Abstract
Central venous catheterization (CVC) is a commonly performed intraoperative procedure. Traditionally, CVC placement is performed blindly using anatomic landmarks as a guide to vessel position. Real-time ultrasound provides the operator the benefit of visualizing the target vein and the surrounding anatomic structures prior to and during the catheter insertion, thereby minimizing complications and increasing speed of placement. A 22-year-old male underwent open reduction and internal fixation of acetabulum fracture in prone position. Excessive continuous bleeding intraoperatively warranted placement of CVC in right internal jugular vein (IJV), which was not possible in prone position without the help of ultrasound. Best view of right IJV was obtained and CVC was placed using real-time ultrasound without complications. Ultrasound-guided CVC placement can be done in atypical patient positions where traditional anatomic landmark technique has no role. Use of ultrasound not only increases the speed of placement but also reduces complications known with the traditional blind technique.
Keywords: Ultrasound, central venous catheterization, prone position, internal jugular vein
INTRODUCTION
Central venous catheterization (CVC) for central venous access is an essential part of clinical management in many patients intraoperatively. The complications associated with attempted CVC insertion are many and include carotid artery puncture, pneumothorax and hemothorax, nerve and thoracic duct injuries. Complication rates as high as 15% have been reported. [1]The complications are more in the presence of abnormal anatomy, coagulopathy, emergency clinical settings, abnormal patient position (which distorts anatomy) and inexperience of the clinician inserting CVC. Since the first report of combined real-time visual ultrasonographic imaging for internal jugular catheter placement by Yonei in 1986,[2] there has been mounting evidence and studies demonstrating benefits of ultrasound for CVC placement including rapid vein localization, a reduction in needle attempts and fewer complications.[3,4]We present a case of internal jugular vein (IJV) catheterization in prone position using ultrasound. The objective of this report is to describe the use of ultrasonography for placement of a central venous catheter in prone position where conventional line placement is technically challenging.
CASE REPORT
A 22-year-old male was involved in a road traffic accident, scheduled for fixation of acetabulum fracture under general anesthesia. The patient had no previous history of any medical illness. He was hemodynamically stable with blood pressure 123/82 mmHg, heart rate 76 bpm and O2 sat 98% on room air. Laboratory results: Hb, Na +, K +, creatinine and BUN were in normal range. Chest X-ray showed no pneumothorax and X-ray pelvis revealed the head of femur impacted in the pelvis, and the decision was made to operate the patient in prone position. As a part of the anesthesia plan, patient received general anesthesia with two large bore peripheral lines and an arterial line. CVC was not in the anesthesia plan. However, due to significant and continuous bleeding, it was decided to insert central venous access through right IJV under ultrasound guidance in prone position. After sterile preparation, the lateral aspect of the neck was scanned in prone position [Figure 1 and 2] with GE ultrasound machine (Logiq e, General Electric Healthcare, Pewaukee, WI) using a linear 12 MHz probe. Under direct visualization the needle was inserted through the lateral wall of the IJV, which was cannulated successfully.
Figure 1.
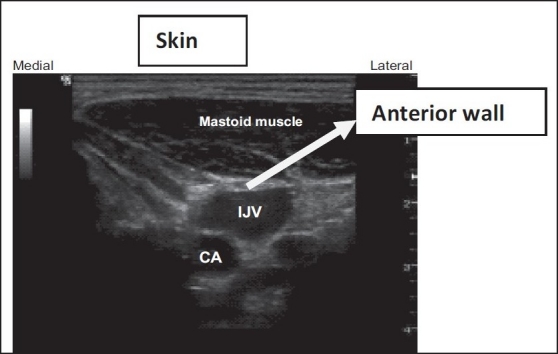
Patient is in supine position and IJV is anterio-lateral to the carotid
Figure 2.
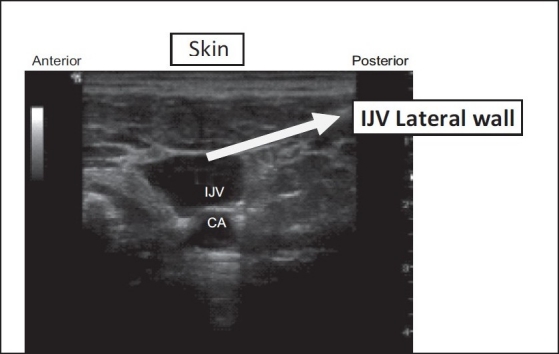
Patient is in prone position and the IJV is above the carotid artery
The difference between the supine and the prone position is that IJV will be seen superficial to the carotid artery when scanning the lateral aspect of the neck in prone position and the needle will enter the lateral wall of IJV, instead of the anterior wall as is seen in supine position.
DISCUSSION
More than 5 million central venous catheters are placed each year in the United States with an associated complication rate of >15%.[1] The risk of complications depends on several factors, including (but not limited to) operator experience, urgency of placement, as well as patient factors such as obesity, prior difficult cannulation and coagulopathy.[5] Use of real-time two-dimensional ultrasound guidance for IJV cannulation in adults has been associated with a reduction in complication rate and a significantly lower failure rate both overall and on the first attempt.[4,6] The Agency for Healthcare Quality Research has recommended that Ultrasound Guidance be used for central line placement due to an improved margin of patient safety.[7] Some authors suggest using ultrasound-guided vascular access in all central line attempts, and recommend that it should become the standard of practice for central line placement.[3,8] Similarly, in September 2002, the National Institute of Clinical Excellence (NICE) issued Guidelines for England and Wales suggesting that ultrasound guidance should be used for all electives, and should be considered for most emergency CVC.[9] The use of ultrasound besides improving safety has resource and training implications. To gain the skills required to incorporate ultrasound in clinical practice, the non-radiologist needs training in image acquisition and interpretation, which can be achieved through didactic lectures and demonstrations by a skilled sonographer. Didactics should include lectures on the basic physics and principles of ultrasound, ′knobology′ (how to actually operate the ultrasound machine), image acquisition, identification and interpretation of ultrasound artifacts, identification of the relevant anatomy and knowledge of anatomic variation.[10]The laboratory training should include exposure to a variety of ultrasound machines, examination of normal vascular anatomy of healthy volunteers as well as hands-on simulation with vascular access models.
All approaches described for IJV cannulation; central, anterior and posterior are performed blindly, guided only by anatomic landmarks and do not consider anatomic variation or abnormality.[11] Any standard 2D ultrasound machine with a mid-high frequency (7.7–12 MHz) linear array flat probe can be used for central venous cannulation with ultrasound. It is possible for a single user to operate the ultrasound and perform vascular access simultaneously. The use of ultrasound becomes more important in situations with abnormal anatomy, like IJV being medial to the carotid artery or posterior to the artery, and in anticoagulated patients and helps in eliminating the chances of carotid artery puncture. In addition, abnormal patient position, as in our case, also distorts normal anatomy, which makes IJV cannulation impossible with landmark technique.
The differences between the appearance of IJV on the US screen in prone and supine positions are:
In supine position the IJV will be lateral to the CA and the IJV will be punctured through the anterior wall.
In prone position [Figure 2] the IJV will be superficial to the carotid artery (CA) and the IJV will be punctured through the lateral wall.
So, once the anesthetist becomes oriented with the prone position, he can visualize the tip of the needle and direct it towards the lateral wall of the IJV. This technique is also handy in case of accidental dislodgement of the CVC, which can be reinserted without turning the patient supine. However, the key to safety is that this technique should be used by those who are good in using ultrasound for CVC cannulation in supine position.
The fact that real-time ultrasound guidance for CVC placement improves success rate, reduces the number of attempts prior to successful placement and reduces the number of complications associated with catheter insertion has been proved in three meta-analyses.[5,12]
Randolph et al. included eight published trials in the meta-analysis, with six trials reporting outcomes for internal jugular, one trial reporting outcomes for subclavian and one trial describing both internal jugular and subclavian vein catheter placement. They found that compared with the landmark technique for placement of internal jugular and subclavian central venous catheters, ultrasound guidance significantly increases the probability of successful catheter placement, significantly reduces the number of complications encountered during catheter placement and significantly decreases the need for multiple catheter placement attempts.[4]
Central venous catheter placement under ultrasound guidance ensures safe and timely catheter placement and reduces many of the potential complications associated with anatomical landmark method.
To our knowledge, this is the first case report in which IJV was cannulated for central venous access in prone position with the use of ultrasound. The aim of this case report is to demonstrate the effectiveness of ultrasound technique for central venous cannulation in abnormal positions. It is our responsibility to develop training guidelines and create educational opportunities for members of our society, and incorporate ultrasound training in our fellowship programs.
However, we would like to emphasize the Anesthesia community to make use of ultrasound for CVC placement as a standard of practice rather than just a rescue technique.
Acknowledgments
Our special thanks to Dr. Mohammed El-Gammal, Chairman Department of Anesthesia, King Abdul-Aziz Medical City, King Fahad National Guard Hospital, Riyadh, for his invaluable support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123–33. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- 2.Yonei A, Nonoue T, Sari A. Real-time ultrasonic guidance for percutaneous puncture of the internal jugular vein. Anesthesiology. 1986;64:830–1. doi: 10.1097/00000542-198606000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Leung J, Duffy M, Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: A randomized, prospective study. Ann Emerg Med. 2006;48:540–7. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 4.Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: A meta-analysis of the literature. Crit Care Med. 1996;24:2053–8. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Goldfarb G, Lebrec D. Percutaneous cannulation of the internal jugular vein in patients with coagulopathies: An experience based on 1,000 attempts. Anesthesiology. 1982;56:321–3. doi: 10.1097/00000542-198204000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, et al. Ultrasonic locating devices for central venous cannulation: Meta-analysis. BMJ. 2003;327:361. doi: 10.1136/bmj.327.7411.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: A critical analysis of patient safety practices. Evid Rep Technol Assess (Summ) 2001;43:668–1. [PMC free article] [PubMed] [Google Scholar]
- 8.Scott DH. In the country of the blind, the one-eyed man is king, Erasmus (1466-1536) Br J Anaesth. 1999;82:820–1. doi: 10.1093/bja/82.6.820. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Clinical Excellence. Guidance on the use of ultrasound locating devices for placing central venous catheters. London: NICE: 2002. [NICE Technology Appraisal No 49.] [Google Scholar]
- 10.Feller-Kopman D. Ultrasound-guided internal jugular access: A proposed standardized approach and implications for training and practice. Chest. 2007;132:302–9. doi: 10.1378/chest.06-2711. [DOI] [PubMed] [Google Scholar]
- 11.Roberts JR, Hedges J. Clinical procedures in emergency medicine. 4th ed. Philadelphia, PA: Saunders; 2003. [Google Scholar]
- 12.Keenan SP. Use of ultrasound to place central lines. J Crit Care. 2002;17:126–37. doi: 10.1053/jcrc.2002.34364. [DOI] [PubMed] [Google Scholar]


