Abstract
Background
There are increasing calls for regionalization of acute myocardial infarction (AMI) care in the U.S. to hospitals with capacity to perform percutaneous coronary intervention (PCI). Whether regionalization will improve outcomes depends, in part, on the magnitude of existing differences in outcomes between PCI and non-PCI hospitals within the same healthcare market.
Methods
A 100% sample of claims from Medicare fee-for service beneficiaries age >=65 years hospitalized for AMI in 2004–2006 was used to calculate hospital-level 30-day risk-standardized mortality rates (RSMRs). RSMRs between PCI and local non-PCI hospitals were compared within hospital referral regions (HRRs) representing local healthcare markets.
Results
523,119 AMI patients were admitted to 1,382 PCI hospitals and 194,909 AMI patients were admitted to 2,491 non-PCI hospitals in 295 HRRs with at least one PCI and non-PCI hospital. While on average PCI hospitals had lower RSMRs than non-PCI hospitals (mean 16.1% v 16.9%, p<0.001), there was considerable overlap in RSMRs between non-PCI and PCI hospitals within the same HRR. In 80 HRRs, RSMRs at the best-performing PCI hospital were lower than those at local non-PCI hospitals by ≥3%. Among the remaining HRRs, RSMRs at the best-performing PCI-hospital were lower by 1.5–3.0% in 104 HRRs and by 0.01–1.5% in 74 HRRs. In 37 HRRs, RSMRs at the best-performing PCI hospital were no better or were higher than local non-PCI hospitals.
Conclusions
The magnitude of this benefit from regionalizing AMI care to PCI hospitals appears to vary greatly across HRRs. These findings support a tailored regionalization policy targeting areas with the greatest outcome differences between PCI and local non-PCI hospitals.
There is increasing support for regionalizing care of patients with acute myocardial infarction (AMI) to hospitals with the capacity to perform percutaneous coronary intervention (PCI).1, 2 Under this approach, AMI patients initially evaluated at non-PCI hospitals would be diagnosed and transferred to regional centers with high-volume specialty care and experienced PCI operators.1, 2 While clinical trials demonstrate that regionalization of ST-elevation myocardial infarction (STEMI) under certain conditions reduces short-term mortality, 3–5 there is uncertainty whether comprehensive regionalization of AMI care in general would lead to improved patient outcomes.6 Prior studies have estimated potential benefits at a national or state level,7, 8 but did not consider the implications of regionalization within the context of local healthcare markets (where such policies are likely to be implemented). If there are substantial differences in AMI mortality between PCI hospitals and local non-PCI hospitals, directing AMI patients to regional centers would improve outcomes. However, if PCI and non-PCI hospitals within the same region had similar outcomes, then efforts to regionalize AMI care beyond existing referral practices would be less beneficial.
To better appreciate the implications of proposals1, 2 of comprehensive regionalization of AMI care in the United States, we examined a series of research questions. First, do AMI patients have lower risk-adjusted 30-day mortality when treated at PCI hospitals compared with non-PCI hospitals? This is a necessary, but not sufficient, condition for regionalization to improve outcomes. Second, what is the hospital-level variation in risk-adjusted 30-day mortality at PCI and non-PCI hospitals? Ideally, PCI hospitals would have uniformly better outcomes than non-PCI hospitals. Finally, on a region-by-region basis, how would mortality change if all AMI patients at local non-PCI hospitals had outcomes similar to the best-performing PCI hospital within the same healthcare market (i.e., the most optimistic scenario for comprehensive regionalization)? Each of these analyses has unique implications for assessing the potential benefits of regionalizing AMI care across the United States.
Methods
Patient Data
The study population consisted of Medicare fee-for service patients age 65 years or older hospitalized with a principal discharge diagnosis of AMI (International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes 410.xx, excluding 410.x2). Three years of hospitalization data were obtained from the 2004–2006 Medicare Provider Analysis and Review (MedPAR) from the Centers for Medicare & Medicaid Services (CMS), including Part A hospital data and Part B outpatient data.
MedPAR data contain demographic information, principal discharge and secondary diagnosis codes, and procedure codes for each hospitalization. Patients discharged alive within 1 day and not against medical advice were excluded because these individuals were unlikely to have had an AMI. Additional information on comorbidities was obtained from diagnosis codes for the 12 months preceding the index admission for AMI from Part A hospital data and Part B outpatient facility data. Patient characteristics were classified into categories of comorbidities using the hierarchical condition categories classification system used by CMS to calculate risk-standardized hospital-specific AMI mortality rates.9 Dates of death were obtained from Medicare enrollment files.
We excluded patients who did not have 12 months of continuous coverage in Medicare or were hospitalized outside of the United States. Healthcare markets were defined using hospital referral regions (HRRs) from the Dartmouth Atlas of Healthcare, which empirically constructs markets based on referral patterns for major cardiovascular and neurosurgical procedures of Medicare beneficiaries.10 Because the focus of this analysis was on the impact of regionalizing AMI care, we also excluded patients admitted (1) at 59 hospitals with inadequate information in the American Hospital Association (AHA) Survey of Hospitals or unresolved zip codes; and (2) at 46 hospitals in 11 HRRs without at least 1 PCI hospital and 1 non-PCI hospital. We excluded patients admitted at hospitals with fewer than 10 AMI cases in the 3-year combined sample given the insufficient data for evaluating hospital performance.
For patients transferred from one acute-care hospital to another, hospitalizations were combined into a single episode of care with outcomes attributed to the first hospital (regardless of whether the hospital was a PCI or non-PCI hospital). Comorbidities in claims related to the second hospitalization were not included in order to avoid the misclassification of complications as pre-existing conditions.
Hospital data
We classified hospitals as PCI and non-PCI based on their capability to perform primary PCI, which we defined as emergent revascularization during ST-segment elevation myocardial infarction (STEMI). We specifically chose to define PCI hospitals based on primary PCI because this is likely to be a distinguishing characteristic of regional centers for AMI care.1, 2 Hospitals that have part-time PCI capacity in this manner is that these hospitals would be unlikely to be considered as major centers in hub-spoke regionalization efforts for AMI patients. To identify PCI hospitals, we used data from the American College of Cardiology National Cardiac Database Registry Cath-PCI (ACC-NCDR Cath-PCI) and the Hospital Quality Alliance door-to-balloon time database between 2004 and 2006. In cases where there was inconsistency, we identified billing claims related to any PCI in MedPAR data between 2004 and 2006, and then directly verified the capability to perform primary PCI using telephone interviews. Additional facility characteristics were obtained from the 2004 AHA Survey of Hospitals while AMI volume was determined by aggregating the number of AMI admissions between 2004 and 2006 in MedPAR data.
Statistical analysis
We compared baseline characteristics of patients and hospitals based on their capability for PCI, using chi-square tests for categorical variables and t-test for continuous variables. The primary outcome was death due to any cause within 30 days after the index hospitalization for AMI.
We first performed a patient-level analysis of 30-day mortality comparing AMI patients admitted at PCI hospitals with those admitted at non-PCI hospitals. We used multivariable logistic regression to determine the association between admission at PCI hospitals and 30-day mortality, adjusting for patient demographics and comorbidites. Hospital-level random intercepts were included to account for the clustering (non-independence) of patients within hospitals. Covariates used in these analyses were previously published in risk-adjustment model of 30-day mortality after AMI.11
We then performed a hospital-level analysis by calculating risk-standardized 30-day mortality rates (RSMRs) specific to each hospital. RSMRs were determined using the same methodology used by CMS for its public reporting efforts for hospital performance in AMI — an administrative risk-adjustment method validated against a medical chart-based model11 and approved by the National Quality Forum. RSMRs represent a ratio of the hospital’s predicted mortality rate to the expected mortality of an average hospital treating patients at similar clinical risk, multiplied by the national mortality rate. RSMRs were calculated using a hierarchical general linear model that adjusted for patient characteristics including age, gender, and comorbidities. A Bayesian statistical method was used to calculate RSMRs based on available information in a given sample size and number of deaths; however, hospital volume itself was not used as a variable for risk-adjustment. We categorized hospitals into quintiles of RSMR, and examine the distribution of RSMRs for PCI and non-PCI hospitals overall and within quintiles of RSMR.
Lastly, we performed a regional-level analysis to approximate how regionalization of AMI care would be expected to impact on AMI mortality within each HRR. For this analysis, we examined the difference in 30-day RSMRs between the best-performing PCI hospital and the mean of all local non-PCI hospitals within the same HRR. Comparing RSMRs for patients admitted at non-PCI hospitals to those at the PCI hospital with the lowest mortality rate in a particular HRR (i.e., the best-performing PCI hospital) represents the most optimistic scenario for regionalization. We report the number of HRRs where the RSMR difference between the best-performing PCI hospital and mean of non-PCI hospitals fell within the following categories: >3%, 1.5–2.9%, and 0–1.4% in favor of PCI hospitals, and <0% (where the best-performing PCI hospitals had a mortality rate higher than local non-PCI hospitals). We used bootstrapping methods to calculate 95% interval estimates of the number of HRRs that fall in each of these categories: the cohort of hospitals was sampled with replacement, and the RSMR difference between best-performing PCI hospital and the mean of all local non-PCI hospitals with a HRR was recalculated; this procedure was repeated for 1,600 iterations. The resulting set of RSMR differences between best-performing PCI hospital and mean of non-PCI hospitals was rank-ordered for each RSMR difference category. The 95% interval estimate of the number of HRRs for each category of RSMR difference between PCI and non-PCI hospitals was then determined using the bottom 2.5% and top 97.5% of RSMR differences within each category.
All analyses were conducted with SAS software, version 9.1.3 (SAS Institute, Inc, Cary, NC).
Results
Between 2004 and 2006, we identified 718,028 patients hospitalized for AMI at 3,873 hospitals who met our inclusion criteria. Of these, 523,119 (73%) AMI patients were admitted to 1,382 PCI hospitals and 194,909 AMI patients were admitted to 2,491 non-PCI hospitals. Mean patient age was 79 years (standard deviation, 7.9) and 51.2% were women. Due to the large sample size, statistically significant differences were observed for several patient characteristics between PCI and non-PCI hospitals; however, clinically important differences between the 2 groups were few (Table 1). Patients initially admitted to non-PCI hospitals were more likely to be transferred to another acute-care facility compared with patients initially admitted to PCI hospitals (31.4% v. 3.3%, p<0.001). Patients admitted to PCI-hospitals were more likely to have undergone cardiac catheterization, PCI, or coronary artery bypass surgery within 30-days of admission compared with patients admitted at non-PCI hospitals (Table 1).
Table 1.
Baseline patient characteristics and outcomes of AMI patients, by admission to PCI and non-PCI Hospitals
| Characteristics | Overall (N = 718,028) | PCI (n = 523,119) | Non-PCI (n = 194,909) |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD), y | 79.04 (7.9) | 78.37 (7.8) | 80.85 (8.1) |
| Female | 367,343 (51.2%) | 258,188 (49.4%) | 109,155 (56%) |
| Past cardiovascular history | |||
| History of PCI | 34,170 (4.8%) | 27,269 (5.2%) | 6,901 (3.5%) |
| History of CABG | 46,909 (6.5) | 31,577 (6.0) | 15,332 (7.9) |
| History of anterior AMI | 80,525 (11.2) | 63,860 (12.2) | 16,665 (8.6) |
| Inferior/lateral/posterior MI location | 104,992 (14.6) | 85,968 (16.4) | 19,024 (9.8) |
| History of heart failure | 216,460 (30.2) | 141,886 (27.1) | 74,574 (38.3) |
| History of prior AMI | 109,082 (15.2) | 75,099 (14.4) | 33,983 (17.4) |
| Unstable angina | 82,677 (11.5) | 59,299 (11.3) | 23,378 (12.0) |
| Chronic atherosclerosis | 528,356 (73.6) | 408,103 (78.0) | 120,253 (61.7) |
| Respiratory failure/shock | 52,490 (7.3) | 35,643 (6.8) | 16,847 (8.6) |
| Valvular heart disease | 133,287 (18.6) | 91,831 (17.6) | 41,456 (21.3) |
| Comorbid conditions | |||
| Hypertension | 424,843 (59.2) | 311,835 (59.6) | 113,008 (58.0) |
| Stroke | 49,914 (7.0) | 33,083 (6.3) | 16,831 (8.6) |
| Cerebrovascular disease | 90,304 (12.6) | 62,999 (12.0) | 27,305 (14.0) |
| Renal failure | 94,737 (13.2) | 64,889 (12.4) | 29,848 (15.3) |
| Chronic obstructive pulmonary disease | 207,250 (28.9) | 144,179 (27.6) | 63,071 (32.4) |
| Pneumonia | 90,886 (12.7) | 58,920 (11.3) | 31,966 (16.4) |
| Diabetes mellitus | 281,906 (39.3) | 200,521 (38.3) | 81,385 (41.8) |
| Protein-calorie malnutrition | 24,867 (3.5) | 17,160 (3.3) | 7,707 (4.0) |
| Dementia | 104,496 (14.6) | 65,488 (12.5) | 39,008 (20.0) |
| Paralysis, plegia | 34,118 (4.8) | 22,588 (4.3) | 11,530 (5.9) |
| Peripheral vascular disease | 147,956 (20.6) | 103,042 (19.7) | 44,914 (23.0) |
| Metastatic cancer | 25,527 (3.6) | 18,106 (3.5) | 7,421 (3.8) |
| Trauma in past year | 160,456 (22.4) | 110,206 (21.1) | 50,250 (25.8) |
| Major psychiatric disorders | 39,374 (5.5) | 25,331 (4.8) | 14,043 (7.2) |
| Chronic liver disease | 6,373 (0.9) | 4,519 (0.9) | 1,854 (1.0) |
| Discharge status (#, %) | |||
| Home | 298,084 (41.5) | 257,707 (49.3) | 40,377 (20.7) |
| Transferred | 78,248 (10.9) | 17,128 (3.3) | 61,120 (31.4) |
| SNF/ICF | 124,001 (17.3) | 84,901 (16.2) | 39,100 (20.1) |
| Home care | 92,898 (12.9) | 74,191 (14.2) | 18,707 (9.6) |
| Hospice | 12,977 (1.8) | 9,230 (1.8) | 3,747 (1.9) |
| Length of stay (mean, SD) | |||
| Mean length of stay | 6.6 (5.3) | 6.7 (5.5) | 6.3 (4.3) |
| Observed mortality (#, %) | |||
| In-hospital | 77,216 (10.8) | 53,984 (10.3) | 23,232 (11.9) |
| 30-day | 119,385 (16.6) | 79,086 (15.1) | 40,299 (20.7) |
| Procedures within 30 days (#, %) | |||
| Cardiac catheterization | 321,492 (44.8) | 302,432 (57.8) | 19,060 (9.8) |
| PCI | 198,889 (27.7) | 195,380 (37.4) | 3,509 (1.8) |
| CABG | 57,324 (8.0) | 56,110 (10.7) | 1,214 (0.6) |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; ICF, intermediate care facility; PCI, percutaneous coronary intervention; SD, standard deviation; SNF, skilled nursing facility
Patients who were transferred to another acute care hospital had outcomes assigned to the initial index hospitalization. P<0.001 for all comparisons between PCI and non-PCI hospital.
Differences in facility characteristics between PCI and non-PCI hospitals are summarized in Table 2. On average, PCI hospitals had more beds (339 v. 109, p<0.001) and annual Medicare fee-for-service AMI admissions (125 v. 25, p<0.001). A greater proportion of PCI hospitals were teaching hospitals and not-for-profit or privately-owned hospitals compared with non-PCI hospitals.
Table 2.
Characteristics of PCI and non-PCI hospitals
| Characteristics | All hospitals (n = 3873) | PCI hospitals (n = 1382) | Non-PCI hospitals (n = 2491) |
|---|---|---|---|
| Teaching | 740 (19.1) | 589 (42.6) | 151 (6.1) |
| COTH member | 283 (7.3) | 251 (18.2) | 32 (1.3) |
| Ownership | |||
| Public | 706 (19.4) | 152 (11.3) | 554 (24.2) |
| Not-for-profit | 2,350 (64.5) | 947 (70.1) | 1,403 (61.3) |
| Private | 585 (16.1) | 252 (18.7) | 333 (14.5) |
| No. of beds, mean (SD) | 195 (189.6) | 339 (220.1) | 109 (95.4) |
| Annual AMI volume (SD) | 61.5 (77.4) | 125.3 (95.6) | 25.1 (26.3) |
| Urban | 2,114 (54.6) | 1,201 (86.9) | 913 (36.7) |
| Census division | |||
| Northeast | 178 (4.6) | 53 (3.8) | 125 (5.0) |
| Middle Atlantic | 419 (10.8) | 153 (11.1) | 266 (10.7) |
| South Atlantic | 629 (16.2) | 201 (14.5) | 428 (17.2) |
| East North Central | 644 (16.6) | 234 (16.9) | 410 (16.5) |
| East South Central | 350 (9.0) | 110 (8.0) | 240 (9.6) |
| West North Central | 461 (11.9) | 117 (8.5) | 344 (13.8) |
| West South Central | 522 (13.5) | 212 (15.3) | 310 (12.4) |
| Mountain | 217 (5.6) | 107 (7.7) | 110 (4.4) |
| Pacific | 453 (11.7) | 195 (14.1) | 258 (10.4) |
AMI, acute myocardial infarction; COTH, Council of Teaching Hospitals and Health Systems; SD, standard deviation; PCI, percutaneous coronary intervention
Patient-level analysis
Overall, 30-day mortality was significantly lower for AMI patients admitted to PCI hospitals compared with patients admitted at non-PCI hospitals (15.1% vs. 20.7%, p<0.001; odds ratio [OR], 0.68, 95% confidence interval 12 0.76–0.69). After adjusting for age, gender, and comorbidities, this difference in 30-day mortality diminished but remained significantly lower for patients admitted at PCI hospitals (OR=0.89, 95% CI 0.88–0.91).
Hospital-level analysis
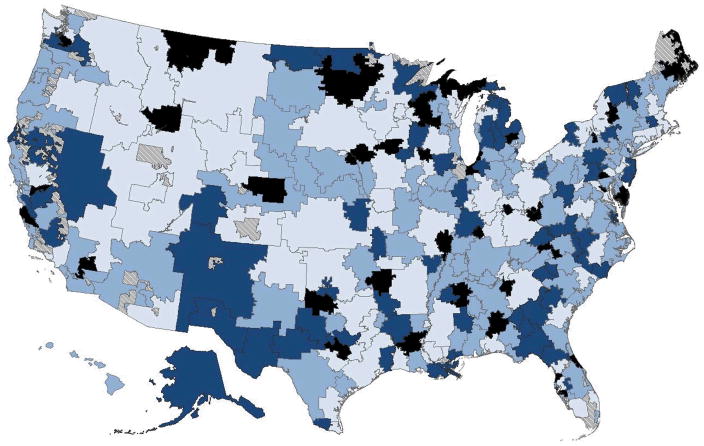
On average, PCI hospitals had lower RSMRs compared with non-PCI hospitals (mean RSMR 16.1% v 16.9%, p<0.001), an absolute difference of 0.8%. However, RSMRs varied widely within both PCI hospitals (SD=1.8%, range 10.8% to 23.8%) and non-PCI hospitals (SD=1.4%, range 12.6% to 23.0%), leading to substantial overlap between the two hospital groups (Figure 1).
Figure 1.
Distributions of 30-day risk-standardized mortality rate by percutaneous coronary intervention (PCI) and non-PCI hospitals.
Stratifying all hospitals into RMSR quintiles, we observed a larger number of PCI hospitals in the best-performing quintile. The top performing quintile (RSMR range 10.8% to 15.5%) included 440 (31.8%) of all PCI hospitals and 335 (13.5%) of all non-PCI hospitals. Hospitals in the top performing quintile treated 209,990 (40.1%) of all patients at PCI hospitals and 41870 (21.5%) of all patients at non-PCI hospitals. By contrast, hospitals in the lowest performing quintile included a comparable proportion of PCI hospitals (n=259, 18.7%) and non-PCI hospitals (n=516, 20.7%).
Regional-level analysis
In order to examine the impact of comprehensive regionalization of AMI care on outcomes at the regional level, absolute differences in 30-day RSMRs between the best-performing PCI hospital and the mean of the RSMRs of all local non-PCI hospitals within the same HRR were compared. This represents an optimistic scenario for regionalization to change local outcomes. The overall mean difference across all HRRs between the two hospital groups was 1.9%, favoring the best-performing PCI hospitals. However, there was a wide range of differences across individual HRRs, varying from a 6.1% lower RSMR favoring the best-performing PCI hospital to a 2.8% lower RSMR favoring the local non-PCI hospitals.
HRRs were categorized into four groups based on the extent of absolute differences between the best-performing PCI hospital and non-PCI hospitals within the same HRR (Table 3). Overall, 80 HRRs had ≥3% difference in RSMRs favoring the best-performing PCI hospital, 104 HRRs with a 1.5–3% difference, and 74 HRRs with a 0.01–1.5% difference compared with local non-PCI hospitals. However, there were 37 HRRs where the best-performing PCI hospital had RSMRs that were no better or higher than local non-PCI hospitals; in these 37 HRRs, the difference in favor of non-PCI hospitals was in general small (mean 1.0%, with standard deviation of 0.7%).
Table 3.
Difference in 30-day RSMR between PCI hospital with the lowest RSMR and the mean RSMR of all non-PCI hospitals within a healthcare referral region (HRR)
| ≥3% | 1.5–3% | 0.01–1.5% | <0% | Overall | |
|---|---|---|---|---|---|
| Percentage point difference in | |||||
| RSMR, | |||||
| median, | 3.6 | 2.4 | 0.9 | −0.9 | 2.2 |
| mean (range) | 3.8 (3.0–6.1) | 2.4 (1.5–3.0) | 0.9 (0.01–1.5) | −1.0 (−2.8–[−]0.2) | 1.9 (−2.8–6.1) |
| # PCI hospitals, mean (range) | 7.3 (1–42) | 4.9 (1–25) | 3.0 (1–10) | 1.7 (1–4) | 4.7 (1–42) |
| # non-PCI hospitals, mean (range) | 12.7 (1–49) | 8.4 (1–31) | 5.8 (1–16) | 4.7 (1–16) | 8.4 (1–49) |
| # HRRs (95% interval estimate) | 80 (69 to 94) | 104 (88 to 117) | 74 (61 to 87) | 37 (29 to 46) | 295 |
| # PCI hospital patients | 215,149 | 190,910 | 87,394 | 29,666 | 523,119 |
| # non-PCI hospital patients | 76,628 | 73,519 | 32,423 | 12,339 | 194,909 |
HRR, hospital referral region; PCI, percutaneous coronary intervention; RSMR, risk-standardized mortality rate
Positive RSMR differences represent that the best PCI hospital had lower RSMR than the mean of all non-PCI hospitals within the HRR.
Negative RSMR differences represent that the best PCI hospital had higher RSMR than the mean of all non-PCI hospitals within the HRR.
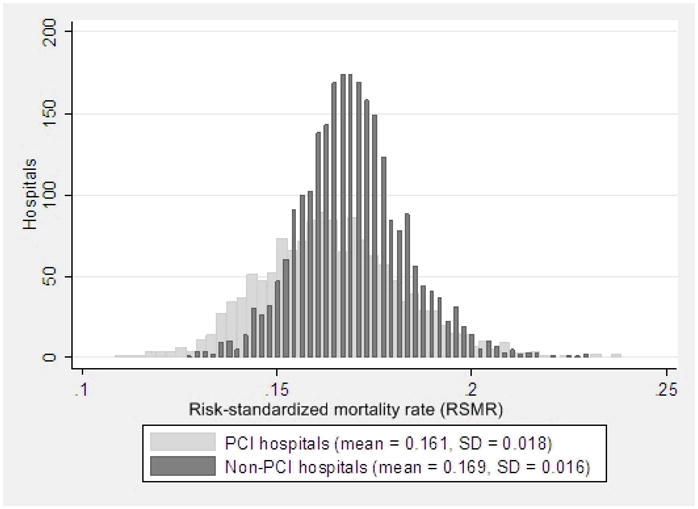
Most HRRs (Figure 2) where differences in RSMRs were ≥3% and favored the best-performing PCI hospital were concentrated in the Mountain and Midwest regions, although select major urban areas were also identified in the Northeast. No discernable geographic pattern was seen for HRRs where the best-performing PCI hospital had RSMRs that were no better or higher than local non-PCI hospitals.
Figure 2.
Differences in 30-day risk-standardized mortality rate between best-performing percutaneous coronary intervention (PCI) hospital and mean non-PCI hospitals by hospital referral region (HRR)
Light blue: Difference ≥3% between best-performing PCI hospital RSMR and the mean of local non-PCI hospital RSMRs within the same hospital referral region
Medium blue: Difference of 1.5–3% between best-performing PCI hospital RSMR – mean of local non-PCI hospital RSMRs within the same hospital referral region
Dark blue: Difference of 0–1.5% between best-performing PCI hospital RSMR – mean of local non-PCI hospital RSMRs within the same hospital referral region
Black: Best-performing PCI hospital RSMR > mean of local non-PCI hospital RSMRs within the same hospital referral region
Hatched: Data not available for hospital referral region
Discussion
Our study illustrates the complexity surrounding decisions to regionalize AMI care in the United States. We found that admission to a PCI hospital was associated with a lower 30-day mortality compared with admission to a non-PCI hospital. Prior studies that have examined the association between a hospital’s capacity for invasive cardiac procedures and clinical outcomes focused almost exclusively on this type of patient-level analysis.13–17 If the benefits of AMI regionalization are judged by results from this perspective alone, our data would support regionalizing AMI care at PCI hospitals – a strategy, however, that could be misleading for a number of regions.
To understand why this may be true requires an examination of our hospital- and regional-level analyses. Our hospital-level analysis found considerable overlap in the distribution of RSMRs between PCI and non-PCI hospitals, demonstrating that PCI hospitals do not uniformly have better outcomes than non-PCI hospitals. Our regional-level analysis found that an absolute mortality difference ≥3% was present between the best-performing PCI and non-PCI hospitals in 80 out of 295 HRRs (95% interval estimate 69 to 94 HRRs). In contrast, there were 37 HRRs where the best-performing PCI hospital had a higher RSMR than local non-PCI hospitals (95% interval estimate 29 to 46 HRRs). This wide variation in differences in RSMRs between the two groups of hospitals across HRRs reinforces the need to carefully examine outcomes on a region-by-region basis prior to embarking on strategies to direct AMI care to PCI hospitals.
Our results do not imply that transfer of high-risk patients to PCI-hospitals for invasive cardiac procedures or advanced specialty care is not warranted. Many clinical scenarios exist where patients are likely to benefit from transfer to these specialized centers. Instead, what these findings highlight is that the presence or absence of PCI alone has a limited ability to stratify hospital performance with respect to 30-day mortality rates. Since the effectiveness of proposals to comprehensively regionalize all AMI care1, 2 depends on the magnitude of existing differences between hospitals that initiate or receive transfers, it would be valuable to consider differences in hospital-specific outcomes within a region when planning strategies to consolidate AMI care at particular facilities.
The finding that many non-PCI hospitals performed as well or better than even the best PCI hospital in their region suggests that factors other than availability of invasive cardiac procedures likely contribute to hospital performance for AMI care. In an earlier Canadian study, for example, better outcomes at hospitals with invasive cardiac procedures were predominantly explained by teaching status, which itself is a proxy for important processes of care that have yet to be identified.13 As such the capacity for PCI may be one of many structural and process characteristics of hospital performance to be considered when developing regional systems of care for AMI.18 Determining the most effective and transferable elements of hospital structure and the processes and treatments that hospitals employ to lower AMI mortality is challenging, and will likely require novel research methods with comprehensive clinical data. One such approach is to combine qualitative and quantitative analysis to identify operational strategies associated with outstanding performance in door-to-balloon times for primary PCI;19 there is a need to perform similar studies for overall AMI outcomes.
Limitations
Our study should be interpreted in the context of the following limitations. First, Medicare claims data are unable to reliably distinguish AMI patients with STEMI from those with non-STEMI. While this makes our analysis less germane for systems of care that specifically target the emergent transfer of patients with STEMI for primary PCI, it directly informs the larger debate on centralizing care of all patients with acute coronary syndromes,1, 2, 6 including the much larger group of AMI patients with non-STEMI.
Second, the number of AMI regionalization programs has likely expanded since the 2004–2006 time period of our study. While the number of regionalization systems has increased over time, not all areas in the country currently have such strategies and our study provides guidance to policymakers regarding new implementations of regionalization programs. While an implicit but limited form of AMI regionalization exists in the form of select transfers from non-PCI to PCI hospitals for STEMI care the goal of our study was to investigate how outcomes would be expect to differ from directing the majority of AMI patients (including non-STEMI) to PCI hospitals within a particular HRR, as advocated by some experts.1, 2
Third, we were unable to assess non-fatal outcomes such as reinfarction and readmission. Similarly, we were unable to assess important dimensions to care that may affect AMI regionalization such as patient preferences for transfer and quality of life after AMI. However, because the primary motivation for regionalization of AMI care is the reduction of short-term mortality, we believe this issue is of secondary importance.
Fourth, our analysis assumes that redistributing patients across hospitals has no adverse consequences. It is possible that logistical issues such as longer transportation time or delays due to reaching capacity limits may reduce the benefit actually achievable from transferring patients to PCI hospitals. As such our analysis represents the most optimistic scenario for regionalization assuming with the greatest potential difference between non-PCI and PCI hospital outcomes.
Lastly, due to the Bayesian statistical approach used to calculate RSMRs, low-volume hospitals typically have RSMRs closer to the mean mortality rate compared with high-volume hospitals. This is because with limited information, the best estimate of a hospital’s RSMR is the mean mortality rate on average, (i.e. small samples contain less information to determine whether the RSMR deviates from the mean). Because non-PCI hospitals typically have fewer AMI cases than PCI hospitals, non-PCI hospitals would be less able to distinguish themselves as high performers on the basis of RSMR. We attempt to mitigate this concern by limiting our analysis to hospitals with at least 10 AMIs over three years.
Conclusion
Our study found that 30-day mortality rates for AMI are lower for PCI hospitals when compared with non-PCI hospitals. However, we also noted considerable overlap in hospital performance between the two groups of hospitals. Examining healthcare markets, we found that regionalizing AMI care to PCI hospitals is likely to reduce mortality in a subset of regions where differences in mortality between PCI and non-PCI hospitals are substantial, but less likely to do so in many regions where differences were less sizeable. In designing systems for regionalizing AMI care across the United States, policy-makers should specifically consider the performances of hospitals within each region to optimize the benefits of this approach.
Acknowledgments
The authors would like to acknowledge the review of earlier drafts of the manuscript by Andrew J. Epstein, Ph.D. Yale University School of Epidemiology and Public Health
The Centers for Medicare & Medicaid Services reviewed and approved the use of its data for this work, and approved submission of the manuscript; this approval is based on data use only, and does not represent a Centers for Medicare & Medicaid Services endorsement or comment on the manuscript content.
Drs. Chen and Wang had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The following authors have the potential conflicts of interest to disclose in relation to this study: Dr. Normand is a primary investigator for the Mass-DAC trial examining new capacity of primary PCI centers in Massachusetts. The remaining authors have no conflicts of interest to disclose related to this manuscript.
References
- 1.Califf RM, Faxon DP. Need for centers to care for patients with acute coronary syndromes. Circulation. 2003 Mar 25;107(11):1467–1470. doi: 10.1161/01.cir.0000065160.19016.26. [DOI] [PubMed] [Google Scholar]
- 2.Topol EJ, Kereiakes DJ. Regionalization of care for acute ischemic heart disease: a call for specialized centers. Circulation. 2003 Mar 25;107(11):1463–1466. doi: 10.1161/01.cir.0000063680.45780.a0. [DOI] [PubMed] [Google Scholar]
- 3.Andersen HR, Nielsen TT, Rasmussen K, et al. A Comparison of Coronary Angioplasty with Fibrinolytic Therapy in Acute Myocardial Infarction. N Engl J Med. 2003 August 21;349(8):733–742. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]
- 4.Grines CL, Westerhausen DR, Jr, Grines LL, et al. A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction: the Air Primary Angioplasty in Myocardial Infarction study. J Am Coll Cardiol. 2002 Jun 5;39(11):1713–1719. doi: 10.1016/s0735-1097(02)01870-3. [DOI] [PubMed] [Google Scholar]
- 5.Widimsky P, Budesinsky T, Vorac D, et al. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial--PRAGUE-2. Eur Heart J Jan. 2003;24(1):94–104. doi: 10.1016/s0195-668x(02)00468-2. [DOI] [PubMed] [Google Scholar]
- 6.Rathore SS, Epstein AJ, Volpp KGM, Krumholz HM. Regionalization of Care for Acute Coronary Syndromes: More Evidence Is Needed. JAMA. 2005 March 16;293(11):1383–1387. doi: 10.1001/jama.293.11.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright SM, Daley J, Peterson ED, Thibault GE. Outcomes of acute myocardial infarction in the Department of Veterans Affairs: does regionalization of health care work? Med Care Feb. 1997;35(2):128–141. doi: 10.1097/00005650-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Epstein AJ, Rathore SS, Krumholz HM, Volpp KG. Volume-based referral for cardiovascular procedures in the United States: a cross-sectional regression analysis. BMC Health Serv Res. 2005;5:42. doi: 10.1186/1472-6963-5-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev Summer. 2004;25(4):119–141. [PMC free article] [PubMed] [Google Scholar]
- 10.Wennberg DE. Dartmouth Atlas of Cardiovascular Health Care Health Forum Publishing Company. 2000. [PubMed] [Google Scholar]
- 11.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006 Apr 4;113(13):1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 12.Henry TD, Atkins JM, Cunningham MS, et al. ST-segment elevation myocardial infarction: recommendations on triage of patients to heart attack centers: is it time for a national policy for the treatment of ST-segment elevation myocardial infarction? J Am Coll Cardiol. 2006 Apr 4;47(7):1339–1345. doi: 10.1016/j.jacc.2005.05.101. [DOI] [PubMed] [Google Scholar]
- 13.Alter DA, Naylor CD, Austin PC, Tu JV. Long-term MI outcomes at hospitals with or without on-site revascularization. JAMA. 2001 Apr 25;285(16):2101–2108. doi: 10.1001/jama.285.16.2101. [DOI] [PubMed] [Google Scholar]
- 14.Every NR, Parsons LS, Fihn SD, et al. Long-term outcome in acute myocardial infarction patients admitted to hospitals with and without on-site cardiac catheterization facilities. MITI Investigators. Myocardial Infarction Triage and Intervention. Circulation. 1997 Sep 16;96(6):1770–1775. doi: 10.1161/01.cir.96.6.1770. [DOI] [PubMed] [Google Scholar]
- 15.Every NR, Larson EB, Litwin PE, et al. The association between on-site cardiac catheterization facilities and the use of coronary angiography after acute myocardial infarction. Myocardial Infarction Triage and Intervention Project Investigators. N Engl J Med. 1993 Aug 19;329(8):546–551. doi: 10.1056/NEJM199308193290807. [DOI] [PubMed] [Google Scholar]
- 16.Halabi AR, Beck CA, Eisenberg MJ, Richard H, Pilote L. Impact of on-site cardiac catheterization on resource utilization and fatal and non-fatal outcomes after acute myocardial infarction. BMC Health Serv Res. 2006;6:148. doi: 10.1186/1472-6963-6-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krumholz HM, Chen J, Murillo JE, Cohen DJ, Radford MJ. Admission to hospitals with on-site cardiac catheterization facilities :impact on long-term costs and outcomes. Circulation. 1998 Nov 10;98(19):2010–2016. doi: 10.1161/01.cir.98.19.2010. [DOI] [PubMed] [Google Scholar]
- 18.Peterson ED, Ohman EM, Brindis RG, Cohen DJ, Magid DJ. Development of systems of care for ST-elevation myocardial infarction patients: evaluation and outcomes. Circulation. 2007 Jul 10;116(2):e64–67. doi: 10.1161/CIRCULATIONAHA.107.184051. [DOI] [PubMed] [Google Scholar]
- 19.Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006 Nov 30;355(22):2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]