Abstract
Unidentified nerve root anomalies, conjoined nerve root (CNR) being the most common, may account for some failed spinal surgical procedures as well as intraoperative neural injury. Previous studies have failed to clinically discern CNR from herniated discs and found their surgical outcomes as being inferior. A comparative study of CNR and disc herniations was undertaken. Between 2002 and 2008, 16 consecutive patients were diagnosed intraoperatively with CNR. These patients were matched 1:2 with 32 patients diagnosed with intervertebral disc herniations. Matching was done according to age (within 5 years), gender and level of pathology. Surgery for patients with CNR or disc herniations consisted of routine microsurgical techniques with microdiscectomy, hemilaminotomy, hemilaminectomy and foraminotomy as indicated. Outcomes were measured using the Oswestry Disability Index and the Short Form-36 Questionnaire. Clinical presentation, imaging studies and surgical outcomes were compared between the groups. Conjoined nerve root’s incidence in this study was 5.8% of microdiscectomies performed. The S1 nerve root was mainly involved (69%), followed by L5 (31%). Patients with CNR tended to present with nerve root claudication (44%) compared to the radiculopathy accompanying disc herniations (75%). Neurologic deficit was less prevalent among patients with CNR. Nerve root tension tests were not helpful in distinguishing between the etiologies. Radiologist’s suspicion threshold for nerve root anomalies was low (0%) and no coronal reconstructions were obtained. The surgeon’s clinical suspicion accurately predicted 40% of the CNRs. Surgical outcomes did not differ between the cohorts regarding the rate of postoperative improvement, but CNR patients showed a trend toward having mildly worse long-term outcomes. Suspecting CNRs preoperatively is beneficial for appropriate treatment and avoiding the risk of intraoperative neural injury. With nerve root claudication and imaging suggestive of a “disc herniation”, the surgeon should be alert to the differential diagnosis of a CNR. Treatment is directed at obtaining adequate decompression by laminectomy and foraminotomy to relieve the lateral recess stenosis. Outcomes can be expected to be similar to routine disc herniations.
Keywords: Conjoined lumbosacral nerve roots, Lumbar disc herniation, Surgical outcome, Nerve root anomalies
Introduction
Conjoined lumbosacral nerve roots (CNR) are composed of two adjacent nerve roots, which share a common dural envelope at some time during their coursing from the thecal sac. CNR incidence is reported to be 2–17.3% in patients undergoing lumbar spine imaging (CT, MRI and myelography) [1–8] and as high as 30% in cadaveric studies [9, 10]. Nerve root anomalies are mentioned as differential diagnosis to herniated intervertebral discs [2, 5].
Although CNR case series are scarce with few patients each, there are five classification systems [8, 10–13]. No study has identified any specific or sensitive clinical pattern that uniquely distinguishes CNR. Lack of straight leg raising sign is more suggestive of CNR than disc herniation, as this sign generally indicates an acute inflammatory response [14]. A CNR may be subject to overcrowding in its nerve canal and claudication symptoms would seem logical; however, a secondary radicular component may occur with flares of inflammation. The clinical presentation of CNR is “lumbosciatic pain” due to the crowding of two nerve roots in the same foramen or lateral recess.
Symptomatic and undiagnosed CNR is one of the causes of failed back surgery, as a simple discectomy without adequate lateral recess and foraminal decompression does not address the pathology [2, 15]. Furthermore, inadvertent nerve route injury can occur or battered nerve syndrome if the second nerve in the field is not appreciated.
Diagnosis is usually made with computerized tomography (CT) [3, 7, 16], water-soluble contrast myelography [4, 16–19], high-quality magnetic resonance imaging (MRI) with coronal views [1, 2, 6, 16, 20–22], or intraoperatively [8, 15, 23–25]. Radiological diagnosis is still challenging despite the improvement in imaging modalities.
The primary purpose of this study was to examine the surgical outcomes of patients with CNR. A secondary purpose was to compare and contrast the presenting history and signs between patients who were diagnosed with disc herniation, but ultimately found to have CNR at surgery.
Materials and methods
Between 2002 and 2008, 16 patients were diagnosed intraoperatively with conjoined nerve root. The preoperative diagnosis was disc herniation from the referring doctor and the radiologist report. There was a suspicion of conjoined nerve root in some patients based on symptoms and past personal experience of the senior surgeon. All patients were treated by microsurgical unilateral decompression. During the same time period, 260 were treated in a similar fashion, but diagnosis was an expected disc herniation. All surgeries were performed by a single fellowship trained spine surgeon. Surgery for CNR consisted of hemilaminectomy, partial pediculectomy and foraminotomy with or without discectomy. Surgical outcomes, Oswestry Disability Index (ODI) and the Short Form-36 Questionnaire (SF-36) were measured preoperatively, and 6 weeks, 3 months and 6 months postoperatively. Where disc herniation was present without CNR, routine microdiscectomy was performed with lateral recess and foraminal decompression performed as indicated.
The CNR cohort was matched 1:2 with 32 patients diagnosed with intervertebral disc herniations. Matching was done according to age (within 5 years), gender and level of pathology. Surgical outcomes for the control group were collected prospectively in the same fashion as for the CNR cohort. The initial clinical presentation (claudication, radiculopathy), physical examination (straight leg raising, neurologic deficit), imaging studies (CT and MRI) and surgical outcomes were compared between the groups.
Chi square was used to test for difference in proportions in clinical presentation between the groups of CNR and herniated intervertebral disc. Student’s t test was used for determining statistically significant differences between the standardized means for the SF-36 and the means of the ODI.
Results
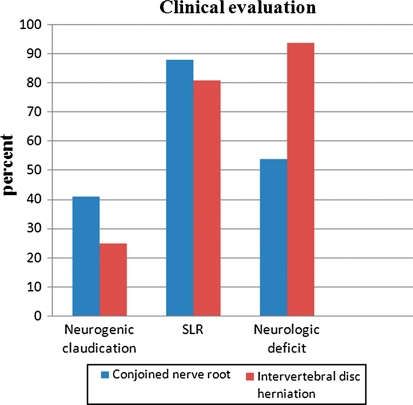
The incidence of CNR identified at surgery in this cohort was 5.8%. The L5–S1 nerve roots were most frequently involved in accordance with the published data. This occurred in 69% of the cases. An L4–L5 CNR occurred in 31%. Clinical presentation differed in patients with CNR. The pattern of pain was more commonly claudication as a prodrome with or without the development of radiculopathy. Claudication was defined as symptoms in the leg that correspond to a nerve root distribution, which can include pain, numbness or weakness but being manifested with activity such as walking or standing. Generally, claudicant symptoms are relieved with sitting or cessation of activity. This occurred in 44% of the patients with CNR compared to 25% of the disc herniation patients. This was significantly different, p < 0.05. Radicular symptoms with rest pain were more frequent in the disc herniation patients, 75 versus 56% (p < 0.05) (Fig. 1). Radiculopathy is defined as constant nerve root symptoms, which are present with activity and also with rest. Generally, sitting or standing does not affect radiculopathy. Neurologic deficits such as anesthesia over a dermatome or motor weakness were less prevalent among patients with CNR 55 versus 94% (p < 0.05). Nerve root tension tests were not helpful in distinguishing between CNR and disc herniations, as both cohorts had similar rates of positive straight leg raising (SLR) tests.
Fig. 1.
Clinical evaluation of intervertebral disc herniation and CNR
Of the 16 CNR identified intraoperatively, only three patients (18.75%) underwent a microdiscectomy while boney decompression only was deemed necessary for the remaining patients.
The correct diagnosis of a CNR made by the authors preoperatively based on history, clinical examination and review of the imaging studies was correct in 40% of the cases. CNR was never suspected by the radiologists.
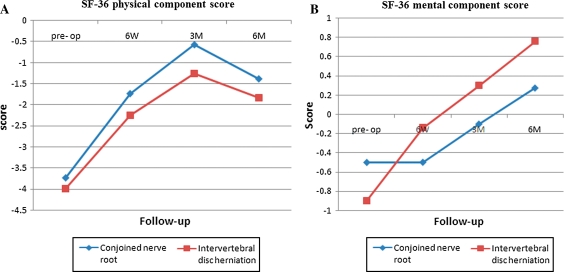
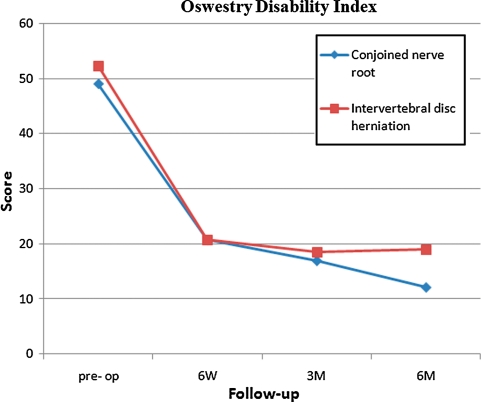
Figure 2a, b depicts the mean and the standard deviation of SF-36 outcome measuring scales pre-operatively, at 6 weeks, and 3 and 6 months in each group. SF-36 components showed the same pattern of postoperative improvement; however, the CNR cohort had a consistently lesser degree of improvement. In contrast, the ODI (Fig. 3) did not differ between the cohorts regarding the amount or rate of postoperative improvement. One patient in the CNR cohort required a revision decompression due to recurrence of symptoms. Reimaging showed continued lateral recess stenosis. There were no recurrent disc herniations in the disc herniation group within the study period.
Fig. 2.
a SF-36 mental component score. b SF-36 physical component score
Fig. 3.
Oswestry Disability Index score
Discussion
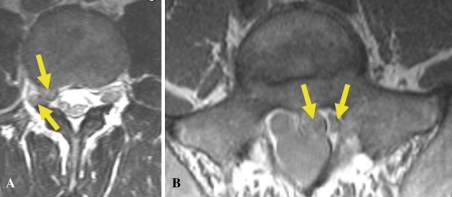
Suspecting CNRs preoperatively is beneficial for appropriate treatment and avoiding the risk of intraoperative neural injury, which can be due to traumatic manipulation or retraction with little mobility of the nerve. Potentially, one may cut the nerve if a second nerve overlying the disc space is not suspected. The CNR cohort in this study did not have any perioperative complications; however, they were identified either preoperatively or intraoperatively. Previous studies have described the potential hazards of unrecognized CNR at spinal surgery. There should be a heightened awareness of CNR if there is a prodrome of claudicant symptoms concurrent with or preceding radiculopathy. SLR test was found to be unreliable in the diagnosis of CNR. Imaging findings can range from more discrete features (Fig. 4a, b) to less obvious ones, which resemble a disc herniation. However, there are unique features that appear to be more typical of CNR. Reported MRI signs for CNR have previously been noted to include the almost equal density of the nerve root anomaly and the thecal sac, an asymmetry or pouching out of the subarachnoid space in the axial view and the location of the root anomaly, which is often above the intervertebral disc space [1, 2, 6, 20–22]. Song et al. [22] found three MRI signs for CNR: a “corner” (asymmetric morphology of the anterolateral corner of the dural sac), “fat crescent” (intervening extradural fat between the asymmetric dura and the nerve root) and the “parallel” sign (visualization of the entire parallel course of the nerve root at the disc level). If there is clinical suspicion of a CNR based on patient’s history, or the initial MRI is suggestive of CNR, we agree with the recommendations for further coronal reformations that better outline a CNR [6, 7, 15–17, 20, 22].
Fig. 4.
a A pair of nerve roots exiting a single foramen. b Fat crescent sign between nerve roots
The CNR pathoanatomy is a result of focal lateral recess and foraminal stenosis. Creating room for the increased nerve tissue in the exit zone and foramen is paramount for treatment. A variety of surgical procedures such as pediculectomy and facetectomy have been described as treatment for CNR [8, 13–15, 19, 23–27]. In our study, the surgery consisted of a hemilaminectomy, lateral recess decompression, partial pediculectomy and foraminotomy. The goal of all approaches is to achieve adequate decompression. In 18% of our patients, a microdiscectomy was also performed as the disc was bulging or herniated and contributed to the neurocompression. This subgroup consisted of only three patients, so a specific surgical outcome analysis was impossible. CNR surgical outcomes have varied in literature from 30% good results to results comparable to microdiscectomy. In our cohort, there were comparable outcomes between the groups with no statistical differences; however, there was a trend for inferior outcomes at 6 months in the CNR group. We can postulate that the CNR group may have other factors that affect recovery, such as the longer time course of compression or less nerve mobility.
Summary
Conjoined nerve roots occurred in our experience in over 5% of cases, which were classified preoperatively as “disc herniation”. The clinical picture that should raise awareness of this entity is a prodrome of claudication with or without radiculopathy. Certain MRI imaging findings should raise awareness of a CNR, particularly in the context of a mixed claudication/radiculopathy pain pattern. MRI coronal reformats may increase the preoperative identification of CNR. Preoperative awareness may reduce the risk of inadvertent nerve root injury. The treatment entails decompression of the bony canal of the nerve root exit zone. Outcomes are comparable to those of disc herniations, provided surgical management addresses the pathology of lateral recess stenosis. The earlier reported poorer results of CNR may reflect the lack of appreciation of the finding and inadequate decompression.
References
- 1.Aota Y, Saito Y, Yoshikawa K, Asada T, Kondo S, Watanabe K. Presurgical identification of extradural nerve root anomalies by coronal fat-suppressed magnetic resonance imaging: a report of six cases and a review of the literature. J Spinal Disord. 1997;10(2):167–175. doi: 10.1097/00002517-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Artico M, Carloia S, Piacentini M, Ferretti G, Dazzi M, Franchitto S, et al. Conjoined lumbosacral nerve roots: observations on three cases and review of the literature. Neurocirugia (Astur) 2006;17(1):54–59. doi: 10.1016/s1130-1473(06)70370-0. [DOI] [PubMed] [Google Scholar]
- 3.Broom MJ. Congenital anomalies of the lumbosacral spine causing nerve root entrapment: the role of high-resolution CT in diagnosis. Orthopedics. 1994;17(1):63–67. doi: 10.3928/0147-7447-19940101-11. [DOI] [PubMed] [Google Scholar]
- 4.Cail WS, Butler AB (1983) Conjoined lumbosacral nerve roots. Diagnosis with metrizamide myelography. Surg Neurol 20(2):113–119 [DOI] [PubMed]
- 5.Gado M, Patel J, Hodges FJ 3rd (1983) Lateral disk herniation into the lumbar intervertebral foramen: differential diagnosis. AJNR Am J Neuroradiol 4(3):598–600 [PMC free article] [PubMed]
- 6.Haijiao W, Koti M, Smith FW, Wardlaw D. Diagnosis of lumbosacral nerve root anomalies by magnetic resonance imaging. J Spinal Disord. 2001;14(2):143–149. doi: 10.1097/00002517-200104000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Peyster RG, Teplick JG, Haskin ME (1985) Computed tomography of lumbosacral conjoined nerve root anomalies. Potential cause of false-positive reading for herniated nucleus pulposus. Spine 10(4):331–337 [DOI] [PubMed]
- 8.Postacchini F, Urso S, Ferro L. Lumbosacral nerve-root anomalies. J Bone Joint Surg Am. 1982;64(5):721–729. [PubMed] [Google Scholar]
- 9.Chotigavanich C, Sawangnatra S (1992) Anomalies of the lumbosacral nerve roots. An anatomic investigation. Clin Orthop Relat Res. May(278):46–50 [PubMed]
- 10.Kadish LJ, Simmons EH. Anomalies of the lumbosacral nerve roots. An anatomical investigation and myelographic study. J Bone Joint Surg Br. 1984;66(3):411–416. doi: 10.1302/0301-620X.66B3.6725353. [DOI] [PubMed] [Google Scholar]
- 11.Cannon BW, Hunter SE, Picaza JA. Nerve-root anomalies in lumbar-disc surgery. J Neurosurg. 1962;19:208–214. doi: 10.3171/jns.1962.19.3.0208. [DOI] [PubMed] [Google Scholar]
- 12.Kikuchi S, Hasue M, Nishiyama K, Ito T. Anatomic and clinical studies of radicular symptoms. Spine. 1984;9(1):23–30. doi: 10.1097/00007632-198401000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Neidre A, MacNab I. Anomalies of the lumbosacral nerve roots. Review of 16 cases and classification. Spine. 1983;8(3):294–299. doi: 10.1097/00007632-198304000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Taghipour M, Razmkon A, Hosseini K. Conjoined lumbosacral nerve roots: analysis of cases diagnosed intraoperatively. J Spinal Disord Tech. 2009;22(6):413–416. doi: 10.1097/BSD.0b013e31818f00a0. [DOI] [PubMed] [Google Scholar]
- 15.Scuderi GJ, Vaccaro AR, Brusovanik GV, Kwon BK, Berta SC. Conjoined lumbar nerve roots: a frequently underappreciated congenital abnormality. J Spinal Disord Tech. 2004;17(2):86–93. doi: 10.1097/00024720-200404000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Bottcher J, Petrovitch A, Soros P, Malich A, Hussein S, Kaiser WA. Conjoined lumbosacral nerve roots: current aspects of diagnosis. Eur Spine J. 2004;13(2):147–151. doi: 10.1007/s00586-003-0634-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouchard JM, Copty M, Langelier R. Preoperative diagnosis of conjoined roots anomaly with herniated lumbar disks. Surg Neurol. 1978;10(4):229–231. [PubMed] [Google Scholar]
- 18.Coughlin JR, Miller JD. Metrizamide myelography in conjoined lumbosacral nerve roots. J Can Assoc Radiol. 1983;34(1):23–25. [PubMed] [Google Scholar]
- 19.Maiuri F, Gambardella A. Anomalies of the lumbosacral nerve roots. Neurol Res. 1989;11(3):130–135. doi: 10.1080/01616412.1989.11739877. [DOI] [PubMed] [Google Scholar]
- 20.Hashimoto M, Watanabe O, Hirano H. Extraforaminal stenosis in the lumbosacral spine. Efficacy of MR imaging in the coronal plane. Acta Radiol. 1996;37(5):610–613. doi: 10.3109/02841859609177684. [DOI] [PubMed] [Google Scholar]
- 21.Savas R, Calli C, Yunten N, Alper H. Hypoplastic lumbar pedicle in association with conjoined nerve root MRI demonstration. Comput Med Imaging Graph. 1998;22(1):77–79. doi: 10.1016/S0895-6111(98)00003-2. [DOI] [PubMed] [Google Scholar]
- 22.Song SJ, Lee JW, Choi JY, Hong SH, Kim NR, Kim KJ, et al. Imaging features suggestive of a conjoined nerve root on routine axial MRI. Skeletal Radiol. 2008;37(2):133–138. doi: 10.1007/s00256-007-0403-6. [DOI] [PubMed] [Google Scholar]
- 23.Prestar FJ. Anomalies and malformations of lumbar spinal nerve roots. Minim Invasive Neurosurg. 1996;39(4):133–137. doi: 10.1055/s-2008-1052233. [DOI] [PubMed] [Google Scholar]
- 24.Stambough JL, Balderston RA, Booth RE, Rothman RH. Surgical management of sciatica involving anomalous lumbar nerve roots. J Spinal Disord. 1988;1(2):111–114. doi: 10.1097/00002517-198801020-00002. [DOI] [PubMed] [Google Scholar]
- 25.White JG, 3rd, Strait TA, Binkley JR, Hunter SE. Surgical treatment of 63 cases of conjoined nerve roots. J Neurosurg. 1982;56(1):114–117. doi: 10.3171/jns.1982.56.1.0114. [DOI] [PubMed] [Google Scholar]
- 26.Epstein JA, Carras R, Ferrar J, Hyman RA, Khan A. Conjoined lumbosacral nerve roots. Management of herniated discs and lateral recess stenosis in patients with this anomaly. J Neurosurg. 1981;55(4):585–589. doi: 10.3171/jns.1981.55.4.0585. [DOI] [PubMed] [Google Scholar]
- 27.Pamir MN, Ozek MM, Ozer AF, Keles GE, Erzen C. Surgical considerations in patients with lumbar spinal root anomalies. Paraplegia. 1992;30(5):370–375. doi: 10.1038/sc.1992.85. [DOI] [PubMed] [Google Scholar]