Abstract
The relationship of Modic change to pain and inflammation remains to be unclear. Recently, some authors have reported that Modic type 1 signals are closely related to infection. However, if the patients do not have severe back pain, fever, or an abnormal blood profile, it is difficult to distinguish between common Modic change and infection. The purpose of this study was to examine the prevalence of pyogenic spondylitis in patients who showed Modic type 1 change without other signs of infection. Seventy-one patients with Modic type 1 change were evaluated (average age 55, 32 males and 39 females). X-ray and magnetic resonance imaging (MRI) were performed to investigate low-back pain and leg pain. Body temperature was measured and blood analysis (including white blood cell count and level of C-reactive protein) was conducted for all patents. All 71 patients with Modic type 1 change, but without other signs of infection were followed for 2 years. Low-back pain, X-ray, and blood analyses were performed every 3 months; and MRI was performed every year. Severe low-back pain or abnormal signs developed in four patients during the follow-up. Pyogenic spondylitis was diagnosed in three patients by symptoms, blood results, and imaging, and confirmed by biopsy. Two of the three patients were diabetic. A total of 4.2% of patients with Modic type 1 change, but without other signs of infection were diagnosed as having pyogenic spondylitis during the 2-year follow-up, therefore, it is important to consider this before treating Modic type 1 change.
Keywords: Modic, Infection, Pyogenic, Spondylitis
Introduction
Abnormalities of the vertebral endplate have been described by Modic et al. [8, 9]. We previously conducted magnetic resonance imaging (MRI) studies of patients with endplate and vertebral bone marrow changes associated with degenerative lumbar disc disease [14]. Abnormalities associated with decreased signal intensity on T1-weighted spin-echo images (Modic type 1) correlated with segmental hypermobility and low-back pain [14]. We have also reported that Modic type 1 changes in discogenic pain patients are related to inflammation and axonal growth in the abnormal bone marrow induced by cytokines, such as tumour necrosis factor-α (TNF) [10].
Spinal infection may manifest as Modic type 1 signal on MRI. It is difficult to distinguish between common Modic change and infection by low-virulent bacteria [2]. We have retrospectively reviewed the records of 111 patients who had pyogenic vertebral osteomyelitis [6]. Infection found in 41 patients (37%) was caused by microorganisms, such as Staphylococcus epidermidis, Propionibacterium acnes, and diphtheroid species, which are usually considered to be of low virulence [5]. Surprisingly, it has been reported that in nuclear tissue removed under sterile conditions during surgery for lumbar herniated discs, 53% of patients were found to be infected with low-virulent anaerobic organisms [12]. Recently, some authors have reported that Modic type 1 signals are closely related to infection by microorganisms. However, if the patients do not have severe back pain, fever, or an abnormal blood profile, it is difficult to distinguish between common Modic change and infection.
Therefore, the purpose of the current study was to examine the frequency of pyogenic spondylitis in patients who showed Modic type 1 change without other signs of infection during a 2-year follow-up.
Materials and methods
The protocol for human procedures used in this study was approved by our institution’s ethics committee. Our study involved 512 patients (250 males and 262 females) with an average age of 55.7 ± 8 years (mean ± SEM, range 18–82 years).
Patients
Inclusion criteria
Low-back pain or leg pain (radicular pain), continuing for at least 2 weeks, was found in 512 patients. Patients who had previously undergone spinal surgery were excluded. We also excluded spinal tumour, apparent infection, and trauma.
Patients underwent X-ray examination and MRI. They were diagnosed with normal findings, disc degeneration, disc herniation, and spinal stenosis. In 512 patients, endplate and bone marrow abnormalities were examined from the L2/3 to L5/S1 level.
Endplate and bone marrow abnormalities were subclassified into those with Modic type 1 signals (n = 73, low intensity on T1-weighted spin-echo images and high-intensity T2-weighted spin-echo images), those with Modic type 2 signals without type 1 change signals (n = 87, high intensity on both T1- and T2-weighted spin-echo images), those with Modic type 3 signals without type 1 change signals (n = 36, low intensity on both T1- and T2-weighted spin-echo images), and those with Modic type 0 (n = 390, normal intensity on both T1- and T2-weighted spin-echo images). Some patients show some type of Modic change at several levels. If a patient has at least one level Modic type 1 change, we defined the patient as being Modic type 1.
In the patients showing Modic type 1 signals, body temperature was measured and blood analysis [including white blood cell count (WBC) and level of C-reactive protein (CRP)] was performed in all patients. Two patients with fever (>37°C) and abnormal blood test results were excluded (WBC >8,500 cells/mm3 or CRP >0.3 mg/dl). Therefore, 71 patients with Modic type 1 change without other signs of infection were followed up for 2 years. Evaluation of low-back pain, blood analysis (including WBC count and CRP level), and X-ray examination were performed every 3 months. MRI was performed every year. All patients had low back pain were treated with oral of nonsteroidal anti-inflammatory drugs (NSAIDs). All patients were not treated with antibiotics.
Evaluation
The change in disc height and endplate abnormality on X-ray imaging, bone marrow abnormality on MRI, blood examination, and symptoms were evaluated to determine whether infection was present or not from start-up to final follow-up. Evaluation was blinded and performed by three observers. If at least two of the observers were in agreement, evaluation of infection was conducted. Finally, if the patient was strongly suspected to have infection, the final diagnosis was confirmed by biopsy, 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) [13], Tc-bone scan, or open biopsy during lumbar surgery.
Results
No severe low back pain or leg pain developed in 55 patients during the 2-year follow-up. Moderate low back pain or leg pain developed in 11 patients; however, this could be decreased using NSAIDs. Severe low back pain or leg pain developed in five patients during the 2-year follow-up; the symptoms were not decreased by using NSAIDs.
Abnormal blood data were shown in 15 patients (WBC >8,500 cells/mm3 or CRP >0.3 mg/dl); however, this abnormality was transient in 12 patients. Abnormal blood data were persistent in three patients. Six patients showed endplate bone marrow abnormalities on X-ray imaging during the 2-year follow-up. Four patients showed endplate bone marrow abnormalities on final MRI during the 2-year follow-up.
Finally, pyogenic spondylitis was strongly suspected from symptoms, blood results, X-ray imaging, and MRI in four patients during this period. Pyogenic spondylitis was strongly suspected in two patients at final follow-up (2 years), in one patient at (18 months), and in one patient (20 months). Two of the four patients were diabetic. The diagnosis was confirmed by biopsy, FDG–PET, or open surgery biopsy in all four patients. One patient was negative; the other three patients were ultimately diagnosed with infection. The patients finally diagnosed as having pyogenic spondylitis did not have any illnesses that could be related to subsequent pyogenic spondylitis.
The frequency of pyogenic spondylitis in patients who showed Modic type 1 change without other signs of infection during the 2-year follow-up was calculated. We found that 4.2% (3/71 patients) were ultimately diagnosed with infection.
Case 1: finally diagnosed with infection
A 72-year-old diabetic woman presented with low back pain and bilateral-leg pain. MRI indicated Modic type 1 change. X-ray imaging did not show endplate abnormality and blood examination was normal. Her symptoms and regular X-ray and blood examinations were normal; however, at final follow-up (2 years), low back pain increased, and abnormal blood data (CRP 4.50 mg/dl) and signs of infection on MRI were observed. A biopsy was conducted and infection by Staphylococcus epidermidis was diagnosed (Figs. 1, 2).
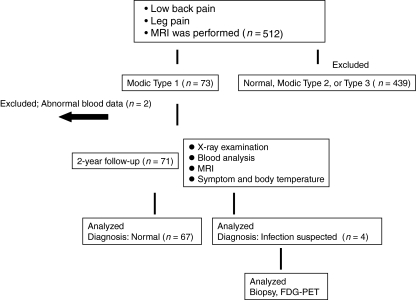
Fig. 1.
Consort diagram of the current study
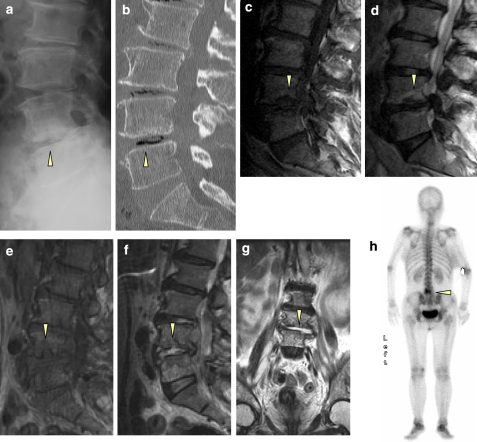
Fig. 2.
Case 1: finally diagnosed with infection. A 72-year-old diabetic woman presenting with low back pain and bilateral-leg pain. X-ray imaging and CT did not show endplate abnormality at the L4/5 level (a, b), and blood examination was normal. MRI indicated Modic type 1 change at the L4/5 level (c T1 weighted, d T2 weighted). During the 2-year follow-up, her symptoms and regular X-ray and blood examination results were normal; however, at final follow-up (2 years), low back pain increased, abnormal blood data (WBC 12,000 cells/mm3 and CRP 4.50 mg/dl) and signs of infection on MRI were observed at the L4/5 level (e T1 weighted, f T2 weighted, g T2-weighted coronal section). A Tc-bone scan also showed abnormal accumulation (h). A biopsy was performed and infection by Staphylococcus epidermidis was diagnosed
Case 2: finally diagnosed with non-infection
A 62-year-old woman presented with low back pain and bilateral-leg pain. MRI indicated Modic type 1 change. X-ray imaging showed endplate and bone marrow abnormality; however, blood examination was normal. We conducted FDG-PET and no abnormal findings were disclosed. We performed a posterior lumbar interbody fusion with a pedicle screw for her severe low back pain. The endplate and vertebral body were harvested during surgery, and were subsequently cultured; however, no infection was found (Fig. 3).
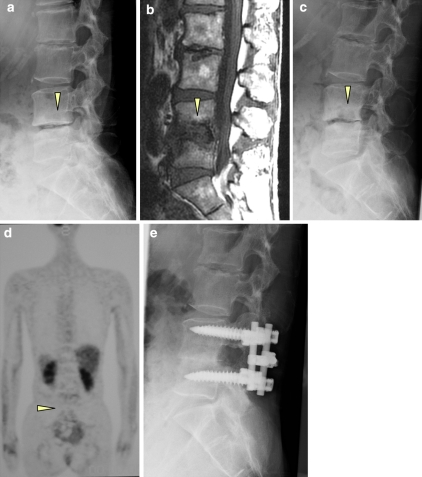
Fig. 3.
Case 2: finally diagnosed with non-infection. A 62-year-old woman presenting with low back pain and bilateral-leg pain. X-ray imaging shows slight endplate and bone marrow abnormality (a); however, blood examination was normal. MRI indicated Modic type 1 change (b). Follow-up X-ray imaging at 2 years shows an increase of the endplate and bone marrow abnormality (c); however, blood examination was also normal. We conducted FDG-PET and no abnormal findings were revealed (d). The result of a biopsy was also negative. We performed a posterior lumbar interbody fusion with a pedicle screw for her severe low back pain (e). The endplate and vertebral body were harvested during surgery, and were subsequently cultured; however, no infection was found
Discussion
A total of 4% of patients with Modic type 1 change without other signs of infection were diagnosed as having pyogenic spondylitis during the 2-year follow-up period, and it is important to consider this before treating Modic type 1 change.
It has been reported that Modic type 1 change shows disruption and fissuring of the endplate with regions of degeneration, regeneration, and vascular granulation of tissue [9, 14]. Increased amounts of reactive woven bone, prominent osteoclasts, and osteoblasts have been found, thus Modic type 1 change is considered to be an inflammatory condition [9].
Some authors have reported a relationship between low back pain and inflammation in intervertebral discs and vertebral endplates. The association between Modic changes on MRI and discogenic back pain on lumbar discography has been examined and the investigators concluded that Modic changes appear to be a relatively specific, but insensitive sign of a painful lumbar disc in patients with discogenic low back pain [3]. The levels of interleukin (IL)-6 and 8 production in disc tissue from patients undergoing discectomy for sciatica were compared with those from patients undergoing fusion for discogenic low back pain. IL-6 and 8 productions in the low back pain group was significantly higher when compared with that in the sciatica group [4]. The number of TNF-immunoreactive cells in endplates exhibiting Modic type 1 changes was significantly higher than in endplates exhibiting normal and Modic type 2 changes. These findings suggest that endplate abnormalities (Modic type 1 change) are related to inflammation induced by TNF and may be a cause of low back pain [10].
Therapeutic targets for low back pain and inflammation in endplates have been proposed. Low-grade inflammation indicated by high-serum CRP levels in patients with chronic low back pain could indicate Modic type 1 signal changes and thus antiinflammatory treatment was recommended in such patients [11]. Furthermore, intradiscal chymopapain injection resulted in Modic type 1 change in vertebral body endplates adjacent to the level of injection, and the investigators concluded that this change was due to inflammation [7]. Intradiscal injection of corticosteroids can be an efficient short-term treatment for patients with chronic low back pain and predominantly inflammatory endplate signs, such as Modic type 1 change [6].
On the other hand, it is difficult to distinguish between normal inflammatory change and infection. Albert et al. proposed a bacterial cause of common Modic type 1 change following tears in the outer fibres of the annulus, e.g., in disc herniation, where new capillarisation and inflammation developed around the extruded nuclear material. It is possible for anaerobic bacteria to enter the anaerobic disc interior through this tissue and in this environment to cause a slowly developing low-virulent infection. They proposed that common Modic type 1 change could be the visible sign of the inflammation and oedema surrounding this infection [2]. Following this hypothesis, they assessed the clinical effect of antibiotic treatment in a cohort of patients with low back pain and common Modic type 1 changes. After treatment with amoxicillin–clavulanate, there was both clinically important and statistically significant improvement in all outcome measures [1]. These findings supported the hypothesis that the common Modic type 1 change originated from the infection in these patients.
In the current study, we diagnosed that about 4% of patients with Modic type 1 change, but without other signs of infection had pyogenic spondylitis during the 2-year follow-up period. However, some limitations of the current study exist. First, we did not perform a biopsy in all patients. However, Wedderkopp et al. [15] have reported that 24 consecutive patients with Modic type I changes in lumbar vertebrae had a biopsy taken from the affected vertebra. None of the biopsies yielded growth of anaerobic bacteria. They concluded that no evidence of bacteria in vertebrae with Modic type I changes. We thought that biopsy is not necessary to distinguish between common Modic change and infection. Second, the number of patients was statistically small. Third, we ultimately used FDG-PET as a method to distinguish between infection and Modic type 1 change. FDG-PET may prove useful in differentiation of degenerative and infectious endplate abnormalities detected on MRI [13]. However, the reliability of FDG-PET needs further investigation. Fourth, there was a possibility that infection accidentally occurred at inflammatory Modic change.
In conclusion, 4.2% of patients with Modic type 1 change, but without other signs of infection were diagnosed as having pyogenic spondylitis during the 2-year follow-up period of this study, and it would appear important to consider this before treating patients with Modic type 1 changes.
References
- 1.Albert HB, Manniche C, Sorensen JS, Deleuran BW. Antibiotic treatment in patients with low-back pain associated with Modic changes Type 1 (bone oedema): a pilot study. Br J Sports Med. 2008;42:969–973. doi: 10.1136/bjsm.2008.050369. [DOI] [PubMed] [Google Scholar]
- 2.Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C. Modic changes: possible causes and relation to low back pain. Med Hypotheses. 2008;70:361–368. doi: 10.1016/j.mehy.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 3.Braithwaite I, White J, Saifuddin A, Renton P, Taylor BA. Vertebral end-plate (Modic) changes on lumbar spine MRI: correlation with pain reproduction at lumbar discography. Eur Spine J. 1998;7:363–368. doi: 10.1007/s005860050091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burke JG, Watson RW, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg Br. 2002;84:196–201. doi: 10.1302/0301-620X.84B2.12511. [DOI] [PubMed] [Google Scholar]
- 5.Carragee EJ. Pyogenic vertebral osteomyelitis. J Bone Joint Surg Am. 1997;79:874–880. doi: 10.1302/0301-620X.79B5.8078. [DOI] [PubMed] [Google Scholar]
- 6.Fayad F, Lefevre-Colau MM, Rannou F, Quintero N, Nys A, Mace Y, Poiraudeau S, Drapé JL, Revel M. Relation of inflammatory Modic changes to intradiscal steroid injection outcome in chronic low back pain. Eur Spine J. 2007;16:925–931. doi: 10.1007/s00586-006-0301-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Masaryk TJ, Boumphrey F, Modic MT, Tamborrello C, Ross JS, Brown MD. Effects of chemonucleolysis demonstrated by MR imaging. J Comput Assist Tomogr. 1986;10:917–923. doi: 10.1097/00004728-198611000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–186. doi: 10.1148/radiology.168.1.3289089. [DOI] [PubMed] [Google Scholar]
- 9.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 10.Ohtori S, Inoue G, Ito T, Koshi T, Ozawa T, Doya H, et al. Tumor necrosis factor-immunoreactive cells and PGP 9.5-immunoreactive nerve fibers in vertebral endplates of patients with discogenic low back pain and Modic type 1 or type 2 changes on MRI. Spine. 2006;31:1026–1031. doi: 10.1097/01.brs.0000215027.87102.7c. [DOI] [PubMed] [Google Scholar]
- 11.Rannou F, Ouanes W, Boutron I, Lovisi B, Fayad F, Mace Y, Borderie D, Guerini H, Poiraudeau S, Revel M. High-sensitivity C-reactive protein in chronic low back pain with vertebral end-plate Modic signal changes. Arthritis Rheum. 2007;57:1311–1315. doi: 10.1002/art.22985. [DOI] [PubMed] [Google Scholar]
- 12.Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS. Association between sciatica and Propionibacterium acnes. Lancet. 2001;357:2024–2025. doi: 10.1016/S0140-6736(00)05109-6. [DOI] [PubMed] [Google Scholar]
- 13.Stumpe KD, Zanetti M, Weishaupt D, Hodler J, Boos N, Schulthess GK. FDG positron emission tomography for differentiation of degenerative and infectious endplate abnormalities in the lumbar spine detected on MR imaging. AJR Am J Roentgenol. 2002;179:1151–1157. doi: 10.2214/ajr.179.5.1791151. [DOI] [PubMed] [Google Scholar]
- 14.Toyone T, Takahashi K, Kitahara H, Yamagata M, Murakami M, Moriya H. Vertebral bone-marrow changes in degenerative lumbar disc disease: an MRI study of 74 patients with low back pain. J Bone Joint Surg Br. 1994;76:757–764. [PubMed] [Google Scholar]
- 15.Wedderkopp N, Thomsen K, Manniche C, Kolmos HJ, Secher Jensen T, Leboeuf Yde C. No evidence for presence of bacteria in Modic type I changes. Acta Radiol. 2009;50:65–70. doi: 10.1080/02841850802524485. [DOI] [PubMed] [Google Scholar]