Abstract
Currently, there are over 300,000 lumbar discectomies performed in the US annually without an objective standard for patient selection. A prospective clinical outcome study of 200 cases with 5-year follow-up was used to develop and validate an MRI-based classification scheme to eliminate as much ambiguity as possible. 100 consecutive lumbar microdiscectomies were performed between 1992 and 1995 based on the criteria for “substantial” herniation on MRI. This series was used to develop the MSU Classification as an objective measure of lumbar disc herniation on MRI to define “substantial”. It simply classifies herniation size as 1-2-3 and location as A-B-C, with inter-examiner reliability of 98%. A second prospective series of 100 discectomies was performed between 2000 and 2002, based on the new criteria, to validate this classification scheme. All patients with size-1 lesions were electively excluded from surgical consideration in our study. The Oswestry Disability Index from both series was better than most published outcome norms for lumbar microdiscectomy. The two series reported 96 and 90% good to excellent outcomes, respectively, at 1 year, and 84 and 80% at 5 years. The most frequent types of herniation selected for surgery in each series were types 2-B and 2-AB, suggesting the combined importance of both size and location. The MSU Classification is a simple and reliable method to objectively measure herniated lumbar disc. When used in correlation with appropriate clinical findings, the MSU Classification can provide objective criteria for surgery that may lead to a higher percentage of good to excellent outcomes.
Keywords: MRI, Discectomy, Classification, Substantial herniated disc, Low back pain
Introduction
Lumbar discectomy is by itself the most common surgical procedure performed in the US for patients suffering from back pain and sciatica, with over 300,000 discectomy procedures done yearly [2, 6]. When treatment outcomes are discussed, acute disc herniations have normally all been lumped into one category. This is probably largely due to the fact that the common variables used in surgical selection normally lack basic objective criteria, and, on account of it, numbers of surgeries per capita may differ substantially from region to region, and from surgeon to surgeon across the United States [19, 20]. This degree of variability may clearly affect the individual rate of success for discectomy patients. Weber [18] indicated that three categories of clinical patients exist within the diagnosis of lumbar disc herniation: one group that beyond a doubt required surgical intervention, a second group that had no good indication for surgery, and a third group of patients for whom surgical indications were less certain. It might be especially useful, among this third group of patients, to have a valid objective standard by which to measure herniated disc on MRI to assist with the overall assessment of the problem, the surgical selection process, and the research of post-operative outcomes, involving comparable levels of pathology.
Although proper assessment of changes on the MRI scan is a key overall component that needs to be factored into the selection process for lumbar disc surgery, Boden and others [3, 10] make it clear that abnormal MRI scans can occur in otherwise asymptomatic patients; hence, clinical correlation is always essential prior to any surgical consideration. On the other hand, it is also known that patients may present with clinical signs and symptoms that suggest the diagnosis of acute herniated disc, and yet lack evidence of sufficient pathology on MRI to warrant surgery. Several authors have already cited the potential value of volumetric analysis of herniated disc on MRI as part of the selection criteria for lumbar surgery [5, 11, 12, 16, 17]. In a practical sense, surgery would seem best indicated in symptomatic cases, where disc herniation is substantial enough, so that its removal would relieve a sufficient level of nerve root compression, or stretch, or both, translating into a successful post-operative outcome.
Simple, yet accurate and objective criteria that could serve to qualify “substantial” herniated disc in terms of both size and location constraints could prove useful to surgeons. In cases where sufficient surgical criteria are not met, conservative treatment, such as epidural steroid injections, physical therapy and osteopathic manipulation, might be deemed the more appropriate choice. In regard to cases where smaller disc pathology exists on MRI, it has already been suggested that symptoms related to sciatica may be associated with a chemical neuritis caused by proteoglycans, nerve root adhesions caused by local inflammation [14] or pain magnification dependent on the patient’s subjective functional response. In addition to this, several authors have suggested that smaller sized, contained disc lesions fare more poorly clinically following surgery, and there is a greater propensity (as high as 40%) for recurrent herniation afterward [4]. Conversely, with respect to larger herniations, Carragee et al. [4] report that larger disc fragments, associated with frank annular defects, appear to fare better following lumbar microdiscectomy with as little as 3.5% recurrence rate afterward. These facts suggest that any MRI criteria that did nothing more than help reduce the frequency of surgical annulotomy for small disc herniation, could, all by itself, improve surgical outcomes.
Better selection criteria are ones that provide a simple description that can be universally understood, resulting in good inter-examiner agreement. Fardon and Milette [9] extensively studied the difficulties posed by terminology used by American surgeons and radiologists in reporting lumbar disc pathology in terms of size, location, and type. Wiltse et al. [21] addressed such difficulties by describing lumbar disc herniation in terms of anatomic location, reported as zones and levels, and defining words that describe normal, mild, moderate, moderately severe, and severe as a number from one to five. Though McCulloch’s classification [21] remains relatively useful in discussing spinal pathology, it is subjective and fails by enlarge to precisely delineate size and location with respect to individual anatomic variations. Therefore, the purpose of this study was to develop and validate a more objective classification scheme to eliminate as much ambiguity as possible. Instead of employing anatomic terminology and subjective size estimates, the MSU Classification reports size and location in three precise increments, described simply 1-2-3 and A-B-C, all taken from a single measurement of the intra-facet line. We showed that this classification (1) defined the term “substantial” in more precise terms and (2) provided a consistent and objective description of disc herniation, resulting in excellent inter-examiner reliability.
Methods
Study design
Two 5-year clinical outcome studies were done based on two separate series of 100 consecutive patients who underwent microdiscectomy for acute herniated lumbar disc. All patients presented to the MSU Spine Center with consistent symptoms of back pain and sciatica between the years 1992–1995 and 2000–2002. All surgeries were performed by the first author at Ingham Regional Orthopedic Hospital. All patients, before and after surgery, were evaluated according to the Oswestry Disability Index [7, 8], and followed up for a period of 5 years, reaching completion of the second series in 2007.
The first series of 100 patients were selected for surgery on the basis of both clinical symptoms and the presence of substantially large lumbar disc herniation on MRI, determined as moderately severe or severe by usual subjective criteria [15]. A retrospective evaluation of all MRIs in this first series was used to develop the MSU Classification. To test its reliability, a blind review of 30 random lumbar MRI studies from that first series was performed independently by three different examiners using the new classification.
A second series of 100 clinically symptomatic patients, selected for surgery with the aid of the MSU Classification, was used to validate the scheme. The outcomes from this second series were, in turn, compared to and combined with the outcomes from the first series to assess overall surgical outcomes.
MSU Classification
The MSU Classification takes into account both the size of disc herniation and its location within the various constraints posed by the local anatomy. It employs a single intra-facet line as a reference point to measure the disc herniation at the level of maximum extrusion, where the most impact on neurologic structures likely occurs. This measurement is taken from the T2 axial MRI cut that corresponds best with the level of maximal herniation, taking into account cephalad or caudal disc displacement. In our experience, whether the greatest dimension of this space occupying lesion is located more caudal or more cephalad has had no critical bearing on whether or not the disc herniation was suited for surgery. Level is only important in terms of where to take the measurements of grade and zone, and as part of the surgeon’s pre-operative planning for precise removal of the lesion. Therefore, level has not been included in our classification.
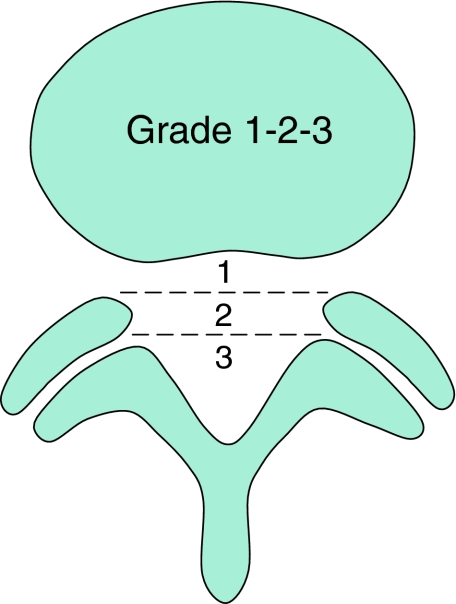
The size and location of disc herniation are measured at the level of maximal extrusion in reference to a single intra-facet line drawn transversely across the lumbar canal, to and from the medial edges of the right and left facet joint articulations (Fig. 1). To portray the size of disc herniation, the lesion is described as 1, 2, or 3. In reference to the intra-facet line, a determination is made as to whether the disc herniation extends up to or less than 50% of the distance from the non-herniated posterior aspect of the disc to the intra-facet line (size-1), or more than 50% of that distance (size-2). If the herniation extends altogether beyond the intra-facet line, it is termed a size-3 disc. In cases of more caudal or more cephalad maximal extrusions, this measurement is taken from the posterior edge of the vertebral cortex/endplate instead of the disc.
Fig. 1.
Grading the disc herniation for size. Grade 1 lesions have little impact and grade 3 have the most impact on nerve compression
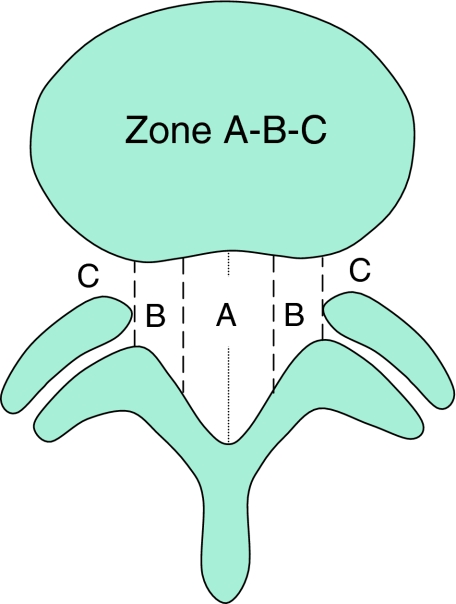
To further qualify location of the disc herniation, the lesion is described as A, B, or C to more exactly locate the position that is routinely, but less accurately, reported as central, lateral or far lateral. Three points are placed along the intra-facet line, dividing it into four equal quarters (Fig. 2). Then, perpendicular lines are drawn through each of these points to create the right and left lateral and right and left central quadrants. The right and left central quadrants represent zone-A. The right and left lateral quadrants represent zone-B. A third zone-C is represented at the level of the foramen by the area that extends beyond the medial margin of either facet joint, past the borderline of the lateral quadrants. It is there, where the herniation extends out into the intra-foraminal space and beyond on the right and left sides, that the lesion is traditionally referred to as far lateral. The lateral zones-B and -C are obviously anatomically more constrained spaces than the more roomy zone-A, which is centered in the middle of the spinal canal. It is, therefore, not surprising that when a size-2 disc herniation occurs within either of the two more constrained zones-B and -C, it typically exerts a greater impact on the spinal nerves. The determination, as into which zone the herniated nucleus intrudes furthest, qualifies the lesion as A, AB, B, or C (Fig. 3).
Fig. 2.
Zoning the disc for location. Lesions have more impact in tighter zone-B and -C
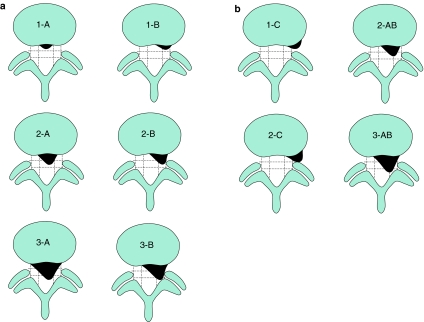
Fig. 3.
Combining size and location. a Lesions 2-B are commonly symptomatic. 3A lesions are often seen in cauda equina. b Lesions 2-C are the largest foraminal lesions. Lesions 2-AB are quite common, occurring on the line between zones-A and -B
Patient population
The average age of the patients with acute lumbar herniated discs in the two combined studies was 35 years, with a standard deviation of 6.5. 59% of the patients were male; 41% were female. 61% of the patients were operated upon for L5–S1 disc herniation, 37% for L4–5, and only 2% for L3–4. Leg pain in every case outweighed the intensity of back pain. Pain was rated by the patient as at least a 7 in all cases, with most patients reporting a 9 or 10 on a scale of 10 at the time of surgery. 98% of the patients had symptoms of sciatic notch pain. All patients reported discreet radicular sensory patterns suggesting one or two dermatome levels, most often L5 or S1 or both. 49% of the patients had some degree of reflex changes, 6% could not walk on their toes, 2.5% of patients had a frank foot drop, and 1% had frank quadriceps weakness prior to surgery. 87% of all patients had positive nerve root tension signs. All patients had either size-2 or size-3 herniations according to the MSU Classification. The majority of patients, whenever feasible, had at least a 6-week trial of conservative treatment prior to surgery, and all patients reported that they were “most tired of the pain” at the time they elected surgery.
Results
Reliability
The three examiners classified acute herniated disc on MRI with a 98% agreement. The only differing grade reported among the three examiners was a single disc herniation out of 30 that was reported as 2-AB by two of the examiners and as 3-AB by the third. Therefore, there were 88 concordant observations out of 90 possible pairs.
Surgery
Of the original 200 patients who underwent surgery in the two combined series, 19 patients were lost to follow-up, so that 181 patients in all were followed-up for 5 years. All 181 of the patients who were selected for surgery had either size-2 or size-3 lesions. All patients with size-1 lesions were electively excluded from surgical consideration in our study. Blood loss in almost every case was minimal, and none of the patients required a transfusion. 1.5%, or a total of three patients, had small inadvertent dural tears, which were repaired at the time of surgery. This complication did not appear to significantly alter the post-operative course in any patient. After 7 to 10 days, as per routine in our practice, all patients in the combined series were prescribed 4–6 weeks of post-operative physical therapy in an effort to restore each patient’s core strength, and to return patients to full activities at a comparably early date. 97% of the patients complied with this recommendation.
Disability scores
Pre-operative scores
The Oswestry Disability Index was used to assess each patient’s function before surgery. The scores for all 181 patients were in the range of 38–81% disability with a mean of 52%, which is described as “severe disability.” All patients, in general, described their pain as the main issue along with physical impairment ranging from some impairment to profound impairment of daily living.
On closer analysis, the range of symptoms reported by patients prior to surgery can be summarized as fairly severe to severe pain levels, inability to lift anything heavy to lifting anything at all, inability to sit for an hour to inability to sit at all, inability to walk a kilometer to inability to walk without crutches, inability to stand less than an hour to barely being able to stand at all, inability to sleep more than 6 h all the way to frank insomnia, some interference caused by pain during sex to a need to abstain from sex altogether, limitation to some or most forms of social life, and travel limitations ranging anywhere from an hour or so to hardly withstanding the trip to the doctor’s office.
Post-operative scores
The Oswestry Disability Index was used to assess each patient’s function at 1- and 5-year post-operative follow-up. GOOD or EXCELLENT outcomes represented minimal to no disability scores of 15% or less. FAIR outcomes represented levels of minimal to moderate disability scored between 15 and 30%. POOR outcomes represented levels of moderate to severe disability scores of greater than 30%.
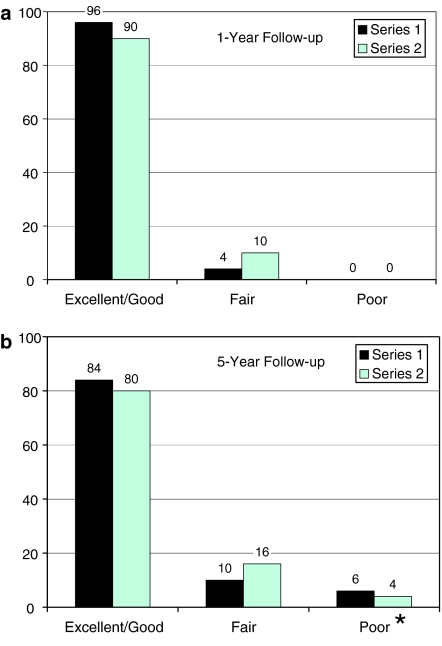
The overall results at 1 and 5 years post-op are summarized in Tables 1 and 2. Out of the total of 181 patients seen at 1-year follow-up, 96% of the patients in the first study and 90% of the patients in the second study were rated as GOOD or EXCELLENT (Fig. 4a). After 5 years, 84% of patients in the first series and 80% of patients in the second series were still rated GOOD or EXCELLENT (Fig. 4b). After 5 years, 10% of the patients in the first series and 16% in the second series were reported as FAIR. Due to problems of recurrent herniation, 6% of the patients in the first series and 4% of the patients in the second series were rated as POOR. Over one half of this latter group of patients required a second operation before the end of 5 years, either re-operative discectomy or a discectomy with fusion. There were no statistically significant differences in the clinical outcomes between the two series (p > 0.05, Two Proportions test, Minitab 13, Minitab Inc., State College, PA).
Table 1.
Combined microdiscectomy outcomes at 1-year post-op
| MSU Classification | Excellent/good | Fair | Poor | Total |
|---|---|---|---|---|
| 2-A | 9 | 0 | 0 | 9 |
| 2-AB | 52 | 4 | 0 | 56 |
| 2-B | 66 | 4 | 0 | 70 |
| 2-C | 3 | 3 | 0 | 6 |
| 3-A | 13 | 0 | 0 | 13 |
| 3-AB | 10 | 0 | 0 | 10 |
| 3-B | 15 | 2 | 0 | 17 |
| Total | 168 | 13 | 0 | 181 |
Table 2.
Combined microdiscectomy outcomes at 5-year post-op
| MSU Classification | Excellent/good | Fair | Poor | Total |
|---|---|---|---|---|
| 2-A | 8 | 1 | 0 | 9 |
| 2-AB | 46 | 8 | 2 | 56 |
| 2-B | 60 | 6 | 4 | 70 |
| 2-C | 3 | 3 | 0 | 6 |
| 3-A | 10 | 1 | 2 | 13 |
| 3-AB | 8 | 1 | 1 | 10 |
| 3-B | 13 | 4 | 0 | 17 |
| Total | 148 | 24 | 9 | 181 |
Fig. 4.
Outcomes of discectomy at 1-year follow-up (a) and 5-year follow-up (b). *Poor outcomes at 5-year follow-up resulted from recurrent herniations sustained between 1 and 5 years post-op
On overall analysis, most post-operative scores were either GOOD or EXCELLENT. The range of findings among these patients at 1 and 5 years after surgery may be summarized as little or no pain, ability to lift heavy weights with little or no pain, ability to walk long distances with little or no limitation, ability to sit as long as they liked with little or no pain, ability to stand up as long as they liked with little or no pain, ability to sleep without being disturbed ever or disturbed just occasionally by pain, a normal sex life, a normal active social life including their favorite sports with little or no pain, and the ability to travel anywhere with little or no pain.
The rest of the patients, excluding those 5% overall who suffered recurrent herniations, were scored as FAIR outcomes. The range of findings among these patients may be summarized as little or moderate back pain, pain when trying to lift heavy weights, inability to walk more than 2 km, inability to sit for more than an hour, inability to sleep more than 6 h at a time, a normal sex life despite occasional pain, inability to pursue more active sports, and inability to sit and travel for more than an hour at a time. It is important to note on follow-up that none of the patients initially reported being made worse by their surgery.
Discussion
The MSU Classification has been shown to be a viable method of measurement that has been coupled to our normal selection criteria for lumbar microdiscectomy at our institution. It arose out of a need to help define, for surgeons and resident surgeons alike, what, in our opinion, constituted a “substantial” lumbar disc herniation on MRI. The first series of 100 patients was used to help develop the classification, and the second series to validate it. There was no difference between the various outcomes in series 1 and series 2, which allowed us to combine the two series in reporting our overall results in 181 patients.
Our reported surgical success rate of or above 90% at 1 year compares favorably with the highest outcomes reported in the literature, and it exceeds the more commonly accepted norms of 75–80% [1]. Some clinical researchers have tried to base outcome differences on whether the herniation was either fragmented or contained within a competent annulus [4]. Others [5, 11, 12], as well as the authors of this study, have examined the relationship between larger size and more constrained location in relationship to clinical symptoms and surgical outcomes. In our experience, the success of lumbar microdiscectomy appears to correlate with our selection, limiting most surgical treatment to more substantial size-2 and size-3 disc herniations.
As opposed to other classifications, which either rely on a great deal of subjectivity or tend to be too complex and cumbersome, the MSU Classification offers a simple, objective method of MRI measurement that seems easy to reproduce with consistency by different examiners. Widespread use of this classification by virtue, first of all, of its ability to objectify “substantial” herniation, and then, secondly, by its ability to convey that information efficiently, could help standardize the way we describe, select, and compare outcomes of surgical patients who undergo treatment for acute lumbar disc herniation. The regular application of such a standard classification among surgeons, radiologists, and researchers might lend itself to a better overall understanding of herniated disc, and suggest specific trends in treatment that might clarify the indications for surgery, and improve overall surgical outcomes across the regions and among institutions [19, 20].
It should be clarified that this classification might be limited to cases where facet margins appear clean and well demarcated on MRI. The moment the margins of the facet begin to appear distorted in any way by osteophyte formation and/or ligamentum flavum hypertrophy, the proposed criteria may no longer be valid. In that instance, canal compromise is based not only on herniated disc, but also on other elements of disc, facet, and ligament degeneration, which are all representative of spinal stenosis.
It is readily acknowledged that no surgery was performed for any size-1 disc herniation in our study. We do not view this necessarily as a shortcoming. The objective of this study was minimally to develop a scheme to quantify “substantial” lesions, selection of which will yield good to excellent surgical outcomes. Size-1 herniations would typically seem to exert minimal impact on nerves; and physical symptoms, in that case, are more likely related to chemical neuritis or nerve root adhesions [14]. Furthermore, annulotomy performed on a protruding disc can be construed as an insult that often leads to more substantial pathology later on. Annulotomy on an intact annulus has been shown experimentally to begin the cascade of disc degeneration [13]. Clinically, surgical annulotomy has been fraught with much higher rates of recurrence afterward [4].
The use of the intra-facet line as a reference, from which to evaluate size, was based on retrospective analysis of 100 MRIs of consecutive patients who had undergone surgery for only substantial, moderately severe to severe, herniated disc. Using the MSU criteria to qualify “substantial”, it is possible for surgeons to electively limit their surgery to size-2 and size-3 lesions in an effort to yield, what our study suggests, may be a higher proportion of GOOD to EXCELLENT outcomes. The numbers of more constrained 2-B and 2-AB lesions, seen in our series, appear to be the types of disc herniation most frequently requiring surgery, while many 2-A lesions, centered more in the middle of the spinal canal, can sometimes prove to be less symptomatic, and quite suited to conservative treatment efforts. The complimentary roles of surgery and conservative treatment for lumbar disc herniation might be better reconciled in reference to such an objective basis. Additional studies dealing with the effects of surgery on size-1 herniations, particularly the 1-AB which could be prone to exert more pressure in the region of the enlarged dorsal root ganglion, would prove to be of further value. And although lumbar microdiscectomy remains an elective operation, except when it is mandatory for the treatment of impending cauda equina syndrome or unrelenting sciatica, it becomes a more viable and attractive alternative for patients and their referring physicians choosing to undergo elective surgery on the basis of more objective MRI guidelines.
The MSU Classification appears not only useful to assist in patient surgical selection, but also to better qualify records, to standardize radiologic description, and to more thoughtfully correlate future research outcome studies. Perhaps, most importantly, as part of any selection process, it may be pragmatic in helping provide a more consistent approach to the treatment of herniated disc, and yield a higher incidence of excellent surgical outcomes for patients in the future.
References
- 1.Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, Clabeaux DE, Hyland AH. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96:34–44. doi: 10.3171/spi.2002.96.1.0034. [DOI] [PubMed] [Google Scholar]
- 2.Atlas SJ, Deyo RA, Patrick DL, Convery K, Keller RB, Singer DE. The Quebec Task Force classification for spinal disorders and the severity, treatment, and outcomes of sciatica and lumbar spinal stenosis. Spine. 1996;21:2885–2892. doi: 10.1097/00007632-199612150-00020. [DOI] [PubMed] [Google Scholar]
- 3.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403–408. [PubMed] [Google Scholar]
- 4.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am A. 2003;85:102–108. [PubMed] [Google Scholar]
- 5.Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine. 1997;22:1650–1660. doi: 10.1097/00007632-199707150-00025. [DOI] [PubMed] [Google Scholar]
- 6.Delamarter RB, McCulloch JA. Microdiscectomy and microsurgical spinal laminotomies. In: Frymoyer JW, editor. The adult spine: principle and practice. 2. Philadelphia: Lippincott-Raven; 1997. pp. 1961–1989. [Google Scholar]
- 7.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 8.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 9.Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 10.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 11.Karppinen J, Malmivaara A, Tervonen O, Paakko E, Kurunlahti M, Syrjala P, Vasari P, Vanharanta H. Severity of symptoms and signs in relation to magnetic resonance imaging findings among sciatic patients. Spine. 2001;26:E149–E154. doi: 10.1097/00007632-200104010-00015. [DOI] [PubMed] [Google Scholar]
- 12.Kortelainen P, Puranen J, Koivisto E, Lahde S. Symptoms and signs of sciatica and their relation to the localization of the lumbar disc herniation. Spine. 1985;10:88–92. doi: 10.1097/00007632-198501000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Lotz JC. Animal models of intervertebral disc degeneration: lessons learned. Spine. 2004;29:2742–2750. doi: 10.1097/01.brs.0000146498.04628.f9. [DOI] [PubMed] [Google Scholar]
- 14.Marshall LL, Trethewie ER, Curtain CC. Chemical radiculitis. A clinical, physiological and immunological study. Clin Orthop Relat Res. 1977;129:61–67. [PubMed] [Google Scholar]
- 15.Mysliwiec L (1999) Keyhole lumbar microdiscectomy for substantial lumbar disc herniation: outcome study of one hundred consecutive cases with average five year follow-up. In: Proceedings of the 14th annual meeting of the North American Spine Society (NASS). Chicago
- 16.Ohnmeiss DD, Vanharanta H, Ekholm J. Degree of disc disruption and lower extremity pain. Spine. 1997;22:1600–1605. doi: 10.1097/00007632-199707150-00015. [DOI] [PubMed] [Google Scholar]
- 17.Takada E, Takahashi M, Shimada K. Natural history of lumbar disc hernia with radicular leg pain: spontaneous MRI changes of the herniated mass and correlation with clinical outcome. J Orthop Surg (Hong Kong) 2001;9:1–7. doi: 10.1177/230949900100900102. [DOI] [PubMed] [Google Scholar]
- 18.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131–140. doi: 10.1097/00007632-198303000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Weinstein JN, Bronner KK, Morgan TS, Wennberg JE (2004) Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood) Suppl Web Exclusives: VAR81-89 [DOI] [PubMed]
- 20.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–2450. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wiltse LL, Berger PE, McCulloch JA. A system for reporting the size and location of lesions in the spine. Spine. 1997;22:1534–1537. doi: 10.1097/00007632-199707010-00023. [DOI] [PubMed] [Google Scholar]