Abstract
To our knowledge, the recommendation to measure cerebrospinal opening pressure in the extended, rather than flexed lateral recumbent position to avoid false elevation of the opening pressure has not been formally evaluated in children. 53 children from a single center prospective study had their opening pressure measured in both the flexed and extended lateral recumbent positions prior to removing any cerebrospinal fluid (mean age 11.7 years; 60% male). The difference between the mean opening pressure in flexed (25.1±9.2 cm H2O) and extended (24.4±8.4 cm H2O) positions reached statistical significance (mean difference = 0.6±2.2 cm H2O; Z = 2.021, p< 0.03). 92.4% of opening pressure measures had less than a 5cm H2O difference between positions. Lumbar puncture performed in the extended, rather than flexed lateral recumbent position results in a statistically significant decrease in cerebrospinal fluid opening pressure, although the magnitude of the difference is small and of doubtful clinical significance.
INTRODUCTION
Current recommendations for measuring the cerebrospinal fluid opening pressure obtained during lumbar puncture include performance of lumbar puncture in the lateral recumbent position, followed by repeat measurement after extension of the legs and placement of the neck in the neutral position. 1,2,3 Extending the legs is thought to decrease intra-abdominal pressure, thereby avoiding false elevations of the opening pressure. In our experience, many pediatric lumbar punctures are performed with the patient in the flexed lateral recumbent position without returning the patient to the extended position for measurement of opening pressure.
Although measurement of opening pressure in the extended, rather than the flexed lateral recumbent position is recommended, to our knowledge, the difference between these measurements has not been formally evaluated in children. We conducted this study to assess the validity of required opening pressure measurement in both the flexed and extended position, under the hypothesis that patient position during lumbar puncture does not significantly alter opening pressure measurement in children.
METHODS
Study Design and Setting
This was a prospective cohort study conducted at The Children's Hospital of Philadelphia, a large, urban, tertiary care children's hospital. Institutional review board approval was obtained prior to study initiation.
Study Participants
Children greater than 1 and less than 19 years of age undergoing lumbar puncture in either the outpatient or inpatient setting at The Children's Hospital of Philadelphia main campus were prospectively enrolled in a study of cerebrospinal fluid opening pressure between February 2007 and February 2008. Patients were eligible for the current study if their opening pressure was measured in both the flexed and extended position during the same lumbar puncture, prior to removal of any cerebrospinal fluid. Patients who had their opening pressure recorded in only one position were not included in the current study. The decision to record the opening pressure in the flexed and or extended lateral recumbent position was made by the physician performing the lumbar puncture. The physicians performing the lumbar puncture were blinded to the study hypothesis. Clinical history was obtained through review of medical records.
Patients were excluded if they had an indwelling ventricular shunt or a history of a brain tumor. Consent from the parent and verbal assent from the child (when applicable) was obtained. Patients were also excluded if consent from the parent and verbal assent from the child (where appropriate) were not provided.
Data Collection and Study Protocol
Immediately after completion of lumbar puncture and opening pressure measurement, the physician performing the procedure recorded the opening pressure measurement (cm H20) in both flexed and or extended lateral recumbent position and the depth of patient sedation during lumbar puncture using previously defined categories (No Sedation, Minimal Sedation/Anxiolysis, Moderate Sedation/Conscious Sedation, Deep Sedation)6. The opening pressure measurement was determined using the highest resting cerebrospinal fluid level, in cm H2O, when sustained for at least 10 seconds.
Statistical Analysis
The Wilcoxon sign rank test, a non-parametric alternative to the paired t-test, was used to compare opening pressure measures between the flexed and extended lateral recumbent position within each subject. The Spearman correlation coefficient, a non-parametric measure of correlation, was used to assess the relationship between mean opening pressure values and differences in opening pressure between the extended and flexed lateral recumbent positions. A p-value <0.05 was considered statistically significant. Linear regression was used to determine adjusted associations of age, length of lumbar puncture needle, training level of physician performing lumbar puncture, and depth of patient sedation during the lumbar puncture on the difference in opening pressure measures between the two positions. Due to the small number of patients not receiving any sedation, these subjects were combined with the minimal sedation/anxiolysis group. Level of training was dichotomized into resident (all levels) and fellow/attending. Data were analyzed using commercially available software (STATA, version 10; StataCorp, College Station, Texas). A Bland-Altman plot was used to assess agreement between two opening pressure measurement techniques (i.e., flexed and extended lateral recumbent positions).7
RESULTS
Of the 241 subjects enrolled, 50 (20.7%) had their opening pressure measured in both the flexed and extended lateral recumbent positions, and were eligible for inclusion in this study. One patient had opening pressures measured on three separate occasions and one patient had opening pressures measured on two separate occasions, therefore 53 opening pressure measurements were included in the study. The mean age was 11.4 years (range: 1.1 – 18.2), and 30 (60%) of subjects were male. The mean body mass index was 20.2 (range: 9.5 – 44.9). 13 of 53 (24.5%) of the subjects were minimally sedated or not sedated at all. Headache and idiopathic intracranial hypertension were the most common discharge diagnoses in the study subjects. The subjects excluded from the analysis had an infectious etiology or meningitis as the most common discharge diagnosis.
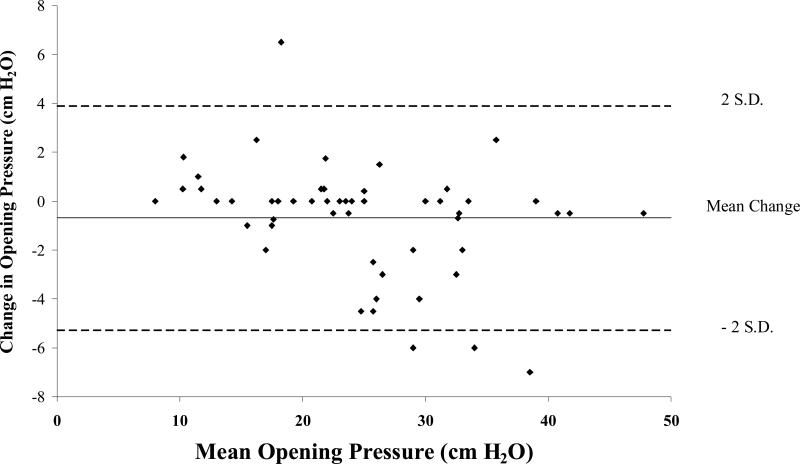
The difference between the mean opening pressures in flexed (25.1 ± 9.2 cm H2O) and extended (24.4 ± 8.4 cm H2O) position reached statistical significance (Wilcoxon sign rank test, Z = 2.021, p = 0.03). The mean difference between positions (extended minus flexed ) was -0.6 ± 2.2 cm H2O, with a range of +6.5 cm H2O to -7 cm H2O. Forty-nine of 53 (92.4%) opening pressure measures changed by less than 5 cm H2O between the two positions. Of the 4 patients who had a 5 cm H2O or greater change in opening pressure when moved from the flexed to the extended position, the opening pressure decreased for three patients, while one patient's opening pressure increased when moved from the flexed to the extended position. The Bland-Altman plot (Figure 1) demonstrates each subject's change in opening pressure (extended opening pressure minus flexed opening pressure) as compared to their average opening pressure. There was a statistically significant negative correlation (r = -.40, p = .003) between the mean opening pressure and change in opening pressure between positions.
Figure 1.
Bland-Altman plot with change in the opening pressure (extended minus flexed ) plotted on the Y-axis and average opening pressure (sum of the flexed and extended opening pressure measures divided by two) plotted on the X-axis.
The results of multivariable linear regression failed to demonstrate a significant effect (p > 0.05) patient age, length of lumbar puncture needle, level of training, and depth of sedation on differences in opening pressure measurements between the flexed and extended lateral recumbent position.
DISCUSSION
To our knowledge, this is the first study to evaluate the effect of patient position on cerebrospinal fluid opening pressure in a pediatric population. Despite finding a statistical difference in opening pressure between the flexed and extended position, this difference is relatively small and of doubtful clinical significance. Measurement of opening pressure in a single position can be of benefit to both the operator and patient, as patient movement during performance of lumbar puncture introduces the potential for lumbar puncture complications such as needle displacement, which can lead to increased time of the procedure, and even failure of the lumbar puncture. Additionally, since procedural sedation is often used, dual position opening pressure measurement increases time of the lumbar puncture, may arouse the calm patient, and therefore may increase the sedation time or even administration of additional sedative medications. However, in the current study, we were unaware of complications that occurred as a result of moving the patient from the flexed to extended position.
Our results are similar to previous reports that found, on average, small differences (i.e., < 2 cm H2O) in opening pressure between positions in adults.4,5 Both studies also found that some patients surprisingly had an increase in cerebrospinal fluid opening pressure when moving from the flexed to the extended position, but neither offered an explanation or hypothesis regarding this finding.4,5
A wide range of opening pressure values were observed in our study, although a majority of patients in our study had an opening pressure greater than 20 cm H2O. Three of 4 patients with a greater than 5 cm H2O change in opening pressure when moved from the flexed to the extended position, had an opening pressure greater than 20 cm H2O, although some suggest that a normal opening pressure in children can be as high as 28 cm H2O.8 We found a significant negative correlation between mean opening pressure and change in opening pressure, suggesting that a larger decrease in opening pressure occurs at a higher opening pressure; however, the decreases were relatively small in magnitude. In adults, most changes in opening pressure greater than 5 cm H2O when moving from flexed or extended position also occurred in subjects with an opening pressure greater than 20 cm H2O.4,5
Degree of sedation has anecdotally been reported to affect the opening pressure in children.9 The results from our study found that the difference in opening pressure between positions was not influenced by depth of sedation. Whether depth of sedation independently influences opening pressure (e.g., deeper sedation results in a lower opening pressure), has not been studied and could not be addressed in our small sample size.
Our study had some degree of selection bias since not all patients enrolled in our study had their opening pressure measured in both the flexed and extended lateral recumbent positions. It is unclear what factors influenced some physicians to measure opening pressure in both positions while others measured opening pressure in just one position. Either most physicians are unaware of the need to move the patient from the flexed to the extended position, or they are fearful that moving the patient may cause them to displace the spinal needle and lose cerebrospinal fluid flow. The percentage of patients being diagnosed with headache or idiopathic intracranial hypertension was higher in our study group as compared to those subjects who were excluded from the analysis. This bias may reflect added attention in obtaining an accurate opening pressure in those subjects with a suspicion of high intracranial pressure. Another limitation of our study is that a majority of patients were sedated for their lumbar puncture. Our findings may not be applicable to other centers that do not sedate patients for lumbar puncture.
Conclusion
Lumbar puncture performed in the extended, rather than the flexed lateral recumbent position results in a statistically significant decrease in cerebrospinal fluid opening pressure, although the magnitude of the difference is small and of doubtful clinical significance. Therefore, sedated children undergoing lumbar puncture in the flexed lateral recumbent position do not need to have their legs extended to obtain another opening pressure measurement.
Acknowledgements
The investigators are indebted to all of the physicians at Children's Hospital of Philadelphia who helped enroll subjects and complete the study forms. We are thankful for the support of the faculty and research staff in the Division of Neurology, Department of Emergency Medicine, and Department of Anesthesiology and Critical Care at Children's Hospital of Philadelphia.
Funding support: Dr. Avery received support from the National Institute of Health Loan repayment program and 1T32NS061779-01 Neurologic Clinical Epidemiology Training Program, PI: Laura Balcer, MD). Dr. Shah received support from the National Institute of Allergy and Infectious Diseases (K01 AI73729) and the Robert Wood Johnson Foundation under its Physician Faculty Scholar Program. Dr. Huh received support from National Institute of Neurological Disorders and Stroke (NS053651). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Financial disclosures: none
Conflict of interests: none
Presented in part at the Annual Meeting of the Child Neurology Society, Santa Clara, CA, November, 2008.
REFERENCES
- 1.Fishman RA. Cerebrospinal Fluid in Diseases of the Nervous System. 2nd ed. WB Saunders; Philadelphia, PA: 1992. [Google Scholar]
- 2.Adams RD, Maurice V, Ropper AH. Principles of Neurology. 6th Edition McGraw-Hill; New York, NY: 1997. [Google Scholar]
- 3.Corbett JJ, Mehta MP. Cerebrospinal fluid opening pressure in normal obese subjects and patients with pseudotumor cerebri. Neurology. 1983;33:1386–1388. doi: 10.1212/wnl.33.10.1386. [DOI] [PubMed] [Google Scholar]
- 4.Abbrescia KL, Brabson TA, Dalsey WC, Kelly JJ, Kaplan JL, the Lumbar Puncture Study Group The effect of lower-extremity position on cerebrospinal fluid pressures. Acad Emerg Med. 2001;8:8–12. doi: 10.1111/j.1553-2712.2001.tb00538.x. [DOI] [PubMed] [Google Scholar]
- 5.Sithinamsuwan P, Sithinamsuwan N, Tejavanija S, Udommongkol C, Nidhinandana S. The effect of whole body position on lumbar cerebrospinal fluid opening pressure. Cerebrospinal Fluid Res. 2008;5:11. doi: 10.1186/1743-8454-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics, Committee on Drugs Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: Addendum. Pediatrics. 2002;110:836–838. doi: 10.1542/peds.110.4.836. [DOI] [PubMed] [Google Scholar]
- 7.Altman DF, Bland JM. Measurement in medicine: the analysis of method comparison studies. Statistician. 1983;32:307–317. [Google Scholar]
- 8.Ellis R. Lumbar cerebrospinal fluid opening pressure measured in a flexed lateral decubitus position in children. Pediatrics. 1994;93:622–623. [PubMed] [Google Scholar]
- 9.Haslam RHA. Neurologic Evaluation. In: Behrman, Kliegman, Jenson, editors. Nelson Textbook of Pediatrics. 17th ed. Saunders; Philadelphia, PA: 2004. pp. 2440–2441. [Google Scholar]