Abstract
The objective of this study was to develop an evidence-based airway management protocol for patients with acute tetraplegia. The method consisted of an analysis of the medical records of patients (September 1997–December 2002) with a spinal cord injury and a neurological deficit less than 8 weeks old. Of the 175 patients, 72 (41, 14%) were tracheotomised. This was influenced by the origin of the paralysis, Frankel score, and number of cervical spine operations, accompanying injuries and accompanying illnesses. Tracheotomy did not affect the duration of treatment, duration of ventilation or length of stay in the intensive care unit. The need for a tracheotomy was able to be predicted in 73.31% with neurological level, Frankel score and severity of accompanying injuries. In patients with acute tetraplegia, primary tracheotomy is indicated in sub C1–C3 with Frankel stage A/B, sub C4–C6 with Frankel stage A/B with trauma and accompanying injuries/accompanying illnesses, and in patients with complex cervical spine trauma that requires a combined surgical approach. In other patients, an attempt at extubation should be made.
Keywords: Tracheotomy, Tetraplegia, Complications, Intubation
Introduction
Due to the permanent impairment of physiological breathing (the severity of which may vary) as a result of injury, patients with tetraplegia represent a particular challenge. In most cases, early intubation is carried out at the accident site. The necessity of additional measures, such as tracheotomy or extubation, during subsequent clinical treatment is the subject of frequent dispute. There is a diversity of opinion on the necessity, correct time point and methods for carrying out tracheotomy. The proposed time ranges from 3 days to 3 weeks [1, 2].
Advocates of early tracheotomy cite a reduction in the length of hospital stay and stay in the intensive care unit, and a reduction in the number of days for which patients are ventilated, with resultant cost savings [3]. Other authors consider that early tracheotomy reduces the duration of the weaning process and increases the patient’s ventilation tolerance. But it also increases the period for which the patient is ventilated and the length of stay in the intensive care unit [4].
Since tracheotomy is not without risks, the optimum time point for tracheotomy and the risks associated with this intervention must be weighed against an extended period of endotracheal intubation [5]. Fromm et al. [6] proposed performing extubation with a short weaning period and only carrying out a tracheotomy when this procedure proved unsuccessful after one or two attempts. Reintubation following failed extubation is, however, according to Epstein [7], associated with increased mortality, increased tracheotomy rate, increased length of hospital stay and consequently increased costs.
The objective of this retrospective study was to draw up a set of airway management guidelines for patients with acute tetraplegia based on treatment data from a centre for spinal cord injuries.
Materials and methods
A retrospective study was carried out by examining the medical records of all patients admitted to the Spinal Cord Injuries Unit at the Unfallkrankenhaus in Berlin between 1 September 1997 and 31 December 2002 following an injury between the craniocervical junction and the first thoracic vertebra. All patients who had sustained this spinal cord injury within the previous 8 weeks and who had undergone continuous inpatient treatment since the injury were included in the study.
The level of the lesion was determined using the American Spinal Injury Association Grading Scale (ASIA). Functional severity was determined internationally using the Frankel scale [8]. On admission, patients were examined by a doctor from the treatment centre for spinal cord injuries. Up to five accompanying injuries and accompanying illnesses were recorded with the severity of the accompanying injuries being classified according to respiration restriction (see Table 1).
Table 1.
Weighting of the severity of accompanying injuries
| Severity | Accompanying injuries | Number |
|---|---|---|
| 0 | None | 103 (58.86%) |
| I | Craniofacial injury, brain injury I°–II° | 19 (10.86%) |
| II | Injuries to the extremities, thoracic vertebral fracture, abdominal trauma | 21 (12.00%) |
| III | Lung contusion, fractured ribs, haemo/pneumothorax, brain injury III° | 24 (13.71%) |
Weighting of accompanying injuries was according to the degree of restriction of pulmonary function (n = 175)
All patients whose paralysis was found to be caused by a constriction of the vertebral canal underwent immediate surgery. Patients were admitted to the intensive care unit for stabilisation of their vital signs or for monitoring following surgery or transfer from another institution. A tracheotomy was considered to be clinically indicated if a ventilation period of more than 10 days was required, the weaning phase was expected to last for more than 72 h and the patient was not able adequately to mobilise secretions [9]. The cannula was removed when the patient no longer required endotracheal suction and had no pulmonary infection within the previous 4 weeks or indication of aspiration.
The data collected was encoded and absolute and relative frequency distributions analysed. Statistical analysis was carried out using SPSS 11.0 (Statistical Package for the Social Sciences). Frequency, means and standard deviations were determined. Correlations within the data were tested in a cross tabulation using the χ2 test at a significance level of P < 0.05. Comparison between groups was carried out using the nonparametric Kruskal–Wallis H test. The null hypothesis (that there is equality between the groups) was rejected if the calculated test statistics was greater than or equal to the χ2 value for the degrees of freedom and the significance level was 5%. Discriminant analysis was used to determine which factors had influenced the need for tracheotomy. The percentage value of the exact analysis was entered.
Results
A total of 185 patients were treated between 1 September 1997 and 31 December 2002; 175 patients for whom complete data were available were included in the analysis.
Patients
Of the 175 patients, 144 (82.29%) were male and 31 (17.71%) female. The age ranged from 14 to 89, with a mean of 43.45 ± 18.98. Men were affected more frequently than women (4.6:1), with similar age profiles for both sexes. As much as 147 patients (84%) suffered paralysis as a result of trauma; 73 (41.71%) patients had a fracture of the vertebral body; 47 (26.86%) had two fractured vertebrae and 16 (9.14%) had fractures of more than two cervical vertebrae. Of the 28 (16%) patients who had not suffered trauma, 15 (8.57%) had a paralysis as a sequela of spondylodiscitis (see Table 2).
Table 2.
Frankel Score, number and frequency (n = 175)
| Frankel | Number |
|---|---|
| A | 103 (58.86%) |
| B | 19 (10.86%) |
| C | 21 (12.00%) |
| D | 24 (13.71%) |
| E | 8 (4.57%) |
Of the 147 patients with traumatic cervical injuries, 70 (47.6%) had accompanying injuries; 31 (21.1%) patients had one, 12 (8.2%) had two, 9 (6.1%) had three, 7 (4.8%) had four and 11 (7.5%) had five accompanying injuries. A total of 70 (40%) patients were suffering from one or more existing disorders on admission (see Table 3).
Table 3.
Accompanying injuries and diseases, number and frequency (injuries n = 70; diseases n = 70)
| Accompanying Injuries | Number | Accompanying diseases | Number |
|---|---|---|---|
| Lung contusion on one side | 23 (35.38%) | Hypertonia | 21 (17.36%) |
| Lung contusion on both sides | 17 (26.15%) | Coronary heart disease | 14 (11.57%) |
| Thoracic vertebrae fracture | 17 (26.15%) | Diabetes | 14 (11.57%) |
| Haemo/pneumothorax | 16 (24.6%) | Ankylosing spondylitis | 10 (8.26%) |
| Fracture of upper extremities | 14 (21.5%) | Depression | 8 (6.61%) |
| Brain injuriy I° | 14 (21.5%) | Alcohol abuse | 8 (6.61%) |
| Fractured ribs > 2 ribs | 13 (20%) | Tumour | 6 (4.96%) |
| Brain Injury III° | 13 (20%) | Smoking | 6 (4.96%) |
| Fractured lower extremities | 13 (20%) | COPD | 5 (4.13%) |
| Blunt abdominal trauma | 7 (10.7%) | Hypothyroidism | 3 (2.48%) |
| Craniofacial injuries | 6 (9.2%) | Asthma | 1 (0.83%) |
| Brain Injury II° | 3 (4.6%) | Parkinson’s disease | 1 (0.83%) |
| Hypoxia | 2 (3.07%) | Syphilis | 1 (0.83%) |
| Stroke | 1 (0.83%) |
Operative treatment
A total of 163 (93.14%) patients were initially treated surgically, in 134 (80.24%) cases via a ventral approach, in 22 (13.17%) via a dorsal approach and in 7 (4.19%) via a combined dorsoventral approach. A total of 49 (30%) patients required a second operation. In 35 (71.42%) patients, a second step of the operative treatment due to continuing instability following initial decompression was performed.
Intensive treatment
A total of 123 (70.85%) patients were treated in the intensive care unit during their admission. The duration of intensive treatment averaged 17.81 ± 24.05 days. As much as 89 patients (50.86%) had a single episode of intensive treatment for an average of 11.3 days, with 29 patients (16.57%) undergoing two episodes of intensive treatment for a mean of 32.63 days as a result of complications. The duration of intensive treatment correlated with the duration of ventilation (χ2 = 120.83, P < 0.05) and tracheotomy (χ2 = 90.57, P < 0.05) and was dependent on the Frankel score (H test 16.23, P = 0.022). In patients whose paralysis had a non-traumatic origin, there was also a correlation between the number of accompanying illnesses (χ2 = 90.63, P < 0.05) and the neurological level (χ2 = 100.03, P < 0.05).
Intubation and mechanical ventilation
Of the 123 patients, 113 (91.85%) treated on the intensive care unit were intubated and mechanically ventilated for 15.78 ± 26.92 days. The need to intubate correlated with the origin of the paralysis (χ2 = 47.79, P < 0.05), the number of accompanying injuries (χ2 = 12.42, P < 0.05), the classification of the accompanying injuries (χ2 = 8.05, P < 0.05), thoracic injuries (χ2 = 6.66, P < 0.05) and the Frankel score (χ2 = 24.78, P < 0.05). The duration of ventilation correlated with thoracic injuries (χ2 = 15.60, P < 0.05), tracheotomy (χ2 = 48.25, P < 0.05) and Frankel score (H test = 22.92, P < 0.001).
An attempt was made at extubation in 67 patients after a mean of 4.74 ± 9.18 days; 45 of the extubated patients (67.2%, n = 67) suffered complications, primarily pulmonary in nature. Thoracic trauma influenced the occurrence of complications (χ2 = 17.05; P < 0.05). A second intubation was required in 33 of the extubated patients (49.25%) after a mean of 3.26 ± 6.46 days. The Frankel score was a relevant factor for reintubation (χ2 = 9.695; P < 0.05).
Tracheotomy
Of the 113 patients with an intubation, 72 (81.36%) were tracheotomised and 34 (30.08%) underwent a primary tracheotomy without an attempt at extubation.
Influencing factors for tracheotomy
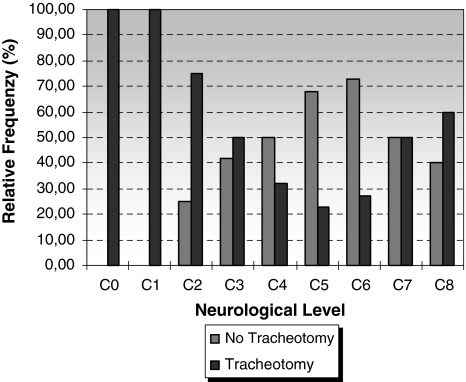
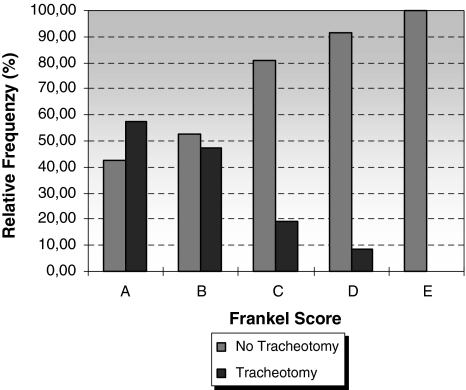
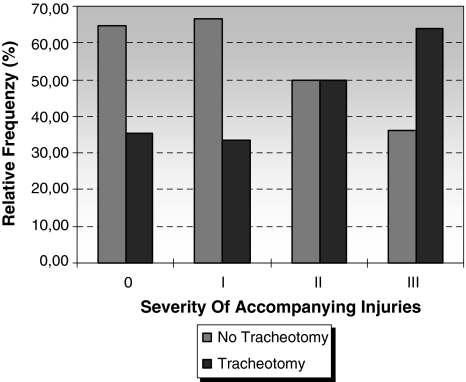
The origin of the paralysis influenced the necessity for tracheotomy (χ2 = 18.42; P < 0.05). Patients with fractured cervical vertebrae and inflammation required tracheotomy more frequently. In the patient population as a whole, the neurological level had no effect on the need for tracheotomy (χ2 = 13.31; P > 0.05) (see Fig. 1). If the patient group was subdivided according to the origin of paralysis, the neurological level did influence the need for tracheotomy in the group with traumatic lesions (χ2 = 17.58; P < 0.05). The need for tracheotomy declined with falling sensorimotor deficit (χ2 = 31.53; P < 0.05) (see Fig. 2). The number of accompanying injuries correlated with the need for tracheotomy (χ2 = 11.78; P < 0.05) (see Fig. 3). In the patient population as a whole, the number of cervical spine operations performed correlated with the need for tracheotomy (χ2 = 6.86; P < 0.05). This was also the case for patients whose condition was of non-traumatic origin (χ2 = 4.86, P < 0.05), but had no influence on patients whose condition was of traumatic origin (χ2 = 4.86, P < 0.05).
Fig. 1.
Neurological level and tracheotomy. The relative frequency of tracheotomy for different neurological levels (n = 175)
Fig. 2.
Frankel score and tracheotomy. The relative frequency of tracheotomy for different Frankel scores (n = 175)
Fig. 3.
Severity of accompanying injuries in tracheotomy. The relative frequency of tracheotomy for different levels of weighting of accompanying injuries according to the degree of restriction of pulmonary function (n = 175)
Predictors for tracheotomy
Discriminant analysis showed that traumatic origin with a combination of neurological level, Frankel score and the severity of accompanying injuries gave a prediction probability of 73.31%. For non-traumatic origin, the prediction probability with neurological level and number of cervical spine operations attained 86.21% (see Table 4).
Table 4.
Prediction of tracheotomy
| Clinical parameter | Trauma (%) | Non-trauma | All |
|---|---|---|---|
| Age | 57.53 | 58.97 | 58.86 |
| Number of cervical spine operations | 52.05 | 79.31 | 56.57 |
| Neurological level | 62.33 | 44.83 | 61.16 |
| Classification of accompanying injuries | 63.70 | – | 61.16 |
| Frankel score | 64.38 | 79.31 | 66.29 |
| Thoracic injuries | 64.38 | – | 64.00 |
| Frankel score, classification of accompanying injuries | 64.38 | – | 66.29 |
| Frankel score, thoracic injuries | 65.38 | – | 66.86 |
| Neurological level, Frankel score | 63.01 | 79.31 | 64.57 |
| Neurological level, number of cervical spine operations | 64.38 | 86.21 | |
| Neurological level, Frankel score, severity of accompanying injuries | 73.29 | – | 73.31 |
Clinical parameters and combinations of clinical parameters, which allow prediction of tracheotomy. A distinction was drawn between traumatic and non-traumatic lesions
Outcome
The average length of hospital stay was 170 ± 138.35 days. No statistically significant correlations with the length of hospital stay were found. Tracheotomy was closed in average after 70.71 ± 72.6 days. The duration of tracheotomy until closure of the stoma did not correlate with any of the parameters examined. On discharge, 144 (82.29%) had no tracheotomy, 4 (2.29%) had a tracheotomy, but were not mechanically ventilated, and 7 (4.00%) had a tracheotomy and were mechanically ventilated.
A total of 20 (11.43%) patients died during their hospital stay; 14 (70%) of the deceased patients were tracheotomised during their stay. Age (χ2 = 58.41, P < 0.05), the need for a tracheotomy (χ2 = 7.11, P < 0.05) and the number of accompanying illnesses (χ2 = 33.26, P < 0.05) all influenced mortality. Younger patients generally died as a result of massive trauma, with patients over 60 years generally suffering from a larger number of accompanying illnesses.
Discussion
This study examined the retrospective clinical parameters, which might be relevant to the necessity for tracheotomy. The neurological level, severity of paralysis, number of cervical spine operations required, origin of paralysis, the number of accompanying injuries, the severity of accompanying injuries and the number of accompanying illnesses were found to have a statistically significant effect on tracheotomy. For description of further correlations, the patients were subdivided according to the origin of their paralysis. In patients with traumatic paralysis, accompanying injuries and in particular thoracic injuries and pre-existing accompanying illnesses influence tracheotomy. In patients with non-traumatic injuries, the number of cervical spine operations required, as an expression of the extent of traumatic damage, had an influence.
The significance of accompanying illnesses and injuries has not been considered in previous studies. The main focus of previous discussion has been on the consequences of paralysis on the mechanics of breathing [10–13]. This is indeed a very serious issue, something which is reflected in our results in the influence of neurological level and severity of paralysis. It was found, however, that the number and severity of accompanying injuries and accompanying illnesses have a profound effect on airway management. In contrast to previous studies, early tracheotomy was not found to influence the length of hospital stay, stay in the intensive care unit or duration of ventilation in either direction. This has already been shown in a meta-analysis, which investigated the significance of the time point at which tracheotomy was performed [14].
In our study, reintubation following a failed attempt at extubation did not demonstrably disadvantage the patients or their treatment. Similarly, no tracheotomy-related complications were observed. Based on these considerations, we have formulated the following proposals for airway management in patients with acute tetraplegia:
Patients sub C1–C3 with a Frankel score A or B should be tracheotomised immediately.
- Patients sub C4–C6 and Frankel A or B should be tracheotomised at an early stage if
- the cause was traumatic and there were accompanying injuries/accompanying illnesses and/or
- there was a complex cervical spine trauma requiring a combined operative procedure and/or
- ventilation for more than 10 days was required.
- An attempt at extubation should be made in patients with
- trauma and Frankel C, D, E,
- injuries sub C7–C8.
Following a failed attempt at extubation, early tracheotomy should be carried out depending on the severity of paralysis and the presence of thoracic trauma.
Airway management in patients with tetraplegia is of critical importance to the patient. As much as 50% of patients with a complete lesion of the cervical or thoracic spinal cord develop atelectasis or pneumonia within 30 days of the injury, with the peak incidence at 3–5 days [15]. A tracheotomy for pulmonary support, weaning or to protect the airway was necessary in 69–77% of patients with complete tetraplegia (Frankel score A) during their hospital stay [16]. Kane et al. [17] describe a significant increase in pneumonia risk with duration of intubation and recommend tracheotomy within 2 days. They consider that early tracheotomy in trauma patients is advantageous, but appreciate the difficulty in deciding whether prolonged intubation will be necessary for a particular patient. Rodriguez states that early tracheotomy reduces the length of hospital stay and stay in the intensive care unit and reduces the number of days for which patients are ventilated, resulting in cost saving [3]. Other authors postulate that patients who require controlled long-term ventilation for more than 36 h should be tracheotomised within a period of 36 h, or earlier when it is apparent within the first 24 h that the patient will require intubation for several days [18]. Various authors consider that early tracheotomy reduces the duration of the weaning process and increases the patient’s ventilation tolerance. But it also increases the period for which the patient is ventilated and the length of stay in the intensive treatment unit [4].
There is relative unanimity in that the incidence of pulmonary infections reduces significantly following tracheotomy and that the rate of pulmonary infections increases with the duration of endotracheal intubation [11]. No data that assesses prospectively which of the patients require a tracheotomy are available. Fromm et al. [6] proposed performing extubation with a short weaning period and only carrying out a tracheotomy if this procedure proved unsuccessful after one or two attempts. Reintubation following failed extubation is, however, according to Epstein associated with increased mortality, increased tracheotomy rate, increased length of hospital stay and thus higher costs [7]. Klockgether-Radke [18] summarise that the decision to tracheotomise patients receiving long-term ventilation is based more on experience than on specific data, and that meta-analysis has failed to show that patients undergoing early tracheotomy are easier to wean from mechanical ventilation.
This study is a retrospective study and therefore has methodological limitations. The study results do not allow predictions of prognoses. We have merely described correlations between individual variables. Data were collected from a single centre only. To produce more meaningful results, data from multiple centres would need to be collected.
It would appear difficult to find methods of improving the treatment options of patients with tetraplegia and accompanying injuries, as it is not possible to exert influence on accompanying injuries and illnesses. One possibility may be to improve the mechanics of breathing to prevent complications such as pneumonia and reduce the duration of ventilation. Another approach may be a supportive electrical stimulation of the abdominal musculature during the weaning and post-extubation phase [19].
References
- 1.Dunham CM, LaMonica C. Prolonged tracheal intubation in the trauma patient. J Trauma. 1984;24:120–124. doi: 10.1097/00005373-198402000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation and tracheotomy. A prospective study of 150 critically ill adult patients. Am J Med. 1981;70:65–76. doi: 10.1016/0002-9343(81)90413-7. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM. Early tracheostomy for primary airway management in the surgical critical care setting. Surgery. 1990;108:655–659. [PubMed] [Google Scholar]
- 4.Berney S, Stockton K, Berlowitz D, Denehy L. Can early extubation and intensive physiotherapy decrease length of stay of acute quadriplegic patients in intensive care? A retrospective case control study. Physiother Res Int. 2002;7:14–22. doi: 10.1002/pri.237. [DOI] [PubMed] [Google Scholar]
- 5.Quintel M, Roth H. Tracheostomy in the critically ill: clinical impact of new procedures. Intensive Care Med. 1999;25:326–328. doi: 10.1007/s001340050845. [DOI] [PubMed] [Google Scholar]
- 6.Fromm B, Hundt G, Gerner HJ, Baer GA, Exner G, Botel U, Naumann CP, Baumberger ME, Zach G. Management of respiratory problems unique to high tetraplegia. Spinal Cord. 1999;37:239–244. doi: 10.1038/sj.sc.3100759. [DOI] [PubMed] [Google Scholar]
- 7.Epstein SK. Extubation failure: an outcome to be avoided. Crit Care. 2004;8:310–312. doi: 10.1186/cc2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 9.Plummer AL, Gracey DR. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest. 1989;96:178–180. doi: 10.1378/chest.96.1.178. [DOI] [PubMed] [Google Scholar]
- 10.O’Keeffe T, Goldman RK, Mayberry JC, Rehm CG, Hart RA. Tracheostomy after anterior cervical spine fixation. J Trauma. 2004;57:855–860. doi: 10.1097/01.TA.0000083006.48501.B2. [DOI] [PubMed] [Google Scholar]
- 11.Lemons VR, Wagner FCJ. Respiratory complications after cervical spinal cord injury. Spine. 1994;19:2315–2320. doi: 10.1097/00007632-199410150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Como JJ, Sutton ERH, McCunn M, Dutton RP, Johnson SB, Aarabi B, Scalea TM. Characterizing the need for mechanical ventilation following cervical spinal cord injury with neurologic deficit. J Trauma. 2005;59:912–916. doi: 10.1097/01.ta.0000187660.03742.a6. [DOI] [PubMed] [Google Scholar]
- 13.Hassid VJ, Schinco MA, Tepas JJ, Griffen MM, Murphy TL, Frykberg ER, Kerwin AJ. Definitive establishment of airway control is critical for optimal outcome in lower cervical spinal cord injury. J Trauma. 2008;65:1328–1332. doi: 10.1097/TA.0b013e31818d07e4. [DOI] [PubMed] [Google Scholar]
- 14.Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330:1243. doi: 10.1136/bmj.38467.485671.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fishburn MJ, Marino RJ, Ditunno JFJ. Atelectasis and pneumonia in acute spinal cord injury. Arch Phys Med Rehabil. 1990;71:197–200. [PubMed] [Google Scholar]
- 16.Harrop JS, Sharan AD, Scheid EHJ, Vaccaro AR, Przybylski GJ. Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg. 2004;100:20–23. doi: 10.3171/spi.2004.100.1.0020. [DOI] [PubMed] [Google Scholar]
- 17.Kane TD, Rodriguez JL, Luchette FA. Early versus late tracheostomy in the trauma patient. Respir Care Clin N Am. 1997;3:1–20. [PubMed] [Google Scholar]
- 18.Klockgether-Radke AP, Neumann P, Quintel M. Tracheotomie—Luftweg der Wahl fur den langzeitbeatmeten Patienten? Anasthesiol Intensivmed Notfallmed Schmerzther. 2004;39:335–343. doi: 10.1055/s-2004-814311. [DOI] [PubMed] [Google Scholar]
- 19.Gollee H, Hunt KJ, Allan DB, Fraser MH, McLean AN (2008) Automatic electrical stimulation of abdominal wall muscles increases tidal volume and cough peak flow in tetraplegia. Technol Health Care 16(4):273–281 [PubMed]