Abstract
Myofibrillar myopathies (MFMs) are a heterogeneous group of neuromuscular disorders characterized by disintegration of myofibrils. The inheritance pattern in MFMs is commonly autosomal dominant, but there has been a striking absence of secondary cases noted in a BAG3-associated subtype. We studied three families with BAG3 p.Pro209Leu mutation showing a severe phenotype of myofibrillar myopathy and axonal neuropathy with giant axons. In one family, transmission to a pair of siblings has occurred from their asymptomatic father who showed somatic mosaicism. In two other families, neither of the parents was affected or showed detectable level of somatic mosaicism. These observations suggest that the BAG3 variant of MFM may result from a spontaneous mutation at an early point of embryonic development and that transmission from a mosaic parent may occur more than once. The study underlines the importance of parental evaluation as it may have implications for genetic counseling.
Keywords: myofibrillar myopathy, limb-girdle muscular dystrophy, cardiomyopathy, giant axons, Bcl-2-associated athanogene 3 (BAG3)
1. Introduction
Myofibrillar myopathies (MFMs) are a group of heterogeneous disorders having in common myopathological features of disintegration of myofibrils and accumulation of degradation products into inclusions containing desmin and other myofibrillar and ectopic proteins [1,2]. These disorders are known to be associated with mutations in one of the MFM-causing genes: DES, CRYAB, MYOT, ZASP, FLNC, or BAG3. The most frequent inheritance pattern in each of the genetically distinct subtypes is autosomal dominant, but in a significant number of patients mutations occurred de novo [3]. For example, several thoroughly studied sporadic patients with desminopathy the transmitting parent was identified as germline mosaic based on haplotype analysis [4,5], while known patients with mutations in MYOT, ZASP or FLNC frequently had late disease onset and their parents were not available for study [6,7,8,9].
An early-onset subtype of MFM caused by a mutation in the BAG3 gene has recently been discovered [10]. Each of the three patients described in the original report had asymptomatic parents. They presented in childhood with rapidly progressive limb and axial muscle weakness, cardiomyopathy and respiratory insufficiency; one of the patients died in his early teens. A heterozygous BAG3 p.Pro209Leu mutation was identified in each patient but not in their parents. The Bcl-2-associated athanogene 3 (BAG3) is a cyto-protective protein that regulates the Hsp70 family of molecular chaperones. BAG3 is expressed in skeletal and cardiac muscles and colocalizes with Z-discs. Mice with homozygous disruption of the bag3 gene developed a fulminant myopathy characterized by myofibrillar degeneration with apoptotic features [11].
We studied patterns of inheritance in a typical BAG3-mutation-associated variant of MFM in three unrelated families in an attempt to identify the mode of disease transmission.
2. Patients and Methods
2.1. Clinical and pathological investigations
We have identified and studied three families (1, 2, and 3) with young patients suffering from severe MFM-like disease. Two individuals were clinically affected in family 1 (patients 1–3 and 1–4), one in family 2 (patient 2–3), and one in family 3 (patient 3–3). Investigations included pedigree analysis, neurologic exam, muscle strength assessment according to the Medical Research Council (MRC) grading scale, serum CK level, nerve conduction tests and concentric needle EMG, respiratory function tests and cardiologic examination with electrocardiography and echocardiography. Skeletal muscle biopsy tissue was processed for routine histochemical reactions and immunocytochemical analysis using antibodies against desmin (DACO); part of the sample was processed for ultrastructural examination by standard methods. Sural nerve biopsy specimens were fixed in either 2.5% or 3% glutaraldehyde buffered to pH 7.4 with 0.1 M phosphate buffer. Transverse sections were post-fixed in 0.1 M osmic tetroxide for 2 h, dehydrated and embedded in Spurt resin. Semi-thin sections were stained with toluidine blue. Genomic DNA was available from each patient and their unaffected parents. Genetic studies were approved by the Institutional Review Board of the National Institute of Neurological Disorders and Stroke, NIH. Informed consent was obtained from each living individual.
2.2. PCR amplification, enzymatic digestion, cloning and sequencing
Genomic DNA was extracted from anticoagulated blood using QIAamp® DNA Blood Kit (Qiagen Sciences, MD, USA) and used as template for amplification of each BAG3 exon with intronic primers (primer sequences are available on request). Resulting fragments were purified by MinElute™ 96 UF PCR Purification Kit (QUAGEN Sciences, Gaithersburg, MD, USA) and sequenced in both directions using DyeTerminator™ Sequencing Protocol on an ABI 3100 DNA Analyzer (Applied Biosystems, Foster City, CA, USA). Exon 3 containing fragments amplified with primers 5′-CAAGCCAGGGGAGTCATTT and 5′-ACCCACAGAGCTCCTGCAC were digested with restriction endonuclease BsaWI (New England Biolabs® Inc, Boston, MA, USA), according to the manufacturer’s instructions, resolved in a 2% UltraPure™ Agarose (Invitrogen, Carlsbad, CA, USA), and photographed under the UV light. The BsaWI-resistant fragment containing the disease-causing mutation was gel-extracted using QIAquick Gel Extraction Kit (Qiagen Sciences, Gaithersburg, MD, USA) and cloned using The Original TA cloning kit (Invitrogen, Carlsbad, CA, USA). Plasmid DNA was isolated from overnight cultures with Purelink™ HQ Mini Plasmid Purification Kit (Invitrogen, Carlsbad, CA, USA) and 10 clones were sequenced with the M13 forward and reverse primers by using the above mentioned sequencing protocol.
2.3. Genotyping and fragment analysis
To determine the parental origin of the mutant allele, genotyping was carried out with 5 markers from the BAG3 region on chromosome 10q: D10S1701, D10S1792, D10S1722, D10S1230, and D10S1483 located within a 2.5 centimorgan (1.5 megabase pairs) chromosomal fragment. PCR amplification was performed by using primers, one of which was fluorescently labeled. Allele code was expressed as “CA” of “TTA” repeat number. This analysis was also used to verify biological parentage. Semi-quantitative analysis of the mutant allele in genomic DNA was accomplished by a separate amplification of a 222-bp exon 3 fragment with primers 5′-TGCTCATCCTCATCCTCCTC and 5′-6FAM-CCCCTGGATCTTGTGGTACA, of which the reverse primer was color-labeled. After restriction with BsaWI, the mutation-containing fragment was profiled. Fragment analysis for genotyping and mutant allele profiling were performed on an ABI 3100 DNA Analyzer (Applied Biosystems, Foster City, CA, USA).
3. Results
3.1. Phenotypic features and disease outcomes
Signs of developing skeletal myopathy or cardiomyopathy first appeared in each child at the age of 5 to 12 years (Table 1). In Family 1, two male siblings (Patients 1–3 and 1–4) born from clinically unaffected and unrelated British parents, current age 55 and 58 years, developed predominantly proximal muscle weakness, restrictive/hypertrophic cardiomyopathy, and respiratory insufficiency. The younger brother died soon after the disease onset at age 9 years; the older had a cardiac transplant at age 14 years and is alive but severely disabled and ventilator dependent at the age of 29 years (Table 1). On muscle biopsy, both showed myofibrillar breakdown, the presence of desmin-reactive inclusions, and Z-line streaming. Sural nerve biopsy in the younger brother revealed signs of axonal pathology with no obvious demyelination and the presence of giant axons (Table 2).
Table 1.
Clinical characteristics of patients with BAG3 p.Pro209Leu mutation
| Features | Family 1 | Family 2 | Family 3 | |
|---|---|---|---|---|
| Patient 1–3 | Patient 1–4 | Patient 2–3 | Patient 3–3 | |
| Onset age (yrs) | 12 | 9 | 12 | 5 |
| Gender (Male-M, Female-F) | M | M | F | M |
| Initial symptoms | ||||
| Skeletal muscles initially involved | Neck, Prox U, L | Prox U, L | Neck, Distal L | Prox U, L |
| Cardiomyopathy | At onset | At onset | At onset | At age 10 |
| Advanced illness | ||||
| Generalized muscle weakness | + | + | + | + |
| Muscle atrophy | + | + | + | + |
| Skeletal deformity | + | − | + | − |
| Respiratory weakness | At age 15 | At age 9 | At age 20 | At age 10 |
| Restrictive CM | + | + | + | + |
| Hypertrophic CM | + | + | + | + |
| Peripheral neuropathy | + | + | + | + |
| Laboratory/physiological studies | ||||
| Creatine kinase level | Normal | NA | 2–3 times Normal | Normal |
| EMG | Neurogenic/Myopathic | NA | Myopathic | Neurogenic/Myopathic |
| Nerve conduction study | Axonal neuropathy | NA | Axonal neuropathy | Axonal neuropathy |
| Outcome | ||||
| Wheelchair dependency | At age 14 | − | + | − |
| Heart transplantation | At age 14 | − | − | At age 13 |
| Ventilator dependency | At age 29 | − | − | At age 13 |
| Sudden death | Alive | At age 9 | At age 20 | At age 15 |
| Duration of illness | 17 yrs | 4 mo | 8 yrs | 10 yrs |
Prox – proximal muscles; Dist – distal muscles; U – upper extremities; L – lower extremities; EMG – electromyography; NA – data not available
Table 2.
Myopathological features in patients with myofibrillar myopathy caused by the BAG3 p.Pro209Leu mutation
| Features | Family 1 | Family 2 | Family 3 | |
|---|---|---|---|---|
| Patient 1–3 | Patient 1–4 | Patient 2–3 | Patient 3–3 | |
| Biopsied muscle | Left triceps | (PM) | Right deltoid | Right vastus lateralis |
| LM: Variation of fiber size | + | NA | + | + |
| Abnormal desmin-positive inclusions | + | +* | + | + |
| EM: Myofibrillar breakdown | + | NA | + | + |
| Granulofilamentous material | + | NA | + | NA |
| Nerve biopsy: axonal loss, giant axons | NA | + | + | + |
LM – light microscopy; EM – electron microscopy; (PM) – postmortem study;
The description of postmortem study in this patient indicates accumulation of desmin between the myofibrils;
NA – data not available
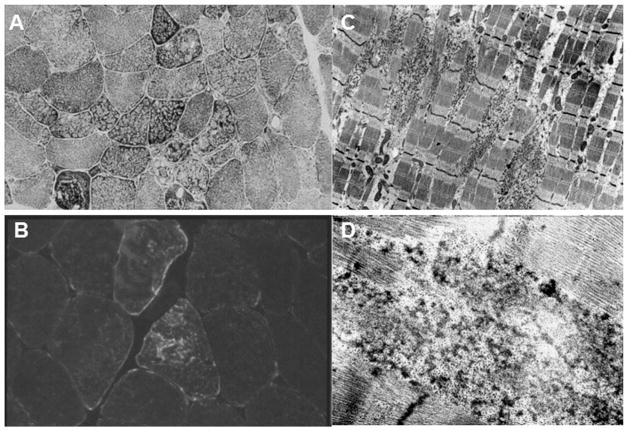
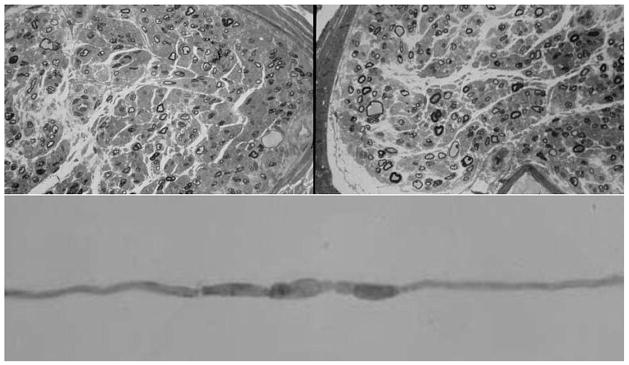
The previously reported [12] patient of Family 2 was the only child of non-consanguineous clinically unaffected parents of Italian descent, currently in their 60s. At the age of 12 years she developed bilateral pes cavus and slight dorsal scoliosis, neck and distal leg muscle weakness progressing to generalized wasting, and restrictive cardiomyopathy with secondary enlargement of both atria (Table 1). Muscle biopsy showed an accumulation of dark dense material throughout the myofiber sarcoplasm, increment of the intermyofibrillar spaces, and multiple core areas (Figure 1A). The intracytoplasmic inclusions were immunopositive for desmin (Figure 1B). Ultrastructurally, there was accumulation of electron dense filamentous and granular material disrupting the Z-lines (Figures 1C and D). Sural nerve biopsy showed reduced density of myelinated axons and the occurrence of giant axons (Figure 2, upper images). Teased-fibre studies revealed focal axonal enlargements (Figure 2, lower image). The patient died at the age of 20 years of cardiac and respiratory failure.
Figure 1.
Analysis of a muscle biopsy sample from a patient with BAG3 p.Pro209Leu mutation (Family 2). A, cryostat section of a muscle biopsy sample stained with NADH shows fibre diameter variability and marked irregularity of the intermyofibrillar network with many fibres showing multiple core areas. B, increased immunoreactivity for desmin under the sarcolemma and within the cytoplasm of some fibres. C, D, on EM analysis, electrondense granulofilamentous material emanating from the Z-discs.
Figure 2.
Sural nerve morphology in a patient with BAG3 p.Pro209Leu mutation (Family 2). A, B, transverse sections show moderate loss of myelinated fibers and the presence of several giant axons (original magnification 1:200). C, teased fibre showing focal axonal enlargements.
The patient of Family 3, one of two children of unaffected parents of British heritage, had problems running since the age of 5 years. He was diagnosed with restrictive cardiomyopathy at age 10 and went on to have heart transplantation at 13. He has been ventilator-dependent ever since. The patient developed global muscle weakness, predominantly in proximal and respiratory muscles and died at 15 years of age. Muscle biopsy showed atrophic fibers, focal myofibrillar disorganization, and dark inclusions with prominence of desmin (Table 2). On right sural nerve biopsy, moderate reduction of large diameter myelinated fibres and visible loss of smaller diameter fibres, occasional giant axons having thin or absent myelin sheaths were observed. His younger brother remains unaffected.
3.2 Transmission patterns
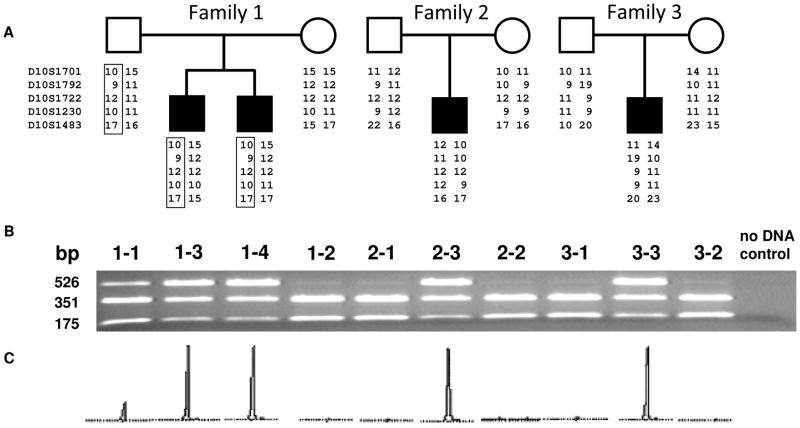
The causative mutation identified in each patient by genomic DNA sequencing was the previously reported [10] CCG-to-CTG substitution at codon 209 of BAG3 predicting a p.Pro209Leu amino acid change. The presence of this mutation was confirmed by digestion with BsaWI endonuclease. Testing with a series of microsatellite markers did not identify alleles coming from a source other than the parents. Both affected children in Family 1 inherited the disease-associated haplotype 10-9-12-10-17 from their father (Figure 3A), suggesting that the father is germline mosaic. DNA analysis (Figure 3B,C) has also identified this father as somatically mosaic for the p.Pro209Leu mutation; the presence of the p.Pro209Leu mutation in his lymphocytes was additionally confirmed by cloning and subsequent sequencing of the BsaWI-resistant portion of the PCR-amplified exon 3. The approximate degree of somatic mosaicism in the mutation-carrying father of the two patients in Family 1 was estimated by considering the area under the peak corresponding to the mutant allele and divided by the sum of the wild-type and mutant peak areas. The calculated proportion of the mutant chromosome is 17%. The mother of the patients in Family 1 was found not to carry this mutation. Haplotype analysis in Families 2 and 3 was non-informative, making it impossible to identify the transmitting parent, and neither parent showed evidence of somatic mosaicism.
Figure 3.
Family structure and mutation analyses in three families affected with BAG3-associated subtype of myofibrillar myopathy. A, family pedigrees and the results of haplotype analysis with microsatellite markers from the BAG3 region on chromosome 10q. Allele identification is provided according to the number of “CA” or “TTA” repeats. BAG3 gene is located between D10S1792 and D10S1722. B, agarose gel electrophoresis of PCR-amplified exon 3 fragments of BAG3 restricted with BsaWI. The upper band is a 526-nt BsaWI-resistant fragment containing the disease-causing mutation; the middle and the lower 353-nt and 173-nt bands are portions of the restricted non-mutant fragment. C, mutant portion of the PCR-amplified exon 3 restricted with BsaWI and subjected to capillary electrophoresis.
DISCUSSION
We conducted a study of the underlying mechanisms of disease transmission in three families with myofibrillar myopathy caused by the BAG3 p.Pro209Leu mutation. Haplotype analysis, informative in Family 1, indicates that two affected siblings inherited the pathogenic allele from their asymptomatic father, suggesting that the father was germline mosaic. Although uninformative in Families 2 and 3 regarding the parental source of the mutant allele, the microsatellite haplotypes were distinct from those in Family 1, clearly excluding haplotype sharing between these families, notably the families of British origin. This indicates that the BAG3 p.Pro209Leu has occurred de novo mutation in each studied family.
Additional studies that included fragment-length analysis and cloning with subsequent sequencing of the BsaWI-resistant portion of exon 3 have shown for the first time that the pathogenic BAG3 mutation can be transmitted from a mosaic father to more than one of his children. A recurrent transmission from the same parent indicates that the mutation is present in a significant proportion of his germ cells [13]. The father in Family 1 also displays somatic mosaicism for the BAG3 p.Pro209Leu mutation; the presence of this substitution in leukocyte DNA is consistent with a postzygotic mutation occurring in early embryonic development.
Somatic mosaicism is considered a reflection of germline mosaicism and is frequently observed in hemophilia A and B, Duchenne muscular dystrophy and facioscapulohumeral muscular dystrophy [13]. As the risk for a second child to inherit a mutation from a germline mosaic parent could be as high as 50%, testing for somatic mosaicism is important, although it has to be cautioned that germline mosaicism may be present in the absence of somatic mosaicism, so the risk of another affected child will never be zero. Since the disease associated with the BAG3 p.Pro209Leu mutation starts early in life and results in incapacity and frequently death before reaching reproductive age, transmission from affected individuals is unlikely.
Each of the studied patients show the same severe phenotype with evidence of myofibrillar myopathy. In at least one patient per family we also found an association of myofibrillar myopathy with axonal polyneuropathy as suggested by nerve conduction studies. Nerve biopsy performed in three patients showed relative reduction of myelinated axons and peculiar scattered giant axons. Thus, axonal neuropathy with giant axons seems to be characteristic of BAG3-related myofibrillar myopathy. We studied recently a patient from an independent (fourth) family with the same BAG3 p.Pro209Leu mutation who on nerve biopsy also had axonal loss, thinly myelinated giant axons, and “abundant collagen pockets” (L. Hudgins, unpublished observation). The disease mechanisms leading to myofibrillar myopathy/axonal neuropathy with giant axons are currently unknown. It has recently been demonstrated that BAG3 interacts with heat shock protein HspB6 to promote clearance of aggregated denatured proteins by targeting them for degradation [14], a function that is critical for preventing protein aggregation in skeletal muscle and the peripheral nerve. In addition, BAG3 deficiency causes a reduction in the endogenous levels of LC3-II, a key molecule involved in macroautophagy [15].
In conclusion, we describe three families with young children showing a severe phenotype of myofibrillar myopathy and axonal neuropathy with giant axons caused by the BAG3 p.Pro209Leu mutation. A recurrent parent-to-child transmission occurred from a completely asymptomatic parent showing somatic mosaicism for the mutation. The disease in two other families was also associated with de novo germline mutations. Counseling of families with presumed de novo mutations should include parental evaluation for somatic mosaicism, but caution is required about the risk of recurrence as low levels of somatic mosaicism may not be detectable in genomic DNA.
Acknowledgments
The authors are grateful to the patients and members of the affected families for the enthusiastic participation in this study. This research was supported in part by the Intramural Research Program of the National Institute of Neurological Disorders and Stroke, National Institutes of Health. Diagnostic and advisory service for rare neuromuscular disorders in the Newcastle upon Tyne area was funded by the UK National Commissioning Group; Newcastle University is a partner in the TREAT-NMD EU Network of Excellence (EC, 6th FP, proposal no. 036825; www.treat-nmd.eu).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nakano S, Engel AG, Waclawik AJ, et al. Myofibrillar myopathy with abnormal foci of desmin positivity. 1. Light and electron microscopy analysis of 10 cases. J Neuropathol Exp Neurol. 1996;55:549–62. doi: 10.1097/00005072-199605000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Selcen D, Ohno K, Engel AG. Myofibrillar myopathy: clinical, morphological and genetic studies in 63 patients. Brain. 2004;127:439–51. doi: 10.1093/brain/awh052. [DOI] [PubMed] [Google Scholar]
- 3.Goldfarb LG, Dalakas MC. Tragedy in a heartbeat: malfunctioning desmin causes skeletal and cardiac muscle disease. J Clin Invest. 2009;119:1806–13. doi: 10.1172/JCI38027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park KY, Dalakas MC, Goebel HH, et al. Desmin splice variants causing cardiac and skeletal myopathy. J Med Genet. 2000;37:851–57. doi: 10.1136/jmg.37.11.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dagvadorj A, Olivé M, Urtizberea JA, et al. West European cluster of patients with severe cardioskeletal myopathy associate with a de novo R406W mutation in desmin. J Neurol. 2004;251:143–9. doi: 10.1007/s00415-004-0289-3. [DOI] [PubMed] [Google Scholar]
- 6.Selcen D, Engel AG. Mutations in myotilin cause myofibrillar myopathy. Neurology. 2004;62:1363–71. doi: 10.1212/01.wnl.0000123576.74801.75. [DOI] [PubMed] [Google Scholar]
- 7.Selcen D, Engel AG. Mutations in ZASP define a novel form of muscular dystrophy in humans. Ann Neurol. 2005;57:269–76. doi: 10.1002/ana.20376. [DOI] [PubMed] [Google Scholar]
- 8.Olivé M, Goldfarb LG, Shatunov A, et al. Myotilinopathy: refining the clinical and myopathological phenotype. Brain. 2005;128:2315–26. doi: 10.1093/brain/awh576. [DOI] [PubMed] [Google Scholar]
- 9.Vorgerd M, van der Ven PF, Bruchertseifer V, et al. A mutation in the dimerization domain of filamin c causes a novel type of autosomal dominant myofibrillar myopathy. Am J Hum Genet. 2005;77:297–304. doi: 10.1086/431959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Selcen D, Muntoni F, Burton BK, et al. Mutation in BAG3 causes severe dominant childhood muscular dystrophy. Ann Neurol. 2009;65:83–9. doi: 10.1002/ana.21553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Homma S, Iwasaki M, Shelton GD, et al. BAG3 deficiency results in fulminant myopathy and early lethality. Am J Pathol. 2006;169:761–73. doi: 10.2353/ajpath.2006.060250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabatelli M, Bertini E, Ricci E, et al. Peripheral neuropathy with giant axons and cardiomyopathy associated with desmin type intermediate filaments in skeletal muscle. J Neurol Sci. 1992;109:1–10. doi: 10.1016/0022-510x(92)90086-z. [DOI] [PubMed] [Google Scholar]
- 13.Zlotogora J. Germ line mosaicism. Hum Genet. 1998;102:381–6. doi: 10.1007/s004390050708. [DOI] [PubMed] [Google Scholar]
- 14.Fuchs M, Poirier DJ, Seguin SJ, et al. Identification of the key structural motifs involved in HspB8/HspB6-Bag3 interaction. Biochem J. 2009;425:245–55. doi: 10.1042/BJ20090907. [DOI] [PubMed] [Google Scholar]
- 15.Carra S, Seguin SJ, Lambert H, Landry J. HspB8 chaperone activity toward poly(Q)-containing proteins depends on its association with Bag3, a stimulator of macroautophagy. J Biol Chem. 2008;283:1437–44. doi: 10.1074/jbc.M706304200. [DOI] [PubMed] [Google Scholar]