Abstract
 Delayed post-traumatic osteonecrosis, also known by its eponym Kummell’s disease, is a rarely reported clinical entity that likely occurs with higher frequency than recognized. We highlight a case of a 75-year-old female household ambulator who presented with significant thoracolumbar pain and delayed T12 collapse after a ground-level fall. The patient had sustained a trivial fall at home 4 months prior to this presentation and had been hospitalized in our institution at that time for a general medical workup. Dedicated spine radiographs were not obtained during this visit. However, lateral chest radiograph demonstrated an intact T12 vertebral body. The patient was able to mobilize successfully with therapy and was discharged home. During the interim between the initial fall and subsequent presentation, she resumed physical activity including ambulating independently and performing various housework. Approximately 4 months following her initial injury, the patient returned to a local emergency department with vague complaints of abdominal pain without any history of recent fall or injury. After an unremarkable workup, the patient was sent home. Ten days later, she represented to our institution’s emergency room with worsening pain. Radiographs and CT scan demonstrated interval collapse of the T12 vertebral body. A linear vacuum cleft was noted on X-rays and CT. An extensive workup to exclude other processes such as malignancy or infection, which was negative, ensued. Delayed post-traumatic vertebral collapse was diagnosed. A trial of medical management and therapy was attempted, but she continued to experience significant pain. A T12 vertebroplasty was therefore offered and performed to stabilize the injury and to relieve the pain. She was subsequently able to be discharged from the hospital and transitioned back to home life. At approximately 2 years following her injury, the patient was noted to be able to ambulate with a walking aid. Her final radiograph after her surgery demonstrated that the T12 vertebroplasty had maintained its height and sagittal alignment. This Grand Round case highlights the clinical presentation of Kummell’s disease. Aspects of the clinical entity that will be discussed include a historical review of the disease, hallmark radiographic findings and treatment options.
Delayed post-traumatic osteonecrosis, also known by its eponym Kummell’s disease, is a rarely reported clinical entity that likely occurs with higher frequency than recognized. We highlight a case of a 75-year-old female household ambulator who presented with significant thoracolumbar pain and delayed T12 collapse after a ground-level fall. The patient had sustained a trivial fall at home 4 months prior to this presentation and had been hospitalized in our institution at that time for a general medical workup. Dedicated spine radiographs were not obtained during this visit. However, lateral chest radiograph demonstrated an intact T12 vertebral body. The patient was able to mobilize successfully with therapy and was discharged home. During the interim between the initial fall and subsequent presentation, she resumed physical activity including ambulating independently and performing various housework. Approximately 4 months following her initial injury, the patient returned to a local emergency department with vague complaints of abdominal pain without any history of recent fall or injury. After an unremarkable workup, the patient was sent home. Ten days later, she represented to our institution’s emergency room with worsening pain. Radiographs and CT scan demonstrated interval collapse of the T12 vertebral body. A linear vacuum cleft was noted on X-rays and CT. An extensive workup to exclude other processes such as malignancy or infection, which was negative, ensued. Delayed post-traumatic vertebral collapse was diagnosed. A trial of medical management and therapy was attempted, but she continued to experience significant pain. A T12 vertebroplasty was therefore offered and performed to stabilize the injury and to relieve the pain. She was subsequently able to be discharged from the hospital and transitioned back to home life. At approximately 2 years following her injury, the patient was noted to be able to ambulate with a walking aid. Her final radiograph after her surgery demonstrated that the T12 vertebroplasty had maintained its height and sagittal alignment. This Grand Round case highlights the clinical presentation of Kummell’s disease. Aspects of the clinical entity that will be discussed include a historical review of the disease, hallmark radiographic findings and treatment options.
Keywords: Kummell’s disease, Delayed vertebral osteonecrosis, Vertebral collapse, Vertebral pseudoarthrosis
Case presentation
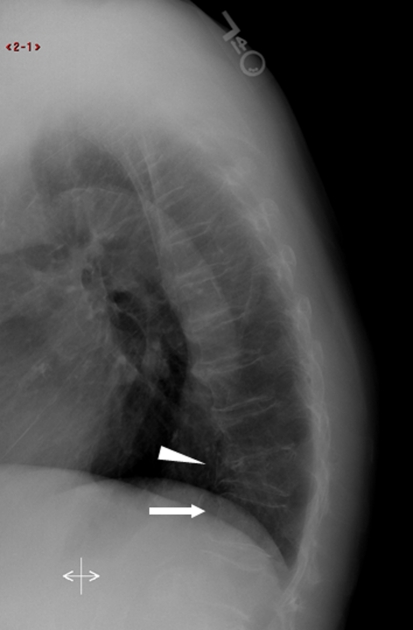
A 75-year-old female household ambulator with a history of dementia, diabetes mellitus type 2, hypertension, hypothyroidism and prior injuries to T11 and L2 presented with thoracolumbar pain in the emergency department after a ground-level fall. The patient complained of weakness and fatigue, which culminated in a fall at home on the morning of presentation. She was hospitalized for a general medical workup and physical therapy. Dedicated spine radiographs were not obtained at that time. However, lateral chest radiograph demonstrated the old T11 injury along with an intact T12 vertebral body (Fig. 1). The patient was able to mobilize successfully with therapy and was subsequently discharged home the following day. During the interim, she was able to resume physical activity including ambulating without a walking aid and performing various housework.
Fig. 1.
Lateral chest radiograph obtained during medical workup at the time of the initial injury. X-ray demonstrated the known old injury to the T11 vertebral body (triangle). Note the intact T12 vertebral body without obvious sign of collapse below (arrow)
Approximately 4 months following her initial injury, the patient returned to an outside hospital’s emergency department with vague complaints of abdominal pain. She endorsed no history of any recent trauma. After an unremarkable workup in the emergency room, the patient was sent home with conservative treatment. Approximately 10 days later, the patient represented to our facility with worsening pain both in the abdomen and thoracolumbar area. The pain was significant and made it difficult for her to perform her daily housework. At that time, she received her first orthopedic evaluation. The family endorsed a 2 weeks history of worsening back pain without known injury. She denied symptoms consistent with radiculopathy.
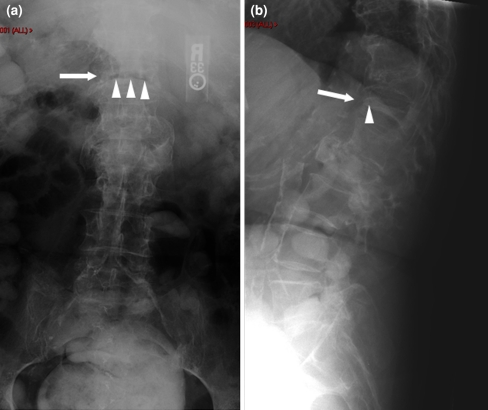
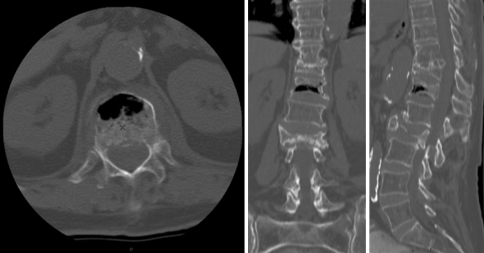
Her spine examination revealed localized axial pain in her thoracolumbar spine. Her motor examination for her lower extremities demonstrated symmetric strength, and no sensory deficits were noted. Radiographs and CT scan at that time demonstrated interval collapse of the T12 vertebral body with minimal retropulsion (Figs. 2, 3). A linear vacuum cleft was noted on X-rays and CT. An extensive workup including MRI and laboratory studies to exclude other processes such as malignancy or infection ensued (Fig. 4). The evaluation was negative. Delayed post-traumatic vertebral collapse was diagnosed. An attempt at conservative management with therapy was tried, but the patient continued to have significant back pain.
Fig. 2.
Repeat radiograph of the T12 vertebral body 4 months after the initial fall (arrow). There is significant collapse of the T12 vertebral body. Intravertebral air (vacuum cleft) can be seen on the AP and lateral projections (triangles). Note the linear shape of the vacuum cleft on the AP X-ray
Fig. 3.
CT scan of the lumbar spine demonstrating the vacuum cleft phenomenon with anterior intraosseous air is identified within the vertebral body. There is minimal compromise of the spinal canal. A small amount of air can also be identified in the T12–L1 disc space
Fig. 4.
MRI of the lumbar spine. The T12 vertebral segment is collapsed. Intraosseous air within the vertebral body can be seen (low signal on both weighted images). Note the intravertebral fluid collection often seen in osteonecrosis (low on T1-weighted images and high on T2-weighted images)
Diagnostic imaging
Historical perspective and diagnosis of Kummell’s disease
This Grand Round case highlights the progression of Kummell’s disease, a relatively rare clinical entity reported in the spine literature. The disease was first publicly presented by Hermann Kummell in 1891 [1]. He observed the delayed development of a painful angular kyphosis in five of his patients that ensued following an initial trivial injury. The injured vertebral body typically is located in the thoracic or lumbar spine with the T12 segment being the most commonly affected [2]. The age range of patients involved in the process is typically middle age or elderly. In their review of English literature, Young et al. [3] had only identified one suspected case of Kummell’s disease in the pediatric population. Given that the anterior vertebral body is a known watershed area, vascular injury leading to impaired bone healing has been proposed as the underlying pathology [3–5] (Figs. 1, 2, 3, 4).
The diagnostic criterion for establishing Kummell’s disease remains unclear and a subject of debate. The disease, as characterized by Kummell, occurred prior to the advent of X-ray imaging. However, as radiographic examination became commonplace, subsequent authors have incorporated an initial negative spine radiograph as a criterion in establishing the spontaneous post-traumatic osteonecrosis inherent in a Kummell’s disease diagnosis. This criterion poses many difficulties given that many trivial back pains that occur after benign mechanisms do not trigger a radiographic examination as with our case presentation. Spine imaging is likely triggered after patients present with recurrence of back pain. By then, the collapse will likely be evident and the patient will likely be diagnosed with an osteoporotic fracture.
Another area of controversy is the role of more sensitive advanced imaging modalities, such as MRI and CT, in establishing Kummell’s disease. One radiographic finding that has been associated with Kummell’s disease is the vacuum cleft phenomenon, which is the accumulation of gas in the affected vertebral body. While this may be at times difficult to visualize on conventional X-rays, this can be easily identified on axial CT scans and reformatted images. Maldague et al. [6] were the first to establish the association between the intravertebral vacuum cleft with Kummell’s disease. Since then, other studies have reported the vacuum cleft phenomenon in other conditions including malignancy [7]. While vacuum clefts are associated with malignancy, research that evaluated the morphology of the vacuum clefts have found that linear-shaped vacuum clefts are almost certainly associated with a benign processes and indicative of ischemic necrosis of the vertebral body [8]. MRI may also be useful to establish the diagnosis of Kummell’s disease. MRI can exclude other causes of vertebral collapse such as malignancy. The intensity of the signals on different weighted images can also be used to delineate a chronic osteoporotic fracture versus osteonecrosis. Chronic osteoporotic fractures are not typically associated with MRI signal changes. Osteonecrosis, on the other hand, has low T1-weighted and increased T2-weighted signals associated with the vertebral cleft [2, 9]. This produces the characteristic ‘double line sign’ on MRI [9].
Rationale for treatment and evidence-based literature
With regard to treatment, a spectrum of options has been described in the literature for Kummell’s disease. Treatment decisions are similar to osteoporotic compression fractures. Factors that are relevant in treatment guidance include patient comorbidities, level of disability and pain, degrees of the kyphotic deformity and presence of neurological compromise. Although early reports were centered on conservative treatment such as bracing and bed rest, more recent reports favor surgical intervention. The advantages of surgery include earlier patient ambulation and correction of the kyphotic deformity.
For acute vertebral collapse with axial back pain, minimally invasive procedures, such as vertebroplasty, are attractive and effective options for pain relief and enable patients to mobilize [10, 11]. Vertebroplasty for vertebral fracture with or without intravertebral clefts have yielded similar results in terms of pain relief [12, 13]. The results with regard to kyphosis reduction, maintenance of disc height and risk of complications, such as cement extrusion after vertebroplasty, for fractures with or without clefts, however, have been heterogeneous [12, 13].
Options for Kummell’s disease with canal compromise and neurological sequelae have traditionally included decompression with instrumentation and fusion [14]. The concern with decompression alone, such as laminectomy, is the progression of the kyphotic deformity, which leads to further complications [15]. Decompression can be approached either anteriorly or posteriorly. The advantage of an anterior approach is the technical ease for removing the retropulsed fragment anteriorly. However, in a patient population where age and comorbidities may be significant, performing a purely posterior procedure to avoid the potential complications associated with violating the thoracic cavity or the retroperitoneal space would also be advantageous. Manual reduction of fracture with transpedicular insertion of vertebral body augments combined with short segment fixation has also been described for fractures with cord compromise [16].
Our patient in the Grand Round case had a T12 injury with minimal retropulsion. Her complaint was axial pain without evidence of neurological symptoms distally. She was not able to mobilize due to her back pain with nonsurgical management, including therapy. Given her age and comorbidities, the family desired a pain-relieving procedure while limiting her surgical risk.
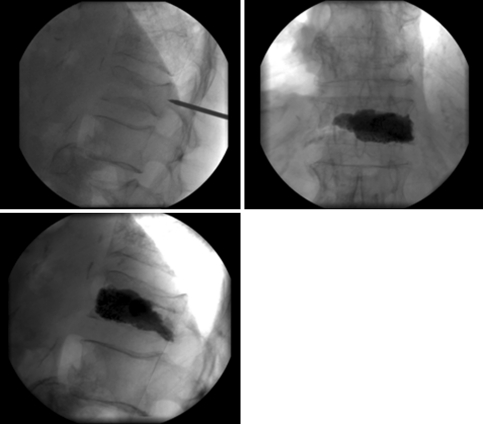
Procedure
A vertebroplasty was therefore offered to stabilize the injury and relieve pain at the T12 level only (Fig. 5). A right transpedicular approach was used for the vertebroplasty. An 11-gauge needle was placed with the tip of the needle located in the midline on AP view, and in the anterior 1/3 of the vertebral body in the lateral view. Subsequently, PMMA mixed with sterile barium sulfate was injected into the vertebral body. Post-vertebroplasty images demonstrate amorphous filling of the vertebral body bilaterally without extravasation of cement beyond the confines of the vertebral body.
Fig. 5.
Intraoperative fluoroscopic imaging demonstrating the vertebroplasty of T12
Outcome
The patient was able to be discharged to a skilled nursing facility after the vertebroplasty for additional daily physical therapy. She was then transitioned back home to her family and additional therapy following the vertebroplasty. She was not completely pain-free following the vertebroplasty. However, the procedure did reduce her pain sufficiently to allow her walk once again and perform portions of her housework. After 2 years following her procedure, her spine radiographs demonstrated that the vertebroplasty had maintained its height and sagittal alignment (Figs. 5, 6).
Fig. 6.
Radiograph obtained after 2 years following vertebroplasty. Height of the T12 vertebral body is maintained along with sagittal alignment
References
- 1.Kummell H. Die rarefizierende Ostitis der Wirbelkörper. Deutsche Med. 1895;21:180–181. doi: 10.1055/s-0029-1199707. [DOI] [Google Scholar]
- 2.Osterhouse MD, Kettner NW. Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J Manipulative Physiol Ther. 2002;25(4):270–275. doi: 10.1067/mmt.2002.123164. [DOI] [PubMed] [Google Scholar]
- 3.Young WF, Brown D, Kendler A, Clements D. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell’s disease) Acta Orthop Belg. 2002;68(1):13–19. [PubMed] [Google Scholar]
- 4.Chou LH, Knight RQ. Idiopathic avascular necrosis of a vertebral body. Case report and literature review. Spine (Phila Pa 1976) 1997;22(16):1928–1932. doi: 10.1097/00007632-199708150-00024. [DOI] [PubMed] [Google Scholar]
- 5.Swartz K, Fee D. Kummell’s disease: a case report and literature review. Spine (Phila Pa 1976) 2008;33(5):E152–E155. doi: 10.1097/BRS.0b013e3181657f31. [DOI] [PubMed] [Google Scholar]
- 6.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978;129(1):23–29. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 7.Mirovsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum clefts of the vertebral bodies. AJNR Am J Neuroradiol. 2005;26(7):1634–1640. [PMC free article] [PubMed] [Google Scholar]
- 8.Bhalla S, Reinus WR. The linear intravertebral vacuum: a sign of benign vertebral collapse. AJR Am J Roentgenol. 1998;170(6):1563–1569. doi: 10.2214/ajr.170.6.9609175. [DOI] [PubMed] [Google Scholar]
- 9.Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ. Vertebral osteonecrosis: MR imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol. 2007;28(1):42–47. [PMC free article] [PubMed] [Google Scholar]
- 10.dS I, Fransen H. Percutaneous vertebroplasty as treatment for Kummell’s disease. JBR-BTR. 2009;92(2):83–85. [PubMed] [Google Scholar]
- 11.Do HM, Jensen ME, Marx WF, Kallmes DF (1999) Percutaneous vertebroplasty in vertebral osteonecrosis (Kummell’s spondylitis). Neurosurg Focus 7(1):e2 [DOI] [PubMed]
- 12.Ha KY, Lee JS, Kim KW, Chon JS. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br. 2006;88(5):629–633. doi: 10.1302/0301-620X.88B5.17345. [DOI] [PubMed] [Google Scholar]
- 13.Krauss M, Hirschfelder H, Tomandl B, Lichti G, Bar I. Kyphosis reduction and the rate of cement leaks after vertebroplasty of intravertebral clefts. Eur Radiol. 2006;16(5):1015–1021. doi: 10.1007/s00330-005-0056-6. [DOI] [PubMed] [Google Scholar]
- 14.Kim KT, Suk KS, Kim JM, Lee SH. Delayed vertebral collapse with neurological deficits secondary to osteoporosis. Int Orthop. 2003;27(2):65–69. doi: 10.1007/s00264-002-0418-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kempinsky WH, Morgan PP, Boniface WR. Osteoporotic kyphosis with paraplegia. Neurology. 1958;8(3):181–186. doi: 10.1212/wnl.8.3.181. [DOI] [PubMed] [Google Scholar]
- 16.Li KC, Li AF, Hsieh CH, Liao TH, Chen CH. Another option to treat Kummell’s disease with cord compression. Eur Spine J. 2007;16(9):1479–1487. doi: 10.1007/s00586-006-0094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]