Given the increasing complexity of oncologic care and population of patients and survivors requiring care, PAs/NPs have the potential to fill important roles in outpatient and inpatient care settings.
Abstract
Purpose:
It is expected that over the next 10 to 15 years, demand for oncology services will increase, potentially surpassing the supply of available oncologists. Physician assistants (PAs) and nurse practitioners (NPs) have the potential to address the anticipated shortage in physician supply. The two objectives of this study were to define how National Cancer Institute (NCI) –designated comprehensive cancer centers use PAs/NPs and to pilot a self-reported PA/NP productivity tool.
Methods:
An online survey addressing practice patterns and productivity in 4-hour outpatient oncology clinics was administered to PAs/NPs practicing at 15 National Comprehensive Cancer Network member institutions.
Results:
A total of 206 PAs/NPs were included in the final analysis. NPs and PAs reported similar clinical activities, with the following exceptions: NPs reported spending more time on telephone triage, and PAs reported spending more time on procedures. Overall, PAs/NPs reported seeing more follow-up (mean, 6.1; standard deviation [SD], 3.5) than new patients (mean, 1.2; SD, 1.3) per clinic. NPs with a medical oncology specialty reported a marginally greater productivity among follow-up patients than did PAs. Otherwise, NPs and PAs saw a similar number of patients regardless of specialty.
Conclusion:
To our knowledge, this is the first study attempting to characterize PA/NP clinical activities and define productivity benchmarks at NCI-designated comprehensive cancer centers. Given the increasing complexity of oncologic care and the increased population of patients with cancer and cancer survivors requiring that care, PAs/NPs have the potential to fill important roles in both outpatient and inpatient care settings.
Introduction
Recent studies have shown that the demand for oncology services will increase dramatically over the next 10 to 15 years, with an acute shortage of oncologists predicted by the year 2020.1 Solutions to this problem have primarily focused on either increasing the supply of services or decreasing the demand for oncologists. Examples include delaying retirement for currently practicing oncologists, using information technology to increase productivity of the existing oncology workforce, increasing the use of palliative and supportive care providers to care for patients at the end of life, increasing the use of primary care providers for survivors, increasing the number of fellowship and training opportunities, and increasing the use of physician assistants (PAs) and nurse practitioners (NPs).
PAs and NPs in particular have the potential to reduce the shortfall in physician supply by effectively extending oncologists' time and increasing their clinical productivity. PAs/NPs have served professionally in oncology practices for more than 30 years.2,3 A PA is a clinician licensed to practice medicine under a physician's supervision. PAs are not nurses and do not necessarily have a clinical background before beginning their PA training, which entails 2 to 3 years of scientific education and clinical training in the medical model. NPs are licensed advanced practice nurses who have clinical training as registered nurses before undertaking additional postgraduate studies. For both PAs and NPs, scope of practice and licensure may vary by state.
Although many academic oncology practices incorporate PAs/NPs in outpatient and inpatient care, little information is available to facilitate an understanding of the specific capacities of PAs/NPs as physician extenders and providers of care or how productive PAs/NPs are in fulfilling these roles. As the number of PAs/NPs in academic oncology practices grows, methodologies for measuring productivity are needed to maximize use of these caregivers. The ability to determine appropriate well-defined roles and productivity benchmarks will assist with decisions related to compensation, funding, and plans for clinical staffing.4 Unlike physicians, whose productivity can be assessed based on billing data and resource-value units (RVUs), many PA/NP services are not billed directly or are billed “incident to” physician services, meaning the nonphysician services are billed in conjunction with the physician services or as if they had been provided by a physician. Furthermore, PAs/NPs may conduct shared visits with physicians, complicating attempts to determine individual clinician productivity.
Because of these factors, alternative metrics for assessing PA/NP productivity must be developed so that the contributions of PAs/NPs to the oncology care team can be sufficiently measured. The two primary objectives of this study were to define how National Cancer Institute (NCI) –designated comprehensive cancer centers use PAs/NPs and to pilot a self-reported PA/NP productivity instrument that may be efficiently deployed in oncology clinics.
Methods
Sample Population
The study population was composed of PAs/NPs from the 21 NCI-designated comprehensive cancer centers that comprise the National Comprehensive Cancer Network (NCCN) membership. The sample population is a convenience sample of PAs/NPs from NCCN member institutions. All data were collected using a self-report online survey. The online survey was distributed via e-mail to PAs/NPs using the internal e-mail list of each institution. Survey distribution was conducted through the NCCN Best Practices Committee (BPC). The NCCN BPC is composed of cancer center administrators and executives, including a number of individuals with both clinical oncology and administrative backgrounds, from NCCN member institutions. The survey was deployed using a Web-based survey tool by SurveyMonkey (Portland, OR). The survey remained available online for approximately 1 month, from April 4, 2006, to May 3, 2006. Members of the NCCN BPC were sent a reminder to invite PAs/NPs to respond after the first 2 weeks.
Fifteen NCCN member institutions chose to participate in the study by distributing the survey to their PA/NP populations. Participating institutions included the City of Hope (Duarte, CA), Fox Chase Cancer Center (Philadelphia, PA), Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University (Baltimore, MD), Fred Hutchinson Cancer Research Center (Seattle, WA), Massachusetts General Hospital (a component of Partners Healthcare and member of the NCCN as the Dana-Farber/Brigham and Women's Cancer Center, Massachusetts General Hospital Cancer Center; Boston, MA), Huntsman Cancer Institute at the University of Utah (Salt Lake City, UT), University of Texas M. D. Anderson Cancer Center (Houston, TX), University of Michigan Comprehensive Cancer Center (Ann Arbor, MI), H. Lee Moffitt Cancer Center & Research Institute (Tampa, FL), Eppley Cancer Center at the University of Nebraska Medical Center (Omaha, NE), Roswell Park Cancer Institute (Buffalo, NY), Siteman Cancer Center at the Barnes-Jewish Hospital and Washington University School of Medicine (St Louis, MO), Stanford Comprehensive Cancer Center (Stanford, CA), University of Alabama at Birmingham Comprehensive Cancer Center (Birmingham, AL), and University of California San Francisco Helen Diller Family Comprehensive Cancer Center (San Francisco, CA). A total of 262 PAs/NPs from these cancer centers responded to the survey (Fig 1).
Figure 1.
Respondent flowchart with distribution of specialties in final cohort. BMT, bone marrow transplantation.
PA/NP respondents were excluded from the quantitative (productivity) analysis if they reported spending no time in outpatient clinics (n = 12) or reported not seeing any patients in outpatient oncology clinics (n = 9; Fig 1). In general, PAs/NPs who were excluded from the productivity analysis were either working primarily in the inpatient setting or assisting with procedures and administrative duties rather than seeing patients in outpatient clinics. PAs/NPs were also excluded from the analysis if they did not complete the productivity tool (n = 35). Only PAs/NPs reporting a medical oncology (MO), hematologic malignancies or stem cell/bone marrow transplantation (Hem/BMT), or surgical oncology (SO) specialty were included in the productivity analysis (n = 176). Respondent comments were reviewed to assess difficulties in completing the productivity tool.
Survey Development
Each survey respondent was required to provide a name and e-mail address so that he or she could be validated against a list of PAs/NPs that was to be furnished by each participating institution. Ten of the participating institutions agreed to furnish such lists for validation. Because the NCCN did not have access to a global list of PAs/NPs at all participating institutions, the response rate of the survey could not be determined.
The survey instrument was initially developed by representatives of the NCCN BPC, including physicians and executive administrators, PAs/NPs working with these NCCN BPC members, and NCCN staff. The survey and PA/NP productivity tool was refined and assessed for content validity by a focus group of PAs/NPs, administrators, and physicians from the University of Michigan Comprehensive Cancer Center and the Fred Hutchinson Cancer Research Center. The survey contained sections on provider characteristics (type of provider, practice specialties, years of experience), work hours and time split (percentage of time spent on clinical, administrative, research, and teaching activities), on-call and emergency coverage, and time spent in outpatient specialty clinics.
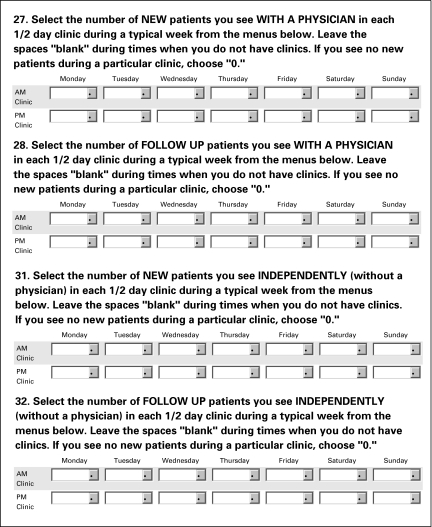
The PA/NP productivity tool was developed to quantify the number of patients seen by a PA/NP per half-day, 4-hour clinic during a typical work week. PAs/NPs were asked to separately provide the number of new patients they saw with a physician, follow-up patients they saw with a physician, new patients they saw independently, and follow-up patients they saw independently. From reviews of participant comments, it seemed as though the definition of “patients seen independently” was not interpreted consistently by all respondents. To address this inconsistent interpretation, reported patients seen “independently” and “with a physician” were combined in all analyses for both new and follow-up patients seen. PAs/NPs reported productivity using a matrix of drop-down menus (Fig 2), with days of the week arrayed across the x-axis and morning or afternoon clinic arrayed across the y-axis.
Figure 2.
Image of the National Cancer Care Network physician assistant (PA)/nurse practitioner (NP) productivity tool containing drop-down menus from which PAs/NPs may select number of patients seen per outpatient clinic.
Analytic Methods
Survey results were maintained and analyzed in a de-identified database to ensure participant confidentiality. All data analyses were conducted using SAS software (SAS, Version 9.1; Cary, NC). Statistically significant differences between groups involving proportions were assessed using Pearson's χ2 tests and between interval data using either t-tests or analysis of variance. The Satterthwaithe adjusted t-test (ts) was used where unequal variances were observed.
Results
A total of 206 PA/NP respondents (79%) were included in the quantitative analysis (Fig 1). Approximately half of PAs/NPs (54%) across all specialties reported working for another institution before gaining their current employment, with 30% of PAs/NPs reporting having worked at three or more institutions. Only 13% of PAs/NPs reported rotating among disease-specific clinics, with the highest rates occurring among PAs/NPs with an MO specialty (22%) and the lowest rates occurring among those with a Hem/BMT specialty (5%). Overall, 42% of PAs/NPs had less than 3 years of seniority, and another 41% had between 3 to 10 years of seniority (Table 1). No discernible difference was observed between NPs and PAs with regard to prior employment, clinical rotation, or seniority (data not shown).
Table 1.
Workplace Characteristics by Specialty
| Characteristic | MO |
Hem/BMT |
SO |
Other* |
Total |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| Specialty | 71 | 34 | 57 | 28 | 48 | 23 | 30 | 15 | 206 | |
| Productivity | ||||||||||
| New patients per clinic | ||||||||||
| Mean | 1.0 | 0.8 | 1.8 | 1.4 | 1.2 | |||||
| SD | 1.2 | 1.2 | 1.0 | 1.6 | 1.3 | |||||
| Follow-up patients per clinic | ||||||||||
| Mean | 6.6 | 5.4 | 6.9 | 4.8 | 6.1 | |||||
| SD | 3.9 | 2.9 | 3.4 | 3.1 | 3.5 | |||||
| Provider type | ||||||||||
| NP | 46 | 65 | 23 | 40 | 27 | 56 | 15 | 50 | 111 | 54 |
| PA | 25 | 35 | 34 | 60 | 21 | 44 | 15 | 50 | 95 | 46 |
| No. of institutions of employment | ||||||||||
| 1 | 30 | 42 | 33 | 58 | 21 | 44 | 11 | 37 | 95 | 46 |
| 2 | 18 | 25 | 12 | 21 | 13 | 27 | 7 | 23 | 50 | 24 |
| ≥ 3 | 23 | 32 | 12 | 21 | 14 | 29 | 12 | 40 | 61 | 30 |
| Disease-specific specialty clinic rotation | ||||||||||
| No | 55 | 77 | 54 | 95 | 42 | 89 | 27 | 93 | 178 | 87 |
| Yes | 16 | 22 | 3 | 5 | 5 | 11 | 2 | 7 | 26 | 13 |
| Seniority, years | ||||||||||
| ≤ 3 | 34 | 48 | 21 | 37 | 22 | 46 | 9 | 30 | 86 | 42 |
| 3-10 | 23 | 32 | 26 | 46 | 23 | 48 | 13 | 43 | 85 | 41 |
| > 10 | 14 | 20 | 10 | 17 | 3 | 6 | 8 | 27 | 35 | 17 |
Abbreviations: MO, medical oncology; Hem, hematologic malignancies; BMT, bone marrow transplantation; SO, surgical oncology; SD, standard deviation; NP, nurse practitioner; PA, physician assistant.
Other includes pediatric oncology, radiation oncology, neurooncology, and pain and palliative care.
No significant differences were observed between NPs and PAs who reported spending clinical time seeing patients, completing paperwork and chemotherapy orders, or performing rounds with inpatients. A greater proportion of NPs (62%) than PAs (36%) reported spending more than 10% of their clinical time on telephone triage (χ2 [df, 2] = 16.9; P < .001). A greater proportion of PAs (28%) than NPs (12%) reported spending more than 11% of their clinical time on procedures, infusions, or surgical assistance (χ2 [df, 2] = 13.1; P = .001; Table 2).
Table 2.
Distribution of PA/NP Time Spent on Clinical Activities in Outpatient Clinics
| Time Spent on Clinical Activity (%) | Provider Type |
|||
|---|---|---|---|---|
| NP |
PA |
|||
| No. | % | No. | % | |
| Seeing patients | ||||
| ≤ 50 | 34 | 31 | 36 | 38 |
| 51-69 | 37 | 33 | 29 | 30 |
| ≥ 70 | 40 | 36 | 30 | 32 |
| Telephone triage | ||||
| ≤ 5 | 20 | 18 | 39 | 41 |
| 6-10 | 22 | 20 | 22 | 23 |
| ≥ 11 | 69 | 62 | 34* | 36* |
| Paperwork and chemotherapy orders | ||||
| ≤ 5 | 46 | 41 | 47 | 49 |
| 6-10 | 35 | 31 | 20 | 21 |
| ≥ 11 | 30 | 27 | 28 | 29 |
| Procedures\infusions\surgical assistance | ||||
| 0 | 56 | 50 | 28 | 29 |
| 1-10 | 42 | 38 | 40 | 42 |
| ≥ 11 | 13 | 12 | 27† | 28† |
| Inpatient rounds | ||||
| 0 | 52 | 47 | 43 | 45 |
| 1-5 | 23 | 21 | 18 | 19 |
| > 5 | 36 | 32 | 34 | 36 |
Abbreviations: NP, nurse practitioner; PA, physician assistant.
P < .01.
P < .001.
Overall, PAs/NPs reported seeing six times as many follow-up patients than new patients per clinic. NPs and PAs saw a similar number of new patients regardless of specialty. Among PAs/NPs with an MO specialty, NPs reported a marginally greater productivity with follow-up patients than did PAs (ts [df, 67.7] = 2.06; P = .04). Among PAs/NPs with a Hem/BMT or SO specialty, no significant productivity difference was observed (Table 3). For PAs/NPs with an MO or SO specialty, no association was observed between the number of prior institutions of employment, rotation among clinics, or seniority and PA/NP productivity. Among PAs/NPs with a Hem/BMT specialty, productivity with new patients was higher among senior PAs/NPs with 10 or more years of experience (F [df, 2] = 8.21; P < .001).
Table 3.
Productivity by Specialty, Patient Type, and Workplace Characteristics
| Characteristic | New Patients |
Follow-Up Patients |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MO |
Hem/BMT |
SO |
MO |
Hem/BMT |
SO |
|||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Provider type | ||||||||||||
| NP | 0.9 | 1.3 | 0.7 | 1.3 | 1.9 | 1.2 | 7.2 | 4.3 | 5.3 | 3.7 | 6.4 | 3.2 |
| PA | 1.1 | 1.1 | 0.8 | 1.0 | 1.7 | 0.8 | 5.5* | 2.7* | 5.4 | 2.2 | 7.5 | 3.7 |
| No. of institutions of employment | ||||||||||||
| 1 | 0.8 | 0.6 | 0.5 | 0.5 | 1.8 | 1.1 | 7.1 | 5.1 | 5.9 | 2.8 | 6.7 | 3.5 |
| 2 | 0.8 | 0.6 | 0.9 | 1.8 | 2.1 | 1.0 | 5.7 | 2.5 | 4.7 | 2.7 | 6.8 | 2.9 |
| ≥ 3 | 1.3 | 2.0 | 1.3 | 1.6 | 1.5 | 1.0 | 6.7 | 2.8 | 4.7 | 3.1 | 7.2 | 3.9 |
| Disease-specific specialty clinic rotation | ||||||||||||
| No | 1.0 | 1.3 | 0.7 | 1.2 | 1.8 | 1.0 | 6.9 | 4.2 | 5.3 | 2.9 | 6.7 | 3.4 |
| Yes | 1.1 | 1.1 | 0.6 | 0.5 | 2.1 | 0.9 | 5.7 | 2.2 | 6.1 | 1.7 | 6.5 | 2.4 |
| Seniority, years | ||||||||||||
| ≤ 3 | 1.1 | 1.2 | 0.4 | 0.4 | 1.8 | 0.9 | 6.2 | 2.8 | 5.6 | 2.4 | 6.3 | 3.4 |
| 3-10 | 0.8 | 0.6 | 0.6 | 0.5 | 1.8 | 1.1 | 6.3 | 2.5 | 5.3 | 3.1 | 7.6 | 3.6 |
| > 10 | 0.9 | 1.2 | 2.0† | 2.4† | 1.9 | 1.2 | 8.3 | 6.9 | 5.3 | 3.5 | 5.6 | 1.2 |
Abbreviations: MO, medical oncology; Hem, hematologic malignancies; BMT, bone marrow transplantation; SO, surgical oncology; SD, standard deviation; NP, nurse practitioner; PA, physician assistant.
P < .05.
P < .001.
Discussion
PA/NP productivity in oncology is not well defined. Because of this, the survey instrument was initially developed to be exploratory and observational. Little evidence is available regarding the relationships between productivity and other characteristics, including demographics, time split, on-call activities, and level of independence or partnering in clinical work. To address these limitations, the objectives of the current study were both to define how NCI-designated comprehensive cancer centers use PAs/NPs and to pilot a self-reported PA/NP productivity instrument that may be efficiently deployed in oncology clinics. Additionally, these data may be the first step in developing a benchmark for PA/NP productivity in academic outpatient oncology clinics and could be used to estimate benchmark RVUs in future studies.
To our knowledge, this is the first study attempting to characterize PA/NP clinical activities and define productivity benchmarks at NCI-designated comprehensive cancer centers. Overall, NPs and PAs reported similar clinical activities, except that PAs reported being more procedure oriented, whereas NPs reported spending a greater proportion of their clinical time on telephone triage.
Roles for PAs/NPs in the oncology context are expanding to include their use in wellness clinics, survivorship and long-term follow-up clinics, breast health clinics, pain and palliative care, and other specialty and subspecialty areas within cancer care. However, great variability exists in the use of PAs/NPs in such expanded roles among different institutions. Also, because of differences in institutional policies and/or state licensure and scope-of-practice regulations, some complex and high-risk processes, such as ordering of chemotherapy or independent prescription authority, are still beyond the range of activities for some PAs/NPs. However, these differences in institutional policies and variances in independent prescription authority and other scopes of practice did not seem to have a measurable impact on the productivity of PAs/NPs as defined by this study. Future iterations of the PA/NP productivity survey will attempt to characterize and quantify these roles as well as identify changes in PA/NP practice patterns and clinical activities. In addition, a future project will include linking PA/NP productivity with physician productivity to assess the impact that partnering with PAs and NPs has on physician productivity.
Overall, PAs/NPs had a measurable impact on clinical productivity. PAs/NPs reported seeing approximately six times as many follow-up patients as they did new patients. In part, this may be because of the increased time required to attend to a new versus follow-up patient visit. However, it may also be a result of PAs/NPs being used to attend primarily to follow-up patients while physicians attend to newly presenting patients. Little difference was observed between NPs or PAs with regard to new patients seen per 4-hour clinics. Among follow-up patients, NPs with an MO specialty reported greater productivity than PAs.
Limitations to the current study include use of a convenience sample of PAs/NPs, which may limit the generalizability of the observed results. Additionally, the format of the productivity metric was not applicable to respondents at all participating institutions. For example, some respondents reported working in daily 10-hour clinics across a 4-day schedule. Lastly, these data do not give a clear answer to whether the observed differences in productivity were because of differences in PA/NP efficiency or differences in how NPs and PAs are used in various clinics. To address these limitations, the productivity tool will be reorganized as an array of weekdays (Sunday through Saturday), in which, for each day, participants will be asked to report the number of new patients seen, follow-up patients seen, and hours worked in clinic. In addition, PAs/NPs who bill independently will be asked to indicate this, and the reported productivity of these respondents will be validated using billing data.
As the roles for PAs/NPs in oncology expand, accurate assessment of their practice is necessary so that these clinicians can be used in an efficient and effective manner within institutions and practices. Although models for PA/NP use currently differ widely among oncology practices, better information on PA/NP roles and practice will allow best practices and standards to emerge. Identifying highly effective models for physician/nonphysician partnering and understanding how varying degrees of PA/NP practice independence affect the quality and efficiency of care are two examples of areas where best practices and standards are currently lacking. Given the increasing complexity of oncologic care and the increased population of patients with cancer and cancer survivors requiring that care, PAs/NPs have the potential to fill important roles in both outpatient and inpatient care settings. PAs/NPs can be trained more quickly than oncology specialty physicians and may have greater scheduling and practice flexibility than physicians. Moreover, although this survey did not collect salary information, the employment of PAs/NPs may be financially prudent for institutions or practices seeking to expand capacity and meet demand. At the same time, if expanded use of PAs/NPs as oncology practitioners is to be a viable solution to possible shortages of oncology physicians, ample and effective training opportunities in oncology for PAs/NPs will be necessary to ensure these practitioners are able to take on expanded roles. For example, specialty training programs for PAs/NPs in areas such as oral chemotherapy, breast biopsies, line placements, bone marrow harvests, and survivorship and long-term follow-up could help ensure a well-trained workforce able to keep pace with the delivery of quality cancer care.
Acknowledgment
Research support was provided by the National Comprehensive Cancer Network Best Practices Committee. This study was presented in part at the 45th Annual Meeting of the American Society of Clinical Oncology, Orlando, FL, May 29, 2009-June 2, 2009 (abstr 6628).
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Jennifer M. Hinkel, Sara J. Perkel, Marcy B. Waldinger, William Levy, F. Marc Stewart
Collection and assembly of data: Jennifer M. Hinkel, Sara J. Perkel
Data analysis and interpretation: Jennifer M. Hinkel, Jonathan L. Vandergrift, Sara J. Perkel, F. Marc Stewart
Manuscript writing: Jennifer M. Hinkel, Jonathan L. Vandergrift, Sara J. Perkel, F. Marc Stewart
Final approval of manuscript: Jennifer M. Hinkel, Jonathan L. Vandergrift, Sara J. Perkel, Marcy B. Waldinger, William Levy, F. Marc Stewart
References
- 1.Association of American Medical Colleges. Forecasting the supply of and demand for oncologists: A report to the American Society of Clinical Oncology (ASCO) from the AAMC Center for Workforce Studies. http://www.asco.org/ASCO/Downloads/Cancer%20Research/Oncology%20Workforce%20Report%20FINAL.pdf.
- 2.Yeung KY, Maxwell V. The training and role of the physician assistant in oncologic practice. Pa J. 1976;6:190–192. [PubMed] [Google Scholar]
- 3.Maxwell MB. Nurse practitioner chemotherapy clinic. Cancer Nurs. 1979;2:211–218. [PubMed] [Google Scholar]
- 4.Rhoads J, Ferguson LA, Langford CA. Measuring nurse practitioner productivity. Dermatol Nurs. 2006;18:32–34. 37–38. [PubMed] [Google Scholar]