] [Google Scholar]
- 12.Chen Y, Chen D, Guo Y, Wang X, Lu X, He Z, Yuan W. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech. 2008;21(7):489–492. doi: 10.1097/BSD.0b013e318158de22. [DOI] [PubMed] [Google Scholar]
- 13.Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, Chiou TL, Chang YL, Su CF, Lin SZ, Chen SY. Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci. 2008;15(11):1240–1245. doi: 10.1016/j.jocn.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Hauerberg J, Kosteljanetz M, Bøge-Rasmussen T, Dons K, Gideon P, Springborg JB, Wagner A. Anterior cervical discectomy with or without fusion with ray titanium cage: a prospective randomized clinical study. Spine. 2008;33(5):458–464. doi: 10.1097/BRS.0b013e3181657dac. [DOI] [PubMed] [Google Scholar]